Mental and Physical Factors Influencing Wellbeing among South Korean Emergency Workers
Abstract
:1. Introduction
1.1. Background
1.2. Precedents of Positive Emotion, Engagement, Relationship, Meaning, and Achievement (PERMA)
1.3. Consequences of Positive Emotion, Engagement, Relationship, Meaning, and Achievement (PERMA)
2. Materials and Methods
2.1. Sample Data
2.2. Measurement
2.2.1. Post-Traumatic Stress Disorder (PTSD)
2.2.2. Burnout
2.2.3. Depression
2.2.4. Positive Emotion, Engagement, Relationship, Meaning, and Achievement (PERMA)
2.2.5. Quality of Life
2.2.6. Life Satisfaction
2.2.7. Sleep Quality
2.2.8. Statistical Analysis
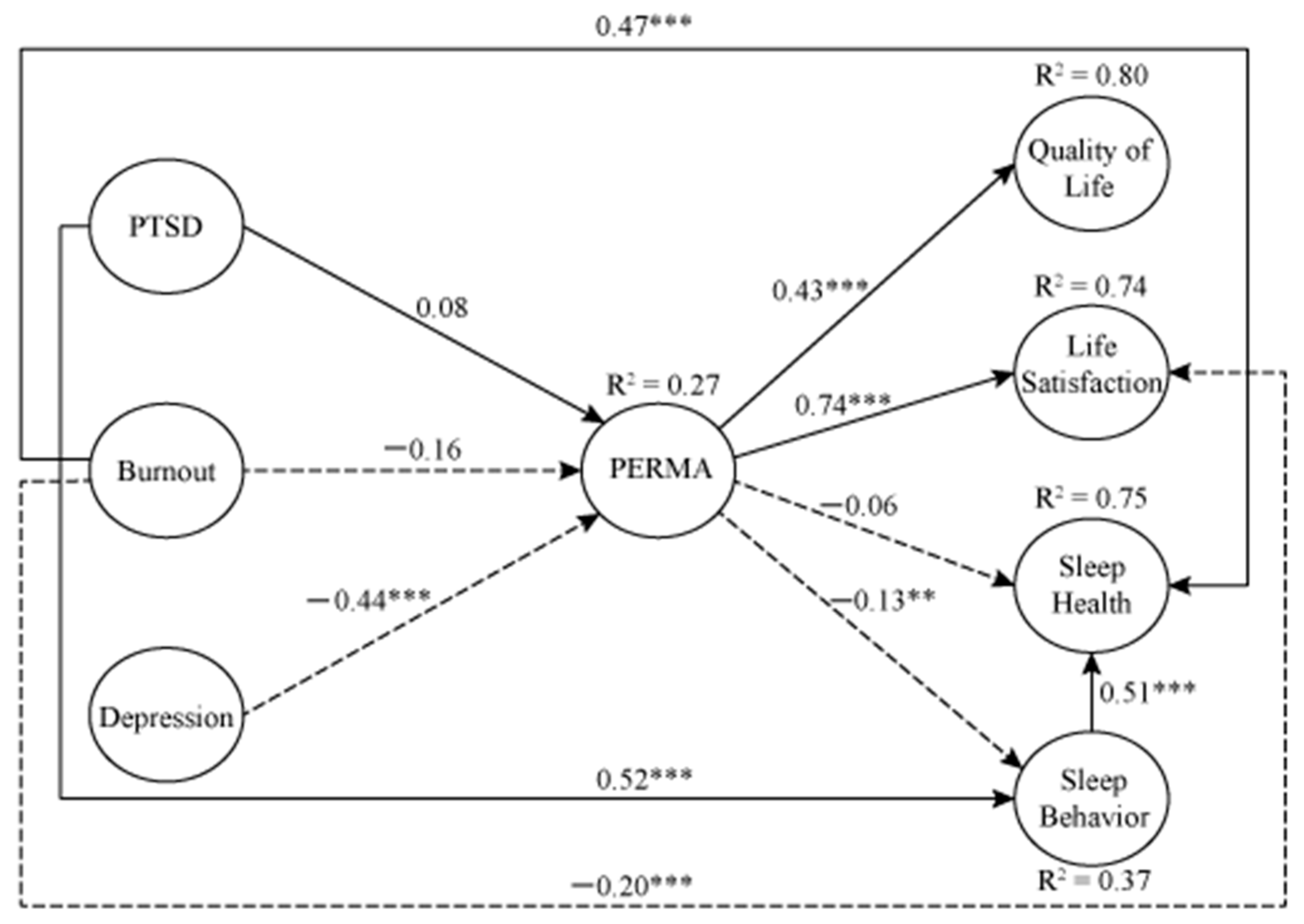
3. Results
4. Discussion
5. Limitations and Suggestions
6. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PTSD | Post-Traumatic Stress Disorder Syndrome |
| PERMA | Positive emotion, Engagement, Relationship, Meaning, and Achievement |
| COVID-19 | Coronavirus Disease 19 |
Appendix A
References
- Boland, L.L.; Kinzy, T.G.; Myers, R.N.; Fernstrom, K.M.; Kamrud, J.W.; Mink, P.J.; Stevens, A.C. Burnout and exposure to critical incidents in a cohort of emergency medical services workers from Minnesota. West. J. Emerg. 2018, 19, 987–995. [Google Scholar] [CrossRef] [PubMed]
- OECD. Korea’s Preparedness for Public Health Emergencies. Available online: https://www.oecd-ilibrary.org/sites/7ba9cad3-en/index.html?itemId=/content/component/7ba9cad3-en (accessed on 4 June 2020).
- Choi, S.K. The View of Emergency Medicine Physicians Over the Korean Emergency Medical System’s Problems and Improvements. Available online: http://pha.or.kr/upload/pdf/pha-3-1-177.pdf (accessed on 20 July 2020).
- Yoon, Y.J.; Hong, S.W. Effects of job stress and burnout on the quality of life among 119 EMTs. J. Korean Soc. Emerg. Med. 2018, 22, 131–148. [Google Scholar] [CrossRef]
- Park, H.J.; Yoon, S.H.; Cho, Y.C. Analysis of the influence of violence experience, burnout and job stress on job satisfaction among 119 rescue workers using the structural equation model. J. Korea Acad. Ind. Coop. Soc. 2018, 19, 267–277. [Google Scholar] [CrossRef]
- Jung, W.Y.; Song, H.S.; Bang, S.H. Effects of a violent experience and job stress on burnout in female 119 emergency medical technicians. J. Korean Soc. Emerg. Med. 2019, 23, 135–143. [Google Scholar] [CrossRef]
- Seligman, M. Flourish: A Visionary New Understanding of Happiness and Well-Being; Free Press: New York, NY, USA, 2011. [Google Scholar]
- Ryan, J.; Curtis, R.; Olds, T.; Edney, S.; Vandelanotte, C.; Plotnikoff, R.; Maher, C. Psychometric properties of the PERMA Profiler for measuring wellbeing in Australian adults. PLoS ONE 2019, 14, e0225932. [Google Scholar] [CrossRef] [Green Version]
- Tansey, T.N.; Smedema, S.; Umucu, E.; Iwanaga, K.; Wu, J.-R.; Cardoso, E.S.; Strauser, D. Assessing college life adjustment of students with disabilities: Application of the PERMA framework. Rehabil. Couns. Bull. 2018, 61, 131–142. [Google Scholar] [CrossRef]
- American Psychiatric Association. What Is Posttraumatic Trauma Disorder? Available online: https://www.psychiatry.org/patients-families/ptsd/what-is-ptsd#:~:text=Posttraumatic%20stress%20disorder%20(PTSD)%20is,sexual%20violence%20or%20serious%20injury (accessed on 3 August 2020).
- Herr, D.J.; Buchanan, E.M. Generativity and other buffers of death awareness in first responders. Anxiety Stress Coping 2020, 33, 193–206. [Google Scholar] [CrossRef]
- Shakespeare-Finch, J.; Rees, A.; Armstrong, D. Social support, self-efficacy, trauma and well-being in emergency medical dispatchers. Soc. Indic. Res. 2015, 123, 549–565. [Google Scholar] [CrossRef]
- Bromet, E.J.; Hobbs, M.J.; Gonzalez, A.; Kotov, R.; Clouston, S.A.P.; Luft, B.J. DSM-IV post-traumatic stress disorder among world trade center responders 11–13 years after the disaster of 11 September 2001 (9/11). Psychol. Med. 2016, 46, 771–783. [Google Scholar] [CrossRef] [Green Version]
- Pines, A.M.; Keinam, G. Stress and burnout in Israeli border police. Int. J. Stress Manag. 2006, 13, 519–540. [Google Scholar] [CrossRef]
- Lee, H.Y.; Kim, Y.R. Effects of burnout on job stress and ego-resilience of fire officials. Fire Sci. Eng. 2017, 31, 106–112. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A.; Beck, J.S.; Newman, C.F. Hopelessness, depression, suicidal ideation, and clinical diagnosis of depression. Suicide Life Threat. Behav. 1993, 23, 139–145. [Google Scholar] [CrossRef] [PubMed]
- The World Health Organization. WHOQOL: Measuring Quality-of-Life; The World Health Organization: Geneva, Switzerland, 1997. [Google Scholar]
- Park, K.S.; Ha, Y.M.; Seo, M.J.; Choi, Y.S.; Kim, M.J.; Jeong, Y.J.; Yang, S.K. Impact of health-related quality of life in firefighters: Focused on posttraumatic stress, health-related work limitations, and family support. Korean J. Occup. Health Nurs. 2017, 26, 142–150. [Google Scholar] [CrossRef]
- Siahpush, M.; Spittal, M.; Singh, G.K. Happiness and life satisfaction prospectively predict self-related health, physical health, and the presence of limiting long-term health conditions. Am. J. Health Promot. 2008, 23, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Butler, J.; Kern, M.L. The PERMA-profiler: A brief multidimensional measure of flourishing. Int. J. Wellbeing 2016, 6, 1–48. [Google Scholar] [CrossRef] [Green Version]
- Morman, M.T.; Schrodt, P.; Adamson, A. Firefighters’ job stress and the (un)intended consequences of relational quality with spouses and firefighter friends. J. Soc. Pers. 2020, 37, 1092–1113. [Google Scholar] [CrossRef]
- Aysan, E.; Karakose, S.; Zaybak, A.; Ismailoglu, E.G. Sleep quality among undergraduate students and influencing factors. J. Dokuz Eylül Univ. S Nurs. 2014, 7, 193–198. [Google Scholar]
- Oh, J.U.; Ko, M.A.; Song, H.R.; Hong, M.H.; Kim, H.S.; Kim, W.J. Factors affecting sleep quality of firefighters. Korean J. Psychosom. Med. 2018, 26, 19–25. [Google Scholar] [CrossRef]
- Lavrakas, P.J. Encyclopedia of Survey Research Methods; Sage Publications, Inc: Thousand Oaks, CA, USA, 2008; Volume 1-0. [Google Scholar] [CrossRef]
- Pett, M.A.; Lackey, N.R.; Sullivan, J.J. Making Sense of Factor Analysis: The Use of Factor Analysis for Instrument Development in Health Care Research; Sage: Thousand Oaks, CA, USA, 2003. [Google Scholar]
- Nunnally, J.C. Psychometric Theory, 2nd ed.; McGraw-Hill: New York, NY, USA, 1978. [Google Scholar]
- Freitas Passos, R.B.; Figueira, I.; Mendlowicz, M.V.; Moraes, C.L.; Freire Coutinho, E.S. Exploratory factor analysis of the Brazilian version of the post-traumatic stress disorder checklist—Civilian version (PCL-C). Rev. Bras. Psychiatry 2012, 34, 155–161. [Google Scholar] [CrossRef]
- García, R.G.; Sangregorio, M.A.; Sánchez, M.L. Factorial validity of the maslach burnout inventory-human services survey (MBI-HSS) in a sample of Spanish social workers. J. Soc. Serv. Res. 2019, 45, 207–219. [Google Scholar] [CrossRef]
- Yildirim, A.; Boysan, M.; Kefeli, M.C. Psychometric properties of the Turkish version of the depression anxiety stress scale-21 (DASS-21). Brit. J. Guid. Couns. 2018, 46, 582–595. [Google Scholar] [CrossRef]
- Umucu, E.; Wu, J.-R.; Sanchez, J.; Brooks, J.M.; Chiu, C.-Y.; Tu, W.-M.; Chan, F. Psychometric validation of the PERMA-profiler as a well-being measure for student veterans. J. Am. Coll. Health 2020, 68, 271–277. [Google Scholar] [CrossRef] [PubMed]
- Perera, H.N.; Izadikhah, Z.; O’Connor, P.; McIlveen, P. Resolving dimensionality problems with WHOQOL-BREF item responses. Assessment 2018, 25, 1014–1025. [Google Scholar] [CrossRef] [PubMed]
- Pavot, W.G.; Diener, E.; Colvin, C.R.; Sandvik, E. Further validation of the satisfaction with life scale: Evidence for the cross-method convergence of well-being measures. J. Pers. Assess. 1991, 57, 149–161. [Google Scholar] [CrossRef]
- Malik, A.A.; Bakarman, M.A.; Butt, N.S. Construct validity and factor structure of the Pittsburgh sleep quality index (PSQI) among physicians in Jeddah, Kingdom of Saudi Arabia. Pak. J. Stat. Op. Res. 2018, 14, 935–943. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Earlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Statistics Korea. Status of Gender Technical Personnel by Professional Field. KOSIS. Available online: http://kosis.kr/statHtml/statHtml.do?orgId=115&tblId=DT_11529_N011 (accessed on 9 March 2020).
- Hu, L.T.; Bentler, P.M. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychol. Methods 1998, 3, 424–453. [Google Scholar] [CrossRef]
- Kang, M.J.; Kim, Y.H.; Han, S.W. A systematic review of the variables related to post-traumatic stress disorder in firefighters. Fire Sci. Eng. 2019, 33, 164–172. [Google Scholar] [CrossRef]
- Biggs, Q.M.; Ursano, R.J.; Wang, J.; Wynn, G.H.; Carr, R.B.; Fullerton, C.S. Posttraumatic stress symptom variation associated with sleep characteristics. BMC Psychiatry 2020, 20, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Short, N.A.; Allan, N.P.; Schmidt, N.B. Sleep disturbance as a predictor of affective functioning and symptom severity among individuals with PTSD: An ecological momentary assessment study. Behav. Res. 2017, 97, 146–153. [Google Scholar] [CrossRef]
- Kim, J.J. Three Out of Ten Emergency Workers Suffer from Sleep Disturbance. Kookmin Daily. Available online: http://news.kmib.co.kr/article/view.asp?arcid=0015238398&code=61111311 (accessed on 10 December 2020).
- Hatt, K. How to Keep PTSD out of Your EMS Agency. EMS1. Available online: https://www.ems1.com/ptsd/articles/how-to-keep-ptsd-out-of-your-ems-agency-sbaqNHdsagI9vkkZ/ (accessed on 10 December 2020).
- DuRousseau, D.R.; Mindlin, G.; Insler, J.; Levin, I.I. Operational study to evaluate music-based neurotraining at improving sleep quality, mood, and daytime function in a first responder population. J. Neurother. 2011, 15, 389–398. [Google Scholar] [CrossRef] [Green Version]
- Eiche, C.; Birkholz, T.; Jobst, E.; Gall, C.; Prottengeier, J. Well-being and PTSD in German emergency medical services—A nationwide cross-sectional survey. PLoS ONE 2019, 14, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Wagstaff, C.; Hings, R.; Larner, R.; Fletcher, D. Psychological resilience’s moderation of the relationship between the frequency of organizational stressors and burnout in athletes and coaches. Sport Psychol. 2018, 32, 178–188. [Google Scholar] [CrossRef] [Green Version]
- Kelly, M.; Soles, R.; Garcia, E.; Kundu, I. Job stress, burnout, work-life balance, well-being, and job satisfaction among pathology residents and fellows. Am. J. Clin. Pathol. 2020, 153, 449–469. [Google Scholar] [CrossRef] [PubMed]
- Almutairi, M.N.; El Mahalli, A.A. Burnout and coping methods among emergency medical services professionals. J. Multidiscip. Health 2020, 271–279. [Google Scholar] [CrossRef] [Green Version]
- Whilmot, R. Avoid Job Burnout with the “PERMA Model” for Happiness: 5 Fitness Tips. Inverse. Available online: https://www.inverse.com/article/54188-how-to-avoid-job-burnout-with-exercise-perma-model-for-happiness (accessed on 15 June 2020).
- Ji, D.H.; Choi, M.S. The comparative study on changes in turnover intention according to the level of burn out and the convergence mediating factors in fire officer. J. Korea Soc. Comput. Inf. 2016, 21, 111–117. [Google Scholar] [CrossRef] [Green Version]
- Shumye, S.; Belayneh, Z.; Mengistu, N. Health-related quality of life and its correlates among people with depression attending outpatient department in Ethiopia: A cross-sectional study. Health Qual. Life Outcomes 2019, 17, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Harvey, S.B.; Milligan-Saville, J.S.; Paterson, H.M.; Harkness, E.L.; Marsh, A.M.; Dobson, M.; Kemp, R.; Bryant, R.A. The mental health of fire-fighters: An examination of the impact of repeated trauma exposure. Aust. N. Z. J. Psychiatry 2016, 50, 649–658. [Google Scholar] [CrossRef]
- Cho, M.; Kwon, S.A.; Hyeon, S.H.; Lee, J.H.; Lee, M.K.; Ryu, S.I. The effect of firefighters’ mental wellbeing on morale. J. Korean Soc. Sec. 2018, 17, 95–112. [Google Scholar]
- Bracken, S.M.; McGilloway, S.; Gallagher, S.; Mitchell, J.T. Life after the emergency services: An exploratory study of wellbeing and quality of life in emergency service retirees. Int. J. Emerg. Ment. Health 2014, 16, 44–51. [Google Scholar] [CrossRef]
- Im, C.H.; Rhee, S.Y. The effects of sleep deprivation on job burnout and well-being: Focusing on mediating roles of sleep deprivation, job satisfaction and job burnout in the JD-R model. J. Organ. Manag. 2013, 37, 1–38. [Google Scholar]
- Chin, M.C. Sleep and wellbeing, now and in the future. Int. J. Env. Res. Public Health 2020, 17, 2883. [Google Scholar] [CrossRef]
- Aufderheide, D.; Gondles, E. The psychology of COVID-19: How to manage your mental health and take back control. Correct. Today 2020, 82, 8–13. [Google Scholar]
- Lee, J.; Walker, T. Managing Stress During COVID-19. EMS World. Available online: https://www.emsworld.com/article/1224326/stress-management-during-covid-19-lee-walker (accessed on 10 June 2020).
- Eacker, A. Well-being definition and measures in medical education. In Medical Professionalism Best Practices: Addressing Burnout and Resilience in Our Profession; Byyny, R.L., Byyny, R., Christensen, S., Fish, J.D., Eds.; Alpha Omega Alpha Honor Medical Society: Aurora, CO, USA, 2020; pp. 91–103. [Google Scholar]
| Item Number | PTSD | Burnout | Depression | PERMA | Quality of Life | Life Satisfaction | Sleep Health | Sleep Behavior |
|---|---|---|---|---|---|---|---|---|
| 1 | 0.878 | 0.842 | 0.904 | 0.864 | 0.703 | 0.920 | 0.806 | |
| 2 | 0.876 | 0.856 | 0.900 | 0.915 | 0.767 | 0.936 | 0.836 | |
| 3 | 0.887 | 0.828 | 0.884 | 0.908 | 0.848 | 0.921 | 0.710 | |
| 4 | 0.897 | 0.827 | 0.901 | 0.894 | 0.852 | 0.875 | 0.730 | |
| 5 | 0.849 | 0.838 | 0.891 | 0.891 | 0.638 | |||
| 6 | 0.831 | 0.835 | 0.878 | 0.717 | ||||
| 7 | 0.851 | 0.814 | 0.873 | 0.642 | ||||
| 8 | 0.857 | 0.806 | 0.910 | 0.736 | ||||
| 9 | 0.853 | 0.640 | ||||||
| 10 | 0.851 | 0.669 | ||||||
| 11 | 0.845 | 0.681 | ||||||
| 12 | 0.816 | |||||||
| Eigenvalue | 5.99 | 8.35 | 3.21 | 6.36 | 2.52 | 4.12 | 5.64 | 1.08 |
| Variance Explained | 74.99 | 69.62 | 80.47 | 79.53 | 63.14 | 82.56 | 51.29 | 9.87 |
| KMO | 0.933 | 0.953 | 0.855 | 0.949 | 0.647 | 0.897 | 0.906 | 0.906 |
| Bartlett’s test (X2) | 4631.63 | 6628.01 | 1715.37 | 5207.48 | 1131.42 | 2926.08 | 3338.89 | 3338.89 |
| Degrees of Freedom | 28 | 66 | 6 | 28 | 6 | 10 | 55 | 55 |
| p value | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Cronbach’s Alpha | 0.95 | 0.96 | 0.92 | 0.96 | 0.79 | 0.94 | 0.87 | 0.83 |
| Variable | N | % |
|---|---|---|
| Gender | ||
| Male | 524 | 87.8 |
| Female | 73 | 12.2 |
| Age | ||
| 20s | 84 | 14.1 |
| 30s | 360 | 60.3 |
| 40s | 109 | 18.3 |
| 50s | 42 | 7.0 |
| Over 60 | 2 | 0.3 |
| Education | ||
| Under Middle School | 12 | 2.0 |
| High School | 0 | 0.0 |
| 2-Year College | 423 | 70.9 |
| 4-Year College | 157 | 26.3 |
| Graduate School | 5 | 0.8 |
| Position | ||
| Rescuers | 27 | 4.5 |
| Paramedics | 443 | 74.2 |
| Firefighters | 87 | 14.6 |
| Administration | 36 | 6.0 |
| Training | 4 | 0.7 |
| Annual Income ($) | ||
| Under 20,000 | 0 | 0.0 |
| 20,001–30,000 | 0 | 0.0 |
| 30,001–40,000 | 140 | 23.5 |
| 40,001–50,000 | 256 | 42.9 |
| 50,001–60,000 | 135 | 22.6 |
| 60,001–70,000 | 54 | 9.0 |
| Over 70,000 | 12 | 2.0 |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1. PTSD | ||||||||
| 2. Burnout | 0.79 *** | |||||||
| 3. Depression | 0.76 *** | 0.85 *** | ||||||
| 4. PERMA | −0.39 *** | −0.46 *** | −0.49 *** | |||||
| 5. Quality of Life | −0.36 *** | −0.42 *** | −0.42 *** | 0.68 *** | ||||
| 6. Life Satisfaction | −0.41 *** | −0.51 *** | −0.49 *** | 0.78 *** | 0.67 *** | |||
| 7. Sleep Health | 0.65 *** | 0.66 *** | 0.65 *** | −0.40 *** | −0.37 *** | −0.40 *** | ||
| 8. Sleep Behavior | 0.53 *** | 0.56 *** | 0.49 *** | −0.33 *** | −0.35 *** | −0.41 *** | 0.69 *** | |
| Mean | 1.86 | 1.92 | 1.65 | 3.73 | 3.62 | 3.51 | 1.98 | 2.61 |
| Standard Deviation | 0.95 | 0.88 | 0.79 | 0.86 | 0.86 | 0.92 | 0.78 | 0.99 |
| Skewness | 1.07 | 0.84 | 1.28 | −0.68 | −0.27 | −0.25 | 0.62 | 0.21 |
| Kurtosis | 0.40 | 0.06 | 1.39 | 0.79 | 0.04 | −0.26 | 0.02 | −0.54 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, M.Y. Mental and Physical Factors Influencing Wellbeing among South Korean Emergency Workers. Int. J. Environ. Res. Public Health 2021, 18, 70. https://doi.org/10.3390/ijerph18010070
Choi MY. Mental and Physical Factors Influencing Wellbeing among South Korean Emergency Workers. International Journal of Environmental Research and Public Health. 2021; 18(1):70. https://doi.org/10.3390/ijerph18010070
Chicago/Turabian StyleChoi, Mi Young. 2021. "Mental and Physical Factors Influencing Wellbeing among South Korean Emergency Workers" International Journal of Environmental Research and Public Health 18, no. 1: 70. https://doi.org/10.3390/ijerph18010070
APA StyleChoi, M. Y. (2021). Mental and Physical Factors Influencing Wellbeing among South Korean Emergency Workers. International Journal of Environmental Research and Public Health, 18(1), 70. https://doi.org/10.3390/ijerph18010070





