A Cumulative Framework for Identifying Overburdened Populations under the Toxic Substances Control Act: Formaldehyde Case Study
Abstract
:1. Introduction
2. Statutory Context
Identification of PESS under TSCA
3. Case Study Demonstration with Formaldehyde
3.1. Methods and Approach
3.2. Identification of Populations with Potential for Greater Exposure to Formaldehyde
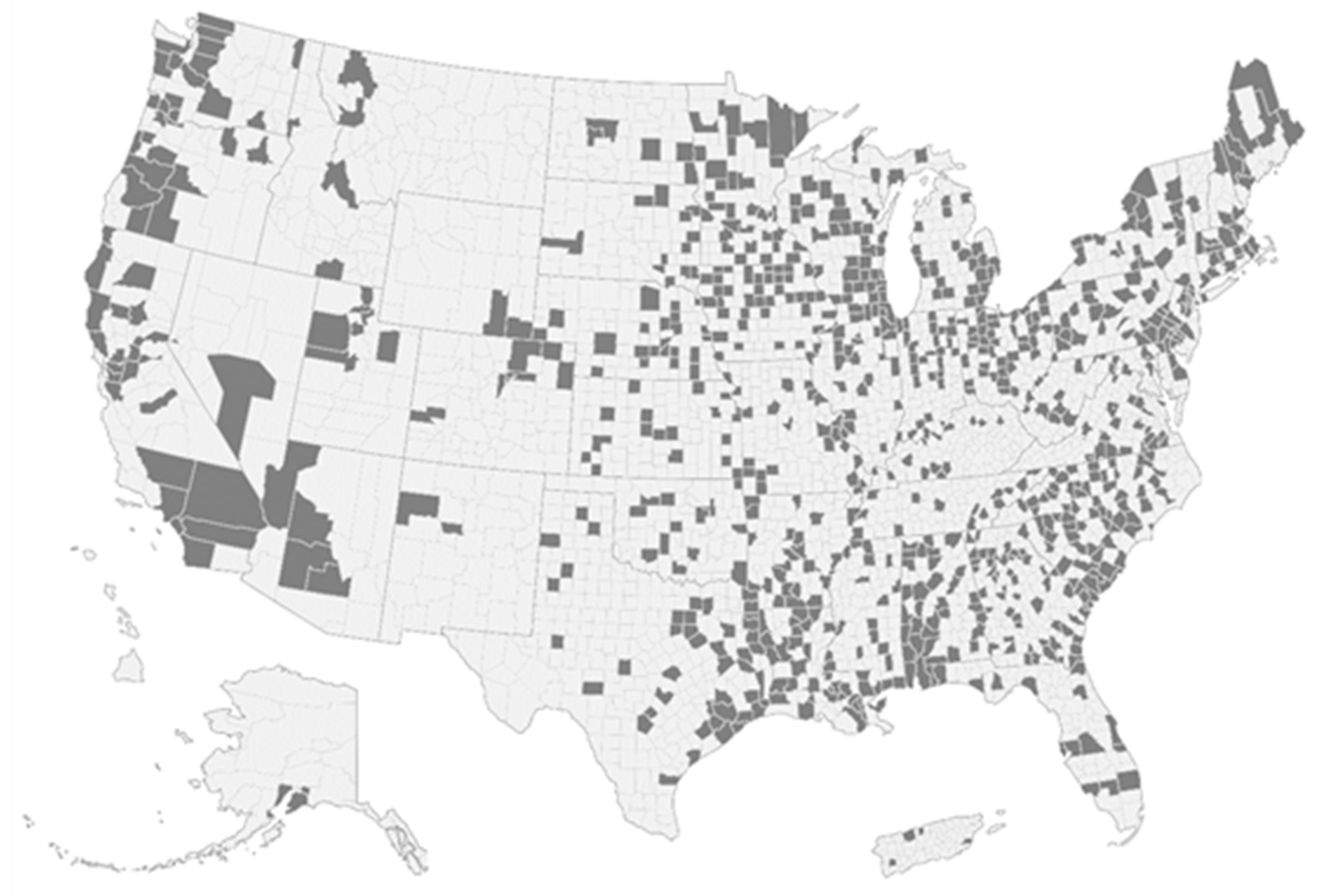
3.2.1. Increased Exposure to Formaldehyde from Far-Field Exposures
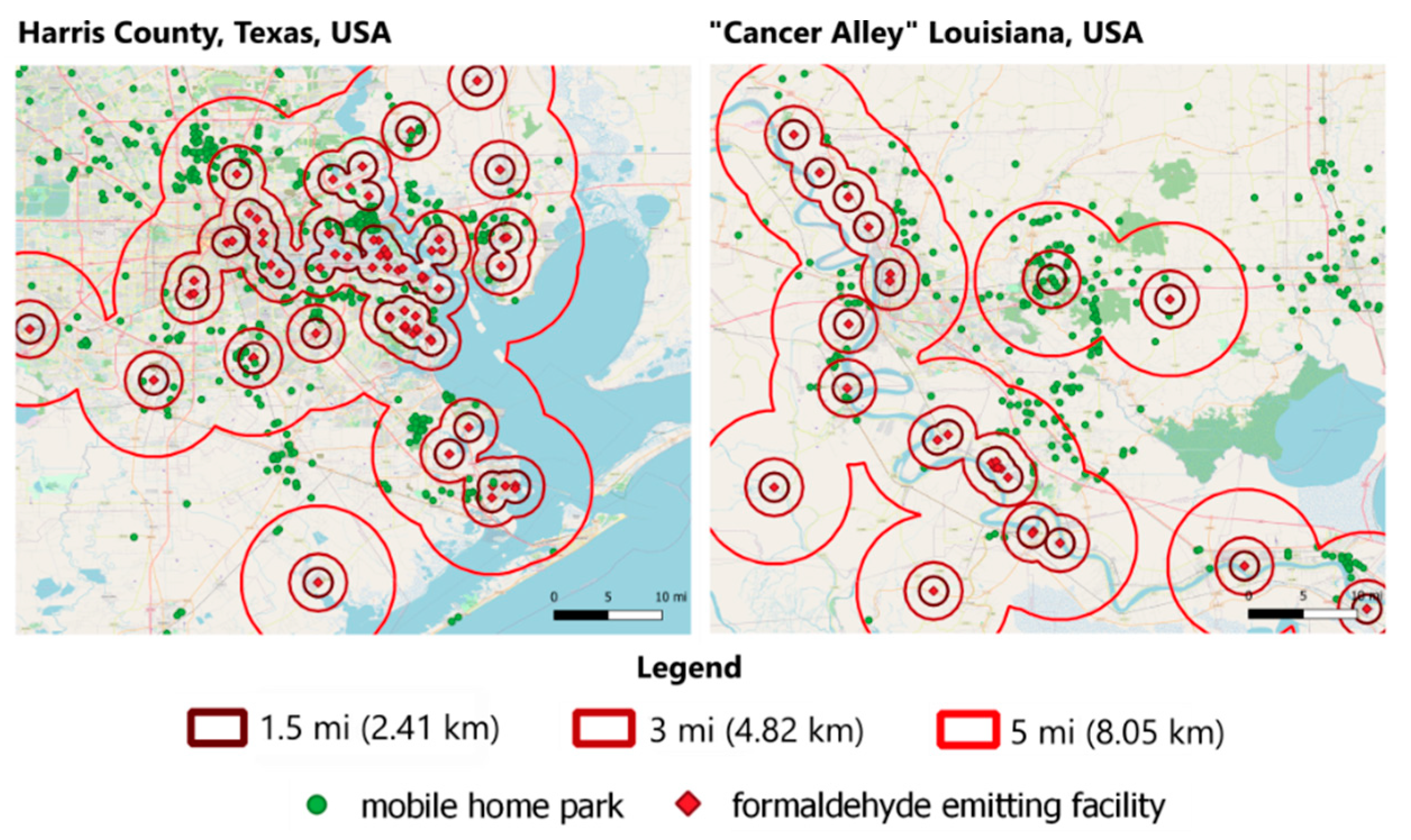
3.2.2. Increased Exposure to Formaldehyde from Near-Field Exposures
3.3. Identification of Populations with Increased Susceptibility to Formaldehyde
3.3.1. Increased Susceptibility to the Health Risk of Formaldehyde Exposures Due to Co-Exposures to Chemicals with Similar Health Endpoints
3.3.2. Increased Susceptibility to Formaldehyde Due to Co-Exposures to Socially-Derived Nonchemical Stressors
3.3.3. Specific Characteristics of PESS in Areas with Increased Exposure and Susceptibility to Formaldehyde
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Burwell-Naney, K.; Zhang, H.; Samantapudi, A.; Jiang, C.; Dalemarre, L.; Rice, L.; Williams, E.; Wilson, S. Spatial Disparity in the Distribution of Superfund Sites in South Carolina: An Ecological Study. Environ. Health 2013, 12, 96. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.; Mohai, P. Environmental Justice Implications of Brownfield Redevelopment in the United States. Soc. Nat. Resour. 2012, 25, 602–609. [Google Scholar] [CrossRef]
- Samet, J.M. Urban Air Pollution and Health Inequities: A Workshop Report. Environ. Health Perspect. Suppl. 2001, 109, 357. [Google Scholar] [CrossRef] [Green Version]
- Mohai, P.; Lantz, P.M.; Morenoff, J.; House, J.S.; Mero, R.P. Racial and Socioeconomic Disparities in Residential Proximity to Polluting Industrial Facilities: Evidence from the Americans’ Changing Lives Study. Am. J. Public Health 2009, 99, S649–S656. [Google Scholar] [CrossRef]
- White, R. Life at the Fenceline—English; Environmental Justice Health Alliance for Chemical Policy Reform: Brattleboro, VT, USA, 2018. [Google Scholar]
- Davis, H.T.; Aelion, C.M.; Liu, J.; Burch, J.B.; Cai, B.; McDermott, S. Potential Sources and Racial Disparities in the Residential Distribution of Soil Arsenic and Lead among Pregnant Women. Sci. Total Environ. 2017, 23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hyland, C.; Laribi, O. Review of Take-Home Pesticide Exposure Pathway in Children Living in Agricultural Areas. Environ. Res. 2017, 156, 559–570. [Google Scholar] [CrossRef]
- Zota, A.R.; Shamasunder, B. The Environmental Injustice of Beauty: Framing Chemical Exposures from Beauty Products as a Health Disparities Concern. Am. J. Obstet. Gynecol. 2017, 6, 418.e1–418.e6. [Google Scholar] [CrossRef] [Green Version]
- Seabury, S.A.; Terp, S.; Boden, L.I. Racial and Ethnic Differences in the Frequency of Workplace Injuries and Prevalence of Work-Related Disability. Health Aff. 2017, 36, 266–273. [Google Scholar] [CrossRef] [PubMed]
- Pullen Fedinick, K.; Taylor, S.; Roberts, M.; Moore, R.; Olson, E. Watered Down Justice; Natural Resources Defense Council: New York, NY, USA, 2019; p. 52. [Google Scholar]
- Castorina, R.; Bradman, A.; Fenster, L.; Barr, D.B.; Bravo, R.; Vedar, M.G.; Harnly, M.E.; McKone, T.E.; Eisen, E.A.; Eskenazi, B. Comparison of Current-Use Pesticide and Other Toxicant Urinary Metabolite Levels among Pregnant Women in the CHAMACOS Cohort and NHANES. Environ. Health Perspect. 2010, 118, 856–863. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cushing, L.; Faust, J.; August, L.M.; Cendak, R.; Wieland, W.; Alexeeff, G. Racial/Ethnic Disparities in Cumulative Environmental Health Impacts in California: Evidence from a Statewide Environmental Justice Screening Tool (CalEnviroScreen 1.1). Am. J. Public Health 2015, 105, 8. [Google Scholar] [CrossRef]
- Huang, H.; Tornero-Velez, R.; Barzyk, T.M. Associations between Socio-Demographic Characteristics and Chemical Concentrations Contributing to Cumulative Exposures in the United States. J. Expo. Sci. Environ. Epidemiol. 2017, 27, 544–550. [Google Scholar] [CrossRef] [PubMed]
- Bullard, R.D.; Mohai, P.; Saha, R.; Wright, B. Toxic Wastes and Race at Twenty, 1987–2007; A Report Prepared for the United Church of Christ Justice and Witness Ministries; United Church of Christ Justice and Witness Ministries: San Leandro, CA, USA, 2007. [Google Scholar]
- Mohai, P. Which Came First, People or Pollution? A Review of Theory and Evidence from Longitudinal Environmental Justice Studies. Environ. Res Lett. 2015, 10, 125011. [Google Scholar] [CrossRef]
- Chaves, K.; Wilson, N.; Gray, D.; Barton, B.; Bonnett, D.; Azam, I. 2018 National Healthcare Quality and Disparities Report. Available online: https://www.ahrq.gov/research/findings/nhqrdr/nhqdr18/index.html (accessed on 2 June 2021).
- Shi, L.; Chen, C.-C.; Nie, X.; Zhu, J.; Hu, R. Racial and Socioeconomic Disparities in Access to Primary Care Among People with Chronic Conditions. J. Am. Board. Fem. Med. 2014, 27, 189–198. [Google Scholar] [CrossRef] [Green Version]
- Morland, K.; Filomena, S. Disparities in the Availability of Fruits and Vegetables between Racially Segregated Urban Neighbourhoods. Public Health Nutr. 2007, 10, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walker, R.E.; Keane, C.R.; Burke, J.G. Disparities and Access to Healthy Food in the United States: A Review of Food Deserts Literature. Health Place 2010, 16, 876–884. [Google Scholar] [CrossRef]
- Hilmers, A.; Hilmers, D.C.; Dave, J. Neighborhood Disparities in Access to Healthy Foods and Their Effects on Environmental Justice. Am. J. Public Health 2012, 102, 1644–1654. [Google Scholar] [CrossRef] [PubMed]
- Committee on Developing Indicators of Educational Equity; Board on Testing and Assessment; Committee on National Statistics; Division of Behavioral and Social Sciences and Education; National Academies of Sciences, Engineering, and Medicine. Monitoring Educational Equity; Edley, C., Koenig, J., Nielsen, N., Citro, C., Eds.; National Academies Press: Washington, DC, USA, 2019; p. 25389. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine. Communities in Action: Pathways to Health Equity; Weinstein, J.N., Geller, A., Negussie, Y., Baciu, A., National Academies of Sciences, Engineering, and Medicine (U.S.), Eds.; The National Academies Press: Washington, DC, USA, 2017. [Google Scholar] [CrossRef]
- Antonovsky, A. Social Class, Life Expectancy and Overall Mortality. Milbank Mem. Fund. Q. 1967, 45, 31. [Google Scholar] [CrossRef]
- DuBois, W.E.B. The Health and Physique of the Negro American. Am. J. Public Health 2003, 93, 272–276. [Google Scholar] [CrossRef]
- Frost, W.H. How Much Control of Tuberculosis? Am. J. Public Health Nations Health 1937, 27, 759–766. [Google Scholar] [CrossRef]
- Phelan, J.C.; Link, B.G.; Tehranifar, P. Social Conditions as Fundamental Causes of Health Inequalities: Theory, Evidence, and Policy Implications. J. Health Soc. Behav. 2010, 51 (Suppl. 1), S28–S40. [Google Scholar] [CrossRef] [Green Version]
- Chari, R.; Burke, T.A.; White, R.H.; Fox, M.A. Integrating Susceptibility into Environmental Policy: An Analysis of the National Ambient Air Quality Standard for Lead. Int. J. Environ. Res. Public. Health 2012, 9, 1077–1096. [Google Scholar] [CrossRef]
- National Research Council. Science and Decisions: Advancing Risk Assessment; National Academies Press: Washington, DC, USA, 2009; pp. 1–403. [Google Scholar]
- Environmental Protection Agency. Framework for Cumulative Risk Assessment; USEPA: Washington, DC, USA, 2003; p. 129.
- United States, Executive Office of the President [Joseph Biden]. Executive Order 13990 of 20 January 2021 Protecting Public Health and the Environment and Restoring Science to Tackle the Climate Crisis; Federal Register: Washington, DC, USA, 2021.
- Krimsky, S. The Unsteady State and Inertia of Chemical Regulation under the US Toxic Substances Control Act. PLoS Biol. 2017, 15, e2002404. [Google Scholar] [CrossRef] [Green Version]
- EPA. Toxic Substances Control Act; USEPA: Washington, DC, USA, 2016.
- Sexton, K. Sociodemographic Aspects of Human Susceptibility to Toxic Chemicals: Do Class and Race Matter for Realistic Risk Assessment? Environ. Toxicol. Pharmacol. 1997, 9, 261–269. [Google Scholar] [CrossRef]
- Payne-Sturges, D.; Scammell, M.; Levy, J.; Cory-Slechta, D.; Symanski, E.; Carr Shmool, J.; Laumbach, R.; Linder, S.; Clougherty, J. Methods for Evaluating the Combined Effects of Chemical and Nonchemical Exposures for Cumulative Environmental Health Risk Assessment. Int. J. Environ. Res. Public. Health 2018, 15, 2797. [Google Scholar] [CrossRef] [Green Version]
- United States Environmental Protection Agency. Final Scope of the Risk Evaluation for Formaldehyde CASRN 50-00-0; USEPA: Washington, DC, USA, 2020; p. 172.
- Agency for Toxic Substances and Disease Registry. Addendum to the Toxicological Profile for Formaldehyde; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2010.
- TRI Form R & A Download. Available online: https://enviro.epa.gov/facts/tri/form_ra_download.html? (accessed on 27 April 2021).
- USEPA Office of Research and Development. Chemical and Products Database (CPDat). Available online: https://www.epa.gov/chemical-research/chemical-and-products-database-cpdat (accessed on 27 April 2021).
- Chemical Search|IRIS|US USEPA. Available online: https://cfpub.epa.gov/ncea/iris/search/index.cfm (accessed on 16 May 2020).
- Chemicals in Cosmetics—California Health and Human Services Open Data Portal. Available online: https://data.chhs.ca.gov/dataset/chemicals-in-cosmetics (accessed on 26 April 2021).
- Mobile Home Parks—Data.gov. Available online: https://catalog.data.gov/dataset/mobile-home-parks (accessed on 23 May 2020).
- CDC SVI Data and Documentation Download|Place and Health|ATSDR. Available online: https://www.atsdr.cdc.gov/placeandhealth/svi/data_documentation_download.html (accessed on 27 April 2021).
- US USEPA. National Air Toxics Assessment. Available online: https://www.epa.gov/national-air-toxics-assessment (accessed on 26 May 2021).
- World Health Organization. WHO Guidelines for Indoor Air Quality: Selected Pollutants; WHO: Copenhagen, Denmark, 2010. [Google Scholar]
- American Academy of Pediatrics. Involuntary Smoking—A Hazard to Children. Pediatrics 1986, 77, 755. [Google Scholar]
- Schick, S.; Glantz, S. Philip Morris Toxicological Experiments with Fresh Sidestream Smoke: More Toxic than Mainstream Smoke. Tob. Control 2005, 14, 396–404. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.K. Chamber Assessment of Formaldehyde and VOC Emissions from Wood-Based Panels. Indoor Air-Int. J. Indoor Air Qual. Clim. 1999, 9, 209–215. [Google Scholar] [CrossRef]
- Myers, G. Formaldehyde Emission from Particleboard and Plywood Paneling—Measurement, Mechanism, and Product Standards. For. Prod. J. 1983, 33, 27–37. [Google Scholar]
- Gox, E. Urea Formaldehyde Foam Insulation-Defusing A Timebomb. Am. J. Law Med. 1985, 11, 81–104. [Google Scholar]
- Hawthorne, A.; Gammage, R. Formaldehyde Release from Simulated Wall Panels Insulated with Urea-Formaldehyde Foam Insulation. J. Air Pollut. Control Assoc. 1982, 32, 1126–1131. [Google Scholar] [CrossRef]
- Kelly, T.J.; Smith, D.L.; Satola, J. Emission Rates of Formaldehyde from Materials and Consumer Products Found in California Homes. Environ. Sci. Technol. 1999, 33, 81–88. [Google Scholar] [CrossRef]
- Weschler, C.J.; Hodgson, A.T.; Wooley, J.D. Indoor Chemistry: Ozone, Volatile Organic Compounds, and Carpets. Environ. Sci. Technol. 1992, 26, 2371–2377. [Google Scholar] [CrossRef]
- Gilbert, N.L.; Gauvin, D.; Guay, M.; Heroux, M.-E.; Dupuis, G.; Legris, M.; Chan, C.C.; Dietz, R.N.; Levesque, B. Housing Characteristics and Indoor Concentrations of Nitrogen Dioxide and Formaldehyde in Quebec City, Canada. Environ. Res. 2006, 102, 1–8. [Google Scholar] [CrossRef]
- De Groot, A.C.; Flyvholm, M.; Lensen, G.; Menne, T.; Coenraads, P.-J. Formaldehyde-Releasers: Relationship to Formaldehyde Contact Allergy. Contact Allergy to Formaldehyde and Inventory of Formaldehyde-Releasers. Contact Dermat. 2009, 61, 63–85. [Google Scholar] [CrossRef] [Green Version]
- Schwartz, J.; Bellinger, D.; Glass, T. Expanding the Scope of Environmental Risk Assessment to Better Include Differential Vulnerability and Susceptibility. Am. J. Public Health 2011, 101, S88–S93. [Google Scholar] [CrossRef] [PubMed]
- National Research Council (U.S.); Committee on the Health Risks of Phthalates. Phthalates and Cumulative Risk Assessment: The Tasks Ahead; National Academies Press: Washington, DC, USA, 2008. [Google Scholar]
- NTP (National Toxicology Program). Report on Carcinogens, 14th ed.; U.S. Department of Health and Human Services, Research Triangle Park: Durham, NC, USA, 2016.
- Committee to Review Advances Made to the IRIS Process; Board on Environmental Studies and Toxicology; Division on Earth and Life Studies; National Academies of Sciences, Engineering, and Medicine. Progress toward Transforming the Integrated Risk Information System (IRIS) Program: A 2018 Evaluation; National Academies Press: Washington, DC, USA, 2018; p. 25086. [Google Scholar] [CrossRef]
- USEPA Office of Research and Development. Basic Information about the Integrated Risk Information System. Available online: https://www.epa.gov/iris/basic-information-about-integrated-risk-information-system (accessed on 27 April 2021).
- United States Government Accountability Office. Chemical Assessments: Annual USEPA Survey Inconsistent with Leading Practices in Program Management; GAO-21-156; U.S. Government Printing Office: Washington, DC, USA, 2020.
- Emeny, R.T.; Carpenter, D.O.; Lawrence, D.A. Health Disparities: Intracellular Consequences of Social Determinants of Health. Toxicol. Appl. Pharmacol. 2021, 416, 115444. [Google Scholar] [CrossRef]
- Olden, K.; Lin, Y.-S.; Gruber, D.; Sonawane, B. Epigenome: Biosensor of Cumulative Exposure to Chemical and Nonchemical Stressors Related to Environmental Justice. Am. J. Public Health 2014, 104, 1816–1821. [Google Scholar] [CrossRef] [PubMed]
- Goosby, B.J.; Cheadle, J.E.; Mitchell, C. Stress-Related Biosocial Mechanisms of Discrimination and African American Health Inequities. Annu. Rev. Sociol. 2018, 44, 319–340. [Google Scholar] [CrossRef]
- Williams, D.R.; Lawrence, J.A.; Davis, B.A.; Vu, C. Understanding How Discrimination Can Affect Health. Health Serv. Res. 2019, 54, 1374–1388. [Google Scholar] [CrossRef] [Green Version]
- Snyder-Mackler, N.; Burger, J.R.; Gaydosh, L.; Belsky, D.W.; Noppert, G.A.; Campos, F.A.; Bartolomucci, A.; Yang, Y.C.; Aiello, A.E.; O’Rand, A.; et al. Social Determinants of Health and Survival in Humans and Other Animals. Science 2020, 368, eaax9553. [Google Scholar] [CrossRef] [PubMed]
- Children’s Health Protection Advisory Committee. Protecting Children’s Health under Amended TSCA: Chemical Prioritization. United States Environmental Protection Agency: Washington, DC, USA, 2021; p. 60. [Google Scholar]
- Lee, C. A Game Changer in the Making? Lessons from States Advancing Environmental Justice through Mapping and Cumulative Impact Strategies. Environ. Law Rep. 2020, 50, 14. [Google Scholar]
- Baptista, A.I. Local Policies for Environmental Justice: A National Scan; Tishman Environment and Design Center at the New School: New York, NY, USA, 2019. [Google Scholar]
- Singleton, T.; Weinberg, L. S232 2R SCS SCS; State of New Jersey: New Jersey City, NJ, USA, 2020.
- Lam, J.; Koustas, E.; Sutton, P.; Padula, A.M.; Cabana, M.D.; Vesterinen, H.; Griffiths, C.; Dickie, M.; Daniels, N.; Whitaker, E.; et al. Exposure to Formaldehyde and Asthma Outcomes: A Systematic Review, Meta-Analysis, and Economic Assessment. PLoS ONE 2021, 16, e0248258. [Google Scholar] [CrossRef] [PubMed]


| Step | Description |
|---|---|
| 1 | Identify chemical of concern being evaluated |
| 2 | a. Determine geographic locations with potential for far-field exposure. Sources of geographic information include peer-reviewed literature, chemical release databases (e.g., Toxic Release Inventory), modeled exposure databases (e.g., National Emissions Inventory). |
| b. Identify possible sources of near-field exposures. Sources of information include peer-reviewed literature, grey literature, product databases (e.g., Chemical and Products Database), authoritative assessments (e.g., Integrated Risk Information System assessments). | |
| 3 | a. Identify most sensitive endpoints for chemical being evaluated. This step is often performed during the risk evaluation scoping phase and can include peer-reviewed literature, grey-literature, authoritative evaluations, and other information sources. |
| b. Identify chemicals with common health endpoint. Sources of data include peer-reviewed literature, grey literature, authoritative assessments (e.g., Integrated Risk Information System), toxicological databases (e.g., ToxCast). | |
| c. Determine geographic locations with overlap between chemical of concern and other chemicals with shared endpoint. Sources of geographic information include peer-reviewed literature, chemical release databases (e.g., Toxic Release Inventory), modeled exposure databases (e.g., National Emissions Inventory). | |
| 4 | a. Identify relevant non-chemical stressors to be accounted for in assessment. Sources of information include peer-reviewed literature, reports, and datasets with sociodemographic indicators (e.g., American Community Survey, Social Vulnerability Index). |
| b. Assess the overlap of chemical and non-chemical stressors for geographic hotspots (i.e., areas with co-exposures to multiple chemicals associated with shared adverse health outcome). | |
| 5 | Develop profile of populations with greater exposure and/or susceptibility to be used in risk characterization and management strategies. |
| SVI 2018 Variable Name | SVI 2018 Variable Description | Number of Formaldehyde Emitting Facilities in 2000 |
|---|---|---|
| EP_PCI | Per capita income estimate, 2014–2018 ACS | 0.122752422 |
| EP_NOHSDP | Percentage of persons with no high school diploma (age 25+) estimate | −0.049584352 |
| EP_AGE65 | Percentage of persons aged 65 and older estimate, 2014–2018 ACS | −0.169812317 |
| EP_AGE17 | Percentage of persons aged 17 and younger estimate, 2014–2018 ACS | 0.052260265 |
| EP_DISABL | Percentage of civilian noninstitutionalized population with a disability estimate, 2014–2018 ACS | −0.1451448 |
| EP_SNGPNT | Percentage of single parent households with children under 18 estimate, 2014–2018 ACS | 0.111258637 |
| EP_MINRTY | Percentage minority (all persons except white, non-Hispanic) estimate, 2014–2018 ACS | 0.132175661 |
| EP_LIMENG | Percentage of persons (age 5+) who speak English “less than well” estimate, 2014–2018 ACS | 0.110177734 |
| EP_MUNIT | Percentage of housing in structures with 10 or more units estimate | 0.249835074 |
| EP_MOBILE | Percentage of mobile homes estimate | −0.151929548 |
| RPL_THEME3 | Percentile ranking for Minority Status/Language theme | 0.185509699 |
| RPL_THEME4 | Percentile ranking for Housing Type/Transportation theme | 0.109942915 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pullen Fedinick, K.; Yiliqi, I.; Lam, Y.; Lennett, D.; Singla, V.; Rotkin-Ellman, M.; Sass, J. A Cumulative Framework for Identifying Overburdened Populations under the Toxic Substances Control Act: Formaldehyde Case Study. Int. J. Environ. Res. Public Health 2021, 18, 6002. https://doi.org/10.3390/ijerph18116002
Pullen Fedinick K, Yiliqi I, Lam Y, Lennett D, Singla V, Rotkin-Ellman M, Sass J. A Cumulative Framework for Identifying Overburdened Populations under the Toxic Substances Control Act: Formaldehyde Case Study. International Journal of Environmental Research and Public Health. 2021; 18(11):6002. https://doi.org/10.3390/ijerph18116002
Chicago/Turabian StylePullen Fedinick, Kristi, Ilch Yiliqi, Yukyan Lam, David Lennett, Veena Singla, Miriam Rotkin-Ellman, and Jennifer Sass. 2021. "A Cumulative Framework for Identifying Overburdened Populations under the Toxic Substances Control Act: Formaldehyde Case Study" International Journal of Environmental Research and Public Health 18, no. 11: 6002. https://doi.org/10.3390/ijerph18116002






