Stress-Recovery State in Fibromyalgia Patients and Healthy People. Relationship with the Cardiovascular Response to Stress in Laboratory Conditions
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Questionnaire Measures
2.3. Body Mass Index
2.4. Cardiovascular Recording
2.5. Stress Task: Mental Arithmetic with Harassment
2.6. Procedure
2.7. Statistical Analysis
2.7.1. Preliminary Analyses
2.7.2. Cardiovascular Responses to the Stressor Task
2.7.3. Influence of Stress-Recovery Processes on the Cardiovascular Response
3. Results
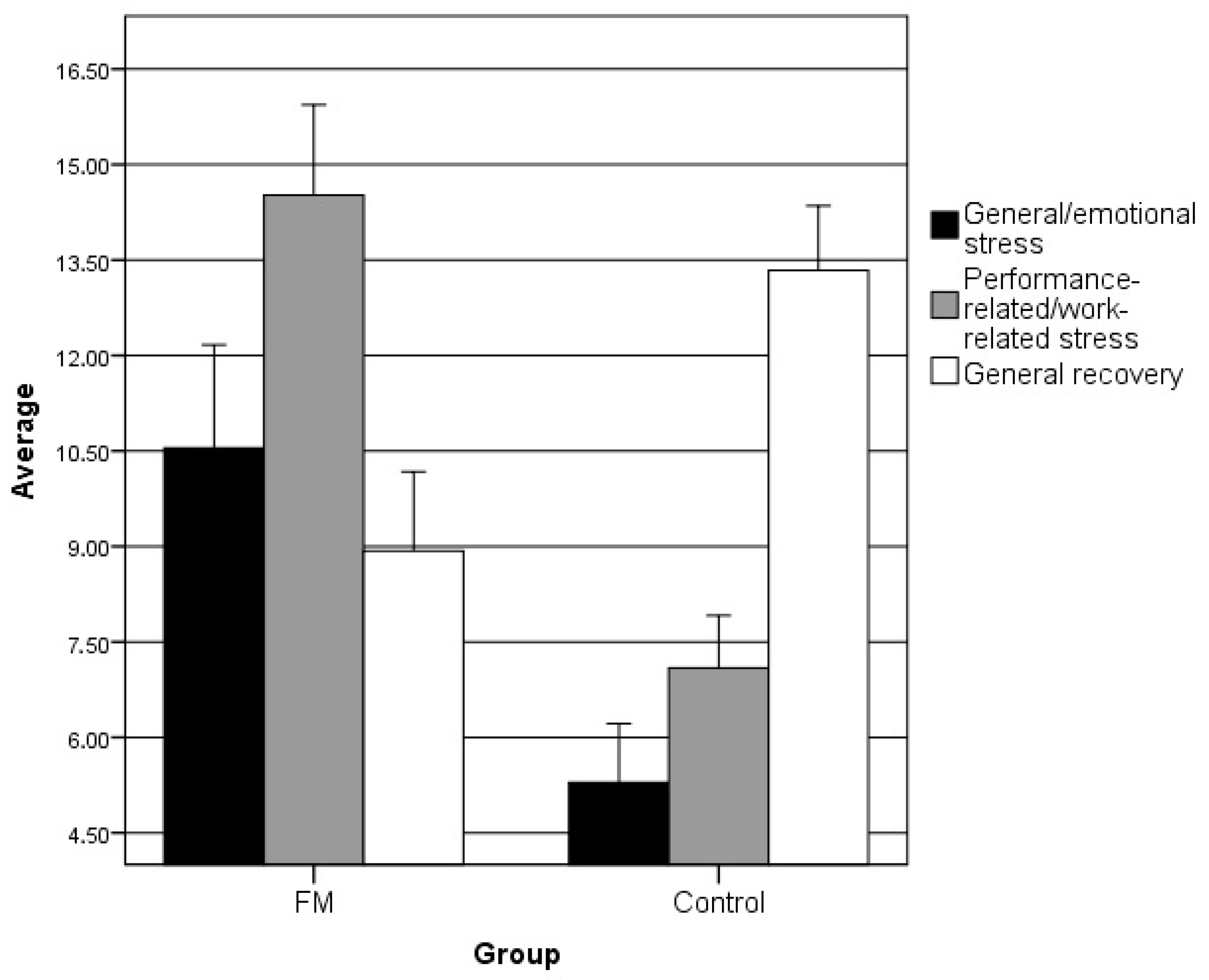
3.1. Preliminary Analyses
3.2. Cardiovascular Responses to the Stressor Task
3.3. The Group as a Moderating Factor in the Relationship between Stress-Recovery Processes and Cardiovascular Response
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kallus, W.K. Impact of Recovery in Different Areas of Application. In Enchancing Recovery: Preventing Underperfomance in Athletes; Kellmann, M., Ed.; Human Kinetics: Champaign, IL, USA, 2002; pp. 283–300. [Google Scholar]
- Secades, G.; Barquín, R.; Vega, D.L.; Márquez, R. Resiliencia y Recuperación-Estrés En Deportistas de Competición Resilience and Recovery-Stress in Competitive Athletes Resiliência e Recuperação-Estresse Em Atletas de Competição. Cuad. Psicol. Deporte 2017, 17, 73–80. [Google Scholar]
- Kellmann, M. Preventing Overtraining in Athletes in High-Intensity Sports and Stress/Recovery Monitoring. Scand. J. Med. Sci. Sports 2010, 20, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Wright, B.J.; O’brien, S.; Hazi, A.; Kent, S. Increased Systolic Blood Pressure Reactivity to Acute Stress Is Related with Better Self-Reported Health. Sci. Rep. 2014, 4, 6882. [Google Scholar] [CrossRef] [Green Version]
- Thieme, K.; Turk, D.C.; Gracely, R.H.; Maixner, W.; Flor, H. The Relationship among Psychological and Psychophysiological Characteristics of Fibromyalgia Patients. J. Pain 2015, 16, 186–196. [Google Scholar] [CrossRef] [PubMed]
- Heidari, J.; Mierswa, T.; Hasenbring, M.; Kleinert, J.; Levenig, C.; Belz, J.; Kellmann, M. Recovery-Stress Patterns and Low Back Pain: Differences in Pain Intensity and Disability. Musculoskelet. Care 2018, 16, 18–25. [Google Scholar] [CrossRef]
- Cohen, H.; Neumann, L.; Kotler, M.; Buskila, D. Autonomic Nervous System Derangement in Fibromyalgia Syndrome and Related Disorders. Isr. Med. Assoc. J. 2001, 3, 755–760. [Google Scholar]
- Meeus, M.; Goubert, D.; De Backer, F.; Struyf, F.; Hermans, L.; Coppieters, I.; De Wandele, I.; Da Silva, H.; Calders, P. Heart Rate Variability in Patients with Fibromyalgia and Patients with Chronic Fatigue Syndrome: A Systematic Review. Semin. Arthritis Rheum. 2013, 43, 279–287. [Google Scholar] [CrossRef]
- Häuser, W.; Kosseva, M.; Üceyler, N.; Klose, P.; Sommer, C. Emotional, Physical, and Sexual Abuse in Fibromyalgia Syndrome: A Systematic Review with Meta-Analysis. Arthritis Care Res. 2011, 63, 808–820. [Google Scholar] [CrossRef]
- Bojner-Horwitz, E.; Theorell, T.; Anderberg, U. Dance/movement therapy and changes in stress-related hormones: A study of fibromyalgia patients with video-interpretation. Arts Psychother. 2003, 30, 255–264. [Google Scholar] [CrossRef]
- Wolfe, F.; Smythe, H.A.; Yunus, M.B.; Bennett, R.M.; Bombardier, C.; Goldenberg, D.L.; Tugwell, P.; Campbell, S.M.; Abeles, M.; Clark, P. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990, 33, 160–172. [Google Scholar] [CrossRef]
- Spindelegger, C.J.; Papageorgiou, K.; Grohmann, R.; Engel, R.; Greil, W.; Konstantinidis, A.; Agelink, M.W.; Bleich, S.; Ruether, E.; Toto, S.; et al. Cardiovascular Adverse Reactions during Antidepressant Treatment: A Drug Surveillance Report of German-Speaking Countries Between 1993 and 2010. Int. J. Neuropsychopharmacol. 2015, 18, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Earlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Dworkin, R.H.; Turk, D.C.; Farrar, J.T.; Haythornthwaite, J.A.; Jensen, M.P.; Katz, N.P.; Kerns, R.D.; Stucki, G.; Allen, R.R.; Bellamy, N.; et al. Core Outcome Measures for Chronic Pain Clinical Trials: IMMPACT Recommendations. Pain 2005, 113, 9–19. [Google Scholar] [CrossRef]
- Bernstein, D.; Fink, L. Manual for the Childhood Trauma Questionnaire; The Psychological Corporation: New York, NY, USA, 1998. [Google Scholar]
- Nijenhuis, E.R.S.; Van der Hart, O.; Kruger, K. The Psychometric Characteristics of the Traumatic Experiences Checklist (TEC): First Findings among Psychiatric Outpatients. Clin. Psychol. Psychother. 2002, 9, 200–210. [Google Scholar] [CrossRef]
- DeLongis, A.; Folkman, S.; Lazarus, R.S. The Impact of Daily Stress on Health and Mood: Psychological and Social Resources as Mediators. J. Pers. Soc. Psychol. 1988, 54, 486–495. [Google Scholar] [CrossRef] [PubMed]
- Sarason, I.G.; Johnson, J.H.; Siegel, J.M. Assessing the Impact of Life Changes: Development of the Life Experiences Survey. J. Consult. Clin. Psychol. 1978, 46, 932–946. [Google Scholar] [CrossRef] [PubMed]
- Aitken, R.C. Measurement of Feelings Using Visual Analogue Scales. Proc. R. Soc. Med. 1969, 62, 989–993. [Google Scholar]
- Lesage, F.X.; Berjot, S.; Deschamps, F. Clinical Stress Assessment Using a Visual Analogue Scale. Occup. Med. 2012, 62, 600–605. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gortner, S.R.; Rankin, S.H.; Wolfe, M.M. Elders’ Recovery from Cardiac Surgery. Prog. Cardiovasc. Nurs. 1988, 3, 54–61. [Google Scholar]
- Kallus, W.K. Der Erholungs-Belastungs-Fragebogen (EBF) [The Recovery-Stress Questionnaire]; Swets & Zeitlinger: Frankfurt, Germany, 1995. [Google Scholar]
- Cairo, E.; García, F.E.Y.; Vancol, R. Consistencia de La Versión Española Del Cuestionario de Estrés- Recuperación (RESTQ 76 Sport), En Deportistas Cubanos. Av. Psicol. Deport. Iberoamérica 2012, 1, 31–40. [Google Scholar]
- Lazarus, R.S. Psychological Stress and the Coping Process; McGraw-Hill: New York, NY, USA, 1966. [Google Scholar]
- Kallus, W.; Kellmann, M. The Recovery-Stress Questionnaires: User Manual; Kallus, K.W., Kellmann, M., Eds.; Pearson Assessment & Information GmbH: Frankfurt, Germany, 2016. [Google Scholar]
- Parati, G.; Casadei, R.; Groppelli, A.; Di Rienzo, M.; Mancia, G. Comparison of Finger and Intra-Arterial Blood Pressure Monitoring at Rest and during Laboratory Testing. Hypertens 1989, 13, 647–655. [Google Scholar] [CrossRef] [Green Version]
- Gerin, W.; Pieper, C.; Pickering, T.G. Measurement Reliability of Cardiovascular Reactivity Change Scores: A Comparison of Intermittent and Continuous Methods of Assessment. J. Psychosom. Res. 1993, 37, 493–501. [Google Scholar] [CrossRef]
- Janssen, S.A.; Spinhoven, P.; Brosschot, J.F. Experimentally Induced Anger, Cardiovascular Reactivity, and Pain Sensitivity. J. Psychosom. Res. 2001, 51, 479–485. [Google Scholar] [CrossRef]
- Glynn, L.M.; Christenfeld, N.; Gerin, W. The Role of Rumination in Recovery from Reactivity: Cardiovascular Consequences of Emotional States. Psychosom. Med. 2002, 64, 714–726. [Google Scholar] [PubMed] [Green Version]
- Radstaak, M.; Geurts, S.A.E.; Brosschot, J.F.; Cillessen, A.H.N.; Kompier, M.A.J. The Role of Affect and Rumination in Cardiovascular Recovery from Stress. Int. J. Psychophysiol. 2011, 81, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Jennings, J.R.; Kamarck, T.; Stewart, C.; Eddy, M.; Johnson, P. Alternate Cardiovascular Baseline Assessment Techniques: Vanilla or Resting Baseline. Psychophysiology 2007, 29, 742–750. [Google Scholar] [CrossRef]
- Hayes, A.F.; Little, T.D. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; The Guilford Press: New York, NY, USA, 2018. [Google Scholar]
- Llabre, M.M.; Spitzer, S.B.; Saab, P.G.; Ironson, G.H.; Schneiderman, N. The Reliability and Specificity of Delta Versus Residualized Change as Measures of Cardiovascular Reactivity to Behavioral Challenges. Psychophysiology 1991, 28, 701–711. [Google Scholar] [CrossRef]
- Buijs, R.M. The Autonomic Nervous System. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2013; Volume 117, pp. 1–11. [Google Scholar] [CrossRef] [Green Version]
- Japundžić-Žigon, N. Vasopressin and Oxytocin in Control of the Cardiovascular System. Curr. Neuropharmacol. 2013, 11, 218–230. [Google Scholar] [CrossRef]
- Mendelson, N.; Gontmacher, B.; Vodonos, A.; Novack, V.; Abu-AjAj, M.; Wolak, A.; Shalev, H.; Wolak, T. Benzodiazepine Consumption Is Associated with Lower Blood Pressure in Ambulatory Blood Pressure Monitoring (ABPM): Retrospective Analysis of 4938 ABPMs. Am. J. Hypertens. 2018, 31, 431–437. [Google Scholar] [CrossRef] [Green Version]
- Wilens, T.E.; Biederman, J.; Baldessarini, R.J.; Geller, B.; Schleifer, D.; Spencer, T.J.; Birmaher, B.; Goldblatt, A. Cardiovascular Effects of Therapeutic Doses of Tricyclic Antidepressants in Children and Adolescents. J. Am. Acad. Child Adolesc. Psychiatry 1996, 35, 1491–1501. [Google Scholar] [CrossRef]
- Zanstra, Y.J.; Johnston, D.W. Cardiovascular Reactivity in Real Life Settings: Measurement, Mechanisms and Meaning. Biol. Psychol. 2011, 86, 98–105. [Google Scholar] [CrossRef] [Green Version]
- Salomon, K.; Bylsma, L.M.; White, K.E.; Panaite, V.; Rottenberg, J. Is Blunted Cardiovascular Reactivity in Depression Mood-State Dependent? A Comparison of Major Depressive Disorder Remitted Depression and Healthy Controls. Int. J. Psychophysiol. 2013, 90, 50–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lyon, P.; Cohen, M.; Quintner, J. An Evolutionary Stress-Response Hypothesis for Chronic Widespread Pain (Fibromyalgia Syndrome). Pain Med. 2011, 12, 1167–1178. [Google Scholar] [CrossRef] [PubMed]
- Bradley, L.A. Pathophysiologic Mechanisms of Fibromyalgia and Its Related Disorders. J. Clin. Psychiatry 2008, 69 (Suppl. 2), 6–13. [Google Scholar]
- Turk, D.; Sherman, J. Treatment of Patients with Fibromyalgia Syndrome. In Psychological Approaches to Pain Management; Turk, D., Gatchel, J., Eds.; Guilford Press: New York, NY, USA, 2002; pp. 390–416. [Google Scholar]
- Williams, D. Cogntive and Behavioral Approaches to Chronic Pain. In Fibromyalgia & Other Central Pain Syndromes; Wallace, D., Clauw, D.J., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2005; pp. 343–352. [Google Scholar]
- Smith, M.T.; Haythornthwaite, J.A. How Do Sleep Disturbance and Chronic Pain Inter-Relate? Insights from the Longitudinal and Cognitive-Behavioral Clinical Trials Literature. Sleep Med. Rev. 2004, 8, 119–132. [Google Scholar] [CrossRef]
- Cully, J.; Teten, A. A Therapist’s Guide to Brief Cognitive Behavioral Therapy; Department of Veterans Affairs South Central MIRECC: Houston, TX, USA, 2008.



| Fibromyalgia | Controls | U Mann-Whitney | |||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Median | Mean | SD | Median | ||
| Severity of Childhood Abuse and Neglect (CTQ) | 49.95 | 17.24 | 46 | 41.21 | 11.51 | 38.5 | 440 ** |
| Potentially Traumatizing Experiences (TEC) | |||||||
| Total Presence | 7.03 | 4.36 | 7 | 3.76 | 2.93 | 3 | 358.500 *** |
| Total Severity | 3.78 | 3.24 | 3 | 1.74 | 1.84 | 1 | 382.500 ** |
| Hassles and Uplifts (HSUP) | |||||||
| Hassles | 40.33 | 21.99 | 40.5 | 28.66 | 17.09 | 25 | 460 * |
| Uplifts | 45.61 | 19.57 | 45 | 60.45 | 26.44 | 60 | 469 * |
| Occurrence of Significant Life Changes (LES) | |||||||
| Frequency | 6.94 | 3.63 | 6.5 | 3.84 | 3.61 | 3 | 365.500 ** |
| Negative Change | −10.05 | 7.01 | −11 | −4.26 | 4.06 | −3 | 346.500 *** |
| Positive Change | 3.89 | 4.06 | 3 | 2.82 | 3.95 | 2 | 539 |
| SBP 1 | DBP 2 | HR 3 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Beta | SE | T(p) | Inc.R2 | F(p) | Beta | SE | T(p) | Inc.R2 | F(p) | Beta | SE | T(p) | Inc.R2 | F(p) | |
| General Stress | −0.24 | 0.55 | −0.44(0.66) | - | - | 0.26 | 0.38 | 0.69(0.49) | - | - | −0.13 | 0.37 | −0.36(0.72) | - | - |
| Group | −9.21 | 8.73 | −1.05(0.29) | - | - | 1.28 | 6.02 | 0.21(0.83) | - | - | −6.79 | 5.82 | −1.17(0.25) | - | - |
| General Stress × Group | 0.74 | 1.12 | 0.66(0.51) | 0.01 | 0.44(0.51) | −0.72 | 0.77 | −0.94(0.35) | 0.01 | 0.88(0.35) | 0.49 | 0.74 | 0.67(0.51) | 0.01 | 0.45(0.51) |
| Performance-Related Stress | 0.57 | 0.63 | 0.91(0.36) | - | - | 0.46 | 0.43 | 1.09(0.28) | - | - | 0.28 | 0.41 | 0.70(0.49) | - | - |
| Group | 3.76 | 12.81 | 0.29(0.77) | - | - | 8.55 | 8.70 | 0.98(0.33) | - | - | −16.1 | 8.35 | −1.93(0.06) | - | - |
| Performance-Related Stress × Group | −1.19 | 1.25 | −1.00(0.34) | 0.01 | 0.91(0.34) | −1.39 | 0.86 | −1.62(0.11) | 0.04 | 2.64(0.11) | 0.97 | 0.82 | 1.18(0.24) | 0.02 | 1.38(0.24) |
| General Recovery | 0.31 | 0.57 | 0.55(0.58) | - | - | 0.14 | 0.39 | 0.35(0.73) | - | - | −0.54 | 0.38 | −1.42(0.16) | - | - |
| Group | −11.9 | 14.01 | −0.85(0.40) | - | - | −10.5 | 9.57 | −1.10(0.27) | - | - | −5.43 | 9.14 | −0.59(0.55) | - | - |
| General Recovery × Group | 0.76 | 1.14 | 0.67(0.51) | 0.01 | 0.44(0.51) | 0.73 | 0.79 | 0.92(0.36) | 0.01 | 0.86(0.36) | −0.05 | 0.75 | −0.06(0.95) | 0.00 | 0.00(0.95) |
| SBP 1 | DBP 2 | HR 3 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Beta | SE | T(p) | Inc.R2 | F(p) | Beta | SE | T(p) | Inc.R2 | F(p) | Beta | SE | T(p) | Inc.R2 | F(p) | |
| General Stress | −0.74 | 0.41 | −1.83(0.07) | - | - | −0.37 | 0.23 | −1.57(0.12) | - | - | −0.16 | 0.23 | −0.69(0.49) | - | - |
| Group | −10.2 | 6.42 | −1.58(0.12) | - | - | −3.83 | 3.68 | −1.04(0.30) | - | - | −6.68 | 3.60 | −1.85(0.07) | - | - |
| General Stress × Group | 0.81 | 0.81 | 1.00(0.32) | 0.01 | 1.00(0.32) | 0.49 | 0.47 | 1.05(0.30) | 0.01 | 1.10(0.30) | 0.15 | 0.45 | 0.32(0.75) | 0.00 | 0.11(0.75) |
| Performance-Related Stress | −0.88 | 0.45 | −1.93(0.06) | - | - | −0.72 | 0.26 | −2.79(0.01) | - | - | −0.55 | 0.25 | −2.20(0.03) | - | - |
| Group | −20.3 | 9.24 | −2.20(0.03) | - | - | −8.06 | 5.24 | −1.54(0.13) | - | - | −11.9 | 5.18 | −2.30(0.02) | - | - |
| Performance-Related Stress × Group | 1.78 | 0.91 | 1.95(0.05) | 0.05 | 3.82(0.05) | 1.10 | 0.52 | 2.14(0.04) | 0.06 | 4.56(0.04) | 0.89 | 0.50 | 1.78(0.08) | 0.03 | 3.16(0.08) |
| General Recovery | 0.30 | 0.42 | 0.72(0.48) | - | - | 0.13 | 0.24 | 0.55(0.58) | - | - | 0.19 | 0.23 | 0.82(0.42) | - | - |
| Group | −19.6 | 10.19 | −1.93(0.06) | - | - | −6.69 | 5.94 | −1.13(0.26) | - | - | −15.9 | 5.50 | −2.89(0.01) | - | - |
| General Recovery × Group | 1.20 | 0.84 | 1.43(0.16) | 0.03 | 2.04(0.16) | 0.48 | 0.49 | 0.98(0.33) | 0.01 | 0.58(0.33) | 0.94 | 0.45 | 2.07(0.04) | 0.05 | 4.29(0.04) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matías Pompa, B.; López López, A.; Alonso Fernández, M.; Vargas Moreno, E.; González Gutiérrez, J.L. Stress-Recovery State in Fibromyalgia Patients and Healthy People. Relationship with the Cardiovascular Response to Stress in Laboratory Conditions. Int. J. Environ. Res. Public Health 2020, 17, 3138. https://doi.org/10.3390/ijerph17093138
Matías Pompa B, López López A, Alonso Fernández M, Vargas Moreno E, González Gutiérrez JL. Stress-Recovery State in Fibromyalgia Patients and Healthy People. Relationship with the Cardiovascular Response to Stress in Laboratory Conditions. International Journal of Environmental Research and Public Health. 2020; 17(9):3138. https://doi.org/10.3390/ijerph17093138
Chicago/Turabian StyleMatías Pompa, Borja, Almudena López López, Miriam Alonso Fernández, Estefanía Vargas Moreno, and José Luis González Gutiérrez. 2020. "Stress-Recovery State in Fibromyalgia Patients and Healthy People. Relationship with the Cardiovascular Response to Stress in Laboratory Conditions" International Journal of Environmental Research and Public Health 17, no. 9: 3138. https://doi.org/10.3390/ijerph17093138
APA StyleMatías Pompa, B., López López, A., Alonso Fernández, M., Vargas Moreno, E., & González Gutiérrez, J. L. (2020). Stress-Recovery State in Fibromyalgia Patients and Healthy People. Relationship with the Cardiovascular Response to Stress in Laboratory Conditions. International Journal of Environmental Research and Public Health, 17(9), 3138. https://doi.org/10.3390/ijerph17093138





