COVID-19 Surface Persistence: A Recent Data Summary and Its Importance for Medical and Dental Settings
Abstract
1. Introduction
1.1. Rationale
1.2. Objectives
- What is the persistence of SARS-CoV-2 on surfaces?
- What is the mean persistence of coronaviruses compared to SARS-CoV-2?
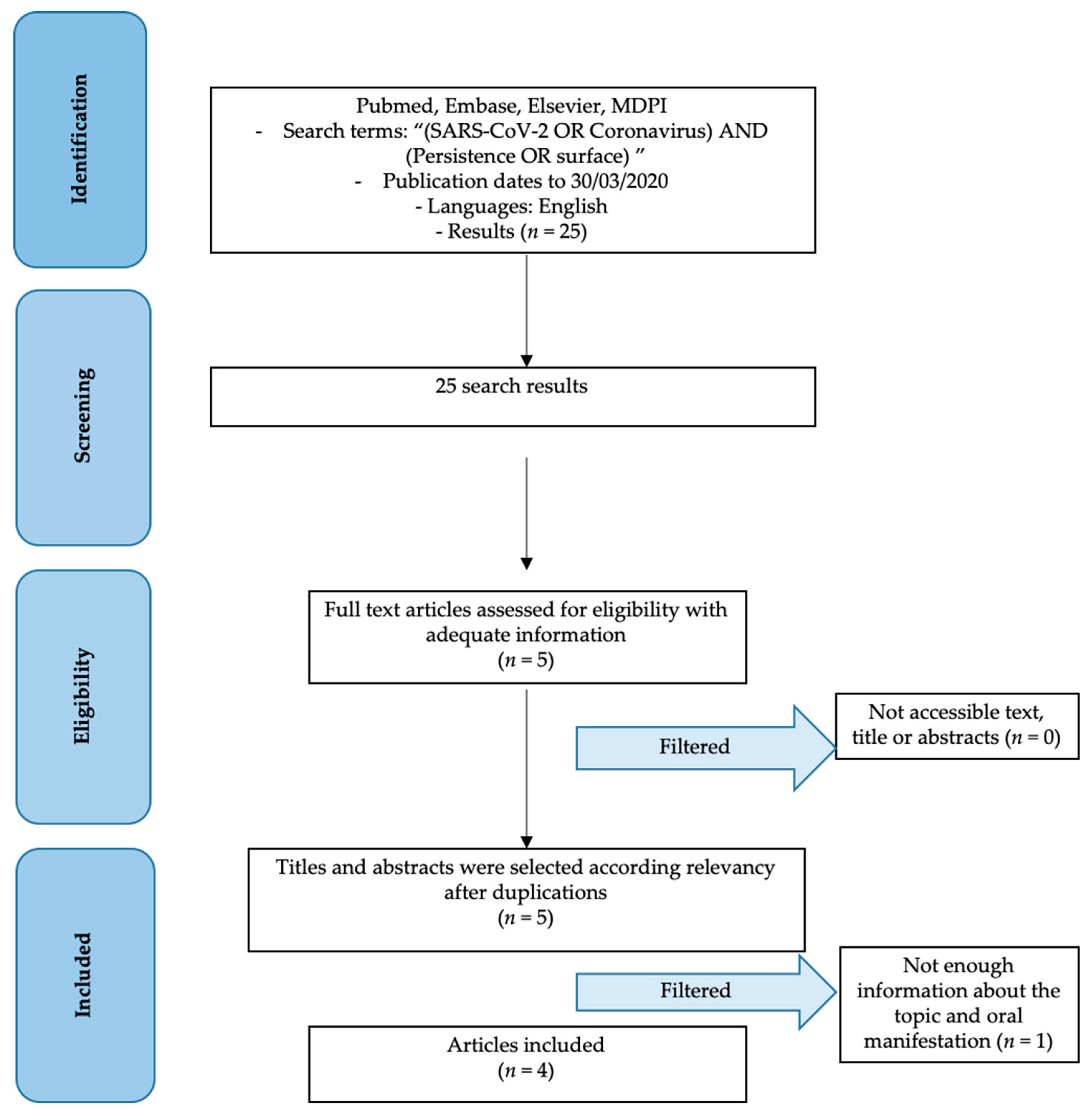
2. Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
- SARS-CoV-2 features articles;
- SARS-CoV-2 persistence;
- The persistence of other coronaviruses.
- Not enough information regarding the topic;
- Articles published prior to 1 January 2010;
- No access to the title and abstract.
2.3. Information Sources
2.4. Search
2.5. Study Selection
2.6. Data Collection Process
2.7. Data Items
- Virus: type of investigated virus;
- Authors and Year: authors, reference (according to journal guidelines) and year of publication;
- Investigated Material: investigated material surfaced by the study;
- Time: persistence time of virus;
- Note on Results: additional notes on results.
2.8. Risk of Bias
- Selection bias;
- Performance bias and detection bias;
- Attrition bias;
- Reporting bias;
- Examiner blinding, examiner calibration, standardized follow-up description, standardized residual graft measurement, standardized radiographic assessment.
2.9. Synthesis of Results
3. Results
3.1. Study Selection
3.2. Results of Individual Studies
| Virus | Authors and Year | Investigated Material | Time | Note on results |
|---|---|---|---|---|
| 2019-nCoV | Van Doremalen et al. 2020 [26] | aerosols | 3 h | Reduction from 103.5 to 102.7 TCID50 per liter of air |
| plastic | 72 h | Reduction from 103.7 to 100.6 TCID50 per millimeter | ||
| stainless steel | 48 h | from 103.7 to 100.6 TCID50 per millimeter | ||
| copper | 4 h | No viable SARS-CoV-2 | ||
| cardboard | 24 h | No viable SARS-CoV-2 | ||
| Other coronaviruses | Van Doremalen et al. 2020 [26] | aerosols | 3 h | reduction from 104.3 to 103.5 TCID50 per liter of air |
| plastic | 72 h | from 103.4 to 100.7 TCID50 per millimeter | ||
| stainless steel | 48 h | from 103.6 to 100.6 TCID50 per millimeter | ||
| copper | 8 h | No viable SARS-CoV-1 | ||
| cardboard | 8 h | No viable SARS-CoV-1 | ||
| Kampf et al. 2020 [27] | paper | 5 min up to 5 days | 105 TCID50 per millimeter | |
| glass | 4–5 d | 104 TCID50 per millimeter | ||
| plastic | 2–9 d | 106 TCID50 per millimeter | ||
| PVC | 5 d | 103 TCID50 per millimeter | ||
| silicon rubber | 5 d | 103 TCID50 per millimeter | ||
| surgical gloves (latex) | 5 d | 103 TCID50 per millimeter | ||
| disposable gowns | 1–2 d | 105 TCID50 per millimeter | ||
| Warnes et al. 2015 [28] | polyfluorotetraethylene (PTFE) | 5 d | 103 TCID50 per millimeter | |
| ceramic | 5 d | 103 TCID50 per millimeter | ||
| glass | 5 d | 103 TCID50 per millimeter | ||
| stainless steel | 5 d | 103 TCID50 per millimeter | ||
| polyvinyl chloride (PVC) | 5 d | 103 TCID50 per millimeter | ||
| silicon rubber | 3 d | 103 TCID50 per millimeter | ||
| brasses containing copper | <40 min | 103 TCID50 per millimeter | ||
| copper nickels | 120 min | 103 TCID50 per millimeter | ||
| zinc | 60 min |
3.3. Synthesis of Results
3.4. Risk of Bias
4. Discussion
4.1. Summary of Evidence
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Zhang, Y.; Xu, J.; Li, H.; Cao, B. A novel coronavirus (COVID-19) outbreak: A call for action. Chest 2020. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Wang, Y.; Yang, L.; Wang, C. Suspending Classes Without Stopping Learning: China’s Education Emergency Management Policy in the COVID-19 Outbreak. J. Risk Financ. Manag. 2020, 13, 55. [Google Scholar] [CrossRef]
- Yu, H.; Sun, X.; Solvang, W.D.; Zhao, X. Reverse Logistics Network Design for Effective Management of Medical Waste in Epidemic Outbreaks: Insights from the Coronavirus Disease 2019 (COVID-19) Outbreak in Wuhan (China). Int. J. Environ. Res. Public Health 2020, 17, 1770. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Shang, W.; Rao, X. Facing the COVID-19 outbreak: What should we know and what could we do? J. Med. Virol. 2020. [Google Scholar] [CrossRef]
- Xu, B.; Kraemer, M.U.G. Open access epidemiological data from the COVID-19 outbreak. Lancet Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 2020. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef]
- Wang, C.; Cheng, Z.; Yue, X.-G.; McAleer, M. Risk Management of COVID-19 by Universities in China. J. Risk Financ. Manag. 2020, 13, 36. [Google Scholar] [CrossRef]
- The, L. COVID-19: Fighting panic with information. Lancet 2020, 395, 537. [Google Scholar] [CrossRef]
- Tetro, J.A. Is COVID-19 Receiving ADE From Other Coronaviruses? Microbes Infect. 2020. [Google Scholar] [CrossRef]
- Nishiura, H. Backcalculating the Incidence of Infection with COVID-19 on the Diamond Princess. J. Clin. Med. 2020, 9, 657. [Google Scholar] [CrossRef]
- Nguyen, T.; Duong Bang, D.; Wolff, A. 2019 Novel Coronavirus Disease (COVID-19): Paving the Road for Rapid Detection and Point-of-Care Diagnostics. Micromachines 2020, 11, 306. [Google Scholar] [CrossRef] [PubMed]
- McAleer, M. Prevention Is Better Than the Cure: Risk Management of COVID-19. J. Risk Financ. Manag. 2020, 13, 46. [Google Scholar] [CrossRef]
- Liu, Z.; Magal, P.; Seydi, O.; Webb, G. Understanding Unreported Cases in the COVID-19 Epidemic Outbreak in Wuhan, China, and the Importance of Major Public Health Interventions. Biology 2020, 9, 50. [Google Scholar] [CrossRef] [PubMed]
- Roosa, K.; Lee, Y.; Luo, R.; Kirpich, A.; Rothenberg, R.; Hyman, J.M.; Yan, P.; Chowell, G. Short-term Forecasts of the COVID-19 Epidemic in Guangdong and Zhejiang, China: February 13–23, 2020. J. Clin. Med. 2020, 9, 596. [Google Scholar] [CrossRef] [PubMed]
- Repici, A.; Maselli, R.; Colombo, M.; Gabbiadini, R.; Spadaccini, M.; Anderloni, A.; Carrara, S.; Fugazza, A.; Di Leo, M.; Galtieri, P.A.; et al. Coronavirus (COVID-19) outbreak: What the department of endoscopy should know. Gastrointest Endosc. 2020. [Google Scholar] [CrossRef] [PubMed]
- Qin, C.; Liu, F.; Yen, T.C.; Lan, X. (18)F-FDG PET/CT findings of COVID-19: A series of four highly suspected cases. Eur J. Nucl. Med. Mol. Imaging 2020. [Google Scholar] [CrossRef] [PubMed]
- Porcheddu, R.; Serra, C.; Kelvin, D.; Kelvin, N.; Rubino, S. Similarity in Case Fatality Rates (CFR) of COVID-19/SARS-COV-2 in Italy and China. J. Infect. Dev. Ctries 2020, 14, 125–128. [Google Scholar] [CrossRef]
- Peeri, N.C.; Shrestha, N.; Rahman, M.S.; Zaki, R.; Tan, Z.; Bibi, S.; Baghbanzadeh, M.; Aghamohammadi, N.; Zhang, W.; Haque, U. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: What lessons have we learned? Int. J. Epidemiol 2020. [Google Scholar] [CrossRef]
- Tian, J.H.; Ge, L.; Li, L. The PRISMA Extension Statement. Ann. Intern. Med. 2015, 163, 566. [Google Scholar] [CrossRef]
- Liu, H.; Zhou, X.; Yu, G.; Sun, X. The effects of the PRISMA statement to improve the conduct and reporting of systematic reviews and meta-analyses of nursing interventions for patients with heart failure. Int. J. Nurs. Pract. 2019. [Google Scholar] [CrossRef] [PubMed]
- Hutton, B.; Salanti, G.; Caldwell, D.M.; Chaimani, A.; Schmid, C.H.; Cameron, C.; Ioannidis, J.P.; Straus, S.; Thorlund, K.; Jansen, J.P.; et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Ann. Intern. Med. 2015, 162, 777–784. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Altman, D.G.; Gotzsche, P.C.; Juni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. Br. Med. J. 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Savovic, J.; Turner, R.M.; Mawdsley, D.; Jones, H.E.; Beynon, R.; Higgins, J.P.T.; Sterne, J.A.C. Association Between Risk-of-Bias Assessments and Results of Randomized Trials in Cochrane Reviews: The ROBES Meta-Epidemiologic Study. Am. J. Epidemiol. 2018, 187, 1113–1122. [Google Scholar] [CrossRef] [PubMed]
- Whiting, P.; Savovic, J.; Higgins, J.P.T.; Caldwell, D.M.; Reeves, B.C.; Shea, B.; Davies, P.; Kleijnen, J.; Churchill, R.; Group, R. ROBIS: A new tool to assess risk of bias in systematic reviews was developed. Recenti. Prog. Med. 2018, 109, 421–431. [Google Scholar] [CrossRef] [PubMed]
- Van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I.; et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 2020. [Google Scholar] [CrossRef]
- Kampf, G.; Todt, D.; Pfaender, S.; Steinmann, E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hosp. Infect. 2020, 104, 246–251. [Google Scholar] [CrossRef]
- Warnes, S.L.; Little, Z.R.; Keevil, C.W. Human Coronavirus 229E Remains Infectious on Common Touch Surface Materials. mBio 2015, 6, e01697. [Google Scholar] [CrossRef]
- Yang, Z.R.; Sun, F.; Zhan, S.Y. Risk of bias assessment: (1) overview. Zhonghua Liu Xing Bing Xue Za Zhi 2017, 38, 983–987. [Google Scholar] [CrossRef]
- Dexter, F.; Parra, M.C.; Brown, J.R.; Loftus, R.W. Perioperative COVID-19 Defense: An Evidence-Based Approach for Optimization of Infection Control and Operating Room Management. Anesth. Analg. 2020. [Google Scholar] [CrossRef]
- Ong, S.W.X.; Tan, Y.K.; Chia, P.Y.; Lee, T.H.; Ng, O.T.; Wong, M.S.Y.; Marimuthu, K. Air, Surface Environmental, and Personal Protective Equipment Contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) From a Symptomatic Patient. JAMA 2020. [Google Scholar] [CrossRef] [PubMed]
- Izzetti, R.; Nisi, M.; Gabriele, M.; Graziani, F. COVID-19 Transmission in Dental Practice: Brief Review of Preventive Measures in Italy. J. Dent. Res. 2020. [Google Scholar] [CrossRef] [PubMed]
- Smieszek, T.; Lazzari, G.; Salathe, M. Assessing the Dynamics and Control of Droplet- and Aerosol-Transmitted Influenza Using an Indoor Positioning System. Sci. Rep. 2019, 9, 2185. [Google Scholar] [CrossRef] [PubMed]
- Spagnuolo, G.; De Vito, D.; Rengo, S.; Tatullo, M. COVID-19 Outbreak: An Overview on Dentistry. Int. J. Environ. Res. Public Health 2020, 17, 2094. [Google Scholar] [CrossRef] [PubMed]
- Cavallo, L.; Marcianò, A.; Cicciù, M.; Oteri, G. 3D Printing beyond Dentistry during COVID 19 Epidemic: A Technical Note for Producing Connectors to Breathing Devices. Prosthesis 2020, 2, 46–52. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fiorillo, L.; Cervino, G.; Matarese, M.; D’Amico, C.; Surace, G.; Paduano, V.; Fiorillo, M.T.; Moschella, A.; La Bruna, A.; Romano, G.L.; et al. COVID-19 Surface Persistence: A Recent Data Summary and Its Importance for Medical and Dental Settings. Int. J. Environ. Res. Public Health 2020, 17, 3132. https://doi.org/10.3390/ijerph17093132
Fiorillo L, Cervino G, Matarese M, D’Amico C, Surace G, Paduano V, Fiorillo MT, Moschella A, La Bruna A, Romano GL, et al. COVID-19 Surface Persistence: A Recent Data Summary and Its Importance for Medical and Dental Settings. International Journal of Environmental Research and Public Health. 2020; 17(9):3132. https://doi.org/10.3390/ijerph17093132
Chicago/Turabian StyleFiorillo, Luca, Gabriele Cervino, Marco Matarese, Cesare D’Amico, Giovanni Surace, Valeria Paduano, Maria Teresa Fiorillo, Antonio Moschella, Alessia La Bruna, Giovanni Luca Romano, and et al. 2020. "COVID-19 Surface Persistence: A Recent Data Summary and Its Importance for Medical and Dental Settings" International Journal of Environmental Research and Public Health 17, no. 9: 3132. https://doi.org/10.3390/ijerph17093132
APA StyleFiorillo, L., Cervino, G., Matarese, M., D’Amico, C., Surace, G., Paduano, V., Fiorillo, M. T., Moschella, A., La Bruna, A., Romano, G. L., Laudicella, R., Baldari, S., & Cicciù, M. (2020). COVID-19 Surface Persistence: A Recent Data Summary and Its Importance for Medical and Dental Settings. International Journal of Environmental Research and Public Health, 17(9), 3132. https://doi.org/10.3390/ijerph17093132











