Analyzing Spatial Patterns of Health Vulnerability to Drought in the Brazilian Semiarid Region
Abstract
:1. Introduction
2. Materials and Methods
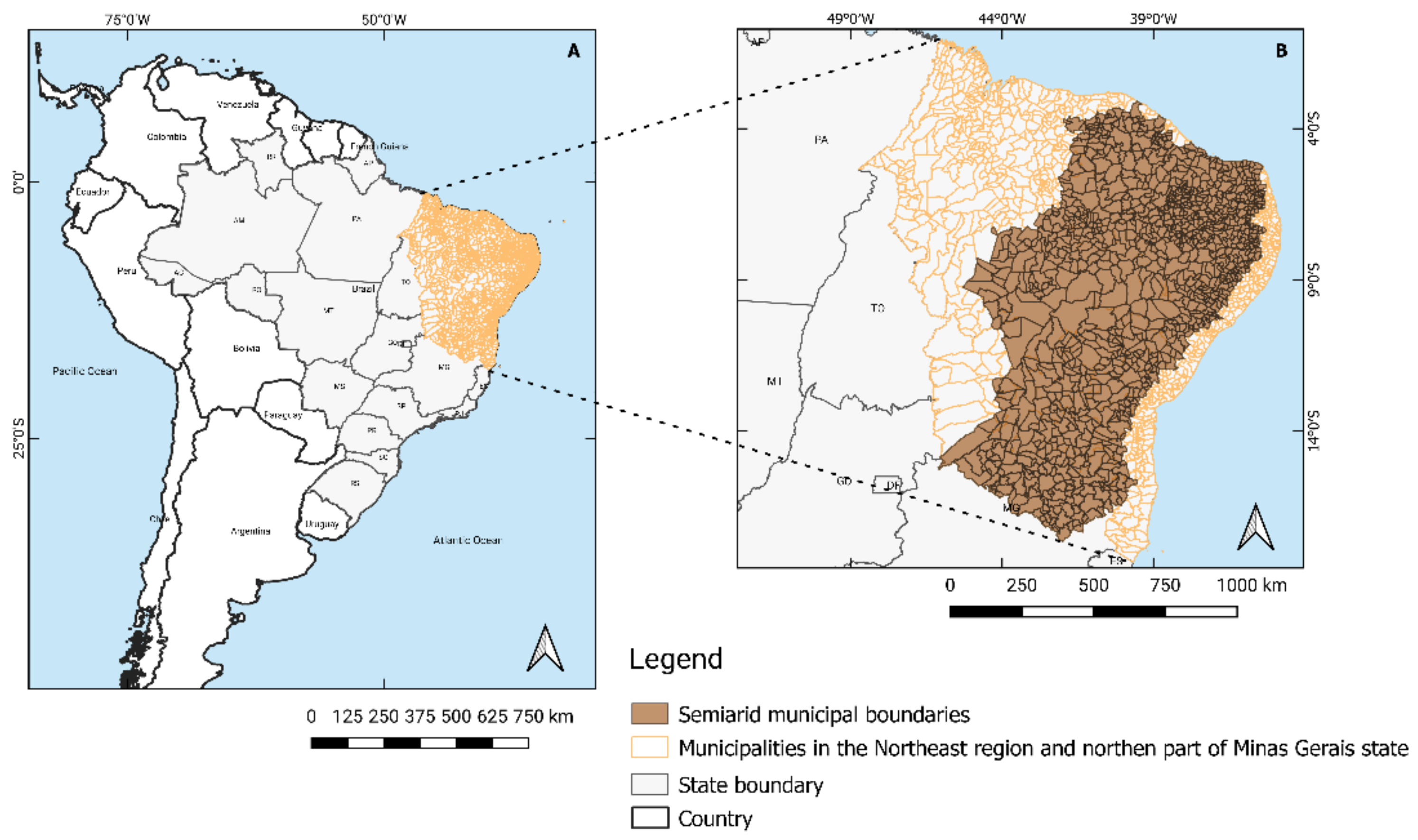
2.1. Study Area
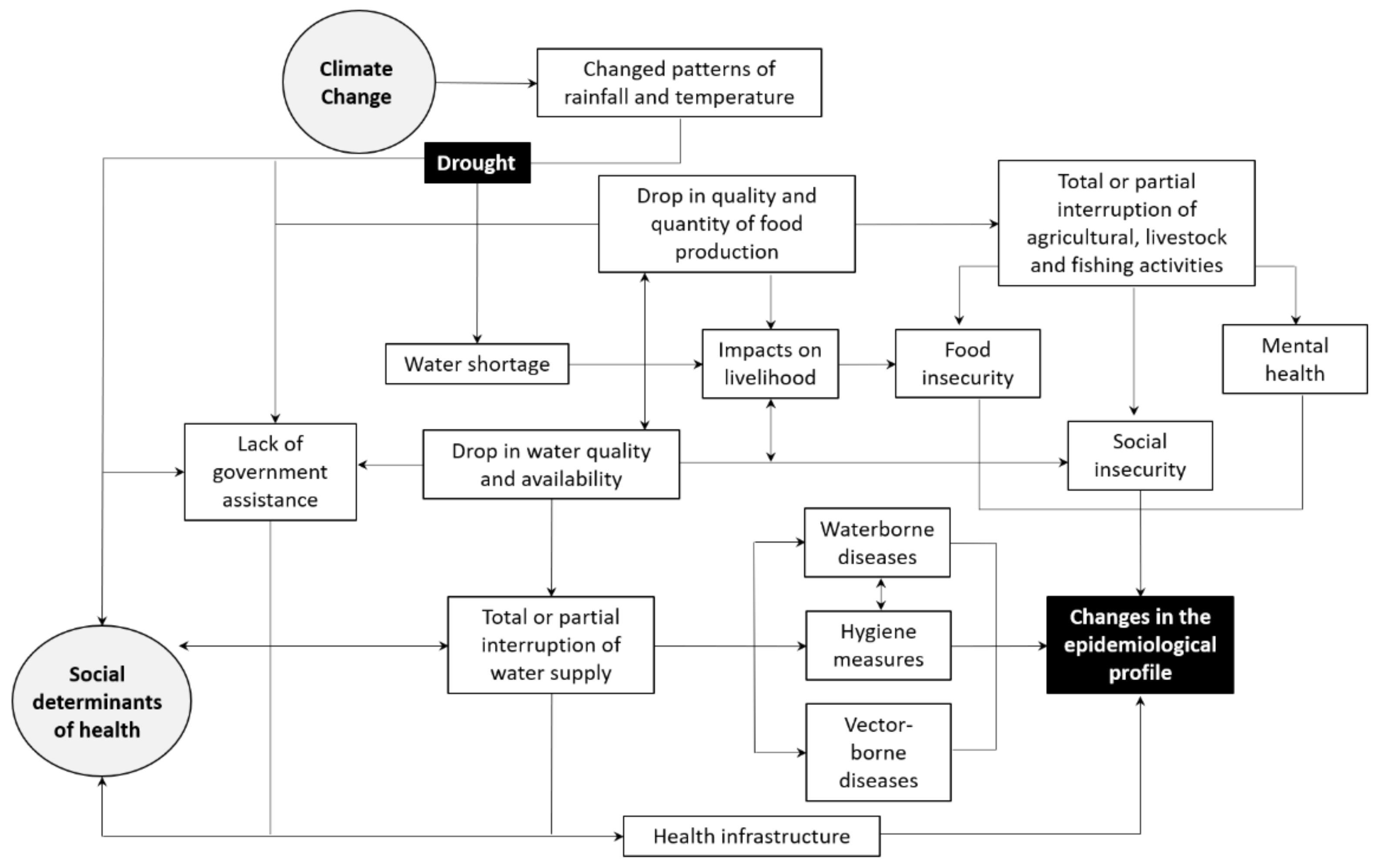
2.2. Conceptual Framework
2.3. Vulnerability Data
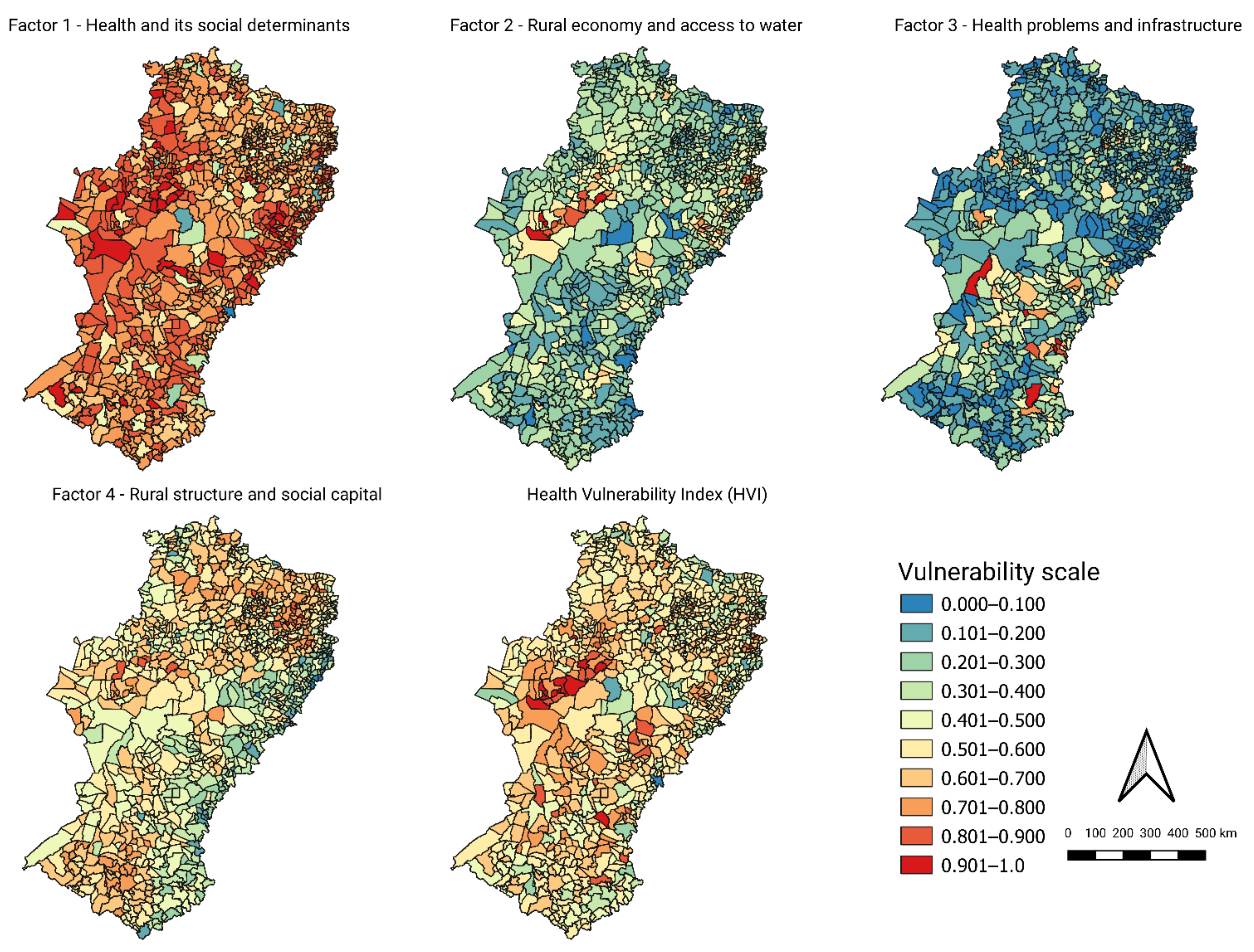
2.4. Multivariate Analysis
2.5. Indices and Maps
3. Results
4. Discussion
4.1. Rural and Social Characteristics Influencing Health Vulnerabilities
4.2. Social Determinants at the Borders, Rural Aspects in the Inland Regions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health. Final Report of the Commission on Social Determinants of Health; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Lucyk, K.; McLaren, L. Taking stock of the social determinants of health: A scoping review. PLoS ONE 2017, 12, e0177306. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rasella, D.; Machado, D.B.; Castellanos, M.E.P.; Paim, J.; Szwarcwald, C.L.; Lima, D.; Magno, L.; Pedrana, L.; Medina, M.G.; Penna, G.O.; et al. Assessing the relevance of indicators in tracking social determinants and progress toward equitable population health in Brazil. Glob. Health Action 2016, 9, 29042. [Google Scholar] [CrossRef] [PubMed]
- Pedrana, L.; Pamponet, M.; Walker, R.; Costa, F.; Rasella, D. Scoping review: National monitoring frameworks for social determinants of health and health equity. Glob. Health Action 2016. [Google Scholar] [CrossRef] [PubMed]
- Gray, L. Social determinants of health, disaster vulnerability, severe and morbid obesity in adults: Triple jeopardy? Int. J. Environ. Res. Public Health 2017, 14, 1452. [Google Scholar] [CrossRef] [Green Version]
- Nomura, S.; Parsons, A.J.Q.; Hirabayashi, M.; Kinoshita, R.; Liao, Y.; Hodgson, S. Social determinants of mid-to long-term disaster impacts on health: A systematic review. Int. J. Disaster Risk Reduct. 2016, 16, 53–67. [Google Scholar] [CrossRef]
- Lindsay, J.R. The determinants of disaster vulnerability: Achieving sustainable mitigation through population health. Nat. Hazards 2003, 28, 291–304. [Google Scholar] [CrossRef]
- Alpino, T.A.; de Sena, A.R.M.; de Freitas, C.M. Disasters related to droughts and public health—A review of the scientific literature. Cienc. Saude Coletiva 2016, 21, 809–820. [Google Scholar] [CrossRef] [Green Version]
- Centre for Research on the Epidemiology of Disasters—CRED EM-DAT—The International Disaster Database. Available online: https://public.emdat.be/ (accessed on 10 January 2020).
- Masson-Delmotte, V.; Zhai, P.; Pörtner, H.-O.; Roberts, D.; Skea, J.; Shukla, P.R.; Pirani, A.; Moufouma-Okia, W.; Péan, C.; Pidcock, R.; et al. (Eds.) IPCC Summary for policy makers. In Global Warming of 1.5 °C. An IPCC Special Report on the Impacts of Global Warming of 1.5 °C above Pre-Industrial Levels and Related Global Greenhouse Gas Emission Pathways, in the Context of Strengthening the Global Response to the Threat of Climate Change; World Meteorological Organization: Geneva, Switzerland, 2018; p. 32. ISBN 1496354044. [Google Scholar]
- Obermaier, M.; Rosa, L.P. Mudança climática e adaptação no Brasil: Uma análise crítica. Estud. Av. 2013, 27, 155–176. [Google Scholar] [CrossRef] [Green Version]
- Wilhite, D.A.; Sivakumar, M.V.K.; Pulwarty, R. Managing drought risk in a changing climate: The role of national drought policy. Weather Clim. Extrem. 2014, 3, 4–13. [Google Scholar] [CrossRef] [Green Version]
- Sena, A.; Ebi, K.L.; Freitas, C.; Corvalan, C.; Barcellos, C. Indicators to measure risk of disaster associated with drought: Implications for the health sector. PLoS ONE 2017, 12. [Google Scholar] [CrossRef]
- Sena, A.; Barcellos, C.; Freitas, C.; Corvalan, C. Managing the health impacts of drought in Brazil. Int. J. Environ. Res. Public Health 2014, 11, 10737–10751. [Google Scholar] [CrossRef] [Green Version]
- Sena, A.; Freitas, C.; Feitosa Souza, P.; Alpino, T.; Pedroso, M.; Corvalan, C.; Barcellos, C.; Carneiro, F. Drought in the Semiarid Region of Brazil: Exposure, Vulnerabilities and Health Impacts from the Perspectives of Local Actors. PLoS Curr. 2018. [Google Scholar] [CrossRef]
- Stanke, C.; Kerac, M.; Prudhomme, C.; Medlock, J.; Murray, V. Health effects of drought: A systematic review of the evidence. PLoS Curr. 2013, 5, 1–40. [Google Scholar] [CrossRef] [Green Version]
- Coêlho, A.E.L.; Adair, J.G.; Mocellin, J.S.P. Psychological responses to drought in northeastern Brazil. Interam. J. Psychol. 2004, 38, 95–103. [Google Scholar]
- McCann, D.G.C.; Moore, A.; Walker, M.-E. The water/health nexus in disaster medicine: I. Drought versus flood. Curr. Opin. Environ. Sustain. 2011, 3, 480–485. [Google Scholar] [CrossRef]
- Vins, H.; Bell, J.; Saha, S.; Hess, J.J. The mental health outcomes of drought: A systematic review and causal process diagram. Int. J. Environ. Res. Public Health 2015, 12, 13251–13275. [Google Scholar] [CrossRef] [Green Version]
- Organização Pan-Americana da Saúde (OPAS). Atuação do Setor Saúde Frente a Situações de Seca. In Série Desenvolvimento Sustentável e Saúde; Ministério da Saúde: Brasília, Brazil, 2015. [Google Scholar]
- Yusa, A.; Berry, P.; Cheng, J.J.; Ogden, N.; Bonsal, B.; Stewart, R.; Waldick, R. Climate Change, Drought and Human Health in Canada. Int. J. Environ. Res. Public Health 2015, 12, 8359–8412. [Google Scholar] [CrossRef]
- OBrien, L.V.; Berry, H.L.; Coleman, C.; Hanigan, I.C. Drought as a mental health exposure. Environ. Res. 2014, 131, 181–187. [Google Scholar] [CrossRef] [Green Version]
- Lima, E.d.A.; Firmino, J.L.d.N.; Gomes Filho, M.F. A relação da previsão da precipitação pluviométrica e casos de dengue nos estados de Alagoas e Paraíba nordeste do Brasil. Rev. Bras. Meteorol. 2008, 23, 264–269. [Google Scholar] [CrossRef] [Green Version]
- Londe, L.d.R.; Coutinho, M.P.; Gregório, D.; Torres, L.; Santos, L.B.L.; Soriano, É. Desastres relacionados à água no Brasil: Perspectivas e recomendações. Ambient. Soc. 2014, 17, 133–152. [Google Scholar] [CrossRef] [Green Version]
- Marcynuk, P.B.; Flint, J.A.; Sargeant, J.M.; Jones-Bitton, A.; Brito, A.M.; Luna, C.F.; Szilassy, E.; Thomas, M.K.; Lapa, T.M.; Perez, E. Comparison of the burden of diarrhoeal illness among individuals with and without household cisterns in northeast Brazil. BMC Infect. Dis. 2013, 13, 65. [Google Scholar] [CrossRef] [Green Version]
- Lohmann, S.; Lechtenfeld, T. The Effect of Drought on Health Outcomes and Health Expenditures in Rural Vietnam. World Dev. Vol. 2015, 72, 432–448. [Google Scholar] [CrossRef] [Green Version]
- Confalonieri, U.E.C.; Lima, A.C.L.; Brito, I.; Quintão, A.F. Social, environmental and health vulnerability to climate change in the Brazilian Northeastern Region. Clim. Change. 2014, 127, 123–137. [Google Scholar] [CrossRef]
- Ebi, K.L.; Bowen, K. Extreme events as sources of health vulnerability: Drought as an example. Weather Clim. Extrem. 2016, 11, 95–102. [Google Scholar] [CrossRef] [Green Version]
- Damasceno, N.P.; Khan, A.S.; Lima, P.V.P.S. Desempenho da saúde pública no semiárido brasileiro. Rev. Ibero-Am. Ciências Ambient. 2018, 9, 171–187. [Google Scholar] [CrossRef] [Green Version]
- Alvala, R.; Cunha, A.P.; Brito, S.S.B.; Seluchi, M.E.; Marengo, J.A.; Moraes, O.L.L.; Carvalho, M.A. Drought monitoring in the Brazilian Semiarid region. An. Acad. Bras. Cienc. 2019, 91, e20170209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vieira, R.M.d.S.P.; Sestini, M.F.; Tomasella, J.; Marchezini, V.; Pereira, G.R.; Barbosa, A.A.; Santos, F.C.; Rodriguez, D.A.; do Nascimento, F.R.; Santana, M.O.; et al. Characterizing spatio-temporal patterns of social vulnerability to droughts, degradation and desertification in the Brazilian northeast. Environ. Sustain. Indic. 2020, 5, 100016. [Google Scholar] [CrossRef]
- Chan, E.Y.Y.; Huang, Z.; Lam, H.C.Y.; Wong, C.K.P.; Zou, Q. Health vulnerability index for disaster risk reduction: Application in belt and road initiative (BRI) region. Int. J. Environ. Res. Public Health 2019, 16, 380. [Google Scholar] [CrossRef] [Green Version]
- Menezes, J.A.; Confalonieri, U.; Madureira, A.P.; Duval, I.d.B.; do Santos, R.B.; Margonari, C. Mapping human vulnerability to climate change in the Brazilian Amazon: The construction of a municipal vulnerability index. PLoS ONE 2018, 13, e0190808. [Google Scholar] [CrossRef] [Green Version]
- Vommaro, F.; Menezes, J.A.; Barata, M.M.d.L. Contributions of municipal vulnerability map of the population of the state of Maranhão (Brazil) to the sustainable development goals. Sci. Total Environ. 2020, 706, 134629. [Google Scholar] [CrossRef]
- Asmall, T. The Adverse Health Effects Associated with Drought in Africa: Working towards Developing a Vulnerability Index. Master’s Thesis, Queen’s University, Kingston, ON, Canada, 2020. Available online: http://hdl.handle.net/11427/32447 (accessed on 21 April 2021).
- Secretaria Municipal de Saúde de Belo Horizonte. Índice de Vulnerabilidade da Saúde. Available online: https://prefeitura.pbh.gov.br/sites/default/files/estrutura-de-governo/saude/2018/publicacaoes-da-vigilancia-em-saude/indice_vulnerabilidade2012.pdf (accessed on 21 April 2021).
- Debortoli, N.S.; Camarinha, P.I.M.; Marengo, J.A.; Rodrigues, R.R. An index of Brazil’s vulnerability to expected increases in natural flash flooding and landslide disasters in the context of climate change. Nat. Hazards 2017. [Google Scholar] [CrossRef]
- Cutter, S.L.; Boruff, B.J.; Shirley, W.L. Social Vulnerability to Environmental Hazards. Soc. Sci. Q. 2003, 84, 242–261. [Google Scholar] [CrossRef]
- Hummell, M.B.d.L.; Cutter, S.L.; Emrich, C.T. Social Vulnerability to Natural Hazards in Brazil. Int. J. Disaster Risk Sci. 2016, 7, 111–122. [Google Scholar] [CrossRef] [Green Version]
- Khan, F.A.; Salman, A. A simple human vulnerability index to climate change hazards for Pakistan. Int. J. Disaster Risk Sci. 2012, 3, 163–176. [Google Scholar] [CrossRef] [Green Version]
- Pastrana, M.E.O.; Brito, R.L.; Nicolino, R.R.; de Oliveira, C.S.F.; Haddad, J.P.A. Spatial and statistical methodologies to determine the distribution of dengue in Brazilian municipalities and relate incidence with the health vulnerability index. Spat. Spatiotemporal. Epidemiol. 2014, 11, 143–151. [Google Scholar] [CrossRef]
- Sullivan, C.; Meigh, J. Targeting attention on local vulnerabilities using an integrated index approach: The example of the climate vulnerability index. Water Sci. Technol. 2005, 51, 69–78. [Google Scholar] [CrossRef]
- Silva, V.D.R.P. On climate variability in Northeast of Brazil. J. Arid Environ. 2004, 58, 575–596. [Google Scholar] [CrossRef]
- Marengo, J.A.; Alves, L.M.; Bessera, E.A.; Lacerda, F.F. Variabilidade e mudanças climáticas no semiárido brasileiro. In Recursos Hídricos em Regiões Áridas e Semiáridas; Instituto Nacional do Semiárido—INSA: Campina Grande, Brazil, 2011; pp. 385–422. ISBN 9788564265011. [Google Scholar]
- De Oliveira, M.B.L.; Santos, A.J.B.; Manzi, A.O.; Alvalá, R.C.d.S.; Correia, M.d.F.; de Moura, M.S.B. Trocas de energia e fluxo de carbono entre a vegetação de Caatinga e a atmosfera no Nordeste Brasileiro. Rev. Bras. Meteorol. 2006, 21, 378–386. [Google Scholar]
- Marengo, J.A.; Alves, L.M.; Alvala, R.; Cunha, A.P.; Brito, S.; Moraes, O.L.L. Climatic characteristics of the 2010–2016 drought in the semiarid Northeast Brazil region. An. Acad. Bras. Cienc. 2018, 90, 1973–1985. [Google Scholar] [CrossRef]
- World Health Organization. Operational Framework for Building Climate Resilient Health Systems; World Health Organization: Geneva, Switzerland, 2015; ISBN 978 92 4 156507 3. [Google Scholar]
- Phibbs, S.; Kenney, C.; Severinsen, C.; Mitchell, J.; Hughes, R. Synergising public health concepts with the sendai framework for disaster risk reduction: A conceptual glossary. Int. J. Environ. Res. Public Health 2016, 13, 1241. [Google Scholar] [CrossRef] [Green Version]
- United Nations International Strategy for Disaster Reduction (UNISDR). Sendai Framework for Disaster Risk Reduction 2015–2030; UNISDR: Geneva, Switzerland, 2015. [Google Scholar]
- Confalonieri, U.E.C. Variabilidade climática, vulnerabilidade social e saúde no Brasil. Terra Livre 2003, 1, 193–204. [Google Scholar]
- Sakaluk, J.K.; Short, S.D. A Methodological Review of Exploratory Factor Analysis in Sexuality Research: Used Practices, Best Practices, and Data Analysis Resources. J. Sex Res. 2017, 54, 1–9. [Google Scholar] [CrossRef]
- Holand, I.S.; Lujala, P.; Rod, J.K. Social vulnerability assessment for Norway: A quantitative approach. Nor. Geogr. Tidsskr. 2011, 65, 1–17. [Google Scholar] [CrossRef]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 7th ed.; Pearson: Harlow, UK, 2014; ISBN 978-1-292-02190-4. [Google Scholar]
- Cattell, R.B. The Scientific Use of Factor Analysis in Behavioral and Life; Plenum: New York, NY, USA, 1978. [Google Scholar]
- Fabrigar, L.R.; Wegener, D.T.; MacCallum, R.C.; Strahan, E.J. Evaluating the use of exploratory factor analysis in psychological research. Psychol. Methods 1999, 4, 272–299. [Google Scholar] [CrossRef]
- Gorsuch, R.L. Exploratory Factor Analysis, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, MI, USA, 1988; ISBN 978-0898592023. [Google Scholar]
- MacCallum, R.C.; Widaman, K.F.; Zhang, S.; Hong, S. Sample size in factor analysis. Psychol. Methods 1999, 4, 84. [Google Scholar] [CrossRef]
- Fabrigar, L.R.; Wegener, D.T. Understanding Statistics: Exploratory Factor Analysis; Oxford University Press: New York, NY, USA, 2012. [Google Scholar]
- SAS Institute Inc. SAS® Studio 3.8: User’s Guide; SAS Institute Inc.: Cary, NC, USA, 2018. [Google Scholar]
- De Sherbinin, A.; Bardy, G. Social vulnerability to floods in two coastal megacities: New York City and Mumbai. Vienna Yearb. Popul. Res. 2015, 13, 131–166. [Google Scholar] [CrossRef] [Green Version]
- Thornton, P.K.; Jones, P.G.; Owiyo, T.; Kruska, R.L.; Herrero, M.; Orindi, V.; Bhadwal, S.; Kristjanson, P.; Notenbaert, A.; Bekele, N. Climate change and poverty in Africa: Mapping hotspots of vulnerability. Afr. J. Agric. Resour. Econ. 2008, 2, 24–44. [Google Scholar]
- Tabachnick, B.G.; Fidell, L.S. A Practical Approach to Using Multivariate Analyses; Pearson: Boston, MA, USA, 2012. [Google Scholar]
- Menezes, J.A.; Madureira, A.P.; Santos, R.B.D.; Duval, I.D.B.; Regoto, P.; Margonari, C.; Confalonieri, U. Data for: Analyzing Spatial Patterns of Health Vulnerability to Drought in the Brazilian Semiarid Region; Mendeley Data, V1; Elsevier: Amsterdam, The Netherlands, 2020. [Google Scholar] [CrossRef]
- Freitas, C.; Silva, D.; Sena, A.; Silva, E.; Sales, L.; Carvalho, M.; Mazoto, M.; Barcellos, C.; Costa, A.; Oliveira, M.; et al. Desastres naturais e saúde: Uma análise da situação do Brasil. Cien. Saude Colet. 2014, 19, 3645–3656. [Google Scholar] [CrossRef] [Green Version]
- Bortolotto, C.C.; De Mola, C.L.; Tovo-Rodrigues, L. Qualidade de vida em adultos de zona rural no Sul do Brasil: Estudo de base populacional. Rev. Saude Publica 2018, 52, 4s. [Google Scholar] [CrossRef]
- Instituto Brasileiro de Geografia e Estatística—IBGE. Pesquisa Nacional de Saúde 2013: Percepção do Estado de Saúde, Estilos de Vida e Doenças Crônicas; Fiocruz, IBGE, Ministério da Saúde: Rio de Janeiro, Brazil, 2014.
- Moreira, J.P.d.L.; de Oliveira, B.L.C.A.; Muzi, C.D.; Cunha, C.L.F.; Brito, A.d.S.; Luiz, R.R. A saúde dos trabalhadores da atividade rural no Brasil. Cad. Saude Publica 2015, 31, 1698–1708. [Google Scholar] [CrossRef] [Green Version]
- Instituto Nacional Do Semiárido—INSA. Portal da Desertificação: Dados e Indicadores do Semiárido Brasileiro. Available online: https://portaldadesertificacao.insa.gov.br/ (accessed on 21 April 2021).
- De Albuquerque, M.V.; d’Ávila Viana, A.L.; De Lima, L.D.; Ferreira, M.P.; Fusaro, E.R.; Iozzi, F.L. Regional health inequalities: Changes observed in Brazil from 2000–2016. Cienc. Saude Coletiva 2017, 22, 1055–1064. [Google Scholar] [CrossRef] [Green Version]
- Cunha, A.M.P.d.A.; Brito, S.S.d.B.; Rossato, L.; Célia dos Santos Alvalá, R.; Carvalho, M.A.; Zeri, M.; Cunningham, C.; Paula dos Reis Maciel, A.; Soares Andrade, E.; Marcia da Silva Pinto Vieira, R.; et al. Avaliação de indicador para o monitoramento dos impacos da seca em áreas de pastagens no Semiárido do Brasil. Rev. Bras. Cartogr. 2017, 69, 89–106. [Google Scholar]
- Lemos, M.C.; Lo, Y.J.; Nelson, D.R.; Eakin, H.; Bedran-Martins, A.M. Linking development to climate adaptation: Leveraging generic and specific capacities to reduce vulnerability to drought in NE Brazil. Glob. Environ. Chang. 2016, 39, 170–179. [Google Scholar] [CrossRef] [Green Version]
- Christenson, E.; Elliott, M.; Banerjee, O.; Hamrick, L.; Bartram, J. Climate-related hazards: A method for global assessment of urban and rural population exposure to cyclones, droughts, and floods. Int. J. Environ. Res. Public Health 2014, 11, 2169–2192. [Google Scholar] [CrossRef]
- Tibesigwa, B.; Visser, M. Assessing gender inequality in food security among small-holder farm households in urban and rural South Africa. World Dev. 2016, 88, 33–49. [Google Scholar] [CrossRef]
- Tibesigwa, B.; Visser, M.; Collinson, M.; Twine, W. Investigating the sensitivity of household food security to agriculture-related shocks and the implication of social and natural capital. Sustain. Sci. 2016, 11, 193–214. [Google Scholar] [CrossRef]
- Articulação Semiárido Brasileiro—ASA. Propostas da Sociedade Civil Para Garantia de Acesso à Água às Populações Rurais do Semiárido; Semiárido—Caderno de Debates; Articulação Semiárido Brasileiro—ASA: Recife, Brazil, 2019; Available online: https://www.yumpu.com/pt/document/read/62697726/frente-parlamentar-propostas-da-sociedade-civil-para-a-garantia-do-acesso-a-agua-as-populacoes-rurais-do-semiarido (accessed on 21 April 2020).
- Adler, N.E.; Boyce, W.T.; Chesney, M.A.; Folkman, S.; Syme, S.L. Socioeconomic Inequalities in Health: No Easy Solution. JAMA 1993, 269, 3140–3145. [Google Scholar] [CrossRef]
- Kunst, A.E.; Geurts, J.J.M.; Van Den Berg, J. International variation in socioeconomic inequalities in self reported health. J. Epidemiol. Community Health 1995, 49, 117–123. [Google Scholar] [CrossRef] [Green Version]
- Szwarcwald, C.L.; de Souza-Júnior, P.R.B.; Esteves, M.A.P.; Damacena, G.N.; Viacava, F. Socio-demographic determinants of self-rated health in Brazil. Cad. Saúde Pública/Ministério da Saúde Fundação Oswaldo Cruz Esc. Nac. Saúde Pública 2005, 21, 54–64. [Google Scholar] [CrossRef] [Green Version]
- Almeida, G.; Sarti, F.M.; Ferreira, F.F.; Diaz, M.D.M.; Campino, A.C.C. Analysis of the evolution and determinants of income-related inequalities in the Brazilian health system, 1998–2008. Rev. Panam. Salud Publica 2013, 33, 90–97. [Google Scholar] [CrossRef] [Green Version]
- Carstairs, V. Deprivation indices: Their interpretation and use in relation to health. J. Epidemiol. Community Health 1995, 49, S3–S8. [Google Scholar] [CrossRef] [Green Version]
- Barcellos, C.d.D.; Sabroza, P.C.; Peiter, P.; Rojas, L.I. Organização Espacial, Saúde e Qualidade de Vida: Análise Espacial e Uso de Indicadores na Avaliação de Situações de Saúde. Inf. Epidemiológico SUS 2002, 11, 129–138. [Google Scholar] [CrossRef]
- Yang, K.; LeJeune, J.; Alsdorf, D.; Lu, B.; Shum, C.K.; Liang, S. Global distribution of outbreaks of water-associated infectious diseases. PLoS Negl. Trop. Dis. 2012, 6, e1483. [Google Scholar] [CrossRef] [Green Version]
- Da Silva, J.M.C.; Leal, I.R.; Tabarelli, M. Caatinga—The Largest Tropical Dry Forest Region in South America, 1st ed.; da Silva, J.M.C., Leal, I.R., Tabarelli, M., Eds.; Springer International Publishing: Cham, Switzerland, 2017; ISBN 9783319683386. [Google Scholar]
- Da Silva, T.C.G.; Silva, C.C.M.; Paes, N.A. Mortalidade dos Adultos por Doenças Cardiovasculares e Fatores Associados no Semiárido Brasileiro. Rev. Espaço Para Saúde 2015, 16, 74–86. [Google Scholar] [CrossRef] [Green Version]
- Szwarcwald, C.L.; de Souza Júnior, P.R.B.; Marques, A.P.; de Almeida, W.d.S.; Montilla, D.E.R. Inequalities in healthy life expectancy by Brazilian geographic regions: Findings from the National Health Survey, 2013. Int. J. Equity Health 2016, 15, 141. [Google Scholar] [CrossRef] [Green Version]
- Rufino, I.A.A.; Da Silva, S.T. Análise das relações entre dinâmica populacional, clima e vetores de mudança no Semiárido Basileiro: Uma abordagem metodológica. Bol. Ciencias Geod. 2017, 23, 166–181. [Google Scholar] [CrossRef]
- Duarte, M.M.S. Cobertura das Ações de Vigilância da Qualidade da Água para Consumo Humano e Indicadores de Vulnerabilidade nos Municípios do Semiárido Nordestino, Universidade de Brasília. 2018. Available online: https://1library.org/document/zln3e3lq-cobertura-vigilancia-qualidade-indicadores-vulnerabilidade-municipios-semiarido-nordestino.html (accessed on 21 April 2021).
- Weiss, R.A.; McMichael, A.J. Social and environmental risk factors in the emergence of infectious diseases. Nat. Med. 2004, 10, S70–S76. [Google Scholar] [CrossRef]
- Hacon, S.d.S.; Costa, D.; Siqueira, A.S.P.; Pinheiro, S.d.L.; Gonçalves, K.S.; Oliveira, A.; Barcellos, C. Vulnerabilidade, riscos e impactos das mudanças climáticas sobre a saúde no Brasil. In Modelagem Climática e Vulnerabilidades Setoriais à Mudança do Clima no Brasil; Ministério da Ciência, Tecnologia e Inovação: Brasília, Brazil, 2016; pp. 387–456. [Google Scholar]
- De Oliveira, A.P.C.; Gabriel, M.; Dal Poz, M.R.; Dussault, G. Desafios para assegurar a disponibilidade e acessibilidade à assistência médica no Sistema Único de Saúde. Cienc. Saude Coletiva 2017, 22, 1165–1180. [Google Scholar] [CrossRef] [PubMed]
- Garnelo, L.; Lima, J.G.; Rocha, E.S.C.; Herkrath, F.J. Acesso e cobertura da Atenção Primária à Saúde para populações rurais e urbanas na região norte do Brasil. Saúde Debate 2018, 42, 81–99. [Google Scholar] [CrossRef] [Green Version]
- Massuda, A.; Hone, T.; Leles, F.A.G.; De Castro, M.C.; Atun, R. The Brazilian health system at crossroads: Progress, crisis and resilience. BMJ Glob. Health 2018, 3, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hone, T.; Rasella, D.; Barreto, M.; Atun, R.; Majeed, A.; Millett, C. Large reductions in amenable mortality associated with brazil’s primary care expansion and strong health governance. Health Aff. 2017, 36, 149–158. [Google Scholar] [CrossRef]
- Instituto de Pesquisa Econômica Aplicada—IPEA. Atlas da Vulnerabilidade Social nos Municípios Brasileiros; Costa, M.A., Marguti, B.O., Eds.; IPEA: Brasília, Brazil, 2015; ISBN 978-85-7811-255-4. [Google Scholar]
- Programa das Nações Unidas para o Desenvolvimento—PNUD; Instituto de Pesquisa Econômica Aplicada—IPEA; Fundação João Pinheiro—FJP. Índice de Desenvolvimento Humano Municipal Brasileiro; PNUD: Brasília, Brazil, 2013. [Google Scholar]
- Instituto Brasileito de Geografia e Estatístca—IBGE. Cidades@. [No Date]. Available online: https://cidades.ibge.gov.br/ (accessed on 20 April 2020).
- Marengo, J.A.; Cunha, A.P.; Soares, W.R.; Torres, R.R.; Alves, L.M.; de Barros Brito, S.S.; Cuartas, L.A.; Leal, K.; Neto, G.R.; Alvalá, R.C.S.; et al. Increase Risk of Drought in the Semiarid Lands of Northeast Brazil Due to Regional Warming above 4 °C. In Climate Change Risks in Brazil; Nobre, C., Marengo, J., Soares, W., Eds.; Springer: Cham, Switzerland, 2019; pp. 181–200. [Google Scholar]
- Papathoma-Köhle, M.; Cristofari, G.; Wenk, M.; Fuchs, S. The importance of indicator weights for vulnerability indices and implications for decision making in disaster management. Int. J. Disaster Risk Reduct. 2019, 36, 101103. [Google Scholar] [CrossRef]
- Willis, I.; Fitton, J. A review of multivariate social vulnerability methodologies: A case study of the River Parrett catchment, UK. Hazards Earth Syst. Sci 2016, 16, 1387–1399. [Google Scholar] [CrossRef] [Green Version]
- Becker, W.; Saisana, M.; Paruolo, P.; Vandecasteele, I. Weights and importance in composite indicators: Closing the gap. Ecol. Indic. 2017, 80, 12–22. [Google Scholar] [CrossRef]
| Dimension | Indicator | Variable | Source |
|---|---|---|---|
| Socio-economic | Income below the poverty line | % of households with per capita nominal monthly income (BRL) of up to 1/2 minimum wage in 2010 | Demographic census–IBGE |
| Per capita income | Value in BRL of average household income per capita in 2010 | Demographic census–IBGE | |
| Ratio between rural and urban population | Resident population whose household situation was rural in 2010 | ||
| Resident population whose household situation was urban in 2010 | |||
| Population with complete primary education or more | % population aged 15 years or older with a completed 2nd elementary school or more in 2010 | ||
| Illiterate population | % population aged 15 years and older with no education in 2010 | ||
| Survival probability | Likelihood of a newborn child living up to 40 years if the level and pattern of mortality by age of the 2010 Census remain constant throughout life | Atlas of Human Development in Brazil | |
| Illiterate female heads of household | % of households in which the woman was responsible and illiterate in 2010 | Demographic census–IBGE | |
| Dependency ratio | % of people living in households with a dependency ratio > 75% in 2010 | Atlas of Human Development in Brazil | |
| Unemployment rate | Unemployment rate of people aged 16 years and older in 2010 | Demographic census–IBGE | |
| Population employed in agriculture | % of the employed population in the agricultural sector aged 18 years or older in 2010 | Atlas of Human Development in Brazil | |
| Municipal population engaged in family farming | % of establishments presenting a declaration of suitability to PRONAF (National Program for Strengthening Family Agriculture) in 2017 | Agricultural Census–IBGE | |
| Rural establishments where the producer is an association member | % of establishments in which the producer is associated with a cooperative or class entity in 2017 | Agricultural Census–IBGE | |
| Rural establishments with irrigated agriculture | % of establishments with irrigated agriculture in 2017 | Agricultural Census–IBGE | |
| Rural establishments with access to water | % of establishments with rivers/streams protected by riparian forest in 2017 | Agricultural Census–IBGE | |
| Rural population with access to water technology | Number of rural households served by water access technologies (i.e., consumer cisterns, storage tanks) in 2019 | National Semiarid Institute–INSA | |
| Socio-environmental | Demographic density | Resident population in 2017 | IBGE |
| Municipal area in km2 | National Semiarid Institute–INSA | ||
| Drought index | SPI-12 frequency and duration. Methodology adapted from [48]. Standardized Precipitation Index (SPI) is the most commonly used indicator worldwide for detecting and characterizing meteorological droughts, based on a comparison of observed total precipitation amounts for an accumulation period of interest (e.g., 1, 3, 12, 48 months) | CHIRPS | |
| Number of drought events recorded between 2003 and 2015 | National Water Agency—ANA | ||
| Change in agricultural participation in gross domestic product (GDP) | Gross change in income obtained through work in the rural area between 1999 and 2012 | National Semiarid Institute—INSA | |
| Population with access to sanitation | % of households with general sewerage or septic tank in 2010 | Demographic census—IBGE | |
| Population with access to piped water | % of households with public water supply in 2010 | ||
| Health conditions and systems | Dengue index | Incidence rate, temporal trend, and proportion of cases between 2001 and 2015. Adapted from [26,31] | DATASUS |
| Hepatitis A index | |||
| Asthma admissions rate | Hospital admission rate, temporal trend, and proportion of cases between 2001 and 2015. Adapted from [26,31] | ||
| Malnutrition admissions rate | |||
| Skin infections admissions | |||
| Mental disorders admissions | |||
| Diarrhea admissions | |||
| Admissions sensitive to primary care | % of hospitalizations for conditions sensitive to primary care in 2015 (a set of health problems for which the effective action of primary care would decrease the risk of hospitalizations) | ||
| Infant mortality up to 5 years | Probability of dying between birth and the exact age of 5, per 1000 children born alive in 2010 | Atlas of Human Development in Brazil | |
| Number of beds/inhabitants | Total outpatient, emergency, intensive care, and hospitalization beds per 1000 inhabitants in 2015 | DATASUS | |
| Health professionals per inhabitant | Number of registered health professionals in the public and private sectors per 1000 inhabitants in 2015 | ||
| % population covered by health insurance | Number of health plan beneficiaries that contain hospital and/or outpatient segmentation, and may also contain dental assistance in 2015 | National Supplementary Health Agency | |
| Estimated population in 2015 | IBGE |
| Factor Name | Indicator | Factor Loading | Explained Variance (%) | Cardinality |
|---|---|---|---|---|
| Health and its social determinants | Average household per capita income | 0.803 | 51.8 | + |
| % population with complete primary education or more | 0.705 | |||
| % population covered by health plans | 0.488 | |||
| Survival probability | 0.469 | |||
| Demographic density | 0.448 | |||
| % of households with access to sanitation | 0.427 | |||
| Health professionals per 1000 inhabitants | 0.421 | |||
| Dengue index | 0.393 | |||
| Skin infections admissions | 0.337 | |||
| Hepatitis index | 0.245 | |||
| Mental disorders admissions | 0.203 | |||
| Infant mortality | −0.438 | |||
| Dependency ratio | −0.459 | |||
| % of the population employed in agriculture | −0.666 | |||
| % households with monthly income per capita up to ½ salary | −0.685 | |||
| % population illiterate | −0.693 | |||
| Rural economy and access to water | % rural households with water related technologies | 0.639 | 13.2 | + |
| Rural urban ratio | 0.456 | |||
| Drought index | 0.397 | |||
| Unemployment rate | −0.315 | |||
| % rural establishments with irrigation | −0.319 | |||
| % change in agricultural participation in GDP | −0.354 | |||
| % households with access to piped water | −0.707 | |||
| Health problems and infrastructure | Asthma admissions | 0.783 | 10.1 | + |
| Undernutrition admissions | 0.569 | |||
| Diarrhea admissions | 0.520 | |||
| Admissions sensitive to primary care | 0.520 | |||
| Beds per 1000 inhabitants | 0.387 | |||
| Rural structure and social capital | % family farming establishments | 0.615 | 9.2 | + |
| % rural establishments associated with a cooperative or class entity | 0.418 | |||
| % establishments with water resources | 0.312 | |||
| % of households with female heads of household illiterate | −0.540 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Menezes, J.A.; Madureira, A.P.; Santos, R.B.d.; Duval, I.d.B.; Regoto, P.; Margonari, C.; Barata, M.M.d.L.; Confalonieri, U. Analyzing Spatial Patterns of Health Vulnerability to Drought in the Brazilian Semiarid Region. Int. J. Environ. Res. Public Health 2021, 18, 6262. https://doi.org/10.3390/ijerph18126262
Menezes JA, Madureira AP, Santos RBd, Duval IdB, Regoto P, Margonari C, Barata MMdL, Confalonieri U. Analyzing Spatial Patterns of Health Vulnerability to Drought in the Brazilian Semiarid Region. International Journal of Environmental Research and Public Health. 2021; 18(12):6262. https://doi.org/10.3390/ijerph18126262
Chicago/Turabian StyleMenezes, Júlia Alves, Ana Paula Madureira, Rhavena Barbosa dos Santos, Isabela de Brito Duval, Pedro Regoto, Carina Margonari, Martha Macêdo de Lima Barata, and Ulisses Confalonieri. 2021. "Analyzing Spatial Patterns of Health Vulnerability to Drought in the Brazilian Semiarid Region" International Journal of Environmental Research and Public Health 18, no. 12: 6262. https://doi.org/10.3390/ijerph18126262
APA StyleMenezes, J. A., Madureira, A. P., Santos, R. B. d., Duval, I. d. B., Regoto, P., Margonari, C., Barata, M. M. d. L., & Confalonieri, U. (2021). Analyzing Spatial Patterns of Health Vulnerability to Drought in the Brazilian Semiarid Region. International Journal of Environmental Research and Public Health, 18(12), 6262. https://doi.org/10.3390/ijerph18126262






