Children’s Health in the Digital Age
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Health Risks Related to Children’s over Exposure to Digital Environments
3.1.1. Myopia and Early Blindness
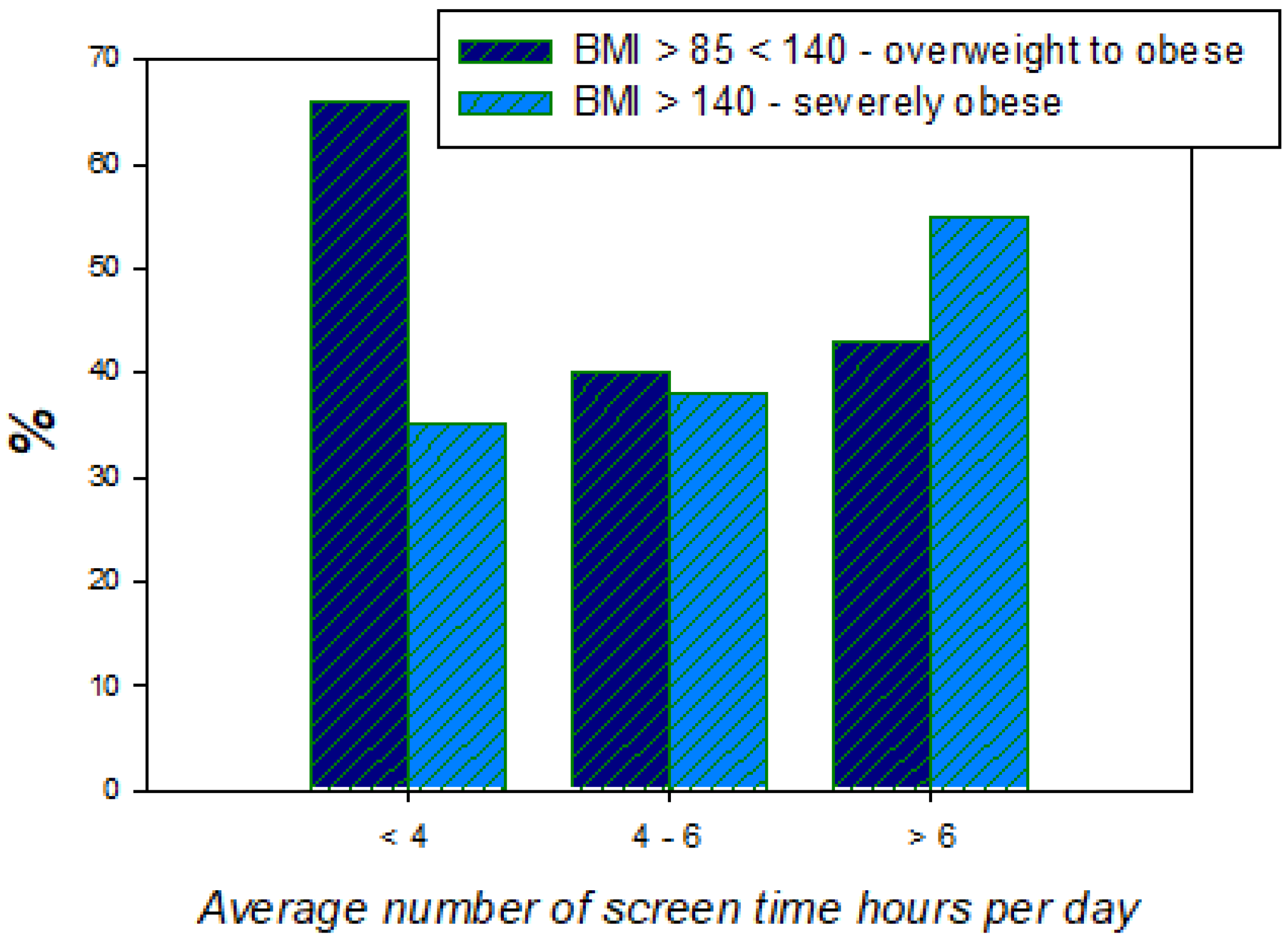
3.1.2. Obesity
3.1.3. Sleep Disorders, Anxiety, Depression
3.1.4. Digital Addiction
3.2. The Early Deregulation of Neurotransmitter Pathways in the Child’s Developing Brain: Towards a Unifying Model Account
3.2.1. Exposure to the Wrong Kind of Light at the Wrong Time
3.2.2. Resulting Functional Consequences of Vitamin D and Melatonin Deficiency
3.2.3. Early Deregulation of Neurotransmitter Pathways in the Developing Brain
4. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Chaudron, S. Young Children (0–8) and Digital Technology: A Qualitative Exploratory Study Across Seven Countries; Luxembourg Publications Office of the European Union: Brussels, Belgium, 2015. [Google Scholar] [CrossRef]
- Spillmann, L. Stopping the rise of myopia in Asia. Graefe’s Arch. Clin. Exp. Ophthalmol. 2020, 258, 943–959. [Google Scholar] [CrossRef] [PubMed]
- Dolgin, E. The myopia boom. Nature 2015, 519, 276–278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holden, B.A.; Fricke, T.R.; Wilson, D.A.; Jong, M.; Naidoo, K.S.; Sankaridurg, P.; Wong, T.Y.; Naduvilath, T.J.; Resnikoff, S. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016, 123, 1036–1042. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holden, B.A.; Jong, M.; Davis, S.; Wilson, D.; Fricke, T.; Resnikoff, S. Nearly 1 billion myopes at risk of myopia-related sight threatening conditions by 2050—Time to act now. Clin. Exp. Optom. 2015, 98, 491–493. [Google Scholar] [CrossRef]
- Iwase, A.; Araie, M.; Tomidokoro, A.; Yamamoto, T.; Shimizu, H.; Kitazawa, Y.; Tajimi Study Group. Prevalence and causes of low vision and blindness in a Japanese adult population: The Tajimi Study. Ophthalmology 2006, 113, 1354–1362. [Google Scholar] [CrossRef]
- Vitale, S.; Sperduto, R.D.; Ferris, F.L., 3rd. Increased prevalence of myopia in the United States between 1971–1972 and 1999–2004. Arch. Ophthalmol. 2009, 127, 1632–1639. [Google Scholar] [CrossRef] [Green Version]
- Pan, C.W.; Dirani, M.; Cheng, C.Y.; Wong, T.Y.; Saw, S.M. The age-specific prevalence of myopia in Asia: A meta-analysis. Optom. Vis. Sci. 2015, 92, 258–266. [Google Scholar] [CrossRef]
- Lin, L.L.; Shih, Y.F.; Hsiao, C.K.; Chen, C.J. Prevalence of myopia in Taiwanese schoolchildren: 1983 to 2000. Ann. Acad. Med. Singap. 2004, 33, 27–33. [Google Scholar]
- Wilson, D.A.; Jong, M.; Sankaridurg, P.; Fricke, T.R.; Resnikoff, S.; Naidoo, K. A global generational shift in myopia. Assoc. Res. Vis. Ophthalmol. 2016, 57, 2468. [Google Scholar]
- Lopez, R.B.; Brand, G.; Gilbert-Diamond, D. Media Multitasking is Associated With Higher Body Mass Index in Pre-adolescent Children. Front. Psychol. 2019, 10, 2534. [Google Scholar] [CrossRef]
- Lopez, R.B.; Heatherton, T.F.; Wagner, D.D. Media multitasking is associated with higher risk for obesity and increased responsiveness to rewarding food stimuli. Brain Imaging Behav. 2019. [Google Scholar] [CrossRef] [Green Version]
- Demirci, K.; Akgönül, M.; Akpinar, A. Relationship of smartphone use severity with sleep quality, depression, and anxiety in university students. J. Behav. Addict. 2015, 4, 85–92. [Google Scholar] [CrossRef] [Green Version]
- Colten, H.R.; Altevogt, B.M. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. In Institute of Medicine Committee on Sleep Medicine and Research; National Academies Press: Washington, DC, USA, 2006. [Google Scholar]
- Weaver, E.; Gradisar, M.; Dohnt, H.; Lovato, N.; Douglas, P. The effect of pre-sleep video game playing on adolescent sleep. J. Clin. Sleep Med. 2010, 6, 184–189. [Google Scholar] [CrossRef] [Green Version]
- Harada, T.; Morikuni, M.; Yoshii, S.; Yamashita, Y.; Takeuchi, H. Usage of mobile phone in the evening or at night makes Japanese students evening-typed and night sleep uncomfortable. Sleep Hypn. 2002, 4, 149–153. [Google Scholar]
- Grandner, M.A. Sleep duration across the lifespan: Implications for health. Sleep Med. Rev. 2012, 16, 199–201. [Google Scholar] [CrossRef] [Green Version]
- Li, S.; Jin, X.; Wu, S.; Jiang, F.; Yan, C.; Shen, X. The impact of media use on sleep patterns and sleep disorders among school-aged children in China. Sleep 2007, 30, 361–367. [Google Scholar] [CrossRef]
- Li, S.; Arguelles, L.; Jiang, F.; Chen, W.; Jin, X.; Yan, C.; Tian, Y.; Hong, X.; Qian, C.; Zhang, J.; et al. Sleep, school performance, and a school-based intervention among school-aged children: A sleep series study in China. PLoS ONE 2013, 8, e67928. [Google Scholar] [CrossRef] [PubMed]
- Galland, B.; Spruyt, K.; Dawes, P.; McDowall, P.S.; Elder, D.; Schaughency, E. Sleep Disordered Breathing and Academic Performance: A Meta-analysis. Pediatrics 2015, 136, e934–e946. [Google Scholar] [CrossRef] [Green Version]
- Goodman, A.; Page, A.S.; Cooper, A.R.; International Children’s Accelerometry Database (ICAD) Collaborators. Daylight saving time as a potential public health intervention: An observational study of evening daylight and objectively-measured physical activity among 23,000 children from 9 countries. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harrison, F.; Goodman, A.; van Sluijs, E.M.F.; Andersen, L.B.; Cardon, G.; Davey, R.; Janz, K.F.; Kriemler, S.; Molloy, L.; Page, A.S.; et al. Weather and children’s physical activity; how and why do relationships vary between countries? Int. J. Behav. Nutr. Phys. Act. 2017, 14, 74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCrorie, P.; Mitchell, R.; Macdonald, L.; Jones, A.; Coombes, E.; Schipperijn, J.; Ellaway, A. The relationship between living in urban and rural areas of Scotland and children’s physical activity and sedentary levels: A country-wide cross-sectional analysis. BMC Public Health 2020, 20, 304. [Google Scholar] [CrossRef] [PubMed]
- Liston, K. Literature Review Methods. Available online: https://web.stanford.edu/class/cee320/CEE320A/POD.pdf (accessed on 20 April 2020).
- Bourne, R.R.; Stevens, G.A.; White, R.A.; Smith, J.L.; Flaxman, S.R.; Price, H.; Jonas, J.B.; Keeffe, J.; Leasher, J.; Naidoo, K.; et al. Causes of vision loss worldwide, 1990–2010: A systematic analysis. Lancet Glob. Health 2013, 1, e339–e349. [Google Scholar] [CrossRef] [Green Version]
- Boren, Z.D. There are officially more mobile devices than people in the world. Independent 2014, 7, 2014. [Google Scholar]
- Kemp, S. Global Digital Overview. 2019. Available online: https://datareportal.com/reports/digital-2019-global-digital-overview (accessed on 20 April 2020).
- Bhattacharjee, P. How Does Your Child’s Screen Time Measure up? 2017. Available online: https://edition.cnn.com/2017/11/15/health/screen-time-averages-parenting/index.html (accessed on 20 April 2020).
- Korvorst, M.; Sleijpen, G. Most Young People Online with Smartphone. 2014. Available online: https://www.cbs.nl/en-gb/news/2014/22/most-young-people-online-with-smartphone (accessed on 20 April 2020).
- Lanca, C.; Saw, S.M. The association between digital screen time and myopia: A systematic review. Ophthalmic Physiol. Opt. 2020, 40, 216–229. [Google Scholar] [CrossRef] [Green Version]
- Internet Penetration and Use in Asia 2000–2020. The Nation, Thailand. 2018. Available online: https://www.nationthailand.com/asean-plus/30355963 (accessed on 20 April 2020).
- Morgan, I.G.; French, A.N.; Ashby, R.S.; Guo, X.; Ding, X.; He, M.; Rose, K.A. The epidemics of myopia: Etiology and prevention. Prog. Retin Eye Res. 2018, 62, 134–149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO Commission on Ending Childhood Obesity: Facts and Figures. 2019. Available online: https://www.who.int/end-childhood-obesity/facts/en/ (accessed on 20 April 2020).
- Robinson, T.N.; Banda, J.A.; Hale, L.; Lu, A.S.; Fleming-Milici, F.; Calvert, S.L.; Wartella, E. Screen Media Exposure and Obesity in Children and Adolescents. Pediatrics 2017, 140 (Suppl. 2), S97–S101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smit, C.R.; Buijs, L.; van Woudenberg, T.J.; Bevelander, K.E.; Buijzen, M. The Impact of Social Media Influencers on Children’s Dietary Behaviors. Front. Psychol. 2020, 10, 2975. [Google Scholar] [CrossRef] [PubMed]
- Phan, T.T.; Tucker, J.M.; Siegel, R.; Christison, A.L.; Stratbucker, W.; Werk, L.N.; Hossain, J.; Datto, G.; Gentile, D.A.; Stubblefield, S. Electronic Gaming Characteristics Associated with Class 3 Severe Obesity in Youth Who Attend the Pediatric Weight Management Programs of the COMPASS Network. Child Obes. 2019, 15, 21–30. [Google Scholar] [CrossRef]
- Braithwaite, I.; Stewart, A.W.; Hancox, R.J.; Beasley, R.; Murphy, R.; Mitchell, E.A. The worldwide association between television viewing and obesity in children and adolescents: Cross sectional study. PLoS ONE 2013, 8, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Gao, Z.; Chen, S.; Pasco, D.; Pope, Z. A meta-analysis of active video games on health outcomes among children and adolescents. Obes. Rev. 2015, 16, 783–794. [Google Scholar] [CrossRef]
- Wang, X.; Perry, A.C. Metabolic and physiologic responses to video game play in 7- to 10-year old boys. Arch. Pediatr. Adolesc. Med. 2006, 160, 411–415. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vucetic, Z.; Reyes, T.M. Central dopaminergic circuitry controlling food intake and reward: Implications for the regulation of obesity. Wiley Interdiscip. Rev. Syst. Biol. Med. 2010, 2, 577–593. [Google Scholar] [CrossRef] [PubMed]
- ABC Australia. Eyes Wide Open; ABC Australia: Sydney, Australia, 2007. [Google Scholar]
- Howard, J. Kids under 9 Spend More than 2 hours a Day on Screens. CNN Health, USA. 2017. Available online: https://edition.cnn.com/2017/10/19/health/children-smartphone-tablet-use-report/index.html (accessed on 20 April 2020).
- Hysing, M.; Pallesen, S.; Stormark, K.M.; Jakobsen, R.; Lundervold, A.J.; Sivertsen, B. Sleep and use of electronic devices in adolescence: Results from a large population-based study. BMJ Open 2015, 5, e006748. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bruni, O.; Sette, S.; Fontanesi, L.; Baiocco, R.; Laghi, F.; Baumgartner, E. Technology use and sleep quality in preadolescence and adolescence. J. Clin. Sleep Med. 2015, 11, 1433. [Google Scholar] [CrossRef] [PubMed]
- Curcio, G.; Ferrara, M.; de Gennaro, L. Sleep loss, learning capacity and academic performance. Sleep Med. Rev. 2006, 10, 323–337. [Google Scholar] [CrossRef] [PubMed]
- Dewald, J.F.; Meijer, A.M.; Oort, F.J.; Kerkhof, G.A.; Bögels, S.M. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: A meta-analytic review. Sleep Med. Rev. 2010, 14, 179–189. [Google Scholar] [CrossRef]
- Gradisar, M.; Terrill, G.; Johnston, A.; Douglas, P. Adolescent sleep and working memory performance. Sleep Biol. Rhythms 2008, 6, 146–154. [Google Scholar] [CrossRef]
- Van den Bulck, J. Text messaging as a cause of sleep interruption in adolescents, evidence from a cross-sectional study. J. Sleep Res. 2003, 12, 263. [Google Scholar] [CrossRef]
- Dworak, M.; Schierl, T.; Bruns, T.; Struder, H.K. Impact of singular excessive computer game and television exposure on sleep patterns and memory performance of school-aged children. Pediatrics 2007, 120, 978–985. [Google Scholar] [CrossRef]
- Hebert, S.; Beland, R.; Dionne-Fournelle, O.; Crete, M.; Lupien, S.J. Physiological stress response to video-game playing: The contribution of built-in music. Life Sci. 2005, 76, 2371–2380. [Google Scholar] [CrossRef]
- Higuchi, S.; Motohashi, Y.; Liu, Y.; Maeda, A. Effects of playing a computer game using a bright display on pre-sleep physiological variables, sleep latency, slow wave sleep and REM sleep. J. Sleep Res. 2005, 14, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Hamblin, D.L.; Wood, A.W. Effects of mobile phone emissions on human brain activity and sleep variables. Int. J. Radiat. Biol. 2002, 78, 659–669. [Google Scholar] [CrossRef] [PubMed]
- Loughran, S.P.; Wood, A.W.; Barton, J.M.; Croft, R.J.; Thompson, B.; Stough, C. The effect of electromagnetic fields emitted by mobile phones on human sleep. Neuroreport 2005, 16, 1973–1976. [Google Scholar] [CrossRef] [PubMed]
- Cain, N.; Gradisar, M. Electronic media use and sleep in school-aged children and adolescents: A review. Sleep Med. 2010, 11, 735–742. [Google Scholar] [CrossRef]
- Arora, T.; Broglia, E.; Thomas, G.N.; Taheri, S. Associations between specific technologies and adolescent sleep quantity, sleep quality, and parasomnias. Sleep Med. 2014, 15, 240–247. [Google Scholar] [CrossRef]
- Anderson, D.; Subrahmanyam, K. Digital Screen Media and Cognitive Development, on behalf of the Cognitive Impacts of Digital Media Workgroup of the OECD. Pediatrics 2017, 140, S57–S61. [Google Scholar] [CrossRef] [Green Version]
- Bavelier, D.; Green, D.; Dye, M. Children, Wired: For Better and for Worse. Neuron 2010, 67, 692–701. [Google Scholar] [CrossRef] [Green Version]
- Brown, A. Media use by children younger than 2 years. J. Am. Acad. Pediatr. 2011, 128, 1040–1045. [Google Scholar]
- Shaw, M.; Black, D.W. Internet addiction: Definition, assessment, epidemiology and clinical management. CNS Drugs 2008, 22, 353–365. [Google Scholar] [CrossRef]
- Cao, F.; Su, L. Internet addiction among Chinese adolescents: Prevalence and psychological features. Child Care Health Dev. 2006, 33, 275–281. [Google Scholar] [CrossRef]
- Fu, K.W.; Chan, W.S.; Wong, P.W.; Yip, P.S. Internet addiction: Prevalence, discriminant validity and correlates among adolescents in Hong Kong. Br. J. Psychiatry 2010, 196, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Nalwa, K.; Anand, A.P. Internet addiction in students: A cause of concern. Cyberpsychol. Behav. 2003, 6, 653–656. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.; Li, A.Y. Internet addiction prevalence and quality of (real) life: A meta-analysis of 31 nations across seven world regions. Cyberpsychol. Behav. Soc. Netw. 2014, 17, 755–760. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krishnamurthy, S.; Chetlapalli, S.K. Internet addiction: Prevalence and risk factors: A cross-sectional study among college students in Bengaluru, the Silicon Valley of India. Indian J. Public Health 2015, 59, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.; Ryu, E.; Chon, M.Y.; Yeun, E.J.; Choi, S.Y.; Nam, B.M. Internet addiction in Korean adolescents and its relation to depression and suicidal ideation: A questionnaire survey. Int. J. Nurs. Stud. 2006, 43, 185–192. [Google Scholar] [CrossRef]
- Dalbudak, E.; Evren, C.; Aldemir, S.; Coskun, K.S.; Ugurlu, H.; Yildirim, F.G. Relationship of internet addiction severity with depression, anxiety and alexithymia, temperament and character in university students. Cyberpsychol. Behav. Soc. Netw. 2013, 16, 272–278. [Google Scholar] [CrossRef]
- Lau, J.T.F.; Walden, D.L.; Wu, A.M.S.; Cheng, K.M.; Lau, M.C.M.; Mo, P.K.H. Bidirectional predictions between Internet addiction and probable depression among Chinese adolescents. J. Behav. Addict. 2018, 7, 633–643. [Google Scholar] [CrossRef]
- Li, J.B.; Lau, J.T.F.; Mo, P.K.H.; Su, X.F.; Tang, J.; Qin, Z.G.; Gross, D.L. Insomnia partially mediates the association between problematic Internet use and depression among secondary school students in China. J. Behav. Addict. 2017, 6, 554–563. [Google Scholar] [CrossRef]
- American Psychiatric Association. DSM-5—Manuel Diagnostique et Statistique des Troubles Mentaux; Elsevier: Amsterdam, The Netherlands, 2019. [Google Scholar]
- World Health Organization. International Classification of Diseases for Mortality and Morbidity Statistics (11th Revision). 2020. Available online: https://icd.who.int/browse11/l-m/en (accessed on 20 April 2020).
- Ojeda, J.; Ávila, A. Early Actions of Neurotransmitters during Cortex Development and Maturation of Reprogrammed Neurons. Front. Synaptic Neurosci. 2019, 11, 33. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.H.; Baik, S.H.; Park, C.S.; Kim, S.J.; Choi, S.W.; Kim, S.E. Reduced striatal dopamine D2 receptors in people with Internet addiction. Neuroreport 2011, 22, 407–411. [Google Scholar] [CrossRef]
- Hou, H.; Jia, S.; Hu, S.; Fan, R.; Sun, W.; Sun, T.; Zhang, H. Reduced striatal dopamine transporters in people with internet addiction disorder. J. Biomed. Biotechnol. 2012, 13, 854524. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Friston, K.J.; Liu, J.; Liu, Y.; Zhang, G.; Cao, F.; Su, L.; Yao, S.; Lu, H.; Hu, D. Impaired Frontal-Basal Ganglia Connectivity in Adolescents with Internet Addiction. Sci. Rep. 2014, 4, 5027. [Google Scholar] [CrossRef] [Green Version]
- Rumpf, H.J.; Achab, S.; Billieux, J.; Bowden-Jones, H.; Carragher, N.; Demetrovics, Z.; Higuchi, S.; King, D.L.; Mann, K.; Potenza, M.; et al. Including gaming disorder in the ICD-11: The need to do so from a clinical and public health perspective. J. Behav. Addict. 2018, 7, 556–561. [Google Scholar] [CrossRef] [PubMed]
- Ryan, P. Technology: The New Addiction. US Naval Institute Publications. Proceedings 2018, 144, 387. [Google Scholar]
- The Center for Epidemiological Studies Depression Scale Revised. 2020. Available online: https://cesd-r.com/ (accessed on 20 April 2020).
- The Pittsburgh Sleep Quality Index. 2020. Available online: https://en.wikipedia.org/wiki/Pittsburgh_Sleep_Quality_Index (accessed on 20 April 2020).
- Young’s Diagnostic Questionnaire for Internet Addiction. 2020. Available online: https://journals.plos.org/plosone/article/file?type=supplementary&id=info:doi/10.1371/journal.pone.0107306.s001 (accessed on 20 April 2020).
- Faraci, P.; Craparo, G.; Messina, R.; Severino, S. Internet Addiction Test (IAT): Which is the best factorial solution? J. Med. Internet Res. 2013, 15, e225. [Google Scholar] [CrossRef] [PubMed]
- Shakya, H.B.; Christakis, N.A. Association of ‘Facebook’ use with compromised well-being: A longitudinal study. Am. J. Epidemiol. 2017, 185, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Dong, G.; Hu, Y.; Lin, X.; Lu, Q. What makes Internet addicts continue playing online even when faced by severe negative consequences? Possible explanations from an fMRI study. Biol. Psychol. 2013, 94, 282–289. [Google Scholar] [CrossRef]
- Dong, G.; Shen, Y.; Huang, J.; Du, X. Impaired error-monitoring function in people with Internet addiction disorder: An event-related FMRI study. Eur. Addict. Res. 2013, 19, 269–275. [Google Scholar] [CrossRef]
- Dong, G.; Huang, J.; Du, X. Enhanced reward sensitivity and decreased loss sensitivity in Internet addicts: An fMRI study during a guessing task. J. Psychiatr. Res. 2011, 45, 1525–1529. [Google Scholar] [CrossRef]
- Dong, G.; Lin, X.; Zhou, H.; Lu, Q. Cognitive flexibility in Internet addicts: fMRI evidence from difficult-to-easy and easy-to-difficult switching situations. Addict. Behav. 2014, 9, 677–683. [Google Scholar] [CrossRef]
- Dong, G.; Lu, Q.; Zhou, H.; Zhao, X. Impulse inhibition in people with Internet addiction disorder: Electrophysiological evidence from a Go/NoGo study. Neurosci. Lett. 2010, 485, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Brand, M.; Young, K.S.; Laier, C. Prefrontal control and internet addiction: A theoretical model and review of neuropsychological and neuroimaging findings. Front. Hum. Neurosci. 2014, 8, 375. [Google Scholar] [CrossRef] [PubMed]
- Fricke, T.R.; Holden, B.A.; Wilson, D.A.; Schlenthe, G.; Naidood, K.S.; Resnikoff, S.; Fric, K.D. Global cost of correcting vision impairment from uncorrected refractive error. Bull. World Health Org. 2012, 90, 728–738. [Google Scholar] [CrossRef] [PubMed]
- Morgan, I.G. What public policies should be developed to deal with the epidemic of myopia? Optom. Vis. Sci. 2016, 93, 108–1060. [Google Scholar] [CrossRef]
- Jong, M.; Sankaridurg, P.; Naidoo, K. Myopia, a public health crisis in waiting: Points de vue. Internat. Rev. Ophthalmic Opt. 2016, 73, 44–48. [Google Scholar]
- Holden, B.A.; Mariotti, S.P.; Kocur, I.; Resnikoff, S.; He, M. The impact of myopia and high myopia. In Proceedings of the World Health Organization’s Brien Holden Vision Institute Global Scientific Meeting on Myopia, Sydney, Australia, 16–18 March 2015. [Google Scholar]
- Knapton, S. Night Time Contact Lenses Stop Children Becoming Short-Sighted. The Telegraph, 27 June 2015. [Google Scholar]
- Sherwin, J.C.; Reacher, M.H.; Keogh, R.H.; Khawaja, A.P.; Mackey, D.A.; Foster, P.J. The Association between Time Spent Outdoors and Myopia in Children and Adolescents. Ophthalmology 2012, 119, 2141–2151. [Google Scholar] [CrossRef]
- Kang, M.T.; Li, S.M.; Peng, X.; Li, L.; Ran, A.; Meng, B.; Sun, Y.; Liu, L.R.; Li, H.; Millodot, M.; et al. Chinese Eye Exercises and Myopia Development in School Age Children: A Nested Case-control Study. Sci. Rep. 2016, 6, 28531. [Google Scholar] [CrossRef] [Green Version]
- Rose, K.A.; Morgan, I.G.; Ip, J.; Kifley, A.; Huynh, S.; Smith, W.; Mitchell, P. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology 2008, 115, 1279–1285. [Google Scholar] [CrossRef]
- Wu, P.C.; Tsai, C.L.; Wu, H.L.; Yang, Y.H.; Kuo, H.K. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology 2013, 120, 1080–1085. [Google Scholar] [CrossRef]
- Kiorpes, L. The Puzzle of Visual Development: Behavior and Neural Limits. J. Neurosci. 2016, 36, 11384–11393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fuhrmann, D.; Knoll, L.; Blakemore, S. Adolescence as a Sensitive Period of Brain Development. Trends Cognit. Sci. 2015, 19, 558–566. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atkinson, J.; Braddick, O. Inferences about infants’ visual brain mechanisms. Vis. Neurosci. 2013, 30, 185–195. [Google Scholar] [CrossRef] [PubMed]
- Bedrosian, T.A.; Nelson, R.J. Timing of light exposure affects mood and brain circuits. Transl. Psychiatry 2017, 7, e1017. [Google Scholar] [CrossRef]
- Rich, C.; Longcore, T. Ecological Consequences of Artificial Night Lighting; Island Press: Washington, DC, USA, 2006. [Google Scholar]
- Navara, K.J.; Nelson, R.J. The dark side of light at night: Physiological, epidemiological, and ecological consequences. J. Pineal Res. 2007, 43, 215–224. [Google Scholar] [CrossRef] [PubMed]
- The Canadian Paediatric Society. Screen time and young children: Promoting health and development in a digital world. Paediatri. Child Health 2017, 22, 461–468. [Google Scholar] [CrossRef] [Green Version]
- Wood, B.; Rea, M.S.; Plitnick, B.; Figueiro, M.G. Light level and duration of exposure determine the impact of self-luminous tablets on melatonin suppression. Appl. Ergon. 2013, 44, 237. [Google Scholar] [CrossRef]
- Calhoun, S.L.; Vgontzas, A.N.; Fernandez-Mendoza, J.; Mayes, S.D.; Tsaoussoglou, M.; Basta, M.; Bixler, E.O. Prevalence and risk factors of excessive daytime sleepiness in a community sample of young children: The role of obesity, asthma, anxiety/depression, and sleep. Sleep 2011, 34, 503–507. [Google Scholar] [CrossRef] [Green Version]
- Cappuccio, F.P.; Taggart, F.M.; Kandala, N.B.; Currie, A.; Peile, E.; Stranges, S.; Miller, M.A. Meta-analysis of short sleep duration and obesity in children and adults. Sleep 2008, 31, 619–626. [Google Scholar] [CrossRef] [Green Version]
- Beebe, D.W. Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents. Pediatr. Clin. N. Am. 2011, 58, 649–665. [Google Scholar] [CrossRef] [Green Version]
- Falbe, J.; Davison, K.K.; Franckle, R.L.; Ganter, C.; Gortmaker, S.L.; Smith, L.; Land, T.; Taveras, E.M. Sleep duration, restfulness, and screens in the sleep environment. Pediatrics 2015, 135, e367–e375. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buxton, O.M.C.A.-M.; Spilsbury, J.C.; Bos, T.; Emsellem, H.; Knutson, K.L. Sleep in the modern family: Protective family routines for child and adolescent sleep. Sleep Health 2015, 1, 15–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hale, L.; Kirschen, G.W.; LeBourgeois, M.K.; Gradisar, M.; Garrison, M.M.; Montgomery-Downs, H.; Kirschen, H.; McHale, S.M.; Chang, A.M.; Buxton, O.M. Youth Screen Media Habits and Sleep: Sleep-Friendly Screen Behavior Recommendations for Clinicians, Educators, and Parents. Child Adolesc. Psychiatr. Clin. N. Am. 2018, 27, 229–245. [Google Scholar] [CrossRef]
- Uncapher, M.R.; Wagner, A.D. Minds and brains of media multitaskers: Current findings and future directions. Proc. Natl. Acad. Sci. USA 2018, 115, 988. [Google Scholar] [CrossRef] [Green Version]
- Muscogiuri, G.; Barrea, L.; Scannapieco, M.; Di Somma, C.; Scacchi, M.; Aimaretti, G.; Savastano, S.; Colao, A.; Marzullo, P. The lullaby of the sun: The role of vitamin D in sleep disturbance. Sleep Med. 2019, 54, 262–265. [Google Scholar] [CrossRef]
- Rajakumar, K.; Greenspan, S.L.; Thomas, S.B.; Holick, M.F. Solar ultraviolet radiation and vitamin D: A historical perspective. Am. J. Public Health 2007, 97, 1746–1754. [Google Scholar] [CrossRef]
- Barger-Lux, M.J.; Heaney, R.P. Effects of above average summer sun exposure on serum 25-hydroxyvitamin D and calcium absorption. J. Clin. Endocrinol. Metab. 2002, 87, 4952–4956. [Google Scholar] [CrossRef]
- St-Onge, M.P.; Mikic, A.; Pietrolungo, C.E. Effects of Diet on Sleep Quality. Adv. Nutr. 2016, 7, 938–949. [Google Scholar] [CrossRef]
- Zhao, K.; Luan, X.; Liu, Y.; Tu, X.; Chen, H.; Shen, H.; Qiu, H.; Zhu, Z.; He, J. Low serum 25-hydroxyvitamin D concentrations in chronic insomnia patients and the association with poor treatment outcome at 2 months. Clin. Chim. Acta 2017, 475, 147–151. [Google Scholar] [CrossRef]
- Majid, M.S.; Ahmad, H.S.; Bizhan, H.; Hosein, H.Z.; Mohammad, A. The effect of vitamin D supplement on the score and quality of sleep in 20–50 year-old people with sleep disorders compared with control group. Nutr. Neurosci. 2018, 21, 511–519. [Google Scholar] [CrossRef]
- Kim, J.H.; Chang, J.H.; Kim, D.Y.; Kang, J.W. Association between self-reported sleep duration and serum vitamin D level in elderly Korean adults. J. Am. Geriatr. Soc. 2014, 62, 2327–2332. [Google Scholar] [CrossRef] [PubMed]
- Bozkurt, N.C.; Cakal, E.; Sahin, M.; Ozkaya, E.C.; Firat, H.; Delibasi, T. The relation of serum 25-hydroxyvitamin-D levels with severity of obstructive sleep apnea and glucose metabolism abnormalities. Endocrine 2012, 41, 518–525. [Google Scholar] [CrossRef] [PubMed]
- Gominak, S.C.; Stumpf, W.E. The world epidemic of sleep disorders is linked to vitamin D deficiency. Med. Hypotheses 2012, 79, 132–135. [Google Scholar] [CrossRef] [PubMed]
- Gong, Q.H.; Li, S.X.; Li, H.; Chen, Q.; Li, X.Y.; Xu, G.Z. 25-Hydroxyvitamin D Status and Its Association with Sleep Duration in Chinese Schoolchildren. Nutrients 2018, 10, 1013. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gao, Q.; Kou, T.; Zhuang, B.; Ren, Y.; Dong, X.; Wang, Q. The Association between Vitamin D Deficiency and Sleep Disorders: A Systematic Review and Meta-Analysis. Nutrients 2018, 10, 1395. [Google Scholar] [CrossRef] [Green Version]
- Dogan-Sander, E.; Willenberg, A.; Batmaz, I.; Enzenbach, C.; Wirkner, K.; Kohls, E.; Mergl, R.; Thiery, J.; Kratzsch, J.; Hegerl, U.; et al. Association of serum 25-hydroxyvitamin D concentrations with sleep phenotypes in a German community sample. PLoS ONE 2019, 14, e0219318. [Google Scholar] [CrossRef]
- Tohari, A.M.; Alhasani, R.H.; Biswas, L.; Patnaik, S.R.; Reilly, J.; Zeng, Z.; Shu, X. Vitamin D Attenuates Oxidative Damage and Inflammation in Retinal Pigment Epithelial Cells. Antioxidants 2019, 8, 341. [Google Scholar] [CrossRef] [Green Version]
- Lee, V.; Rekhi, E.; Hoh Kam, J.; Jeffery, G. Vitamin D rejuvenates aging eyes by reducing inflammation, clearing amyloid beta and improving visual function. Neurobiol. Aging 2012, 33, 2382–2389. [Google Scholar] [CrossRef]
- Yan, G.; Yu, L.; Jiang, S.; Zhu, J. Melatonin antagonizes oxidative stress-induced mitochondrial dysfunction in retinal pigmented epithelium cells via melatonin receptor 1 (MT1). J. Toxicol. Sci. 2018, 43, 659–669. [Google Scholar] [CrossRef] [Green Version]
- Brennan, R.; Jan, J.E.; Lyons, C.J. Light, dark, and melatonin: Emerging evidence for the importance of melatonin in ocular physiology. Eye 2007, 21, 901–908. [Google Scholar] [CrossRef] [Green Version]
- Anjum, I.; Jaffery, S.S.; Fayyaz, M.; Samoo, Z.; Anjum, S. The Role of Vitamin D in Brain Health: A Mini Literature Review. Cureus 2018, 10, e2960. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trinko, J.R.; Land, B.B.; Solecki, W.B.; Wickham, R.J.; Tellez, L.A.; Maldonado-Aviles, J.; de Araujo, I.E.; Addy, N.A.; DiLeone, R.J. Vitamin D3: A Role in Dopamine Circuit Regulation, Diet-Induced Obesity, and Drug Consumption. eNeuro 2016, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zisapel, N. Melatonin-dopamine interactions: From basic neurochemistry to a clinical setting. Cell Mol. Neurobiol. 2001, 21, 605–616. [Google Scholar] [CrossRef] [PubMed]
- Lips, P. Vitamin D physiology. Prog. Biophys. Mol. Biol. 2006, 92, 4–8. [Google Scholar] [CrossRef]
- Weydert, J.A. Vitamin D in Children’s Health. Children 2014, 1, 208–226. [Google Scholar] [CrossRef] [Green Version]
- Holick, M.F. The Vitamin D deficiency pandemic and consequences for non-skeletal health: Mechanism of action. Mol. Asp. Med. 2008, 29, 362–368. [Google Scholar] [CrossRef] [Green Version]
- Bahrami, A.; Mazloum, S.R.; Maghsoudi, S.; Soleimani, D.; Khayyatzadeh, S.S.; Arekhi, S.; Arya, A.; Mirmoosavi, S.J.; Ferns, G.A.; Bahrami-Taghanaki, H.; et al. High Dose Vitamin D Supplementation Is Associated With a Reduction in Depression Score Among Adolescent Girls: A Nine-Week Follow-Up Study. J. Diet Suppl. 2018, 15, 173–182. [Google Scholar] [CrossRef]
- Aguirre Castaneda, R.; Nader, N.; Weaver, A.; Singh, R.; Kumar, S. Response to vitamin D3 supplementation in obese and non-obese Caucasian adolescents. Horm. Res. Paediatr. 2012, 78, 226–231. [Google Scholar] [CrossRef] [Green Version]
- Dileone, R.J.; Taylor, J.R.; Picciotto, M.R. The drive to eat: Comparisons and distinctions between mechanisms of food reward and drug addiction. Nat. Neurosci. 2012, 15, 1330–1335. [Google Scholar] [CrossRef] [Green Version]
- Macchi, M.M.; Bruce, J.N. Human pineal physiology and functional significance of melatonin. Front. Neuroendocrinol. 2004, 25, 177–195. [Google Scholar] [CrossRef]
- Prietl, B.; Treiber, G.; Pieber, T.R.; Amrein, K. Vitamin D and immune function. Nutrients 2013, 5, 2502–2521. [Google Scholar] [CrossRef]
- Harms, L.R.; Burne, T.H.; Eyles, D.W.; McGrath, J.J. Vitamin D and the brain. Best Pract. Res. Clin. Endocrinol. Metab. 2011, 25, 657–669. [Google Scholar] [CrossRef] [PubMed]
- Tofail, F.; Islam, M.M.; Mahfuz, M.; Ashraful Alam, M.; Aktar, S.; Haque, R.; Hossain, M.I.; Mondal, D.; Petri, W.A.; Ahmed, T. Association of vitamin D nutrition with neurodevelopmental outcome of infants of slums in Bangladesh. PLoS ONE 2019, 14, e022180. [Google Scholar] [CrossRef]
- Blum, K.; Gardner, E.; Oscar-Berman, M.; Gold, M. “Liking” and “wanting” linked to Reward Deficiency Syndrome (RDS): Hypothesizing differential responsivity in brain reward circuitry. Curr. Pharm. Des. 2012, 18, 113–118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cui, X.; Pelekanos, M.; Liu, P.Y.; Burne, T.H.; McGrath, J.J.; Eyles, D.W. The vitamin D receptor in dopamine neurons; its presence in human substantia nigra and its ontogenesis in rat midbrain. Neuroscience 2013, 236, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.J.; Volkow, N.D.; Logan, J.; Pappas, N.R.; Wong, C.T.; Zhu, W.; Netusil, N.; Fowler, J.S. Brain dopamine and obesity. Lancet 2001, 357, 354–357. [Google Scholar] [CrossRef]
- Patrick, R.P.; Ames, B.N. Vitamin D and the omega-3 fatty acids control serotonin synthesis and action, part 2: Relevance for ADHD, bipolar disorder, schizophrenia, and impulsive behavior. FASEB J. 2015, 29, 2207–2222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khullar, A. The Role of Melatonin in the Circadian Rhythm Sleep-Wake Cycle. Psychiatr. Times 2012, 29, 1–5. [Google Scholar]
- Morgenthaler, T.I.; Lee-Chiong, T.; Alessi, C.; Friedman, L.; Aurora, R.N.; Boehlecke, B.; Brown, T.; Chesson, A.L., Jr.; Kapur, V.; Maganti, R.; et al. Standards of Practice Committee of the American Academy of Sleep Medicine. Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. An American Academy of Sleep Medicine report. Sleep 2007, 30, 1445–1459. [Google Scholar] [CrossRef] [Green Version]
- Nabavi, S.M.; Nabavi, S.F.; Sureda, A.; Xiao, J.; Dehpour, A.R.; Shirooie, S.; Silva, A.S.; Baldi, A.; Khan, H.; Daglia, M. Anti-inflammatory effects of Melatonin: A mechanistic review. Crit. Rev. Food Sci. Nutr. 2019, 59 (Suppl. 1), S4–S16. [Google Scholar] [CrossRef]
- Li, Y.; Li, S.; Zhou, Y.; Meng, X.; Zhang, J.J.; Xu, D.P.; Li, H.B. Melatonin for the prevention and treatment of cancer. Oncotarget 2017, 8, 39896–39921. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alvarez-García, V.; González, A.; Alonso-González, C.; Martínez-Campa, C.; Cos, S. Antiangiogenic effects of melatonin in endothelial cell cultures. Microvasc. Res. 2013, 87, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Lockley, S.W.; Arendt, J.; Skene, D.J. Visual impairment and circadian rhythm disorders. Dialogues Clin. Neurosci. 2007, 9, 301–314. [Google Scholar] [PubMed]
- Quera Salva, M.A.; Hartley, S.; Léger, D.; Dauvilliers, Y.A. Non-24-Hour Sleep-Wake Rhythm Disorder in the Totally Blind: Diagnosis and Management. Front. Neurol. 2017, 8, 686. [Google Scholar] [CrossRef] [Green Version]
- Chang, C.C.; Huang, T.Y.; Chen, H.Y.; Huang, T.C.; Lin, L.C.; Chang, Y.J.; Hsia, S.M. Protective Effect of Melatonin against Oxidative Stress-Induced Apoptosis and Enhanced Autophagy in Human Retinal Pigment Epithelium Cells. Oxid. Med. Cell Longev. 2018, 2018, 9015765. [Google Scholar] [CrossRef]
- Cardinali, D.P.; Srinivasan, V.; Brzezinski, A.; Brown, G.M. Melatonin and its analogs in insomnia and depression. J. Pineal Res. 2012, 52, 365–375. [Google Scholar] [CrossRef] [Green Version]
- Auld, F.; Maschauer, E.L.; Morrison, I.; Skene, D.J.; Riha, R.L. Evidence for the efficacy of melatonin in the treatment of primary adult sleep disorders. Sleep Med. Rev. 2017, 34, 10–22. [Google Scholar] [CrossRef]
- Ferris, M.J.; España, R.A.; Locke, J.L.; Konstantopoulos, J.K.; Rose, J.H.; Chen, R.; Jones, S.R. Dopamine transporters govern diurnal variation in extracellular dopamine tone. Proc. Natl. Acad. Sci. USA 2014, 111, E2751–E2759. [Google Scholar] [CrossRef] [Green Version]
- Liu, M.; Luo, J. Relationship between peripheral blood dopamine level and internet addiction disorder in adolescents: A pilot study. Int. J. Clin. Exp. Med. 2015, 8, 9943–9948. [Google Scholar]
- Patrick, R.P.; Ames, B.N. Vitamin D hormone regulates serotonin synthesis. Part 1: Relevance for autism. FASEB J. 2014, 28, 2398–2413. [Google Scholar] [CrossRef] [Green Version]
- Reiter, R.J.; Rosales-Corral, S.; Coto-Montes, A.; Boga, J.A.; Tan, D.X.; Davis, J.M.; Konturek, P.C.; Konturek, S.J.; Brzozowski, T. The photoperiod, circadian regulation and chronodisruption: The requisite interplay between the suprachiasmatic nuclei and the pineal and gut melatonin. J. Physiol. Pharmacol. 2011, 62, 269–274. [Google Scholar] [PubMed]
- Ghareghani, M.; Reiter, R.J.; Zibara, K.; Farhadi, N. Latitude, Vitamin D, Melatonin, and Gut Microbiota Act in Concert to Initiate Multiple Sclerosis: A New Mechanistic Pathway. Front. Immunol. 2018, 9, 2484. [Google Scholar] [CrossRef] [PubMed]
- Paredes, S.D.; Barriga, C.; Reiter, R.J.; Rodríguez, A.B. Assessment of the Potential Role of Tryptophan as the Precursor of Serotonin and Melatonin for the Aged Sleep-wake Cycle and Immune Function: Streptopelia Risoria as a Model. Int. J. Tryptophan Res. 2009, 2, 23–36. [Google Scholar] [CrossRef] [Green Version]
- Homberg, J.R. Serotonin and decision making processes. Neurosci. Biobehav. Rev. 2012, 36, 218–236. [Google Scholar] [CrossRef] [PubMed]
- Pittaras, E.; Callebert, J.; Dorey, R.; Chennaoui, M.; Granon, S.; Rabat, A. Mouse Gambling Task reveals differential effects of acute sleep debt on decision-making and associated neurochemical changes. Sleep 2018, 41, 168. [Google Scholar] [CrossRef] [PubMed]
- Juárez Olguín, H.; Calderón Guzmán, D.; Hernández García, E.; Barragán Mejía, G. The Role of Dopamine and Its Dysfunction as a Consequence of Oxidative Stress. Oxid. Med. Cell Longev. 2016, 2016, 9730467. [Google Scholar] [CrossRef] [Green Version]
- Wood, M.D.; Wren, P.B. Serotonin-dopamine interactions: Implications for the design of novel therapeutic agents for psychiatric disorders. Prog. Brain Res. 2008, 172, 213–230. [Google Scholar]
- Ariatama, B.; Effendy, E.; Amin, M.M. Relationship between Internet Gaming Disorder with Depressive Syndrome and Dopamine Transporter Condition in Online Game Players. Open Access Maced. J. Med. Sci. 2019, 7, 2638–2642. [Google Scholar] [CrossRef] [Green Version]
- Weinstein, A.M. An update overview on brain imaging studies of Internet gaming disorder. Front. Psychiatry 2017, 8, 185. [Google Scholar] [CrossRef]
- Russart, K.L.G.; Nelson, R.J. Light at night as an environmental endocrine disruptor. Physiol. Behav. 2018, 190, 82–89. [Google Scholar] [CrossRef]
- Morin-Major, J.K.; Marin, M.F.; Durand, N.; Wan, N.; Juster, R.P.; Lupien, S.J. Facebook behaviors associated with diurnal cortisol in adolescents: Is befriending stressful? Psychoneuroendocrinology 2016, 63, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Belenchia, A.M.; Tosh, A.K.; Hillman, L.S.; Peterson, C.A. Correcting vitamin D insufficiency improves insulin sensitivity in obese adolescents: A randomized controlled trial. Am. J. Clin. Nutr. 2013, 97, 774–781. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salehi, B.; Sharopov, F.; Fokou, P.V.T.; Kobylinska, A.; Jonge, L.; Tadio, K.; Sharifi-Rad, J.; Posmyk, M.M.; Martorell, M.; Martins, N.; et al. Melatonin in Medicinal and Food Plants: Occurrence, Bioavailability, and Health Potential for Humans. Cells 2019, 8, 681. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brody, J. Screen Addiction is Taking a Toll on Children. The New York Times. 6 July 2019. Available online: https://well.blogs.nytimes.com/2015/07/06/screen-addiction-is-taking-a-toll-on-children/?_r=0 (accessed on 20 April 2020).
- Rosen, L.D.; Lim, A.F.; Felt, J.; Carrier, L.M.; Cheever, N.A.; Lara-Ruiz, J.M.; Mendoza, J.S.; Rokkum, J. Media and technology use predicts ill-being among children, preteens and teenagers independent of the negative health impacts of exercise and eating habits. Comput. Hum. Behav. 2014. [Google Scholar] [CrossRef] [Green Version]
- Pujol, J.; Fenoll, R.; Forns, J.; Harrison, B.J.; Martínez-Vilavella, G.; Macià, D.; Alvarez-Pedrerol, M.; Blanco-Hinojo, L.; González-Ortiz, S.; Deus, J.; et al. Video gaming in school children: How much is enough? Ann. Neurol. 2016, 80, 424–433. [Google Scholar] [CrossRef]
- Drummond, A.; Sauer, J. Video-Games Do Not Negatively Impact Adolescent Academic Performance in Science, Mathematics or Reading. PLoS ONE 2014, 9, e87943. [Google Scholar] [CrossRef] [Green Version]
- Franceschini, S.; Trevisan, P.; Ronconi, L.; Bertoni, S.; Colmar, S.; Double, K.; Facoetti, A.; Gori, S. Action video games improve reading abilities and visual-to-auditory attentional shifting in English-speaking children with dyslexia. Sci. Rep. 2017, 7, e5863. [Google Scholar] [CrossRef] [PubMed]
- Tran, P.; Subrahmanyam, K. Evidence-based guidelines for the informal use of computers by children to promote the development of academic, cognitive and social skills. Ergonomics 2013, 56, 1349–1362. [Google Scholar] [CrossRef]
- Dresp-Langley, B. The communication contract and its ten ground clauses. J Business Ethics 2009, 87, article-415. [Google Scholar] [CrossRef]
- The European Environment Agency. Late Lessons from Early Warnings: The Precautionary Principle 1896–2000; EEA Publications: Copenhagen, Denmark, 2001; Available online: https://www.eea.europa.eu/publications (accessed on 15 January 2020).





© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dresp-Langley, B. Children’s Health in the Digital Age. Int. J. Environ. Res. Public Health 2020, 17, 3240. https://doi.org/10.3390/ijerph17093240
Dresp-Langley B. Children’s Health in the Digital Age. International Journal of Environmental Research and Public Health. 2020; 17(9):3240. https://doi.org/10.3390/ijerph17093240
Chicago/Turabian StyleDresp-Langley, Birgitta. 2020. "Children’s Health in the Digital Age" International Journal of Environmental Research and Public Health 17, no. 9: 3240. https://doi.org/10.3390/ijerph17093240
APA StyleDresp-Langley, B. (2020). Children’s Health in the Digital Age. International Journal of Environmental Research and Public Health, 17(9), 3240. https://doi.org/10.3390/ijerph17093240




