Acute Responses of Core Muscle Activity during Bridge Exercises on the Floor vs. the Suspension System
Abstract
1. Introduction
2. Materials and Methods
2.1. Experimental Approach to the Problem
2.2. Participants
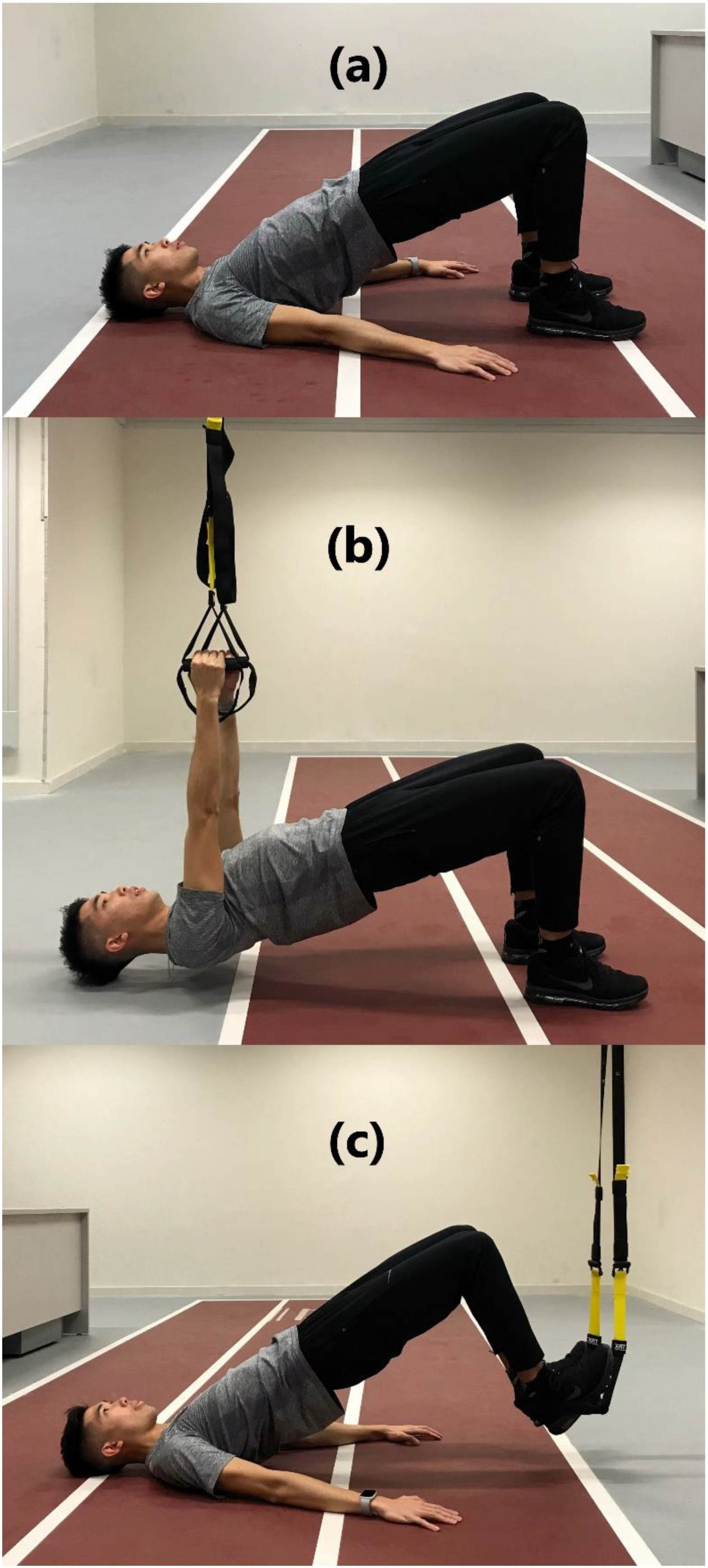
2.3. Procedures
2.4. Statistical Analysis
3. Results
4. Discussion
5. Practical Applications and Study Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kibler, W.B.; Press, J.; Sciascia, A. The role of core stability in athletic function. Sports Med. 2006, 36, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Snarr, R.L.; Esco, M.R. Electromyographical comparison of plank variations performed with and without instability devices. J. Strength Cond. Res. 2014, 28, 3298–3305. [Google Scholar] [CrossRef] [PubMed]
- Hirashima, M.; Kadota, H.; Sakurai, S.; Kudo, K.; Ohtsuki, T. Sequential muscle activity and its functional role in the upper extremity and trunk during overarm throwing. J. Sports Sci. 2002, 20, 301–310. [Google Scholar] [CrossRef] [PubMed]
- Escamilla, R.F.; Lewis, C.; Bell, D.; Bramblet, G.; Daffron, J.; Lambert, S.; Pecson, A.; Imamura, R.; Paulos, L.; Andrews, J.R. Core muscle activation during Swiss ball and traditional abdominal exercises. J. Orthop. Sports Phys. Ther. 2010, 40, 265–276. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.Q.; Zheng, J.J.; Yu, Z.W.; Bi, X.; Lou, S.J.; Liu, J.; Cai, B.; Hua, Y.H.; Wu, M.; Wei, M.L.; et al. A meta-analysis of core stability exercise versus general exercise for chronic low back pain. PLoS ONE 2012, 7, e52082. [Google Scholar] [CrossRef]
- Leetun, D.T.; Ireland, M.L.; Willson, J.D.; Ballantyne, B.T.; Davis, I.M. Core stability measures as risk factors for lower extremity injury in athletes. Med. Sci. Sports Exerc. 2004, 36, 926–934. [Google Scholar] [CrossRef] [PubMed]
- Nelson, N. Diaphragmatic Breathing: The Foundation of Core Stability. Strength Cond. J. 2012, 34, 34–40. [Google Scholar] [CrossRef]
- Bird, S.P.; Stuart, W. Integrating Balance and Postural Stability Exercises into the Functional Warm-up for Youth Athletes. Strength Cond. J. 2012, 34, 73–79. [Google Scholar] [CrossRef]
- Magnus, C.R.; Farthing, J.P. Greater bilateral deficit in leg press than in handgrip exercise might be linked to differences in postural stability requirements. Appl. Physiol. Nutr. Metab. 2008, 33, 1132–1139. [Google Scholar] [CrossRef]
- Ekstrom, R.A.; Donatelli, R.A.; Carp, K.C. Electromyographic analysis of core trunk, hip, and thigh muscles during 9 rehabilitation exercises. J. Orthop. Sports Phys. Ther. 2007, 37, 754–762. [Google Scholar] [CrossRef] [PubMed]
- Atkins, S.J.; Bentley, I.; Brooks, D.; Burrows, M.P.; Hurst, H.T.; Sinclair, J.K. Electromyographic response of global abdominal stabilizers in response to stable- and unstable-base isometric exercise. J. Strength Cond. Res. 2015, 29, 1609–1615. [Google Scholar] [CrossRef] [PubMed]
- Behm, D.; Colado, J.C. The effectiveness of resistance training using unstable surfaces and devices for rehabilitation. Int. J. Sports Phys. Ther. 2012, 7, 226–241. [Google Scholar] [PubMed]
- Marshall, P.W.; Desai, I. Electromyographic analysis of upper body, lower body, and abdominal muscles during advanced Swiss ball exercises. J. Strength Cond. Res. 2010, 24, 1537–1545. [Google Scholar] [CrossRef] [PubMed]
- Wirth, B.; Zurfluh, S.; Muller, R. Acute effects of whole-body vibration on trunk muscles in young healthy adults. J. Electromyogr. Kinesiol. 2011, 21, 450–457. [Google Scholar] [CrossRef]
- Byrne, J.M.; Bishop, N.S.; Caines, A.M.; Crane, K.A.; Feaver, A.M.; Pearcey, G.E. Effect of using a suspension training system on muscle activation during the performance of a front plank exercise. J. Strength Cond. Res. 2014, 28, 3049–3055. [Google Scholar] [CrossRef]
- Tinto, A.; Campanella, M.; Fasano, M. Core strengthening and synchronized swimming: TRX(R) suspension training in young female athletes. J. Sports Med. Phys. Fit. 2017, 57, 744–751. [Google Scholar] [CrossRef]
- Ma, X.; Sun, W.; Lu, A.; Ma, P.; Jiang, C. The improvement of suspension training for trunk muscle power in Sanda athletes. J. Exerc. Sci. Fit. 2017, 15, 81–88. [Google Scholar] [CrossRef]
- Andrejeva, J.; Kasradze, M.; Mockiene, A.; Radziuviene, R.; Zakharchuk, J. Impact of TRX suspension training on patients’ balance, coordination and quality of life after traumatic brain injury. Georgian Med. News 2020, 298, 119–122. [Google Scholar]
- Gaedtke, A.; Morat, T. TRX Suspension Training: A New Functional Training Approach for Older Adults—Development, Training Control and Feasibility. Int. J. Exerc. Sci. 2015, 8, 224–233. [Google Scholar]
- Harris, S.; Ruffin, E.; Brewer, W.; Ortiz, A. Muscle activation patterns during suspension training exercises. Int. J. Sports Phys. Ther. 2017, 12, 42–52. [Google Scholar] [CrossRef]
- Aguilera-Castells, J.; Busca, B.; Fort-Vanmeerhaeghe, A.; Montalvo, A.M.; Pena, J. Muscle activation in suspension training: A systematic review. Sports Biomech. 2020, 19, 55–75. [Google Scholar] [CrossRef] [PubMed]
- Calatayud, J.; Casana, J.; Martin, F.; Jakobsen, M.D.; Colado, J.C.; Gargallo, P.; Juesas, A.; Munoz, V.; Andersen, L.L. Trunk muscle activity during different variations of the supine plank exercise. Musculoskelet. Sci. Pract. 2017, 28, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Jeong, K.; Lee, H.; Shin, J.; Choi, J.; Kang, S.; Lee, B.-H. Comparison of three different surface plank exercises on core muscle activity. Phys. Ther. Rehabil. Sci. 2016, 5, 29–33. [Google Scholar] [CrossRef]
- Schoffstall, J.E.; Titcomb, D.A.; Kilbourne, B.F. Electromyographic response of the abdominal musculature to varying abdominal exercises. J. Strength Cond. Res. 2010, 24, 3422–3426. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.; Yu, J.; Kang, H. Differences in Trunk Muscle Activities and Ratios between Unstable Supine and Prone Bridging Exercises in Individuals with Low Back Pain. J. Phys. Ther. Sci. 2012, 24, 889–892. [Google Scholar] [CrossRef][Green Version]
- Lehman, G.J.; Hoda, W.; Oliver, S. Trunk muscle activity during bridging exercises on and off a Swiss ball. Chiropr. Osteopathy 2005, 13, 14. [Google Scholar] [CrossRef] [PubMed]
- Stevens, V.K.; Bouche, K.G.; Mahieu, N.N.; Coorevits, P.L.; Vanderstraeten, G.G.; Danneels, L.A. Trunk muscle activity in healthy subjects during bridging stabilization exercises. BMC Musculoskelet. Disord. 2006, 7, 75. [Google Scholar] [CrossRef]
- Drysdale, C.L.; Earl, J.E.; Hertel, J. Surface Electromyographic Activity of the Abdominal Muscles During Pelvic-Tilt and Abdominal-Hollowing Exercises. J. Athl. Train. 2004, 39, 32–36. [Google Scholar] [PubMed]
- Ershad, N.; Kahrizi, S.; Abadi, M.F.; Zadeh, S.F. Evaluation of trunk muscle activity in chronic low back pain patients and healthy individuals during holding loads. J. Back Musculoskelet. Rehabil. 2009, 22, 165–172. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. Declaration of Helsinki: Ethical principles for medical research involving human subjects. J. Am. Coll. Dent. 2014, 81, 14–18. [Google Scholar]
- Danneels, L.A.; Coorevits, P.L.; Cools, A.M.; Vanderstraeten, G.G.; Cambier, D.C.; Witvrouw, E.E.; De, C.H. Differences in electromyographic activity in the multifidus muscle and the iliocostalis lumborum between healthy subjects and patients with sub-acute and chronic low back pain. Eur. Spine J. 2002, 11, 13–19. [Google Scholar] [CrossRef]
- Hibbs, A.E.; Thompson, K.G.; French, D.N.; Hodgson, D.; Spears, I.R. Peak and average rectified EMG measures: Which method of data reduction should be used for assessing core training exercises? J. Electromyogr. Kinesiol. 2011, 21, 102–111. [Google Scholar] [CrossRef] [PubMed]
- Cram, J.R. Introduction to Surface Electromyography; Aspen Publishers: Gaithersburg, MD, USA, 1998. [Google Scholar]
- Norwood, J.T.; Anderson, G.S.; Gaetz, M.B.; Twist, P.W. Electromyographic activity of the trunk stabilizers during stable and unstable bench press. J. Strength Cond. Res. 2007, 21, 343–347. [Google Scholar] [CrossRef] [PubMed]
- Beith, I.D.; Synnott, R.E.; Newman, S.A. Abdominal muscle activity during the abdominal hollowing manoeuvre in the four point kneeling and prone positions. Man. Ther. 2001, 6, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Westing, S.H.; Cresswell, A.G.; Thorstensson, A. Muscle activation during maximal voluntary eccentric and concentric knee extension. Eur. J. Appl. Physiol. Occup. Physiol. 1991, 62, 104–108. [Google Scholar] [CrossRef]
- Kendall, F.P. Muscles, Testing and Function: With Posture and Pain, 5th ed.; Lippincott Williams & Wilkins: Baltimore, MD, USA, 2005. [Google Scholar]
- Arokoski, J.P.; Kankaanpaa, M.; Valta, T.; Juvonen, I.; Partanen, J.; Taimela, S.; Lindgren, K.A.; Airaksinen, O. Back and hip extensor muscle function during therapeutic exercises. Arch. Phys. Med. Rehabil. 1999, 80, 842–850. [Google Scholar] [CrossRef]
- Digiovine, N.M.; Jobe, F.W.; Pink, M.; Perry, J. An electromyographic analysis of the upper extremity in pitching. J. Shoulder Elb. Surg. 1992, 1, 15–25. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Portney, L. Foundations of Clinical Research Applications to Practice, 3rd ed.; Pearson/Prentice Hall: Upper Saddle River, NJ, USA, 2015. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; L. Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Imai, A.; Kaneoka, K.; Okubo, Y.; Shiina, I.; Tatsumura, M.; Izumi, S.; Shiraki, H. Trunk muscle activity during lumbar stabilization exercises on both a stable and unstable surface. J. Orthop. Sports Phys. Ther. 2010, 40, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Mathiassen, S.E.; Winkel, J.; Hägg, G.M. Normalization of surface EMG amplitude from the upper trapezius muscle in ergonomic studies—A review. J. Electromyogr. Kinesiol. 1995, 5, 197–226. [Google Scholar] [CrossRef]
- DeLuca, C.J. The use of surface electromyography in biomechanics. J. Appl. Biomech. 1997, 13, 135–163. [Google Scholar] [CrossRef]
- Anderson, T.; Kearney, J.T. Effects of three resistance training programs on muscular strength and absolute and relative endurance. Res. Q. Exerc. Sport 1982, 53, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Gettman, L.R.; Ayres, J.J.; Pollock, M.L.; Jackson, A. The effect of circuit weight training on strength, cardiorespiratory function, and body composition of adult men. Med. Sci. Sports 1978, 10, 171–176. [Google Scholar] [PubMed]
- Sale, D.G.; Jacobs, I.; MacDougall, J.D.; Garner, S. Comparison of two regimens of concurrent strength and endurance training. Med. Sci. Sports Exerc. 1990, 22, 348–356. [Google Scholar] [CrossRef] [PubMed]
- Calatayud, J.; Borreani, S.; Colado, J.C.; Martin, F.F.; Rogers, M.E.; Behm, D.G.; Andersen, L.L. Muscle Activation during Push-Ups with Different Suspension Training Systems. J. Sports Sci. Med. 2014, 13, 502–510. [Google Scholar] [PubMed]


| Variations | Pronecon | Prone-Feetsuspension | Prone-Armsuspension | Supinecon | Supine-Feetsuspension | Supine-Armsuspension |
|---|---|---|---|---|---|---|
| RA | 0.8 | 0.81 | 0.97 | 0.84 | 0.94 | 0.91 |
| RF | 0.87 | 0.85 | 0.9 | 0.86 | 0.9 | 0.87 |
| TES | 0.9 | 0.75 | 0.91 | 0.94 | 0.89 | 0.88 |
| LM | 0.89 | 0.8 | 0.69 | 0.88 | 0.92 | 0.77 |
| GM | 0.82 | 0.56 | 0.75 | 0.81 | 0.89 | 0.92 |
| BF | 0.93 | 0.87 | 0.8 | 0.81 | 0.9 | 0.86 |
| Muscle | Pronecon | Prone-Feetsuspension | Prone-Armsuspension | Supinecon | Supine-Feetsuspension | Supine-Armsuspension | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | 95% CI | Mean ± SD | 95% CI | Mean ± SD | 95% CI | Mean ± SD | 95% CI | Mean ± SD | 95% CI | Mean ± SD | 95% CI | |
| RA # | 26.9 ± 15.1 | 22.3, 31.6 | 48.3 ± 24.3 | 40.8, 55.7 | 136.7 ± 77.7 | 112.8, 160.6 | 2.2 ± 1.8 | 1.6, 2.7 | 4.3 ± 4.2 | 3.0, 5.6 | 2.4 ± 1.3 | 2.0, 2.7 |
| RF * | 19.9 ± 9.5 | 17.0, 22.8 | 27.2 ± 12.9 | 23.2, 31.2 | 40.2 ± 20.1 | 34.0, 46.4 | 2.0 ± 1.1 | 1.7, 2.4 | 3.2 ± 1.8 | 2.6, 3.7 | 2.3 ± 1.3 | 1.9, 2.7 |
| TES * | 4.2 ± 1.5 | 3.8, 4.7 | 6.2 ± 2.4 | 5.4, 6.9 | 9.3 ± 4.7 | 7.9, 10.7 | 34.8 ± 14.1 | 30.4, 39.1 | 49.3 ± 16.7 | 44.2, 54.5 | 38.7 ± 13.6 | 34.5, 42.9 |
| LM * | 3.6 ± 1.9 | 3.0, 4.2 | 5.5 ± 2.6 | 4.7, 6.3 | 9.9 ± 5.0 | 8.4, 11.5 | 45.3 ± 18.3 | 39.7, 51.0 | 53.6 ± 19.6 | 47.6, 59.6 | 46.7 ± 15.9 | 41.8, 51.6 |
| GM &^# | 1.9 ± 2.7 | 1.1, 2.7 | 2.6 ± 3.0 | 1.7, 3.6 | 3.3 ± 1.6 | 2.9, 3.8 | 21.7 ± 7.3 | 19.5, 24.0 | 12.9 ± 6.7 | 10.8, 14.9 | 20.0 ± 9.6 | 17.0, 23.0 |
| BF ^ | 3.6 ± 2.8 | 2.7, 4.4 | 5.4 ± 4.3 | 4.0, 6.7 | 6.3 ± 4.0 | 5.1, 7.6 | 21.4 ± 13.2 | 17.3, 25.5 | 64.3 ± 27.2 | 56.0, 72.7 | 27.8 ± 14.1 | 23.4, 32.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luk, J.T.C.; Kwok, F.K.C.; Ho, I.M.K.; Wong, D.P. Acute Responses of Core Muscle Activity during Bridge Exercises on the Floor vs. the Suspension System. Int. J. Environ. Res. Public Health 2021, 18, 5908. https://doi.org/10.3390/ijerph18115908
Luk JTC, Kwok FKC, Ho IMK, Wong DP. Acute Responses of Core Muscle Activity during Bridge Exercises on the Floor vs. the Suspension System. International Journal of Environmental Research and Public Health. 2021; 18(11):5908. https://doi.org/10.3390/ijerph18115908
Chicago/Turabian StyleLuk, Jim T. C., Freeman K. C. Kwok, Indy M. K. Ho, and Del P. Wong. 2021. "Acute Responses of Core Muscle Activity during Bridge Exercises on the Floor vs. the Suspension System" International Journal of Environmental Research and Public Health 18, no. 11: 5908. https://doi.org/10.3390/ijerph18115908
APA StyleLuk, J. T. C., Kwok, F. K. C., Ho, I. M. K., & Wong, D. P. (2021). Acute Responses of Core Muscle Activity during Bridge Exercises on the Floor vs. the Suspension System. International Journal of Environmental Research and Public Health, 18(11), 5908. https://doi.org/10.3390/ijerph18115908







