Geographic Differences in Lung Cancer Incidence: A Study of a Major Metropolitan Area within Southeastern Pennsylvania
Abstract
1. Introduction
2. Materials and Methods
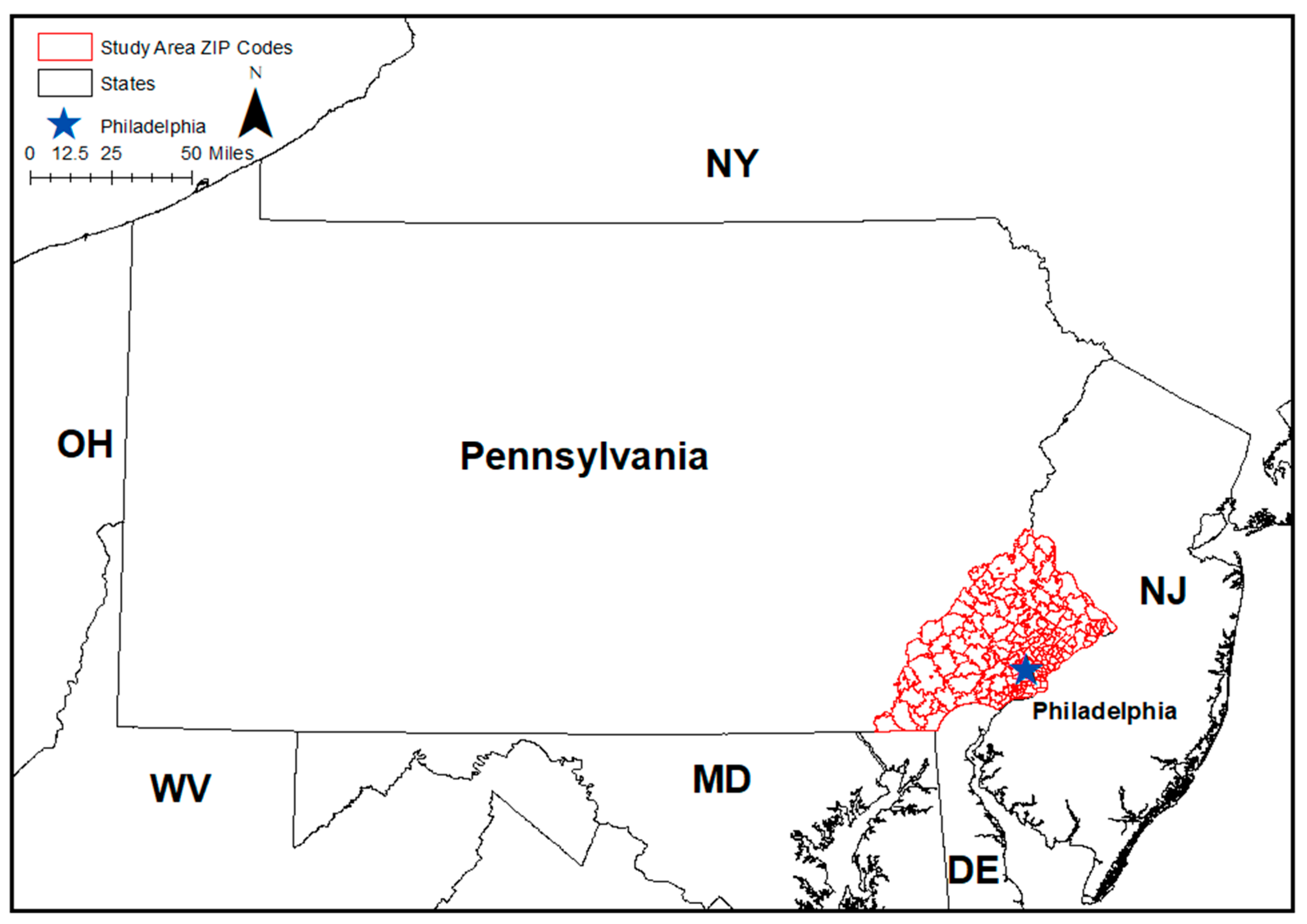
2.1. Study Area
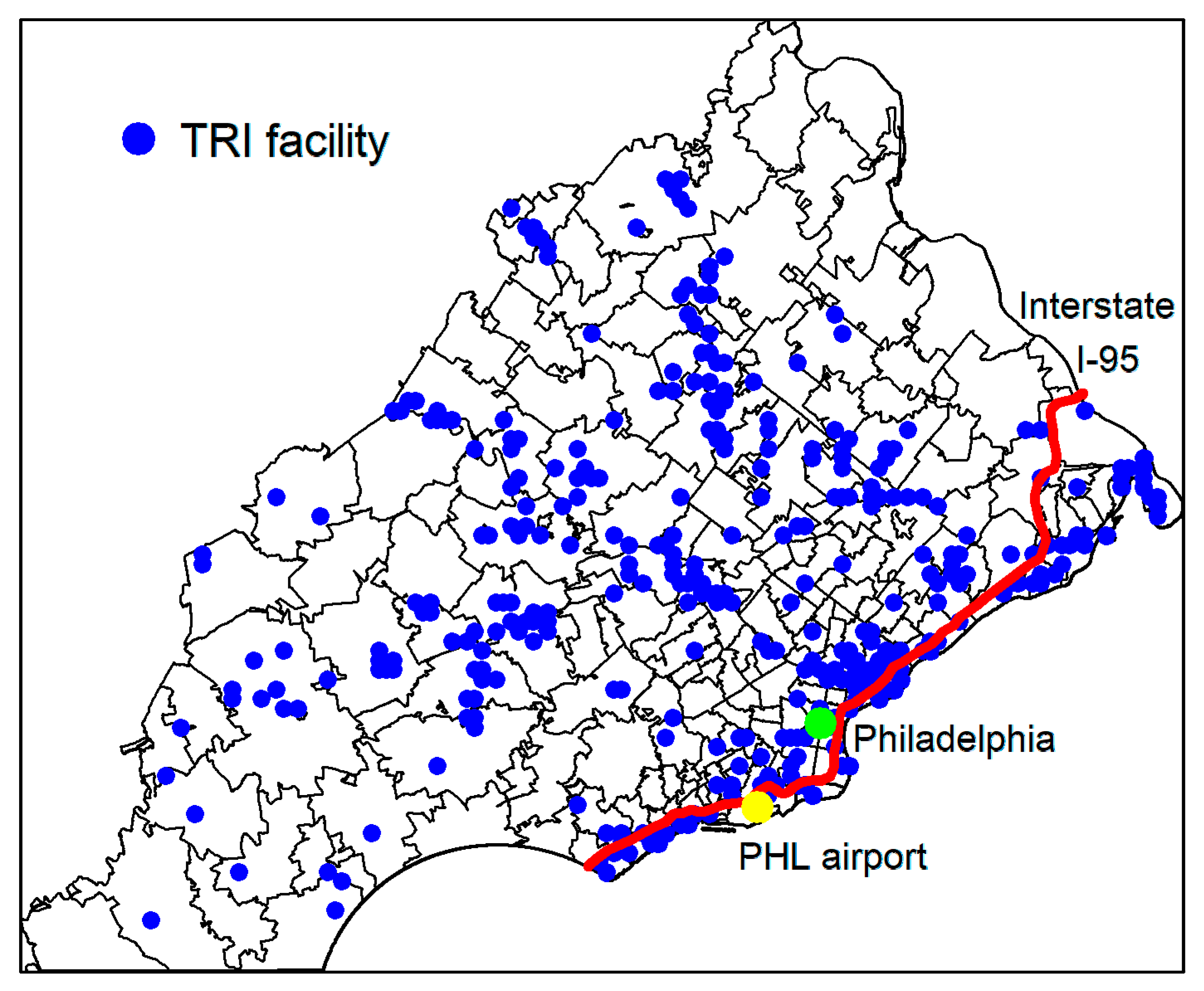
2.2. Data Sources
2.3. Population Size and Covariate Information
2.4. Calculation of Age-Adjusted Incidence Rates
2.5. Mapping of Incidence Rates
2.6. Spatial Autocorrelation and Clustering
3. Results
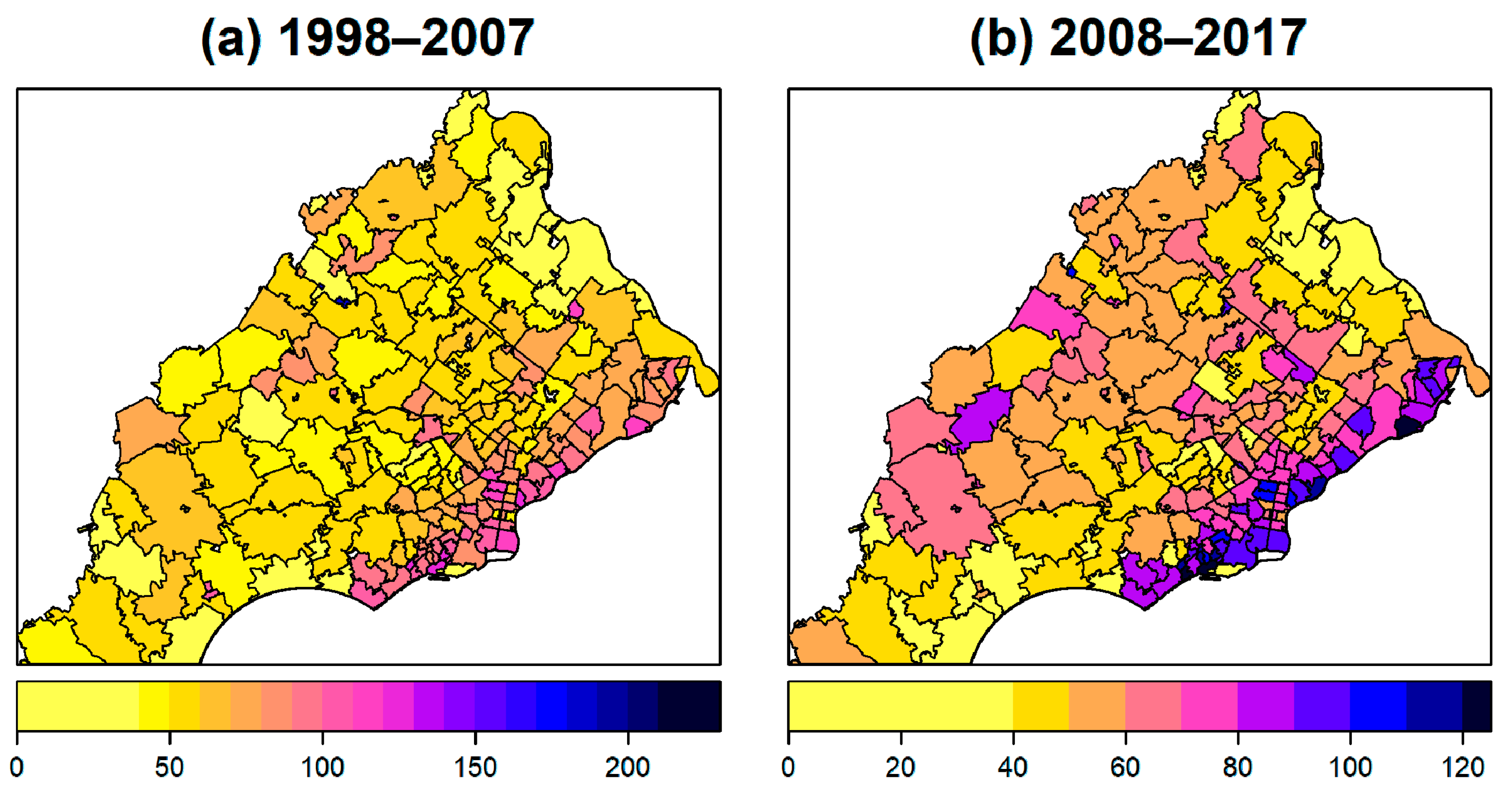
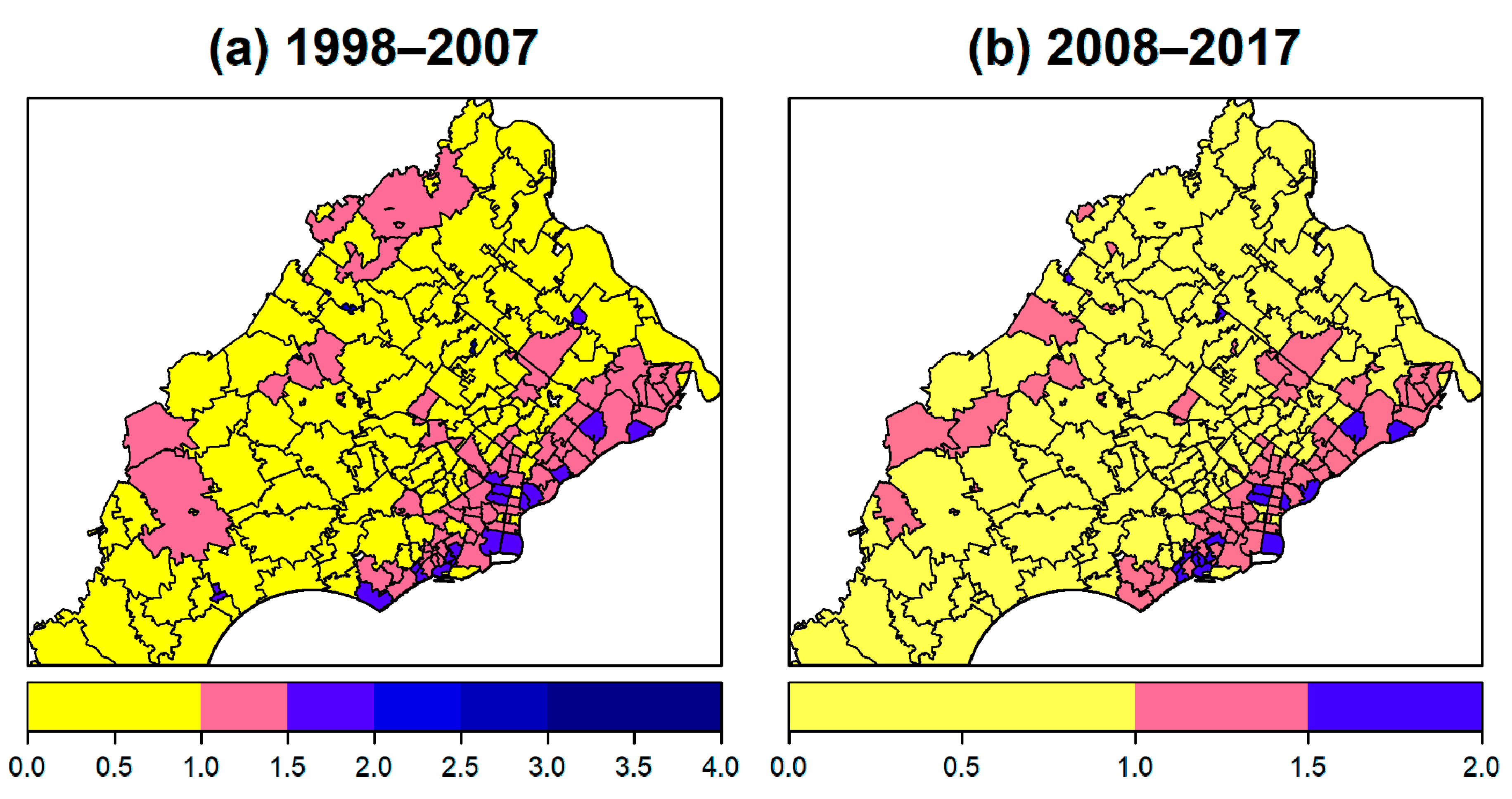
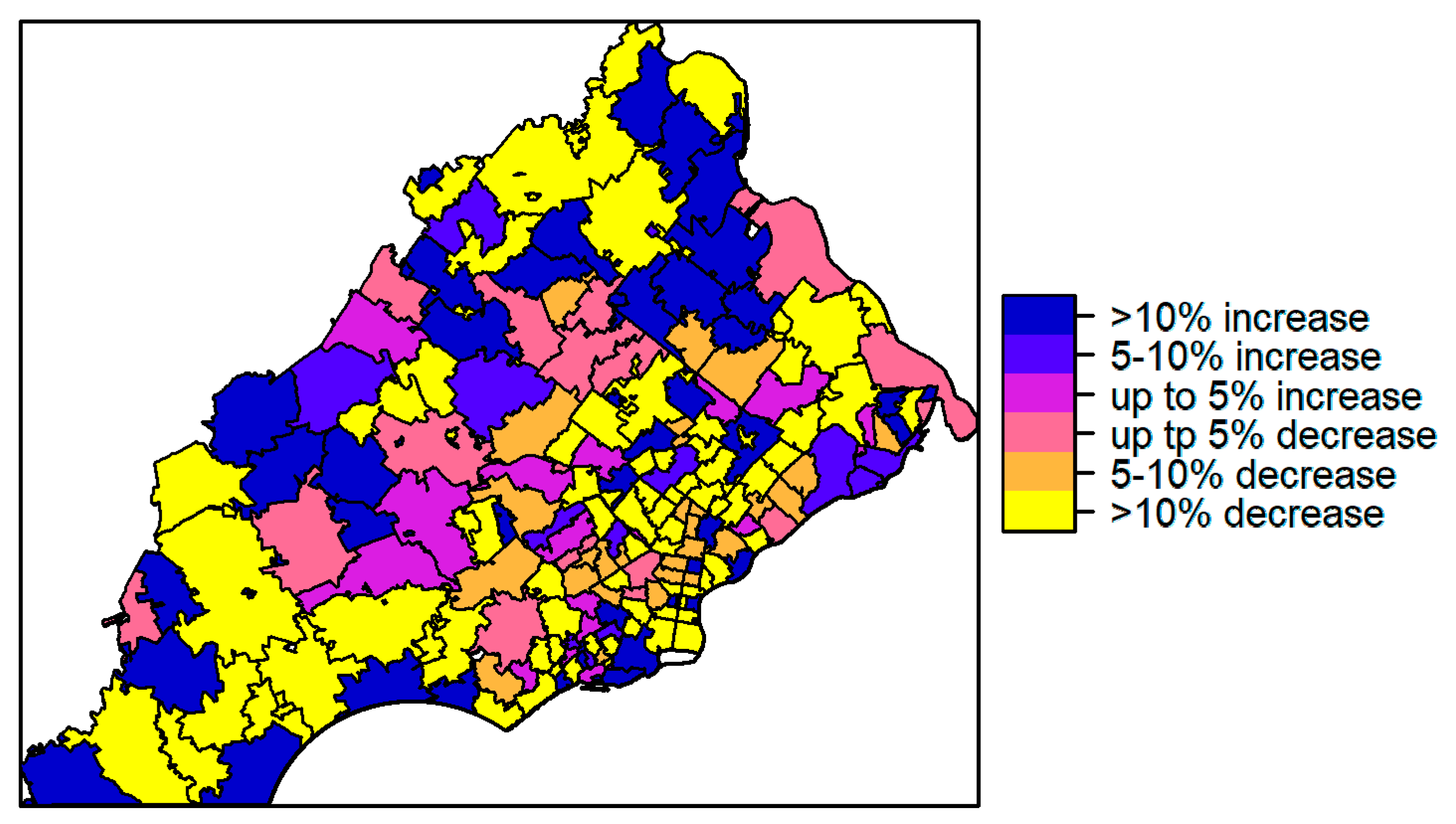
3.1. Mapping of Age-Adjusted Lung Cancer Incidence Rates
3.2. Characterizing ZIP Codes with High Incidence Rates
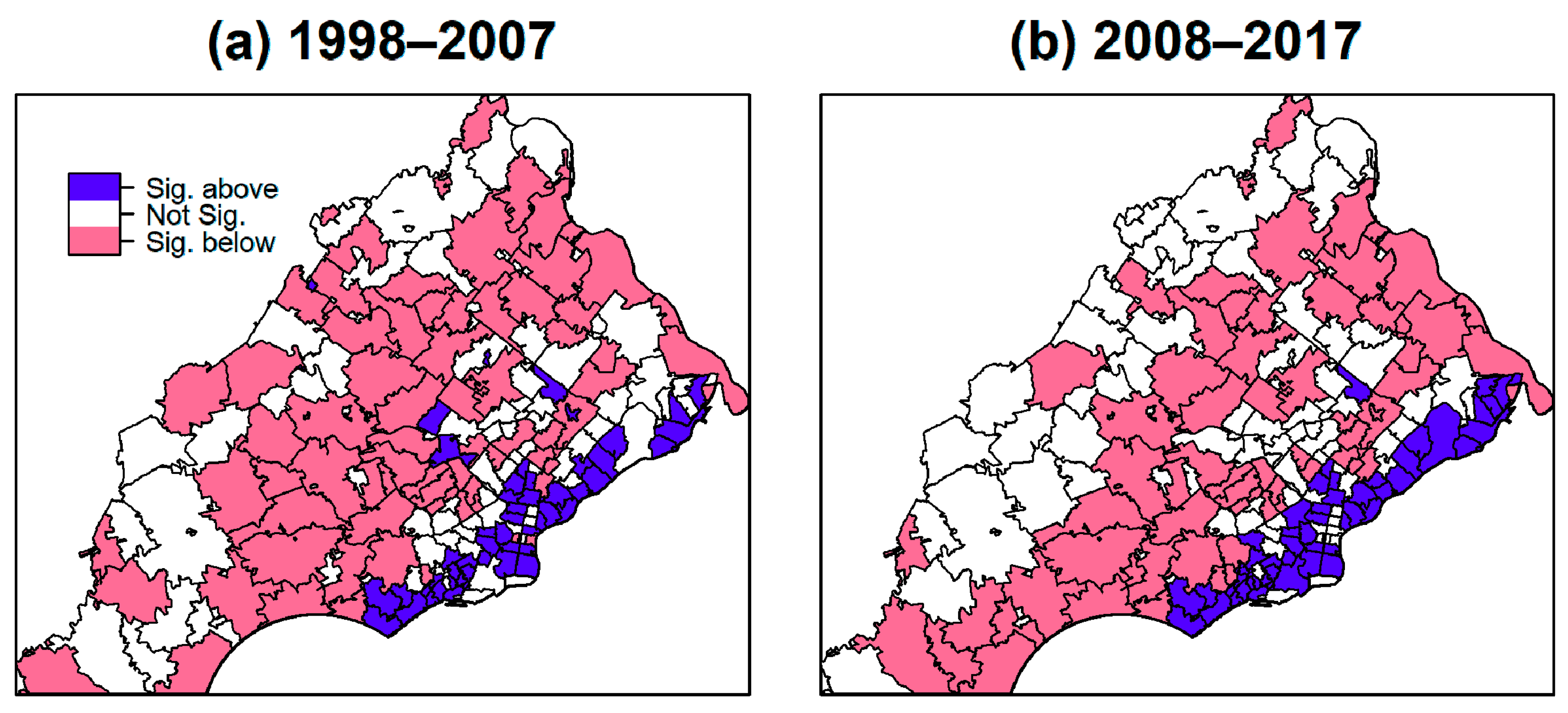
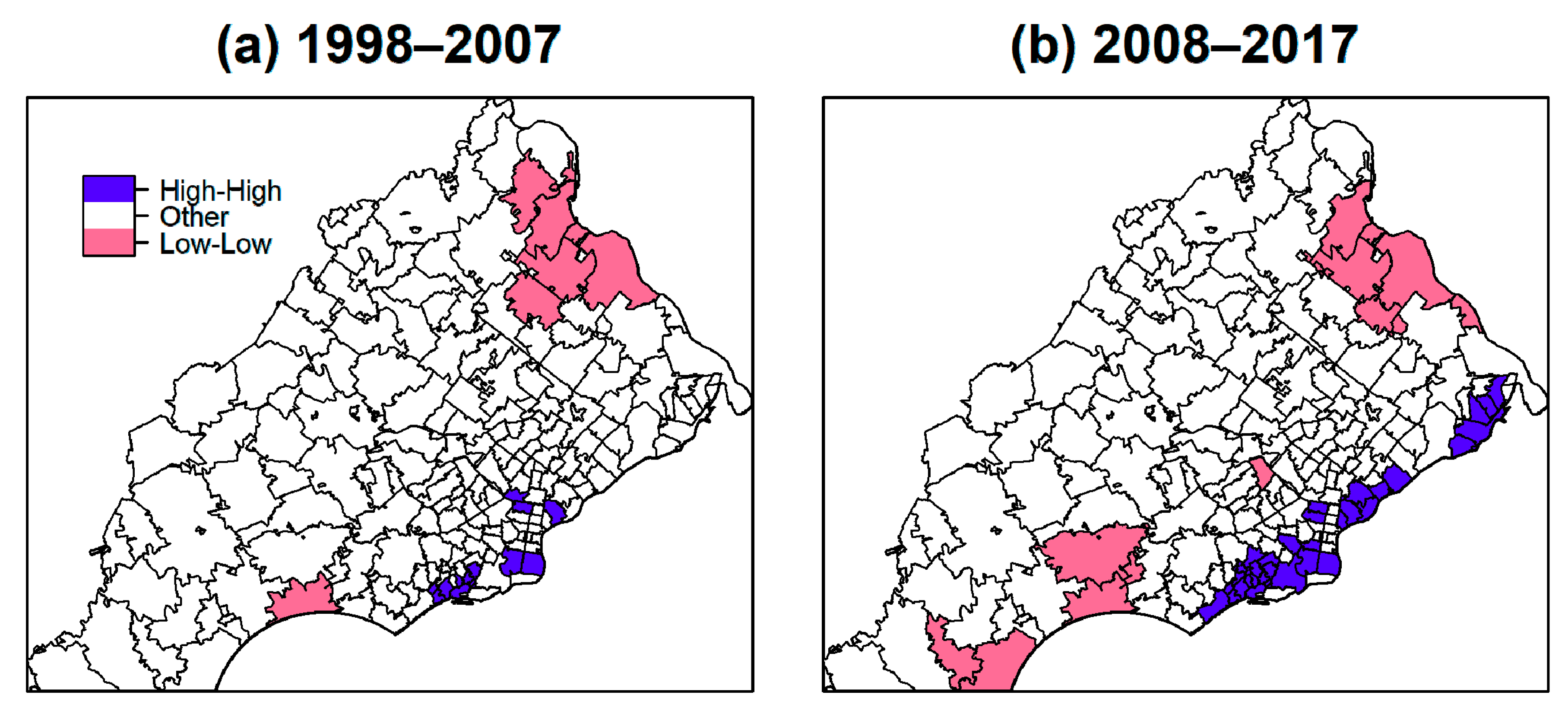
3.3. Spatial Autocorrelation
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Cancer of the Lung and Bronchus—Cancer Stat Facts. Available online: https://seer.cancer.gov/statfacts/html/lungb.html (accessed on 27 July 2020).
- American Lung Association Finds That Pennsylvania Can do More to Reduce the Toll of Lung Cancer—the #1 Cancer Killer of Women and Men|American Lung Association. Available online: https://www.lung.org/media/press-releases/state-of-lung-cancer-pa (accessed on 27 July 2020).
- State Cancer Profiles. Available online: https://statecancerprofiles.cancer.gov/quick-profiles/index.php?statename=pennsylvania (accessed on 27 July 2020).
- Simon, S. Lung Cancer Risks for Non-Smokers. Available online: https://www.cancer.org/latest-news/why-lung-cancer-strikes-nonsmokers.html (accessed on 27 July 2020).
- Lung Cancer Fact Sheet. Available online: https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/resource-library/lung-cancer-fact-sheet (accessed on 27 July 2020).
- Eckel, S.P.; Cockburn, M.; Shu, Y.-H.; Deng, H.; Lurmann, F.W.; Liu, L.; Gilliland, F.D. Air pollution affects lung cancer survival. Thorax 2016, 71, 891–898. [Google Scholar] [CrossRef]
- Benbrahim-Tallaa, L.; Baan, R.A.; Grosse, Y.; Lauby-Secretan, B.; El Ghissassi, F.; Bouvard, V.; Guha, N.; Loomis, D.; Straif, K. Carcinogenicity of diesel-engine and gasoline-engine exhausts and some nitroarenes. Lancet Oncol. 2012, 13, 663–664. [Google Scholar] [CrossRef]
- Garshick, E.; Laden, F.; Hart, J.E.; Smith, T.J.; Rosner, B. Smoking imputation and lung cancer in railroad workers exposed to diesel exhaust. Am. J. Ind. Med. 2006, 49, 709–718. [Google Scholar] [CrossRef] [PubMed]
- IARC—International Agency for Research on Cancer. Available online: https://www.iarc.fr/ (accessed on 27 July 2020).
- Lelieveld, J.; Evans, J.S.; Fnais, M.; Giannadaki, D.; Pozzer, A. The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature 2015, 525, 367–371. [Google Scholar] [CrossRef]
- Cruz, C.S.D.; Tanoue, L.T.; Matthay, R.A. Lung cancer: Epidemiology, etiology, and prevention. Clin. Chest Med. 2011, 32, 605–644. [Google Scholar] [CrossRef] [PubMed]
- Grubesic, T.H. Zip codes and spatial analysis: Problems and prospects. Socioecon. Plan. Sci. 2008, 42, 129–149. [Google Scholar] [CrossRef]
- Thomas, A.J.; Eberly, L.E.; Davey Smith, G.; Neaton, J.D. ZIP-code-based versus tract-based income measures as long-term risk-adjusted mortality predictors. Am. J. Epidemiol. 2006, 164, 586–590. [Google Scholar] [CrossRef] [PubMed]
- Geronimus, A.T.; Bound, J. Use of census-based aggregate variables to proxy for socioeconomic group: Evidence from national samples. Am. J. Epidemiol. 1998, 148, 475–486. [Google Scholar] [CrossRef] [PubMed]
- Holmes, J.R.; Tootoo, J.L.; Chosy, E.J.; Bowie, A.Y.; Starr, R.R. Examining Variation in Life Expectancy Estimates by ZIP Code Tabulation Area (ZCTA) in Hawaii’s Four Main Counties, 2008–2012. Prev. Chronic. Dis. 2018, 15, E114. [Google Scholar] [CrossRef] [PubMed]
- Cordes, J.; Castro, M.C. Spatial analysis of COVID-19 clusters and contextual factors in New York City. Spat. Spatio-Temporal Epidemiol. 2020, 34, 100355. [Google Scholar] [CrossRef] [PubMed]
- TIGER/Line® Shapefiles. 2017. Available online: https://www.census.gov/cgi-bin/geo/shapefiles/index.php?year=2017&layergroup=ZIP+Code+Tabulation+Areas (accessed on 23 November 2020).
- Certified Registries. Available online: https://www.naaccr.org/certified-registries/#CertificationHistory (accessed on 28 November 2020).
- Environmental Systems Research Institute (Esri). ArcGIS; Environmental Systems Research Institute (Esri): Redlands, CA, USA, 2018. [Google Scholar]
- Curado, M.-P.; Edwards, B.; Shin, H.R.; Storm, H.; Ferlay, J.; Heanue, M.; Boyle, P. Cancer Incidence in Five Continents, Volume IX; IARC Scientific Publications; IARC Press, International Agency for Research on Cancer: Lyons, France, 2007; Volume 9, ISBN 92-832-2160-5. [Google Scholar]
- SEER Summary Staging Manual—2000: Codes and Coding Instructions; National Cancer Institute: Bethesda, MD, USA, 2001.
- Wolf, T. Pennsylvania Cancer Registry Manual; Pennsylvania Department of Health: Harrisburg, PA, USA, 2016.
- United States Census Bureau. Available online: https://data.census.gov/cedsci/profile?g=0400000US42 (accessed on 23 November 2020).
- Demographic Data, US Census & GIS Software|GeoLytics. Available online: https://www.geolytics.com/ (accessed on 23 November 2020).
- US EPA Toxics Release Inventory (TRI) Program. Available online: https://www.epa.gov/toxics-release-inventory-tri-program/tri-basic-data-files-calendar-years-1987-2019 (accessed on 27 July 2020).
- US EPA Air Quality System (AQS). Available online: https://aqs.epa.gov/aqsweb/airdata/download_files.html (accessed on 27 July 2020).
- Bulka, C.; Nastoupil, L.J.; Koff, J.L.; Bernal-Mizrachi, L.; Ward, K.C.; Williams, J.N.; Bayakly, A.R.; Switchenko, J.M.; Waller, L.A.; Flowers, C.R. Relations Between Residential Proximity to EPA-Designated Toxic Release Sites and Diffuse Large B-Cell Lymphoma Incidence. South. Med. J. 2016, 109, 606–614. [Google Scholar] [CrossRef] [PubMed]
- Cogliano, V.J.; Baan, R.; Straif, K.; Grosse, Y.; Lauby-Secretan, B.; El Ghissassi, F.; Bouvard, V.; Benbrahim-Tallaa, L.; Guha, N.; Freeman, C.; et al. Preventable Exposures Associated With Human Cancers. JNCI J. Natl. Cancer Inst. 2011, 103, 1827–1839. [Google Scholar] [CrossRef] [PubMed]
- Consumer Expenditures in 2017: BLS Reports: U.S. Bureau of Labor Statistics. Available online: https://www.bls.gov/opub/reports/consumer-expenditures/2017/home.htm (accessed on 25 November 2020).
- Consumer Expenditures Survey Glossary. Available online: https://www.bls.gov/cex/csxgloss.htm (accessed on 2 December 2020).
- EDDIE. Available online: https://www.phaim1.health.pa.gov/EDD/WebForms/PopCntySt.aspx (accessed on 27 July 2020).
- Tiwari, R.C.; Clegg, L.X.; Zou, Z. Efficient interval estimation for age-adjusted cancer rates. Stat. Methods Med. Res. 2006, 15, 547–569. [Google Scholar] [CrossRef]
- Moran, P.A.P. A test for the serial independence of residuals. Biometrika 1950, 37, 178–181. [Google Scholar] [CrossRef] [PubMed]
- Anselin, L. Local Indicators of Spatial Association—LISA. Geogr. Anal. 1995, 27, 93–115. [Google Scholar] [CrossRef]
- Bivand, R.S.; Wong, D.W.S. Comparing implementations of global and local indicators of spatial association. TEST 2018, 27, 716–748. [Google Scholar] [CrossRef]
- Getis, A. Spatial Weights Matrices. Geogr. Anal. 2009, 41, 404–410. [Google Scholar] [CrossRef]
- Sawada, M. LPC. Available online: http://www.lpc.uottawa.ca/publications/moransi/moran.htm (accessed on 27 July 2020).
- PA Environmental Justice Areas. Available online: https://www.dep.pa.gov:443/PublicParticipation/OfficeofEnvironmentalJustice/Pages/PA-Environmental-Justice-Areas.aspx (accessed on 28 August 2020).
| Characteristics | High Incidence ZIP Codes (n = 51) | Remaining ZIP Codes (n = 161) | ||
|---|---|---|---|---|
| Data Source | Median (IQR) | Median (IQR) | p-Value * | |
| Demographic (2017 ACS) | Population size | 21,685 (25,959) | 12,473 (19,196) | 0.00045 |
| Population density (/sq mi) | 7216 (9788) | 1548 (2607) | <0.00001 | |
| Median age | 36.9 (6.2) | 42 (6.8) | <0.00001 | |
| Median income (dollar) | 52,859 (25,036) | 88,558 (32,919) | <0.00001 | |
| Percent White | 72.7 (50.1) | 87.8 (14.2) | <0.00001 | |
| Percent Hispanic | 5.2 (6.5) | 3.3 (3.3) | 0.000472 | |
| Percent below poverty | 11.6 (11.3) | 3.1 (3.4) | <0.00001 | |
| Percent with at least HS education | 88.5 (8.4) | 94.6 (5.5) | <0.00001 | |
| Employment to pop ratio | 59.0 (15.6) | 64.3 (6.3) | 0.000114 | |
| Unemployment rate | 7.8 (5.5) | 5.0 (2.4) | <0.00001 | |
| TRI and distance (1987–2017 TRI) | No. of TRI facility/year ≤ 10 miles | 148.5 (72.3) | 78.0 (84.5) | <0.00001 |
| Total air emission ≤ 10 miles (ton) | 23,898 (7162) | 9120 (13,725) | <0.00001 | |
| Benzene | 1567.501 (1289.7) | 10.197 (30.3) | <0.00001 | |
| Beryllium | 0 (0.3) | 0 (0.3) | 0.03630 | |
| Cadmium | 1.268 (4.7) | 0.145 (2.7) | <0.00001 | |
| Chloromethyl methyl ether | 0 (0.1) | 0 (0) | 0.00007 | |
| Chromium Compounds | 154.949 (123.0) | 15.129 (21.2) | <0.00001 | |
| Crocidolite (Asbestos) | 0 (0) | 0 (0) | 0.08244 | |
| Nickel Compounds | 160.575 (114.1) | 9.721 (16.3) | <0.00001 | |
| No. of TRI facility/year ≤ 15 miles | 267.5 (68.5) | 155.0 (186.5) | <0.00001 | |
| Total air emission ≤ 15 miles (ton) | 40,523 (12,550) | 20,734 (26,047) | <0.00001 | |
| Benzene | 2147.298 (775.2) | 18.101 (1363.4) | <0.00001 | |
| Beryllium | 0.26 (0) | 0.26 (0.3) | 0.02805 | |
| Cadmium | 5.560 (1.1) | 2.750 (5.0) | <0.00001 | |
| Chloromethyl methyl ether | 0.103 (0) | 0 (0.1) | <0.00001 | |
| Chromium Compounds | 173.379 (8.0) | 35.056 (149.7) | <0.00001 | |
| Crocidolite (Asbestos) | 0 (0) | 0 (0.8) | 0.01102 | |
| Nickel Compounds | 192.075 (150.5) | 22.500 (113.0) | <0.00001 | |
| Nearest TRI facility (meters) | 1161 (1248) | 2677 (3417) | <0.00001 | |
| Distance to PHL airport (meters) | 22,451 (11,876) | 23,020 (21,394) | 0.6558 | |
| Distance to I-95/major highway (meters) | 3076 (3429) | 18,811 (22,116) | <0.00001 | |
| Cigarette Use (2004–2008 CES) | Annual household expenditure for tobacco and smoking supplies (dollar) | 285.04 (26.8) | 302.42 (7.5) | <0.00001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, Y.; McKeon, T.P.; Tam, V.; Vachani, A.; Penning, T.M.; Hwang, W.-T. Geographic Differences in Lung Cancer Incidence: A Study of a Major Metropolitan Area within Southeastern Pennsylvania. Int. J. Environ. Res. Public Health 2020, 17, 9498. https://doi.org/10.3390/ijerph17249498
Zhu Y, McKeon TP, Tam V, Vachani A, Penning TM, Hwang W-T. Geographic Differences in Lung Cancer Incidence: A Study of a Major Metropolitan Area within Southeastern Pennsylvania. International Journal of Environmental Research and Public Health. 2020; 17(24):9498. https://doi.org/10.3390/ijerph17249498
Chicago/Turabian StyleZhu, Yaqian, Thomas P. McKeon, Vicky Tam, Anil Vachani, Trevor M. Penning, and Wei-Ting Hwang. 2020. "Geographic Differences in Lung Cancer Incidence: A Study of a Major Metropolitan Area within Southeastern Pennsylvania" International Journal of Environmental Research and Public Health 17, no. 24: 9498. https://doi.org/10.3390/ijerph17249498
APA StyleZhu, Y., McKeon, T. P., Tam, V., Vachani, A., Penning, T. M., & Hwang, W.-T. (2020). Geographic Differences in Lung Cancer Incidence: A Study of a Major Metropolitan Area within Southeastern Pennsylvania. International Journal of Environmental Research and Public Health, 17(24), 9498. https://doi.org/10.3390/ijerph17249498






