Prevalence of Multimorbidity among Asian Indian, Chinese, and Non-Hispanic White Adults in the United States
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Source
2.3. Analytical Sample
2.4. Measures
2.4.1. Dependent Variable: Presence of Multimorbidity
2.4.2. Key Independent Variable: Race/Ethnicity—Asian Indians, Chinese, and NHWs
2.4.3. Other Independent Variables
2.5. Statistical Analysis
3. Results
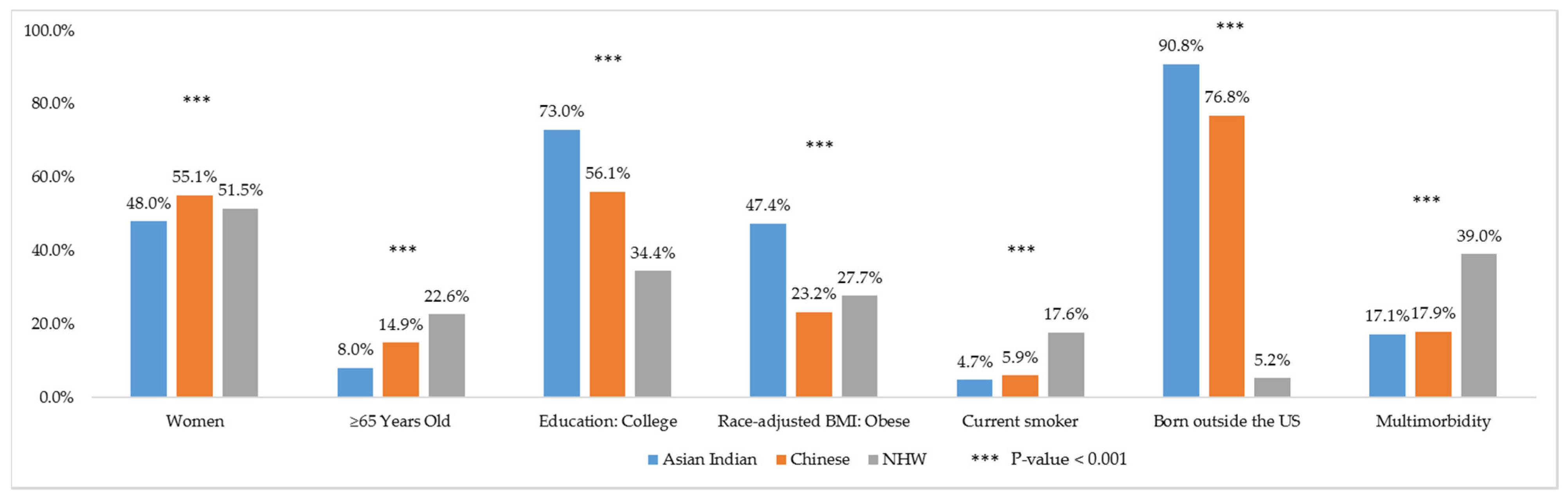
3.1. Description of Characteristics among Asian Indians, Chinese, and NHWs
3.2. Prevalence of Multimorbidity among Asian Indians, Chinese, and NHWs
3.3. Chronic Condition Combinations among Asian Indians, Chinese, and NHWs
3.4. Adjusted Associations of Race/Ethnicity to Multimorbidity
3.5. Asian Indians and Chinese—Comparison of Multimorbidity
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- MacMahon, S.; Calverley, P.; Chaturvedi, N.; Chen, Z.; Corner, L.; Davies, M.; Ezzati, M.; Guthrie, B.; Hanson, K.; Jha, V.; et al. Multimorbidity: A Priority for Global Health Research; The Academy of Medical Sciences: London, UK, 2018. [Google Scholar]
- Publications on Multimorbidity. Available online: https://www.usherbrooke.ca/crmcspl/fileadmin/sites/crmcspl/documents/Publications_on_multimorbidity_01.pdf (accessed on 26 April 2020).
- Hajat, C.; Stein, E. The global burden of multiple chronic conditions: A narrative review. Prev. Med. Rep. 2018, 12, 284–293. [Google Scholar] [CrossRef] [PubMed]
- Cabral, G.G.; Dantas, A.C.; Barbosa, I.R.; Jerez-Roig, J.; Souza, D.L.B. Multimorbidity and Its Impact on Workers: A Review of Longitudinal Studies. Saf. Health Work 2019, 10, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.; Tan, X.; Riley, B.; Zheng, T.; Bias, T.; Sambamoorthi, U. Polypharmacy and Multimorbidity among Medicaid Enrollees: A Multistate Analysis. Popul. Health Manag. 2018, 21, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Menditto, E.; Miguel, A.G.; Juste, A.M.; Plou, B.P.; Pascual-Salcedo, M.A.; Orlando, V.; Rubio, F.G.; Torres, A.P. Patterns of multimorbidity and polypharmacy in young and adult population: Systematic associations among chronic diseases and drugs using factor analysis. PLoS ONE 2019, 14, e0210701. [Google Scholar] [CrossRef]
- Calderón-Larrañaga, A.; Vetrano, D.L.; Ferrucci, L.; Mercer, S.W.; Marengoni, A.; Onder, G.; Eriksdotter, M.; Fratiglioni, L. Multimorbidity and functional impairment–bidirectional interplay, synergistic effects and common pathways. J. Intern. Med. 2019, 285, 255–271. [Google Scholar] [CrossRef]
- Vetrano, D.L.; Palmer, K.; Marengoni, A.; Marzetti, E.; Lattanzio, F.; Roller-Wirnsberger, R.; Lopez Samaniego, L.; Rodríguez-Mañas, L.; Bernabei, R.; Onder, G. Frailty and Multimorbidity: A Systematic Review and Meta-analysis. J. Gerontol. Ser. A 2019, 74, 659–666. [Google Scholar] [CrossRef]
- Makovski, T.T.; Schmitz, S.; Zeegers, M.P.; Stranges, S.; van den Akker, M. Multimorbidity and quality of life: Systematic literature review and meta-analysis. Ageing Res. Rev. 2019, 53, 100903. [Google Scholar] [CrossRef]
- Marengoni, A.; Angleman, S.; Melis, R.; Mangialasche, F.; Karp, A.; Garmen, A.; Meinow, B.; Fratiglioni, L. Aging with multimorbidity: A systematic review of the literature. Ageing Res. Rev. 2011, 10, 430–439. [Google Scholar] [CrossRef]
- Bähler, C.; Huber, C.A.; Brüngger, B.; Reich, O. Multimorbidity, health care utilization and costs in an elderly community-dwelling population: A claims data based observational study. BMC Health Serv. Res. 2015, 15, 23. [Google Scholar] [CrossRef]
- Palladino, R.; Lee, J.T.; Ashworth, M.; Triassi, M.; Millett, C. Associations between multimorbidity, healthcare utilisation and health status: Evidence from 16 European countries. Age Ageing 2016, 45, 431–435. [Google Scholar] [CrossRef]
- Wang, L.; Si, L.; Cocker, F.; Palmer, A.J.; Sanderson, K. A Systematic Review of Cost-of-Illness Studies of Multimorbidity. Appl. Health Econ. Health Policy 2018, 16, 15–29. [Google Scholar] [CrossRef] [PubMed]
- Zulman, D.M.; Chee, C.P.; Wagner, T.H.; Yoon, J.; Cohen, D.M.; Holmes, T.H.; Ritchie, C.; Asch, S.M. Multimorbidity and healthcare utilisation among high-cost patients in the US Veterans Affairs Health Care System. BMJ Open 2015, 5, e007771. [Google Scholar] [CrossRef]
- Nunes, B.P.; Flores, T.R.; Mielke, G.I.; Thumé, E.; Facchini, L.A. Multimorbidity and mortality in older adults: A systematic review and meta-analysis. Arch. Gerontol. Geriatr. 2016, 67, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.; Manolova, G.; Daskalopoulou, C.; Vitoratou, S.; Prince, M.; Prina, A.M. Prevalence of multimorbidity in community settings: A systematic review and meta-analysis of observational studies. J. Comorbidity 2019, 9, 2235042X1987093. [Google Scholar] [CrossRef] [PubMed]
- Van Oostrom, S.H.; Gijsen, R.; Stirbu, I.; Korevaar, J.C.; Schellevis, F.G.; Picavet, H.S.J.; Hoeymans, N. Time Trends in Prevalence of Chronic Diseases and Multimorbidity Not Only due to Aging: Data from General Practices and Health Surveys. PLoS ONE 2016, 11, e0160264. [Google Scholar] [CrossRef]
- Shadmi, E. Disparities in Multiple Chronic Conditions within Populations. J. Comorbidity 2013, 3, 45–50. [Google Scholar] [CrossRef]
- Boutayeb, A.; Boutayeb, S.; Boutayeb, W. Multi-morbidity of non communicable diseases and equity in WHO Eastern Mediterranean countries. Int. J. Equity Health 2013, 12, 60. [Google Scholar] [CrossRef]
- Ofori-Asenso, R.; Chin, K.L.; Curtis, A.J.; Zomer, E.; Zoungas, S.; Liew, D. Recent Patterns of Multimorbidity Among Older Adults in High-Income Countries. Popul. Health Manag. 2019, 22, 127–137. [Google Scholar] [CrossRef]
- Pengpid, S.; Peltzer, K. Multimorbidity in chronic conditions: Public primary care patients in four greater mekong countries. Int. J. Environ. Res. Public Health 2017, 14, 1019. [Google Scholar] [CrossRef]
- Agborsangaya, C.B.; Lau, D.; Lahtinen, M.; Cooke, T.; Johnson, J.A. Multimorbidity prevalence and patterns across socioeconomic determinants: A cross-sectional survey. BMC Public Health 2012, 12, 201. [Google Scholar] [CrossRef]
- Afshar, S.; Roderick, P.J.; Kowal, P.; Dimitrov, B.D.; Hill, A.G. Multimorbidity and the inequalities of global ageing: A cross-sectional study of 28 countries using the World Health Surveys. BMC Public Health 2015, 15, 776. [Google Scholar] [CrossRef] [PubMed]
- Lim, E.; Gandhi, K.; Davis, J.; Chen, J.J. Prevalence of Chronic Conditions and Multimorbidities in a Geographically Defined Geriatric Population With Diverse Races and Ethnicities. J. Aging Health 2018, 30, 421–444. [Google Scholar] [CrossRef] [PubMed]
- Garin, N.; Koyanagi, A.; Chatterji, S.; Tyrovolas, S.; Olaya, B.; Leonardi, M.; Lara, E.; Koskinen, S.; Tobiasz-Adamczyk, B.; Ayuso-Mateos, J.L.; et al. Global Multimorbidity Patterns: A Cross-Sectional, Population-Based, Multi-Country Study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2016, 71, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Pati, S.; Swain, S.; Hussain, M.A.; Van Den Akker, M.; Metsemakers, J.; Knottnerus, J.A.; Salisbury, C. Prevalence and outcomes of multimorbidity in South Asia: A systematic review. BMJ Open 2015, 5, e007235. [Google Scholar] [CrossRef]
- Low, L.L.; Kwan, Y.H.; Ko, M.S.M.; Yeam, C.T.; Lee, V.S.Y.; Tan, W.B.; Thumboo, J. Epidemiologic Characteristics of Multimorbidity and Sociodemographic Factors Associated With Multimorbidity in a Rapidly Aging Asian Country. JAMA Netw. Open 2019, 2, e1915245. [Google Scholar] [CrossRef]
- Bobo, W.V.; Yawn, B.P.; St Sauver, J.L.; Grossardt, B.R.; Boyd, C.M.; Rocca, W.A. Prevalence of Combined Somatic and Mental Health Multimorbidity: Patterns by Age, Sex, and Race/Ethnicity. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2016, 71, 1483–1491. [Google Scholar] [CrossRef]
- Rocca, W.A.; Boyd, C.M.; Grossardt, B.R.; Bobo, W.V.; Finney Rutten, L.J.; Roger, V.L.; Ebbert, J.O.; Therneau, T.M.; Yawn, B.P.; St. Sauver, J.L. Prevalence of Multimorbidity in a Geographically Defined American Population. Mayo Clin. Proc. 2014, 89, 1336–1349. [Google Scholar] [CrossRef]
- Holland, A.T.; Palaniappan, L.P. Problems With the Collection and Interpretation of Asian-American Health Data: Omission, Aggregation, and Extrapolation. Ann. Epidemiol. 2012, 22, 397–405. [Google Scholar] [CrossRef]
- Bloom, B.; Black, L.I. Health of Non-Hispanic Asian Adults: United States, 2010–2014. NCHS Data Brief 2016, 247, 1–8. [Google Scholar]
- Hoeffel, E.M.; Rastogi, S.; Kim, M.O.; Shahid, H. The Asian Population: 2010; U.S. Department of Commerce, Economics and Statistics Administration, U.S. Census Bureau: Washington, DC, USA, 2012.
- Ortman, J.M.; Velkoff, V.A.; Hogan, H. An Aging Nation: The Older Population in the United States; United States Census Bureau, Economics and Statistics Administration, U.S. Department of Commerce: Suitland, MD, USA, 2014.
- U.S. Census Bureau. U.S. Census Bureau 2018 American Community Survey 1-Year Estimates Data Profiles; Table DP05 ACS Demographic and Housing Estimates; U.S. Census Bureau: Hutland Sutherland, MD, USA, 2018.
- U.S. Census Bureau. U.S. Census Bureau 2018 ACS 1-Year Estimates Selected Population Profiles; Table S0201 Selected Population Profile in the United States; U.S. Census Bureau: Hutland Sutherland, MD, USA, 2018.
- Ro, M.J.; Yee, A.K. Out of the shadows: Asian Americans, Native Hawaiians, and Pacific Islanders. Am. J. Public Health 2010, 100, 776–778. [Google Scholar] [CrossRef]
- Islam, N.S.; Khan, S.; Kwon, S.; Jang, D.; Ro, M.; Trinh-Shevrin, C. Methodological issues in the collection, analysis, and reporting of granular data in Asian American populations: Historical challenges and potential solutions. J. Health Care Poor Underserved 2010, 21, 1354–1381. [Google Scholar] [PubMed]
- Protection, P.; Act, A.C. Patient Protection and Affordable Care Act. Public Law 2010, 111, 759–762. [Google Scholar]
- U.S. Department of Health and Human Services. US Department of Health and Human Services Implementation Guidance on Data Collection Standards for Race, Ethnicity, Sex, Primary Language, and Disability Status; U.S. Department of Health and Human Services: Washington, DC, USA, 2010.
- Lochner, K.A.; Cox, C.S. Prevalence of Multiple Chronic Conditions among Medicare Beneficiaries, United States, 2010. Prev. Chronic Dis. 2013, 10, 120137. [Google Scholar] [CrossRef] [PubMed]
- Steiner, C.A.; Friedman, B. Hospital Utilization, Costs, and Mortality for Adults With Multiple Chronic Conditions, Nationwide Inpatient Sample, 2009. Prev. Chronic Dis. 2013, 10, 120292. [Google Scholar] [CrossRef] [PubMed][Green Version]
- St Sauver, J.L.; Boyd, C.M.; Grossardt, B.R.; Bobo, W.V.; Rutten, L.J.F.; Roger, V.L.; Ebbert, J.O.; Therneau, T.M.; Yawn, B.P.; Rocca, W.A. Risk of developing multimorbidity across all ages in an historical cohort study: Differences by sex and ethnicity. BMJ Open 2015, 5, e006413. [Google Scholar] [CrossRef]
- Gordon, N.P.; Lin, T.Y.; Rau, J.; Lo, J.C. Aggregation of Asian-American subgroups masks meaningful differences in health and health risks among Asian ethnicities: An electronic health record based cohort study. BMC Public Health 2019, 19, 1551. [Google Scholar] [CrossRef]
- Johnson-Lawrence, V.; Zajacova, A.; Sneed, R. Education, race/ethnicity, and multimorbidity among adults aged 30–64 in the National Health Interview Survey. SSM Popul. Health 2017, 3, 366–372. [Google Scholar] [CrossRef]
- Ward, B.W.; Schiller, J.S. Prevalence of multiple chronic conditions among US adults: Estimates from the national health interview survey, 2010. Prev. Chronic Dis. 2013, 10, E65. [Google Scholar] [CrossRef]
- Quiñones, A.R.; Botoseneanu, A.; Markwardt, S.; Nagel, C.L.; Newsom, J.T.; Dorr, D.A.; Allore, H.G. Racial/ethnic differences in multimorbidity development and chronic disease accumulation for middle-aged adults. PLoS ONE 2019, 14, e0218462. [Google Scholar] [CrossRef]
- Quiñones, A.R.; Liang, J.; Bennett, J.M.; Xu, X.; Ye, W. How does the trajectory of multimorbidity vary across black, white, and mexican americans in middle and old age? J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2011, 66, 739–749. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention NHIS—About the National Health Interview Survey. Available online: https://www.cdc.gov/nchs/nhis/about_nhis.htm (accessed on 16 December 2019).
- Centers for Disease Control and Prevention NHIS—Race and Hispanic Origin—Historical Context. Available online: https://www.cdc.gov/nchs/nhis/rhoi/rhoi_history.htm (accessed on 16 December 2019).
- Parsons, V.L.; Moriarity, C.; Jonas, K.; Moore, T.F.; Davis, K.E.; Tompkins, L. Design and estimation for the national health interview survey, 2006–2015. Vital Heal. Stat. 2014, 2, 1–53. [Google Scholar]
- Centers for Disease Control and Prevention NHIS—Data, Questionnaires and Related Documentation. Available online: https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm (accessed on 13 March 2020).
- Johnston, M.C.; Crilly, M.; Black, C.; Prescott, G.J.; Mercer, S.W. Defining and measuring multimorbidity: A systematic review of systematic reviews. Eur. J. Public Health 2019, 29, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Goodman, R.A.; Posner, S.F.; Huang, E.S.; Parekh, A.K.; Koh, H.K. Defining and Measuring Chronic Conditions: Imperatives for Research, Policy, Program, and Practice. Prev. Chronic Dis. 2013, 10, 120239. [Google Scholar] [CrossRef]
- Antonovsky, A. Social class, life expectancy and overall mortality. Milbank Mem. Fund Q. 1967, 5, 31–73. [Google Scholar] [CrossRef]
- Adler, N.E.; Boyce, T.; Chesney, M.A.; Cohen, S.; Folkman, S.; Kahn, R.L.; Syme, S.L. Socioeconomic Status and Health: The Challenge of the Gradient. Am. Psychol. 1994, 49, 15. [Google Scholar] [CrossRef] [PubMed]
- House, J.S.; Lepkowski, J.M.; Kinney, A.M.; Mero, R.P.; Kessler, R.C.; Herzog, A.R. The social stratification of aging and health. J. Health Soc. Behav. 1994, 35, 213–234. [Google Scholar] [CrossRef]
- Preston, S.H.; Kitagawa, E.M.; Hauser, P.M. Differential Mortality in the United States: A Study in Socioeconomic Epidemiology. J. Am. Stat. Assoc. 1974, 69, 574. [Google Scholar] [CrossRef]
- Marmot, M. Social determinants of health inequalities. Lancet 2005, 365, 1099–1104. [Google Scholar] [CrossRef]
- Schwandt, H.M.; Coresh, J.; Hindin, M.J. Marital status, hypertension, coronary heart disease, diabetes, and death among African American women and men: Incidence and prevalence in the atherosclerosis risk in communities (ARIC) study participants. J. Fam. Issues 2010, 31, 1211–1229. [Google Scholar] [CrossRef]
- Birk, J.L.; Kronish, I.M.; Moise, N.; Falzon, L.; Yoon, S.; Davidson, K.W. Depression and multimorbidity: Considering temporal characteristics of the associations between depression and multiple chronic diseases. Health Psychol. 2019, 38, 802. [Google Scholar] [CrossRef]
- World Health Organization. Regional Office for the Western Pacific The Asia-Pacific Perspective: Redefining Obesity and Its Treatment; Health Communications Australia: Sydney, Australia, 2000. [Google Scholar]
- Lopez, G.; Ruiz, N.G.; Patten, E. Key facts about Asian Americans. Available online: https://www.pewresearch.org/fact-tank/2017/09/08/key-facts-about-asian-americans/ (accessed on 8 December 2019).
- Centers for Disease Control and Prevention. Variance Estimation and Other Analytic Issues, NHIS 2016–2017; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2018.
- Centers for Disease Control and Prevention. Variance Estimation and Other Analytic Issues, NHIS 2006–2015; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2016.
- Lee, J.W.R.; Brancati, F.L.; Yeh, H.C. Trends in the prevalence of type 2 diabetes in Asians versus whites: Results from the United States National Health Interview Survey, 1997–2008. Diabetes Care 2011, 34, 353–357. [Google Scholar] [CrossRef] [PubMed]
- Misra, R.; Patel, T.; Kotha, P.; Raji, A.; Ganda, O.; Banerji, M.A.; Shah, V.; Vijay, K.; Mudaliar, S.; Iyer, D.; et al. Prevalence of diabetes, metabolic syndrome, and cardiovascular risk factors in US Asian Indians: Results from a national study. J. Diabetes Complicat. 2010, 24, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Machlin, S.R.; Soni, A. Health care expenditures for adults with multiple treated chronic conditions: Estimates from the medical expenditure panel survey, 2009. Prev. Chronic Dis. 2013, 10, E63. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hamilton, T.G. The healthy immigrant (migrant) effect: In search of a better native-born comparison group. Soc. Sci. Res. 2015, 54, 353–365. [Google Scholar] [CrossRef] [PubMed]
- Pathirana, T.I.; Jackson, C.A. Socioeconomic status and multimorbidity: A systematic review and meta-analysis. Aust. N. Z. J. Public Health 2018, 42, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Commodore-Mensah, Y.; Ukonu, N.; Obisesan, O.; Aboagye, J.K.; Agyemang, C.; Reilly, C.M.; Dunbar, S.B.; Okosun, I.S. Length of Residence in the United States is Associated With a Higher Prevalence of Cardiometabolic Risk Factors in Immigrants: A Contemporary Analysis of the National Health Interview Survey. J. Am. Heart Assoc. 2016, 5, e004059. [Google Scholar] [CrossRef]
- Lee, S.; Martinez, G.; Ma, G.X.; Hsu, C.E.; Robinson, E.S.; Bawa, J.; Juon, H.S. Barriers to health care access in 13 Asian American communities. Am. J. Health Behav. 2010, 34, 21–30. [Google Scholar] [CrossRef]
- Becerra, M.B.; Herring, P.; Marshak, H.H.; Banta, J.E. Generational differences in fast food intake among South-Asian Americans: Results from a population-based survey. Prev. Chronic Dis. 2014, 11, E211. [Google Scholar] [CrossRef]
- Unger, J.B.; Reynolds, K.; Shakib, S.; Spruijt-Metz, D.; Sun, P.; Johnson, C.A. Acculturation, physical activity, and fast-food consumption among asian-american and hispanic adolescents. J. Community Health 2004, 29, 467–481. [Google Scholar] [CrossRef]
- O’Keefe, E.L.; DiNicolantonio, J.J.; Patil, H.; Helzberg, J.H.; Lavie, C.J. Lifestyle Choices Fuel Epidemics of Diabetes and Cardiovascular Disease Among Asian Indians. Prog. Cardiovasc. Dis. 2016, 58, 505–513. [Google Scholar] [CrossRef]
- Ardeshna, D.R.; Bob-Manuel, T.; Nanda, A.; Sharma, A.; Skelton IV, W.P.; Skelton, M.; Khouzam, R.N. Asian-Indians: A review of coronary artery disease in this understudied cohort in the United States. Ann. Transl. Med. 2018, 6, 12. [Google Scholar] [CrossRef] [PubMed]
- Misra, R. Immigrant Asian Indians in the U.S.: A Population at Risk for Diabetes and Cardiovascular Disease. Health Educ. 2009, 41, 19–28. [Google Scholar]
- Holland, A.T.; Wong, E.C.; Lauderdale, D.S.; Palaniappan, L.P. Spectrum of Cardiovascular Diseases in Asian-American Racial/Ethnic Subgroups. Ann. Epidemiol. 2011, 21, 608–614. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A. A National Profile of Functional Limitations Among Asian Indians, Chinese, and Filipinos. J. Gerontol. Ser. B 2020, 75, 1021–1029. [Google Scholar] [CrossRef] [PubMed]
- Goodman, R.A.; Ling, S.M.; Briss, P.A.; Parrish, R.G.; Salive, M.E.; Finke, B.S. Multimorbidity Patterns in the United States: Implications for Research and Clinical Practice. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2016, 71, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Aminisani, N.; Stephens, C.; Allen, J.; Alpass, F.; Shamshirgaran, S.M. Socio-demographic and lifestyle factors associated with multimorbidity in New Zealand. Epidemiol. Health 2020, 42, e2020001. [Google Scholar] [CrossRef]
- Nagel, G.; Peter, R.; Braig, S.; Hermann, S.; Rohrmann, S.; Linseisen, J. The impact of education on risk factors and the occurrence of multimorbidity in the EPIC-Heidelberg cohort. BMC Public Health 2008, 8, 384. [Google Scholar] [CrossRef] [PubMed]
- Schiøtz, M.L.; Stockmarr, A.; Høst, D.; Glümer, C.; Frølich, A. Social disparities in the prevalence of multimorbidity—A register-based population study. BMC Public Health 2017, 17, 422. [Google Scholar] [CrossRef]
- National Center for Health Statistics. National Center for Health Statistics 2012 National Health Interview Survey (NHIS) Public Use Data Release: NHIS Survey Description; National Center for Health Statistics: Hayesville, MD, USA, 2013.
- National Center for Health Statistics. National Center for Health Statistics 2013 National Health Interview Survey (NHIS) Public Use Data Release: Survey Description; National Center for Health Statistics: Hayesville, MD, USA, 2014.
- National Center for Health Statistics. National Center for Health Statistics 2014 National Health Interview Survey (NHIS) Public Use Data Release: Survey Description; National Center for Health Statistics: Hayesville, MD, USA, 2015.
- National Center for Health Statistics. National Center for Health Statistics 2015 National Health Interview Survey (NHIS) Public Use Data Release: Survey Description; National Center for Health Statistics: Hayesville, MD, USA, 2016.
- National Center for Health Statistic. National Center for Health Statistics 2016 National Health Interview Survey (NHIS) Public Use Data Release: Survey Description; National Center for Health Statistics: Hayesville, MD, USA, 2017.
- National Center for Health Statistic. National Center for Health Statistics 2017 National Health Interview Survey (NHIS) Public Use Data Release: Survey Description; National Center for Health Statistics: Hayesville, MD, USA, 2018.

| ALL | Asian Indian | Chinese | NHW | p-Value | ||||
|---|---|---|---|---|---|---|---|---|
| N | Wt% | N | Wt% | N | Wt% | |||
| 2297 | 100.0 | 2403 | 100.0 | 127,966 | 100.0 | |||
| Multimorbidity | <0.001 | |||||||
| No (0–1 chronic conditions) | 1946 | 82.9 | 1941 | 82.1 | 73,368 | 61.0 | ||
| Yes (2–3 chronic conditions) | 278 | 14.1 | 372 | 14.9 | 36,360 | 26.8 | ||
| Yes (4+ chronic conditions) | 73 | 3.0 | 90 | 3.0 | 18,238 | 12.2 | ||
| Age in Years | <0.001 | |||||||
| 18–39 | 1376 | 53.5 | 1107 | 42.1 | 37,960 | 33.5 | ||
| 40–49 | 421 | 21.0 | 429 | 21.7 | 18,489 | 16.1 | ||
| 50–64 | 317 | 17.5 | 448 | 21.3 | 35,426 | 27.8 | ||
| ≥65 | 183 | 8.0 | 419 | 14.9 | 36,091 | 22.6 | ||
| Poverty Status | <0.001 | |||||||
| <100% FPL | 253 | 8.2 | 484 | 15.5 | 13,801 | 8.4 | ||
| 100%–<200% FPL | 244 | 10.0 | 311 | 12.3 | 20,102 | 13.7 | ||
| 200%–<400% FPL | 419 | 19.6 | 458 | 18.8 | 34,928 | 26.9 | ||
| ≥400% FPL | 1193 | 54.3 | 917 | 42.9 | 48,655 | 42.7 | ||
| Employment | <0.001 | |||||||
| Employed | 1599 | 68.5 | 1381 | 60.7 | 72,428 | 60.0 | ||
| Not employed | 696 | 31.4 | 1021 | 39.3 | 55,476 | 40.0 | ||
| Health Insurance | 0.177 | |||||||
| Insured | 2102 | 91.6 | 2180 | 91.7 | 116,624 | 91.2 | ||
| Not insured | 188 | 8.1 | 204 | 7.6 | 10,989 | 8.5 | ||
| Marital Status | <0.001 | |||||||
| Married | 1564 | 77.3 | 1263 | 64.1 | 67,217 | 63.5 | ||
| Separated/widowed/divorced | 166 | 5.5 | 322 | 9.0 | 35,667 | 17.9 | ||
| Never married | 564 | 17.2 | 812 | 26.7 | 24,818 | 18.5 | ||
| Doctor’s Office Visit | <0.001 | |||||||
| No visit | 530 | 21.1 | 566 | 21.2 | 18,307 | 14.7 | ||
| 1 visit | 576 | 26.3 | 533 | 24.7 | 21,234 | 17.1 | ||
| 2–3 visits | 620 | 28.3 | 631 | 26.9 | 33,995 | 26.9 | ||
| 4 and more visits | 528 | 22.4 | 631 | 25.7 | 52,422 | 39.7 | ||
| Alcohol Use | <0.001 | |||||||
| Abstained | 1094 | 49.4 | 990 | 41.1 | 18,675 | 14.8 | ||
| Former drinker | 112 | 5.3 | 171 | 6.9 | 20,378 | 14.3 | ||
| Current drinker | 1061 | 43.8 | 1218 | 51.0 | 87,159 | 69.5 | ||
| Physical Activity | <0.001 | |||||||
| Daily | 160 | 6.9 | 112 | 4.8 | 8779 | 7.0 | ||
| Weekly | 983 | 41.3 | 925 | 36.4 | 45,769 | 37.6 | ||
| Monthly/yearly/never/unable | 1129 | 50.4 | 1341 | 57.9 | 71,953 | 54.2 | ||
| Depressive Symptoms | 0.018 | |||||||
| All/most/some of the time | 209 | 8.9 | 219 | 9.2 | 13,477 | 9.8 | ||
| A little/none of the time | 2006 | 86.9 | 2108 | 88.0 | 111,034 | 87.4 | ||
| Region | <0.001 | |||||||
| Northeast | 512 | 24.7 | 587 | 28.5 | 23,151 | 19.0 | ||
| Midwest | 402 | 17.1 | 265 | 10.0 | 33,989 | 27.5 | ||
| South | 753 | 32.0 | 374 | 15.0 | 40,671 | 33.7 | ||
| West | 630 | 26.2 | 1177 | 46.5 | 30,155 | 19.7 | ||
| NHIS Year | 0.003 | |||||||
| 2012 | 404 | 13.3 | 449 | 14.1 | 20,838 | 16.6 | ||
| 2013 | 415 | 14.6 | 458 | 16.2 | 20,795 | 16.6 | ||
| 2014 | 400 | 16.0 | 456 | 16.5 | 23,052 | 16.7 | ||
| 2015 | 417 | 17.6 | 420 | 16.8 | 21,072 | 16.7 | ||
| 2016 | 351 | 20.0 | 329 | 17.3 | 23,370 | 16.7 | ||
| 2017 | 310 | 18.5 | 291 | 19.1 | 18,839 | 16.7 | ||
| ALL | Multimorbidity | No Multimorbidity | p-Value | |||
|---|---|---|---|---|---|---|
| N | Wt% | N | Wt% | |||
| 55,411 | 100% | 77,255 | 100% | |||
| Sex | 0.001 | |||||
| Women | 30,831 | 38.8 | 40,838 | 61.2 | ||
| Men | 24,580 | 37.7 | 36,417 | 62.3 | ||
| Age in Years | <0.001 | |||||
| 18–39 | 4352 | 10.4 | 36,091 | 89.6 | ||
| 40–49 | 5384 | 27.5 | 13,955 | 72.5 | ||
| 50–64 | 18,381 | 49.9 | 17,810 | 50.1 | ||
| ≥65 | 27,294 | 74.3 | 9399 | 25.7 | ||
| Race/Ethnicity | <0.001 | |||||
| Asian Indian | 351 | 17.1 | 1946 | 82.9 | ||
| Chinese | 462 | 17.9 | 1941 | 82.1 | ||
| NHW | 54,598 | 39.0 | 73,368 | 61.0 | ||
| Education | <0.001 | |||||
| Less than high school | 6676 | 51.1 | 4847 | 48.9 | ||
| High school | 15,593 | 43.6 | 16,941 | 56.4 | ||
| Some college | 17,430 | 38.1 | 24,749 | 61.9 | ||
| College | 15,551 | 31.6 | 30,505 | 68.4 | ||
| Poverty Status | <0.001 | |||||
| <100% FPL | 5983 | 38.7 | 8555 | 61.3 | ||
| 100%–<200% FPL | 10,088 | 44.1 | 10,569 | 55.9 | ||
| 200%–<400% FPL | 15,217 | 38.8 | 20,588 | 61.2 | ||
| ≥400% FPL | 19,121 | 35.2 | 31,644 | 64.8 | ||
| Employment | <0.001 | |||||
| Employed | 20,666 | 26.2 | 54,742 | 73.8 | ||
| Not employed | 34,730 | 56.4 | 22,463 | 43.6 | ||
| Health Insurance | <0.001 | |||||
| Insured | 52,624 | 39.7 | 68,282 | 60.3 | ||
| Not insured | 2712 | 22.8 | 8669 | 77.2 | ||
| Marital Status | <0.001 | |||||
| Married | 28,128 | 39.0 | 41,916 | 61.0 | ||
| Separated/widowed/divorced | 21,655 | 58.3 | 14,500 | 41.7 | ||
| Never married | 5528 | 16.8 | 20,666 | 83.2 | ||
| Doctor’s Office Visit | <0.001 | |||||
| No visit | 2740 | 13.0 | 16,663 | 87.0 | ||
| 1 visit | 5396 | 21.1 | 16,947 | 78.9 | ||
| 2–3 visits | 14,113 | 36.3 | 21,133 | 63.7 | ||
| 4 and more visits | 32,253 | 56.8 | 21,328 | 43.2 | ||
| Race-adjusted BMI | < 0.001 | |||||
| Underweight/normal | 14,229 | 26.1 | 33,139 | 73.9 | ||
| Overweight | 18,726 | 39.8 | 24,772 | 60.2 | ||
| Obese | 20,416 | 51.6 | 16,762 | 48.4 | ||
| Smoking | <0.001 | |||||
| Never smoked | 25,912 | 31.8 | 47,308 | 68.2 | ||
| Former smoker | 19,737 | 53.1 | 15,612 | 46.9 | ||
| Current smoker | 9496 | 37.6 | 13,974 | 62.4 | ||
| Alcohol Use | <0.001 | |||||
| Abstained | 8968 | 36.8 | 11,791 | 63.2 | ||
| Former drinker | 12,561 | 57.9 | 8100 | 42.1 | ||
| Current drinker | 33,185 | 34.6 | 56,253 | 65.4 | ||
| Physical Activity | <0.001 | |||||
| Daily | 2906 | 29.2 | 6145 | 70.8 | ||
| Weekly | 13,230 | 26.2 | 34,447 | 73.8 | ||
| Monthly/yearly/never/unable | 38,700 | 47.8 | 35,723 | 52.2 | ||
| Depressive Symptoms | <0.001 | |||||
| All/most/some of the time | 8025 | 54.2 | 5880 | 45.8 | ||
| A little/none of the time | 45,895 | 36.5 | 69,253 | 63.5 | ||
| Region | <0.001 | |||||
| Northeast | 10,385 | 38.0 | 13,865 | 62.0 | ||
| Midwest | 14,416 | 38.0 | 20,240 | 62.0 | ||
| South | 18,155 | 40.1 | 23,643 | 59.9 | ||
| West | 12,455 | 35.6 | 19,507 | 64.4 | ||
| Foreign-Born Status | <0.001 | |||||
| Born in the U.S. | 52,654 | 39.3 | 70,298 | 60.7 | ||
| Born outside the U.S. | 2741 | 26.5 | 6899 | 73.5 | ||
| NHIS Year | <0.001 | |||||
| 2012 | 8716 | 37.7 | 12,975 | 62.3 | ||
| 2013 | 8377 | 36.0 | 13,291 | 64.0 | ||
| 2014 | 10,004 | 38.5 | 13,904 | 61.5 | ||
| 2015 | 9257 | 38.5 | 12,652 | 61.5 | ||
| 2016 | 10,478 | 39.3 | 13,572 | 60.7 | ||
| 2017 | 8579 | 39.4 | 10,861 | 60.6 | ||
| Logistic Regression Model | UOR | 95% CI | p-Value | |
|---|---|---|---|---|
| Model 1—Unadjusted | ||||
| Racial/Ethnic Categories | ||||
| Asian Indian | 0.32 | (0.27, 0.38) | <0.001 | |
| Chinese | 0.34 | (0.30, 0.39) | <0.001 | |
| NHW (Ref) | ||||
| AOR | 95% CI | p-value | ||
| Model 2—adjusted for sex and age | ||||
| Racial/Ethnic Categories | ||||
| Asian Indian | 0.50 | (0.42, 0.59) | <0.001 | |
| Chinese | 0.36 | (0.32, 0.42) | <0.001 | |
| NHW (Ref) | ||||
| Model 3—adjusted for sex, age, education, poverty status, employment status, marital status, health insurance, doctor’s office visit, race-adjusted BMI, physical activity, smoking and alcohol use, depressive symptoms, region, foreign-born status and NHIS year | ||||
| Racial/Ethnic Categories | ||||
| Asian Indian | 0.73 | (0.61, 0.89) | 0.001 | |
| Chinese | 0.63 | (0.53, 0.75) | <0.001 | |
| NHW (Ref) | ||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Y.; Misra, R.; Sambamoorthi, U. Prevalence of Multimorbidity among Asian Indian, Chinese, and Non-Hispanic White Adults in the United States. Int. J. Environ. Res. Public Health 2020, 17, 3336. https://doi.org/10.3390/ijerph17093336
Zhang Y, Misra R, Sambamoorthi U. Prevalence of Multimorbidity among Asian Indian, Chinese, and Non-Hispanic White Adults in the United States. International Journal of Environmental Research and Public Health. 2020; 17(9):3336. https://doi.org/10.3390/ijerph17093336
Chicago/Turabian StyleZhang, Yifan, Ranjita Misra, and Usha Sambamoorthi. 2020. "Prevalence of Multimorbidity among Asian Indian, Chinese, and Non-Hispanic White Adults in the United States" International Journal of Environmental Research and Public Health 17, no. 9: 3336. https://doi.org/10.3390/ijerph17093336
APA StyleZhang, Y., Misra, R., & Sambamoorthi, U. (2020). Prevalence of Multimorbidity among Asian Indian, Chinese, and Non-Hispanic White Adults in the United States. International Journal of Environmental Research and Public Health, 17(9), 3336. https://doi.org/10.3390/ijerph17093336






