Relationship between Determinants of Health, Equity, and Dimensions of Health Literacy in Patients with Cardiovascular Disease
Abstract
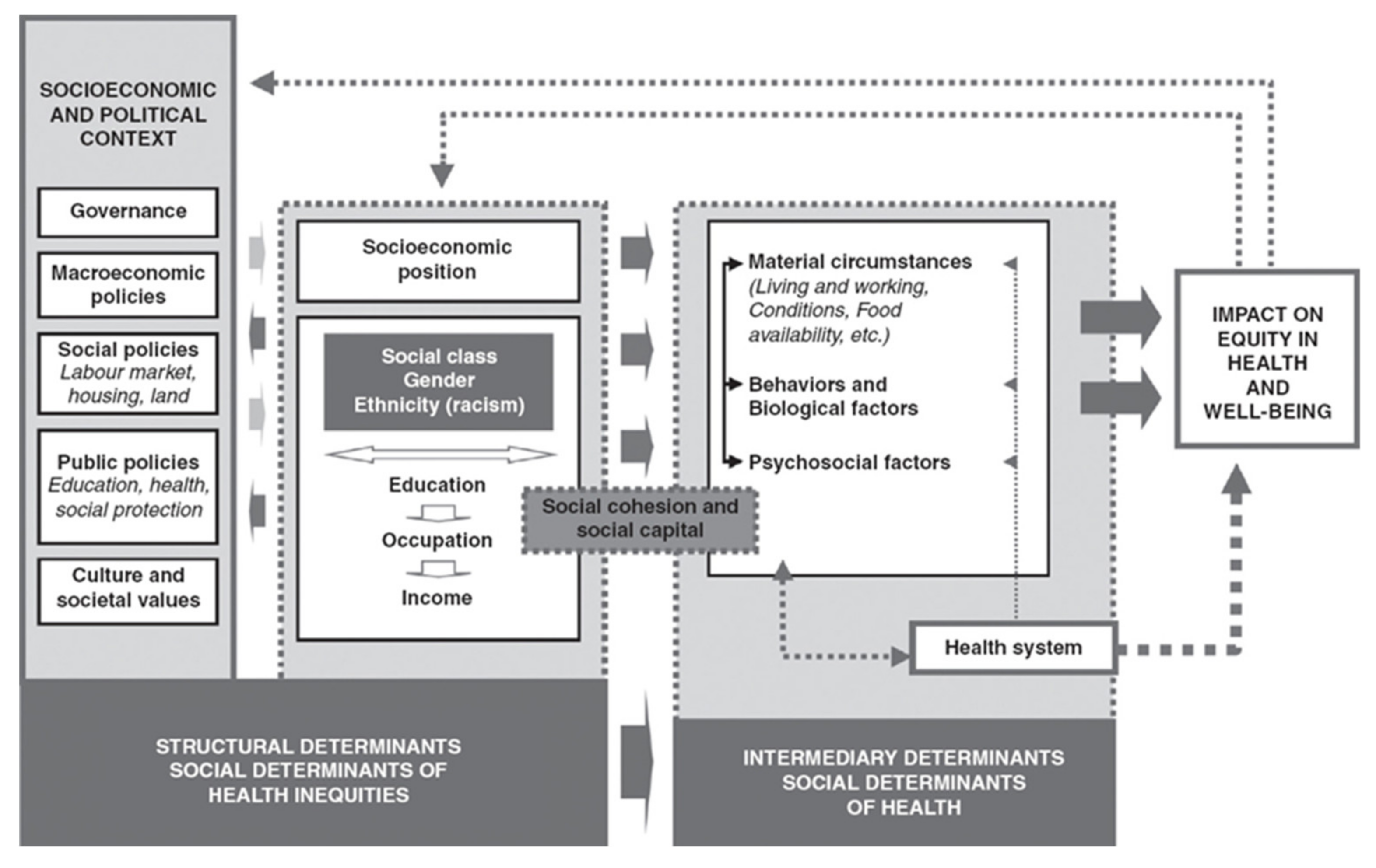
:1. Background
2. Methods
2.1. Studio Design
2.2. Population
2.3. Study Assessment Parameters
- o
- Dimension 1 (D1): Feeling understood and supported by health care providers.
- o
- Dimension 2 (D2): Having enough information to manage my health.
- o
- Dimension 3 (D3): Actively managing my health.
- o
- Dimension 4 (D4): Social health support.
- o
- Dimension 5 (D5): Assessment of health information.
- o
- Dimension 6 (D6): Ability to actively participate with health care providers.
- o
- Dimension 7 (D7): Navigation through the health system.
- o
- Dimension 8 (D8): Ability to find good health information.
- o
- Dimension 9 (D9): Understanding health information well enough to know what to do.
2.4. Statistical Analysis
2.5. Ethical Considerations
3. Results
3.1. Description of the Sample
3.2. Relationships between HL Dimensions and Variables
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Marmot, M.; Friel, S.; Bell, R.; Houweling, T.A.; Taylor, S. Closing the gap in a generation: Health equity through action on the social determinants of health. Lancet 2008, 372, 1661–1669. [Google Scholar] [CrossRef]
- Ministerio de Sanidad, Servicios Sociales e Igualdad. Avanzando hacia la equidad: Propuesta de Políticas e Intervenciones para reducir las desigualdades Sociales en salud en España; Comisión para reducir las desigualdades sociales en salud en España: Madrid, Spain, 2015; pp. 1–112.
- WHO; Solar, O.; Irwin, A. A conceptual framework for action on the social determinants of health. 2020. Available online: https://www.who.int/sdhconference/resources/ConceptualframeworkforactiononSDH_eng.pdf (accessed on 21 January 2020).
- Borrell, C.; Malmusi, D. La investigación sobre los determinantes sociales y las desigualdades en salud: Evidencias para la salud en todas las políticas. Informe SESPAS 2010. Gac Sanit 2010, 24, 101–108. [Google Scholar] [CrossRef] [Green Version]
- Kickbusch, I.; World Health Organization; Pelikan, J.M.; Apfel, F. Health Literacy. The Solid Facts; World Health Organization: Geneva, Switzerland, 2013; Available online: https://apps.who.int/iris/bitstream/handle/10665/128703/e96854.pdf (accessed on 21 January 2020).
- Rowlands, G.; Shaw, A.; Jaswal, S.; Smith, S.; Harpham, T. Health literacy and the social determinants of health: A qualitative model from adult learners. Health Promot. Int. 2017, 32, 130–138. [Google Scholar] [CrossRef] [Green Version]
- Nutbeam, D. The evolving concept of health literacy. Soc. Sci. Med. 2008, 67, 2072–2078. [Google Scholar] [CrossRef]
- Fleary, S.A.; Ettienne, R. Social Disparities in Health Literacy in the United States. Health Lit. Res. Pract. 2019, 3, e47–e52. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. Bmc Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berkman, N.D.; Davis, T.C.; McCormack, L. Health literacy: What is it? J. Health Commun. 2010, 15 Suppl. 2, 9–19. [Google Scholar] [CrossRef]
- Juvinyà-Canal, D.; Bertran-Noguer, C.; Suñer-Soler, R. Alfabetización para la salud, más que información. Gaceta Sanitaria 2018, 32, 8–10. [Google Scholar] [CrossRef] [PubMed]
- Montesi, M. Alfabetización en salud: Revisión narrativa e interdisciplinar de la literatura publicada en biomedicina y en biblioteconomía y documentación. Rev. Cuba. De Inf. En Cienc. De La Salud 2017, 28, 1–21. [Google Scholar]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low health literacy and health outcomes: An updated systematic review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef]
- Sørensen, K.; Van den Broucke, S.; Pelikan, J.M.; Fullam, J.; Doyle, G.; Slonska, Z.; Kondilis, B.; Stoffels, V.; Osborne, R.H.; Brand, H. Measuring health literacy in populations: Illuminating the design and development process of the European Health Literacy Survey Questionnaire (HLS-EU-Q). Bmc Public Health 2013, 13, 948. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- January, C.T.; Wann, L.S.; Alpert, J.S.; Calkins, H.; Cigarroa, J.E.; Cleveland, J.C.; Conti, J.B.; Ellinor, P.T.; Ezekowitz, M.D.; Field, M.E.; et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J. Am. Coll. Cardiol. 2014, 64, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. J. Heart Fail. 2016, 18, 891–975. [Google Scholar] [PubMed]
- Kirchhof, P.; Benussi, S.; Kotecha, D.; Ahlsson, A.; Atar, D.; Casadei, B.; Castella, M.; Diener, H.; Heidbuchel, H.; Hendriks, J.; et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur. Heart J. 2016, 37, 2893–2962. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Osborne, R.H.; Batterham, R.W.; Elsworth, G.R.; Hawkins, M.; Buchbinder, R. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). Bmc Public Health 2013, 13, 658. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beauchamp, A.; Buchbinder, R.; Dodson, S.; Batterham, R.W.; Elsworth, G.R.; McPhee, C.; Sparkes, L.; Hawkins, M.; Osborne, R.H. Distribution of health literacy strengths and weaknesses across socio-demographic groups: A cross-sectional survey using the Health Literacy Questionnaire (HLQ). Bmc Public Health 2015, 15, 678–691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jessup, R.L.; Osborne, R.H.; Beauchamp, A.; Bourne, A.; Buchbinder, R. Health literacy of recently hospitalised patients: A cross-sectional survey using the Health Literacy Questionnaire (HLQ). Bmc Health Serv. Res. 2017, 17, 52–64. [Google Scholar] [CrossRef] [Green Version]
- Seaton, C.L.; Oliffe, J.L.; Rice, S.M.; Bottorff, J.L.; Johnson, S.T.; Gordon, S.J.; Chambers, S.K. Health Literacy Among Canadian Men Experiencing Prostate Cancer. Health Promot. Pract. 2019, 1–8. [Google Scholar] [CrossRef]
- Bennett, I.M.; Chen, J.; Soroui, J.S.; White, S. The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults. Ann. Fam. Med. 2009, 7, 204–211. [Google Scholar] [CrossRef] [Green Version]
- Paasche-Orlow, M.K.; Wolf, M.S. Promoting health literacy research to reduce health disparities. J. Health Commun. 2010, 15 Suppl. 2, 34–41. [Google Scholar] [CrossRef]
- Davis, S.N.; Wischhusen, J.W.; Sutton, S.K.; Christy, S.M.; Chavarria, E.A.; Sutter, M.E.; Roy, S.; Meade, C.D.; Gwede, C.K. Demographic and psychosocial factors associated with limited health literacy in a community-based sample of older Black Americans. Patient Educ. Couns. 2019. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M. Social determinants of health inequalities. Lancet 2005, 365, 1099–1104. [Google Scholar] [CrossRef] [Green Version]
- Case, A.; Deaton, A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc. Natl. Acad. Sci. USA 2015, 112, 15078–15083. [Google Scholar] [CrossRef] [Green Version]
- Bots, S.H.; Peters, S.A.E.; Woodward, M. Sex differences in coronary heart disease and stroke mortality: A global assessment of the effect of ageing between 1980 and 2010. BMJ Glob. Health 2017, 2, e000298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mosca, L.; Barrett-Connor, E.; Wenger, N.K. Sex/gender differences in cardiovascular disease prevention: What a difference a decade makes. Circulation 2011, 124, 2145–2154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vogel, B.; Farhan, S.; Hahne, S.; Kozanli, I.; Kalla, K.; Freynhofer, M.K.; Jarai, R.; Kautzky-Willer, A.; Huber, K. Sex-related differences in baseline characteristics, management and outcome in patients with acute coronary syndrome without ST-segment elevation. Eur. Heart J. Acute Cardiovasc. Care 2016, 5, 347–353. [Google Scholar] [CrossRef]
- O’Neil, A.; Scovelle, A.J.; Milner, A.J.; Kavanagh, A. Gender/Sex as a Social Determinant of Cardiovascular Risk. Circulation 2018, 137, 854–864. [Google Scholar] [CrossRef]
- Fabbri, M.; Yost, K.; Finney Rutten, L.J.; Manemann, S.M.; Boyd, C.M.; Jensen, D.; Weston, S.A.; Jiang, R.; Roger, V.L. Health Literacy and Outcomes in Patients With Heart Failure: A Prospective Community Study. Mayo Clin. Proc. 2018, 93, 9–15. [Google Scholar] [CrossRef]
- Santesmases-Masana, R.; González-de Paz, L.; Real, J.; Borràs-Santos, A.; Sisó-Almirall, A.; Navarro-Rubio, M.D. Alfabetización en salud en pacientes con insuficiencia cardiaca atendidos en atención primaria. Atención Primaria 2017, 49, 28–34. [Google Scholar] [CrossRef] [Green Version]
- Alonso, R.P.; Alvarez, P.M.; Garcia, S.M.; Perez, A.L.; Cano, S.S.; Sanchez, J.L.C. Analisis del nivel de alfabetizacion en salud, en pacientes con insuficiencia renal cronica en hemodialisis/Analysis of the level of health literacy in patients with chronic renal failure on hemodialysis. Revista de la Sociedad Espanola de Enfermeria Nefrologica 2017, 20, 221. [Google Scholar] [CrossRef]
- Rueda Estrada, J.D. La soledad de las personas mayores en España: Una realidad invisible. Actas de coordinación socio-sanitarias 2018, 28, 45–64. [Google Scholar]
- Del Monte Diego, J. Cohousing. Modelo residencial colaborativo y capacitante para un envejecimiento feliz. Fundación Pilares: Madrid, Spain, 2017; ISBN 987-84-617-7793-8. [Google Scholar]
- Monreal Bosch, P.; del Valle Gómez, A. Los Grandes Olvidados: Las Personas Mayores en el Entorno Rural. Psychosoc. Interv. 2009, 18, 269–277. [Google Scholar] [CrossRef]
- Sanchez Oro Sanchez, M.; Pérez Rubio, J.A.; Moreno Ramos, J. Los mayores en el continuo rural-urbano. Aproximación a la percepción subjetiva y expectativas vitales (el caso de Extremadura). Papers. Revista de Sociologia 2012, 98, 143. [Google Scholar] [CrossRef]
- CONSEJO ECONÓMICO Y SOCIAL ESPAÑA El medio rural y su vertebración social y territorial. 2018, pp. 1–172. Available online: http://www.datosdelanzarote.com/Uploads/doc/Informe-sobre-el-Medio-Rural-y-su-vertebraci%C3%B3n-social-y-territorial-(2018)-20180621131520465Medio-Rural.pdf (accessed on 21 January 2020).
- Heng-Hsin, T.; Tse-Min, L.; Liang-Kung, C.; Shu-Yuan, L.; Shu-Fang, W.; Kuei-Hui, C. Health literacy impact on elderly patients with heart failure in Taiwan. Journal of Clinical Gerontology & Geriatrics 2014, 5, 72-76. J. Cin. Gerontol. Geriatr. 2014, 5, 72–76. [Google Scholar]
- Liu, X.B.; Ayatollahi, Y.; Yamashita, T.; Jaradat, M.; Shen, J.J.; Kim, S.J.; Lee, Y.; Hwang, J.; Yeom, H.; Upadhyay, S.; et al. Health Literacy and Mortality in Patients With Heart Failure: A Systematic Review and Meta-Analysis. Res. Gerontol. Nurs. 2019, 12, 99–108. [Google Scholar] [CrossRef]
- Oscalices, M.I.L.; Okuno, M.F.P.; Lopes, M.C.B.T.; Batista, R.E.A.; Campanharo, C.R.V. Health literacy and adherence to treatment of patients with heart failure. Rev. Esc. Enferm. USP 2019, 53, e03447. [Google Scholar] [CrossRef] [Green Version]
- Peterson, P.N.; Shetterly, S.M.; Clarke, C.L.; Bekelman, D.B.; Chan, P.S.; Allen, L.A.; Matlock, D.D.; Magid, D.J.; Masoudi, F.A. Health literacy and outcomes among patients with heart failure. JAMA 2011, 305, 1695–1701. [Google Scholar] [CrossRef] [Green Version]
- McNaughton, C.D.; Cawthon, C.; Kripalani, S.; Liu, D.; Storrow, A.B.; Roumie, C.L. Health literacy and mortality: A cohort study of patients hospitalized for acute heart failure. J. Am. Heart Assoc. 2015, 4. [Google Scholar] [CrossRef] [Green Version]
- Cabellos-García, A.C.; Martínez-Sabater, A.; Castro-Sánchez, E.; Kangasniemi, M.; Juárez-Vela, R.; Gea-Caballero, V. Relation between health literacy, self-care and adherence to treatment with oral anticoagulants in adults: A narrative systematic review. Bmc Public Health 2018, 18, 1–12. [Google Scholar] [CrossRef] [Green Version]
| M/n | Sd/% | ||
|---|---|---|---|
| Age | 74.38 | 7.35 | |
| < 65 years | 26 | 10.3% | |
| = > 65 years | 226 | 89.7% | |
| Gender | Woman | 107 | 42.5% |
| Man | 145 | 57.5% | |
| Education Level | Without Studies | 101 | 40.1% |
| Basic Education | 126 | 50.0% | |
| Higher Education | 25 | 9.9% | |
| Social Class | Low | 33 | 13.1% |
| Middle | 206 | 81.7% | |
| High | 13 | 5.2% | |
| Main Diagnosis | Atrial Fibrillation | 188 | 74.9% |
| Atrial Flutter | 7 | 2.8% | |
| Aortic Prosthesis | 33 | 13.1% | |
| Mitral Prosthesis | 23 | 9.2% | |
| Polypharmacy | No | 86 | 34.1% |
| Yes | 166 | 65.9% | |
| Dimension | Mean | Standard Error of the Mean | Standard Deviation | Median | Maximum | Minimum | 25 Percentile | 75 Percentile |
|---|---|---|---|---|---|---|---|---|
| Dimension 1 | 3.201 | 0.027 | 0.429 | 3.125 | 4.000 | 1.500 | 3.000 | 3.500 |
| Dimension 2 | 2.657 | 0.033 | 0.517 | 2.750 | 4.000 | 1.000 | 2.250 | 3.000 |
| Dimension 3 | 2.817 | 0.032 | 0.511 | 2.800 | 4.000 | 1.000 | 2.600 | 3.000 |
| Dimension 4 | 3.494 | 0.028 | 0.437 | 3.600 | 4.000 | 1.400 | 3.200 | 3.800 |
| Dimension 5 | 2.387 | 0.043 | 0.686 | 2.400 | 4.000 | 1.000 | 2.000 | 2.800 |
| Dimension 6 | 4.106 | 0.038 | 0.596 | 4.200 | 5.000 | 1.200 | 3.800 | 4.600 |
| Dimension 7 | 3.507 | 0.041 | 0.654 | 3.667 | 5.000 | 1.167 | 3.083 | 4.000 |
| Dimension 8 | 3.052 | 0.054 | 0.851 | 3.200 | 5.000 | 1.000 | 2.400 | 3.800 |
| Dimension 9 | 3.268 | 0.055 | 0.871 | 3.400 | 5.000 | 1.400 | 2.600 | 4.000 |
| D1 | D2 | D3 | D4 | D5 | D6 | D7 | D8 | D9 | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Social Class C | Sig. | 0.019 * | <0.001 ** | < 0.001 ** | 0.003 * | < 0.001 ** | <0.001 ** | <0.001 ** | <0.001 ** | <0.001 ** |
| Low | Mean (SD) | 2.98 (0.44) | 2.3 (0.39) | 2.41 (0.53) | 3.38 (0.39) | 1.81 (0.55) | 3.76 (0.56) | 3.04 (0.58) | 2.25 (0.64) | 2.43 (0.61) |
| Median (IQR) | 3.00 (0.50) | 2.25 (0.50) | 2.4 (0.80) | 3.40 (0.40) | 1.80 (0.80) | 3.80 (0.80) | 3.00 (0.67) | 2.20 (0.40) | 2.20 (0.80) | |
| Middle | Mean (SD) | 3.23 (0.4 | 2.71 (0.51) | 2.87 (0.49) | 3.5 (0.45) | 2.45 (0.66) | 4.15 (0.59) | 3.56 (0.65) | 3.14 (0.82) | 3.35 (0.83) |
| Median (IQR) | 3.25 (0.50) | 2.75 (0.75) | 3.00 (0.60) | 3.60 (0.60) | 2.60 (0.80) | 4.20 (0.80) | 3.67 (0.83) | 3.20 (1.20) | 3.40 (1.40) | |
| High | Mean (SD) | 3.27 (0.33) | 2.77 (0.5) | 3 (0.34) | 3.72 (0.29) | 2.88 (0.67) | 4.34 (0.51) | 3.91 (0.31) | 3.66 (0.64) | 4.10 (0.56) |
| Median (IQR) | 3.25 (0.50) | 2.75 (0.25) | 3.00 (0.20) | 3.80 (0.0) | 3.00 (0.40) | 4.20 (0.60) | 4.00 (0.17) | 4.00 (0.80) | 4.20 (0.20) | |
| Gender A | Sig. | 0.496 | 0.055 | 0.298 | 0.137 | 0.096 | 0.217 | 0.142 | 0.028 * | 0.015 * |
| Woman | Mean (SD) | 3.18 (0.46) | 2.58 (0.54) | 2.78 (0.53) | 3.44 (0.5) | 2.3 (0.7) | 4.05 (0.64) | 3.44 (0.66) | 2.92 (0.84) | 3.11 (0.85) |
| Median (IQR) | 3.00 (0.50) | 2.50 (0.75) | 2.80 (0.40) | 3.60 (0.60) | 2.40 (1.00) | 4.00 (1.00) | 3.50 (1.00) | 3.00 (1.40) | 3.20 (1.40) | |
| Man | Mean (SD) | 3.22 (0.4) | 2.71 (0.5) | 2.85 (0.5) | 3.53 (0.38) | 2.45 (0.67) | 4.15 (0.56) | 3.56 (0.65) | 3.15 (0.85) | 3.38 (0.87) |
| Median (IQR) | 3.25 (0.50) | 2.75 (0.75) | 2.80 (0.60) | 3.60 (0.40) | 2.40 (0.80) | 4.20 (0.80) | 3.67 (0.83) | 3.20 (1.20) | 3.40 (1.40) | |
| Age D | Sig. | 0.022 | −0.105 | −0.104 | −0.030 | −0.223 ** | −0.118 | −0.189 * | −0.282 ** | −0.261 ** |
| <65 years | Mean (SD) | 3.18 (0.4) | 2.73 (0.47) | 2.86 (0.58) | 3.48 (0.33) | 2.59 (0.78) | 4.35 (0.49) | 3.74 (0.58) | 3.42 (0.76) | 3.59 (0.85) |
| Median (IQR) | 3.13 (0.50) | 2.75 (0.50) | 3.00 (0.80) | 3.40 (0.60) | 2.60 (1.20) | 4.40 (1.00) | 3.83 (0.67) | 3.50 (1.20) | 3.80 (1.60) | |
| =>65 years | Mean (SD) | 3.2 (0.43) | 2.65 (0.52) | 2.81 (0.5) | 3.5 (0.45) | 2.36 (0.67) | 4.08 (0.6) | 3.48 (0.66) | 3.01 (0.85) | 3.23 (0.87) |
| Median (IQR) | 3.13 (0.50) | 2.75 (0.75) | 2.80 (0.40) | 3.60 (0.60) | 2.40 (0.80) | 4.20 (0.60) | 3.50 (1.00) | 3.00 (1.20) | 3.40 (1.60) | |
| Education Level B, C | Sig. | <0.001 ** | <0.001 ** | <0.001 ** | 0.016 * | <0.001 ** | <0.001 ** | <0.001 ** | <0.001 ** | <0.001 ** |
| Without Studies | Mean (SD) | 3.06 (0.4) | 2.33 (0.43) | 2.51 (0.45) | 3.42 (0.41) | 1.94 (0.54) | 3.85 (0.60) | 3.08 (0.54) | 2.38 (0.57) | 2.56 (0.58) |
| Median (IQR) | 3.00 (0.25) | 2.25 (0.5) | 2.60 (0.60) | 3.60 (0.60) | 2.00 (0.80) | 4.00 (0.60) | 3.17 (0.83) | 2.40 (0.80) | 2.40 (0.80) | |
| Basic Education | Mean (SD) | 3.28 (0.44) | 2.83 (0.47) | 2.96 (0.42) | 3.52 (0.47) | 2.58 (0.56) | 4.23 (0.53) | 3.72 (0.57) | 3.39 (0.66) | 3.62 (0.67) |
| Median (IQR) | 3.25 (0.50) | 3.00 (0.5) | 3.00 (0.40) | 3.80 (0.40) | 2.60 (0.60) | 4.20 (0.60) | 3.83 (0.50) | 3.60 (1.00) | 3.80 (0.60) | |
| Higher Education | Mean (SD) | 3.4 (0.36) | 3.11 (0.32) | 3.36 (0.39) | 3.67 (0.26) | 3.26 (0.56) | 4.54 (0.49) | 4.16 (0.42) | 4.06 (0.63) | 4.35 (0.49) |
| Median (IQR) | 3.25 (0.50) | 3.00 (0.25) | 3.20 (0.80) | 3.80 (0.20) | 3.20 (1.00) | 4.60 (0.60) | 4.00 (0.33) | 4.00 (0.80) | 4.40 (0.60) | |
| Obesity A | Sig. | 0.895 | 0.288 | 0.113 | 0.525 | 0.030 * | 0.318 | 0.142 | 0.030 * | 0.018 * |
| No | Mean (SD) | 3.2 (0.43) | 2.69 (0.52) | 2.86 (0.51) | 3.48 (0.45) | 2.46 (0.7) | 4.14 (0.55) | 3.56 (0.65) | 3.15 (0.84) | 3.38 (0.86) |
| Median (IQR) | 3.13 (0.50) | 2.75 (0.75) | 2.80 (0.60) | 3.60 (0.60) | 2.60 (1.00) | 4.20 (0.80) | 3.67 (0.83) | 3.20 (1.30) | 3.40 (1.30) | |
| Yes | Mean (SD) | 3.2 (0.42) | 2.62 (0.52) | 2.76 (0.51) | 3.52 (0.41) | 2.28 (0.65) | 4.06 (0.66) | 3.43 (0.66) | 2.91 (0.86) | 3.11 (0.86) |
| Median (IQR) | 3.13 (0.50) | 2.50 (0.75) | 2.80 (0.50) | 3.60 (0.50) | 2.40 (1.00) | 4.20 (0.60) | 3.50 (0.83) | 3.00 (1.50) | 3.20 (1.50) | |
| Polypharmacy A | Sig. | 0.255 | <0.001 ** | 0.005 * | 0.780 | <0.001 ** | 0.367 | 0.004 * | <0.001 ** | <0.001 ** |
| No | Mean (SD) | 3.24 (0.4) | 2.82 (0.46) | 2.94 (0.58) | 3.48 (0.4) | 2.62 (0.68) | 4.15 (0.63) | 3.67 (0.64) | 3.4 (0.83) | 3.58 (0.84) |
| Median (IQR) | 3.25 (0.50) | 3.00 (0.50) | 3.00 (0.40) | 3.60 (0.60) | 2.60 (0.60) | 4.20 (0.80) | 3.83 (0.50) | 3.60 (1.20) | 3.80 (1.00) | |
| Yes | Mean (SD) | 3.18 (0.44) | 2.57 (0.53) | 2.75 (0.46) | 3.5 (0.46) | 2.26 (0.66) | 4.08 (0.58) | 3.42 (0.65) | 2.87 (0.81) | 3.10 (0.84) |
| Median (IQR) | 3.00 (0.50) | 2.50 (0.75) | 2.80 (0.40) | 3.60 (0.60) | 2.40 (1.00) | 4.10 (0.60) | 3.33 (0.83) | 2.80 (1.40) | 3.10 (1.40) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cabellos-García, A.C.; Castro-Sánchez, E.; Martínez-Sabater, A.; Díaz-Herrera, M.Á.; Ocaña-Ortiz, A.; Juárez-Vela, R.; Gea-Caballero, V. Relationship between Determinants of Health, Equity, and Dimensions of Health Literacy in Patients with Cardiovascular Disease. Int. J. Environ. Res. Public Health 2020, 17, 2082. https://doi.org/10.3390/ijerph17062082
Cabellos-García AC, Castro-Sánchez E, Martínez-Sabater A, Díaz-Herrera MÁ, Ocaña-Ortiz A, Juárez-Vela R, Gea-Caballero V. Relationship between Determinants of Health, Equity, and Dimensions of Health Literacy in Patients with Cardiovascular Disease. International Journal of Environmental Research and Public Health. 2020; 17(6):2082. https://doi.org/10.3390/ijerph17062082
Chicago/Turabian StyleCabellos-García, Ana Cristina, Enrique Castro-Sánchez, Antonio Martínez-Sabater, Miguel Ángel Díaz-Herrera, Ana Ocaña-Ortiz, Raúl Juárez-Vela, and Vicente Gea-Caballero. 2020. "Relationship between Determinants of Health, Equity, and Dimensions of Health Literacy in Patients with Cardiovascular Disease" International Journal of Environmental Research and Public Health 17, no. 6: 2082. https://doi.org/10.3390/ijerph17062082
APA StyleCabellos-García, A. C., Castro-Sánchez, E., Martínez-Sabater, A., Díaz-Herrera, M. Á., Ocaña-Ortiz, A., Juárez-Vela, R., & Gea-Caballero, V. (2020). Relationship between Determinants of Health, Equity, and Dimensions of Health Literacy in Patients with Cardiovascular Disease. International Journal of Environmental Research and Public Health, 17(6), 2082. https://doi.org/10.3390/ijerph17062082







