Gender Differences in the Prevalence of Mental Health, Psychological Distress and Psychotropic Medication Consumption in Spain: A Nationwide Population-Based Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Study Population
2.2. Study Variables
- Mental health status was measured using three dependent variables:
- The self-reported presence of a “mental disorder”, defined as the person interviewed reporting suffering from depression and/or anxiety, with these conditions having been diagnosed by a medical professional;
- The variable “psychotropic drug consumption”, created using questions regarding the self-reported use of physician-prescribed medications in the last two weeks. We considered any of the following as psychiatric medications: “tranquilizers (anxiolytics)”, “sedatives (anxiolytics)”, “sleeping pills (anxiolytics)” and “antidepressants”.
- Independent variables included were classified into four types:
2.3. Statistical Analysis
2.4. Ethical Aspects
3. Results
3.1. Distribution of Characteristics of the Study Population
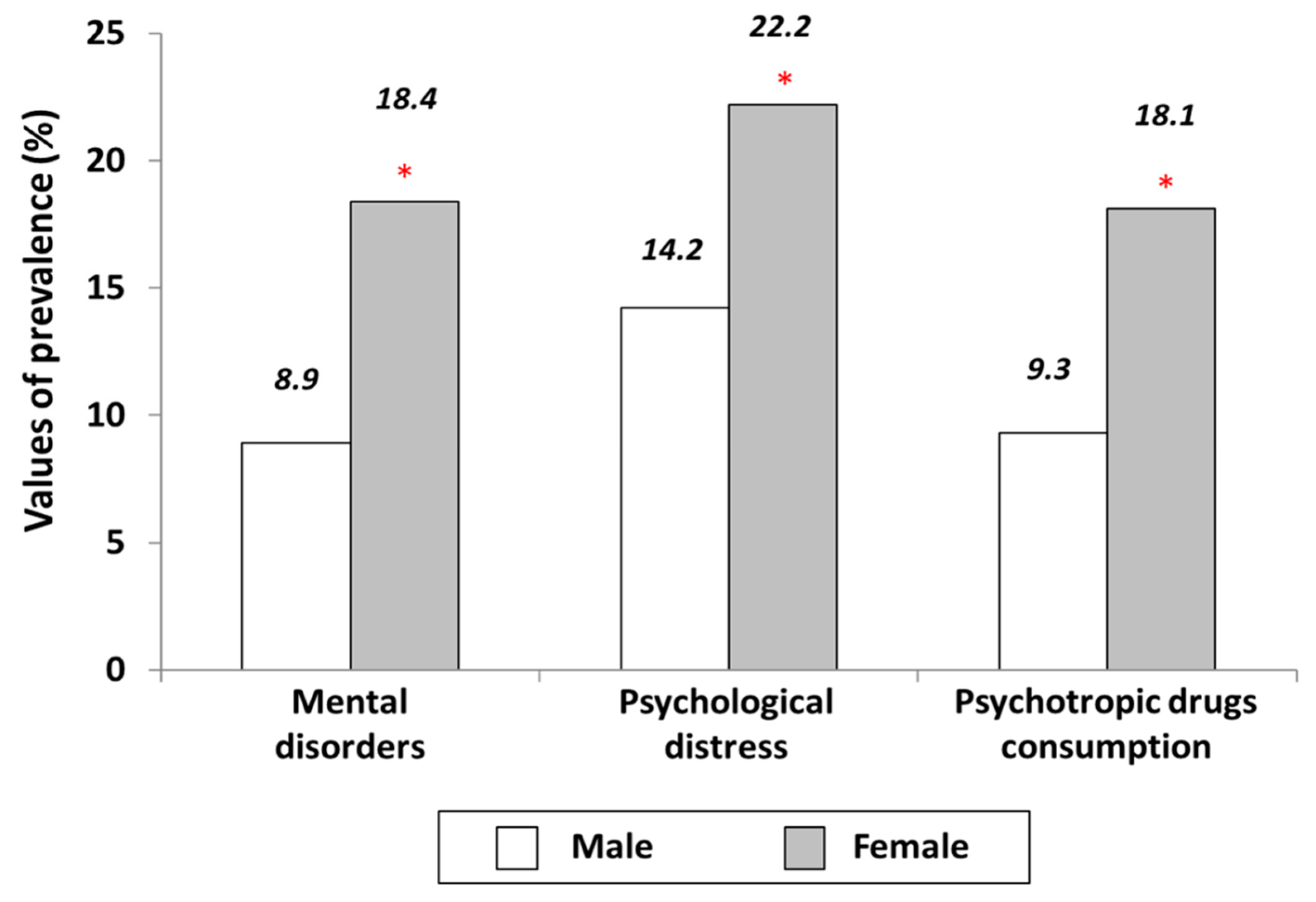
3.2. Prevalence of Mental Health Disorders, Psychiatric Distress and Psychotropic Drug Consumption According to Sociodemographic Variables. Comparison between Men and Women
3.3. Prevalence of Mental Health Disorders, Psychiatric Distress and Psychotropic Drug Consumption According to Health Status. Comparison between Men and Women
3.4. Prevalence of Mental Health Disorders, Psychiatric Distress and Psychotropic Drug Consumption According to Use of Healthcare Services and Lifestyle-Related Variables. Comparison between Men and Women
3.5. Variables Associated to Mental Health Disorders, Psychiatric Distress and Psychotropic Drug Consumption after Multivariable Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ritchie, H.; Roser, M. Mental Health. Available online: https://ourworldindata.org/mental-health (accessed on 29 March 2021).
- WHO. Global Burden of Disease; World Health Organization: Geneva, Switzerland, 2004; Available online: http://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf (accessed on 29 March 2021).
- Alonso, J.; Ferrer, M.; Romera, B.; Vilagut, G.; Angermeyer, M.; Bernert, S.; Brugha, T.; Taub, N.; McColgen, Z.; Girolamo, G.; et al. The European Study of the Epidemiology of Mental Disorders (ESEMeD/MHEDEA 2000) project: Rationale and methods. Int. J. Methods Psychiatr. Res. 2002, 11, 55–67. [Google Scholar] [CrossRef]
- Alonso, J.; Lépine, J.-P. Overview of key data from the European Study of the Epidemiology of Mental Disorders (ESEMeD). J. Clin. Psychiatry 2007, 68, 3–9. [Google Scholar]
- Gabilondo, A.; Rojas-Farreras, S.; Vilagut, G.; Haro, J.M.; Fernández, A.; Pinto-Meza, A.; Alonso, J. Epidemiology of major depressive episode in a southern European country: Results from the ESEMeD-Spain project. J. Affect. Disord. 2010, 120, 76–85. [Google Scholar] [CrossRef] [Green Version]
- Gili, M.; Roca, M.; Basu, S.; McKee, M.; Stuckler, D. The mental health risks of economic crisis in Spain: Evidence from primary care centers, 2006 and 2010. Eur. J. Public Health 2012, 23, 103–108. [Google Scholar] [CrossRef]
- Navarro-Mateu, F.; Tormo, M.J.; Salmeron, D.; Vilagut, G.; Navarro, C.; Ruiz-Merino, G.; Escámez, T.; Júdez, J.; Martinez, S.; Kessler, R.C.; et al. Prevalence of Mental Disorders in the South-East of Spain, One of the European Regions Most Affected by the Economic Crisis: The Cross-Sectional PEGASUS-Murcia Project. PLoS ONE 2015, 10, e0137293. [Google Scholar] [CrossRef] [PubMed]
- OECD. Promoting mental health in Europe: Why and how? In Health at a Glance: Europe; Organization for Economic Co-Operation and Development (OECD): Paris, France, 2018; pp. 19–43. [Google Scholar]
- Sánchez, M.P.V.; Saint-Gerons, D.M.; Honrubia, C.D.L.F.; Bermejo, C.E.O.; Corominas, D.M.; Catalá-López, F. Evolución del uso de medicamentos ansiolíticos e hipnóticos in Spain durante el período 2000-2011. Rev. Esp. Salud Pública 2013, 87, 247–255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rubio-Valera, M.; Fernández, A.; Luciano, J.V.; Hughes, C.M.; Pinto-Meza, A.; Moreno-Küstner, B.; Palao, D.J.; Haro, J.M.; Serrano-Blanco, A. Psychotropic prescribing in Catalonia: Results from an epidemiological study. Fam. Pr. 2011, 29, 154–162. [Google Scholar] [CrossRef] [Green Version]
- Carrasco-Garrido, P.; Hernández-Barrera, V.; Jiménez-Trujillo, I.; Esteban-Hernández, J.; Álvaro-Meca, A.; Andrés, D.; DelBarrio-Fernández, J.L.; Garcia, R.J. Time Trend in Psychotropic Medication Use in Spain: A Nationwide Population-Based Study. Int. J. Approx. Res. Public Health 2016, 13, 1177. [Google Scholar] [CrossRef] [PubMed]
- Aparasu, R.R.; Death, J.R.; Brandt, H. Psychotropic prescription use by community-dwelling elderly in the United States. J. Am. Geriatr. Soc. 2003, 51, 671–677. [Google Scholar] [CrossRef]
- Voyer, P.; Cohen, D.; Lauzon, S.; Collin, J. Factors associated with psychotropic drug use among community-dwelling older persons: A review of empirical studies. BMC Nurs. 2004, 3, 3. [Google Scholar] [CrossRef] [Green Version]
- Wang, P.S.; Lane, M.; Olfson, M.; Pincus, H.A.; Wells, K.B.; Kessler, R.C. Twelve-Month Use of Mental Health Services in the United States. Arch. Gen. Psychiatry 2005, 62, 629–640. [Google Scholar] [CrossRef] [Green Version]
- Carrasco, P.; Astasio, P.; Ortega, P.; Jiménez, R.; Gil, A. Factores asociados al consumo de fármacos psicotropos en la población adulta española. Datos obtained from the Encuestas Nacionales de Salud de España de los años 1993, 1995 y 1997. Med. Clin. 2001, 116, 324–329. [Google Scholar] [CrossRef]
- Carrasco-Garrido, P.; Lopez-De-Andres, A.; Barrera, V.H.; Jiménez-Trujillo, I.; Garcia, R.J. National trends (2003–2009) and factors related to psychotropic medication use in community-dwelling elderly population. Int. Psychogeriatr. 2012, 25, 328–338. [Google Scholar] [CrossRef] [PubMed]
- Salvador-Carulla, L.; Roca, M. Mental health impact of the economic crisis in Spain. Int. Psychiatry 2013, 10, 8–10. [Google Scholar]
- Cuesta, J.D.P.; Ruiz, J.S.; Roca, M.; Noguer, I. Salud mental y salud pública en España: Vigilancia epidemiológica y prevención. Psiquiatr. Biol. 2016, 23, 67–73. [Google Scholar] [CrossRef] [Green Version]
- Garcia, R.J.; Huedo, M.A.M.; Hernandez-Barrera, V.; Andrés, A.L.; Martinez, D.; Jiménez-Trujillo, I.; Carrasco-Garrido, P.; Jiménez-García, R.; Hernandez-Barrera, V. Psychological Distress and mental disorders among Spanish diabetic adults: A case—control study. Prim. Care Diabetes 2012, 6, 149–156. [Google Scholar] [CrossRef]
- Goldberg, D.; Williams, P. User’s Guide to the General Health Questionnaire; NFER-Nelson: Berkshire, UK, 1988. [Google Scholar]
- Muñóz, P.E.; Vázquez, J.L.; Rodríguez Insausti, F.; Pastrana, E.; Varo, J. Adaptación española del General Health Questionnaire (GHQ) by DP Goldberg (a method of identificación de casos psiquiátricos en la comunidad [Spanish adaptation of the General Health Questionnaire (GHQ) of DP Goldberg (a method for identifying psychiatric cases in the community)]. Arch. Neurobiol. 1979, 42, 139–158. [Google Scholar]
- Sánchez-López, P.; Dresch, V. The 12-item General Health Questionnaire (GHQ-12): Reliability, external validity and factor structure in the Spanish population. Psicothema 2008, 20, 839–843. [Google Scholar]
- Gispert, R.; Rajmil, L.; Schiaffino, A.; Herdman, M. Sociodemographic and health-related correlates of psychiatric distress in a general population. Soc. Psychiatry Psychiatr. Epidemiol. 2003, 38, 677–683. [Google Scholar] [CrossRef]
- Instituto Nacional de Estadistica. Encuesta Nacional de Salud 2017. [National Health Survey 2017]. Available online: https://www.ine.es/en/metodologia/t15/t153041917_en.pdf (accessed on 12 February 2021).
- Instituto Nacional de Estadistica. Encuesta Nacional de Salud 2017. Cuestinario de Adultos [National Health Survey 2017. Adults Questionnaire]. Available online: https://www.ine.es/metodologia/t15/ense_adu17.pdf (accessed on 11 March 2020).
- Ministerio de Sanidad Consumo y Bienestar Social. Encuesta Nacional de Salud. 2017. Microdatos. [National Health Survey 2017. Microdata]. Available online: https://www.mscbs.gob.es/estadisticas/microdatos.do (accessed on 18 February 2021).
- Henares-Montiel, J.; Ruiz-Pérez, I.; Sordo, L. Salud mental en España y diferencias por sexo y por comunidades autónomas. Gac. Sanit. 2020, 34, 114–119. [Google Scholar] [CrossRef]
- Munizza, C.; Argentero, P.; Coppo, A.; Tibaldi, G.; Di Giannantonio, M.; Picci, R.L.; Rucci, P. Public Beliefs and Attitudes towards Depression in Italy: A National Survey. PLoS ONE 2013, 8, e63806. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stoyanova, A.; Pinilla, J. Socioeconomic Burden of Mental Disorders in Spain 2006–2017 (3 April 2019). UB Economics Working Papers E19/389. Available online: https://ssrn.com/abstract=3369466 (accessed on 18 February 2021).
- Cebrino, J.; De La Cruz, S.P. Environmental, Health and Sociodemographic Determinants Related to Common Mental Disorders in Adults: A Spanish Country-Wide Population-Based Study (2006–2017). J. Clin. Med. 2020, 9, 2199. [Google Scholar] [CrossRef]
- Von Soest, T.; Bramness, J.G.; Pedersen, W.; Wichstrøm, L. The relationship between socio-economic status and antidepressant prescription: A longitudinal survey and register study of young adults. Epidemiol. Psychiatr. Sci. 2011, 21, 87–95. [Google Scholar] [CrossRef]
- Abbing-Karahagopian, V.; Huerta, C.; Souverein, P.C.; de Abajo, F.; Leufkens, H.G.M.; Slattery, J.; Alvarez, Y.; Miret, M.; Gil, M.; Oliva, B.; et al. Antidepressant prescribing in five European countries: Application of common definitions to assess the prevalence, clinical observations, and methodological implications. Eur. J. Clin. Pharmacol. 2014, 70, 849–857. [Google Scholar] [CrossRef] [PubMed]
- Mojtabai, R.; Olfson, M. National Trends in Psychotropic Medication Polypharmacy in Office-Based Psychiatry. Arch. Gen. Psychiatry 2010, 67, 26–36. [Google Scholar] [CrossRef] [PubMed]
- Meng, X.; D’Arcy, C.; Tempier, R. Trends in Psychotropic Use in Saskatchewan from 1983 to 2007. Can. J. Psychiatry 2013, 58, 426–431. [Google Scholar] [CrossRef] [Green Version]
- Manteuffel, M.; Williams, S.; Chen, W.; Verbrugge, R.R.; Pittman, D.G.; Steinkellner, A. Influence of Patient Sex and Gender on Medication Use, Adherence, and Prescribing Alignment with Guidelines. J. Women’s Health 2014, 23, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Stuckler, D.; Basu, S.; Suhrcke, M.; Coutts, A.; McKee, M. The public health effect of economic crises and alternative policy responses in Europe: An empirical analysis. Lancet 2009, 374, 315–323. [Google Scholar] [CrossRef]
- Gil-Alonso, F.; Thiers-Quintana, J. Population and economic cycles in the main Spanish urban areas: The migratory component. Comp. Popul. Stud. 2019, 44, 317–350. [Google Scholar] [CrossRef]
- Lee, S.; Guo, W.-J.; Tsang, A.; Mak, A.D.P.; Wu, J.; Ng, K.L.; Kwok, K. Evidence for the 2008 economic crisis exacerbating depression in Hong Kong. J. Affect. Disord. 2010, 126, 125–133. [Google Scholar] [CrossRef]
- Wang, J.; Smailes, E.; Sareen, J.; Fick, G.H.; Schmitz, N.; Patten, S.B. The Prevalence of Mental Disorders in the Working Population over the Period of Global Economic Crisis. Can. J. Psychiatry 2010, 55, 598–605. [Google Scholar] [CrossRef] [Green Version]
- Economou, M.; Madianos, M.; Peppou, L.E.; Patelakis, A.; Stefanis, C.N. Major depression in the Era of economic crisis: A replication of a cross-sectional study across Greece. J. Affect. Disord. 2013, 145, 308–314. [Google Scholar] [CrossRef]
- La Torre, J.-D.; Molina, A.J.; Fernández-Villa, T.; Artazcoz, L.; Martín, V. Mental health, family roles and employment status inside and outside the household in Spain. Gac. Sanit. 2019, 33, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Athanasopoulos, C.; Pitychutis, P.M.; Messari, I.; Lionis, C.; Papadopoulou-Daifoti, Z. Is Drug Utilization in Greece Sex dependent? A Population-based Study. Basic Clin. Pharmacol. Toxicol. 2012, 112, 55–62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carrasco-Garrido, P.; Hernández-Barrera, V.; López de Andrés, A.; Jiménez-Trujillo, I.; Jiménez-García, R. Sex--differences on self-medication in Spain. Pharmacoepidemiol Drug Saf. 2010, 19, 1293–1299. [Google Scholar] [CrossRef]
- Kessler, R.C.; Angermeyer, M.; Anthony, J.C.; Graaf, R.; Demyttenaere, K.; Gasquet, I.; de Girolamo, G.; Gluzman, S.; Gureje, O.; Haro, J.M.; et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry 2007, 6, 168–176. [Google Scholar] [PubMed]
- Carstensen, L.L.; Isaacowitz, D.M.; Charles, S.T. Taking time seriously: A theory of socioemotional selectivity. Am. Psychol. 1999, 54, 165–181. [Google Scholar] [CrossRef] [PubMed]
- Simoni-Wastila, L.; Yang, H.K. Psychoactive drug abuse in older adults. Am. J. Geriatr. Pharmacother. 2006, 4, 380–394. [Google Scholar] [CrossRef]
- Bareis, N.; Sando, T.A.; Mezuk, B.; Cohen, S.A. Association Between Psychotropic Medication Polypharmacy and an Objective Measure of Balance Impairment Among Middle-Aged Adults: Results from the US National Health and Nutrition Examination Survey. CNS Drugs 2018, 32, 863–871. [Google Scholar] [CrossRef] [PubMed]
- Linden, M.; Lecrubier, Y.; Bellantuono, C.; Benkert, O.; Kisely, S.; Simon, G. The prescribing of psychotropic drugs by primary care physicians: An international collaborative study. J. Clin. Psychopharmacol. 1999, 19, 132–140. [Google Scholar] [CrossRef]
- Kjosavik, S.R.; Hunskaar, S.; Aarsland, D.; Ruths, S. Initial prescription of antipsychotics and antidepressants in general practice and specialist care in Norway. Acta Psychiatr. Scand. 2011, 123, 459–465. [Google Scholar] [CrossRef]
- Mercier, A.; Bénichou, J.; Auger-Aubin, I.; Lebeau, J.-P.; Houivet, E.; Van Royen, P.; Peremans, L. How do GP practices and patient characteristics influence the prescription of antidepressants? A cross-sectional study. Ann. Gen. Psychiatry 2015, 14, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, D.R.; Takeuchi, D.T.; Adair, R.K. Marital Status and Psychiatric Disorders Among Blacks and Whites. J. Health Soc. Behav. 1992, 33, 140. [Google Scholar] [CrossRef] [PubMed]
- DistelIrene, M.A.; Rebollo-Mesa, I.; Abdellaoui, A.; Derom, C.A.; Willemsen, G.; Cacioppo, J.T.; Boomsma, D.I. Familial Resemblance for Loneliness. Behav. Genet. 2010, 40, 480–494. [Google Scholar] [CrossRef] [Green Version]
- Bhugra, D.; Jones, P. Migration and mental illness. Adv. Psychiatr. Treat. 2001, 7, 216–222. [Google Scholar] [CrossRef] [Green Version]
- Rivera, B.; Casal, B.; Currais, L. The Healthy Immigrant Effect on Mental Health: Determinants and Implications for Mental Health Policy in Spain. Adm. Policy Ment. Health Lying Health Serv. Res. 2016, 43, 616–627. [Google Scholar] [CrossRef]
- Amponsah, M.O.; Non, U.K. Non-UK university students stress levels and their coping strategies. Educ. Res. 2010, 1, 88–98. [Google Scholar]
- Elgorriaga, E.; Ibabe, I.; Arnoso, A. Spanish migrants to European Union countries: Predictors of psychological adjustment/Españoles que emigran a países de la Unión Europea: Predictores de su ajuste psicológico. Int. J. Soc. Psychol. 2016, 31, 1–35. [Google Scholar] [CrossRef]
- Erlinghagen, M. Nowhere Better Than Here? The Subjective Well-Being of German Emigrants and Remigrants. Comp. Popul. Stud. 2012, 36, 899–926. [Google Scholar] [CrossRef]
- Handlos, L.N.; Olwig, K.F.; Bygbjerg, I.C.; Kristiansen, M.; Norredam, M.L. Return Migration among Elderly, Chronically Ill Bosnian Refugees: Does Health Matter? Int. J. Approx. Res. Public Health 2015, 12, 12643–12661. [Google Scholar] [CrossRef] [PubMed]
- Razum, O.; Sahin-Hodoglugil, N.N.; Polit, K. Health, Wealth or Family Ties? Why Turkish Work Migrants Return from Germany. J. Ethn. Migr. Stud. 2005, 31, 719–739. [Google Scholar] [CrossRef]
- Perry, M.J. The relationship between social class and mental disorder. J. Prim. Prev. 1996, 17, 17–30. [Google Scholar] [CrossRef]
- Bossé, R.; Aldwin, C.M.; Levenson, M.R.; Ekerdt, D.J. Mental health differences among retirees and workers: Findings from the normative aging study. Psychol. Aging 1987, 2, 383–389. [Google Scholar] [CrossRef]
- Eurostat. Euroindicators, News Release. 2017. Available online: http://ec.europa.eu/eurostat/documents/2995521/8357265/3-31102017-CP-EN.pdf/cc23432e-f918-4f93-9fe7-0c03badb9792 (accessed on 18 February 2021).
- Mínguez, A.M. Family and Gender Roles in Spain from a Comparative Perspective. Eur. Soc. 2010, 12, 85–111. [Google Scholar] [CrossRef]
- Verhaak, P.F.; Heijmans, M.J.; Peters, L.; Rijken, M. Chronic disease and mental disorder. Soc. Sci. Med. 2005, 60, 789–797. [Google Scholar] [CrossRef]
- Ng, C.G.; Boks, M.P.; Smeets, H.M.; Zainal, N.Z.; De Wit, N.J. Prescription patterns for psychotropic drugs in cancer patients; a large population study in the Netherlands. Psycho Oncol. 2012, 22, 762–767. [Google Scholar] [CrossRef]
- Martín-López, R.; Pérez-Farinós, N.; Hernández-Barrera, V.; Lopez-De-Andres, A.; Carrasco-Garrido, P.; Garcia, R.J. The association between excess weight and self-rated health and psychological distress in women in Spain. Public Health Nutr. 2011, 14, 1259–1265. [Google Scholar] [CrossRef] [Green Version]
- Hong, S.M.; Hur, Y.-I. Relationship between obesity and depression in Korean adults. Medicine 2017, 96, e9478. [Google Scholar] [CrossRef]
- Konttinen, H.; Van Strien, T.; Männistö, S.; Jousilahti, P.; Haukkala, A. Depression, emotional eating and long-term weight changes: A population-based prospective study. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Chauvet-Gelinier, J.-C.; Roussot, A.; Cottenet, J.; Brindisi, M.-C.; Petit, J.-M.; Bonin, B.; Vergès, B.; Quantin, C. Depression and obesity, data from a national administrative database study: Geographic evidence for an epidemiological overlap. PLoS ONE 2019, 14, e0210507. [Google Scholar] [CrossRef]
- Gortmaker, S.L.; Must, A.; Perrin, J.M.; Sobol, A.M.; Dietz, W.H. Social and Economic Consequences of Overweight in Adolescence and Young Adulthood. N. Engl. J. Med. 1993, 329, 1008–1012. [Google Scholar] [CrossRef] [Green Version]
- Ball, K.; Crawford, D.; Kenardy, J. Longitudinal Relationships Among Overweight, Life Satisfaction, and Aspirations in Young Women. Obes. Res. 2004, 12, 1019–1030. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, S.; Gottlieb, B.H. Underwood LG. Social relationship and health. In Social Support Measurement and Intervention: A Guide for Health and Social Scientist; Oxford University Press: Oxford, UK, 2000; pp. 3–25. [Google Scholar]
- Caron, J.; Guay, S. Social support and mental health: Concept, measures, recent research and implications for clinicians. Ment. Health Que. 2005, 30, 15–41. [Google Scholar] [CrossRef] [Green Version]
- Boksa, P. Smoking, psychiatric illness and the brain. J. Psychiatry Neurosci. 2017, 42, 147–149. [Google Scholar] [CrossRef] [Green Version]
- Álvarez, F.J.; Rio, M.C. Gender Differences in Patterns of Alcohol Consumption in Spain. Alcohol. Clin. Exp. Res. 1994, 18, 1342–1347. [Google Scholar] [CrossRef] [PubMed]
- Payton, A.R. Mental Health, Mental Illness, and Psychological Distress: Same Continuum or Distinct Phenomena? J. Health Soc. Behav. 2009, 50, 213–227. [Google Scholar] [CrossRef] [PubMed]
- Teplin, L.A. The prevalence of severe mental disorder among male urban jail detainees: Comparison with the Epidemiologic Catchment Area Program. Am. J. Public Health 1990, 80, 663–669. [Google Scholar] [CrossRef] [Green Version]
| Mental Disorders | Psychological Distress | Psychotropic Drug Consumption | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | Men | Women | p Value | Men | Women | p Value | Men | Women | p Value |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||||
| Age (years) a,b,c | |||||||||
| 18–37 | 154 (5.4) | 254 (9.1) | <0.001 | 314 (11.1) | 482 (17.5) | <0.001 | 107 (3.8) | 131 (4.7) | 0.098 |
| 38–49 | 232 (7.9) | 416 (14.2) | <0.001 | 405 (14.0) | 570 (19.6) | <0.001 | 220 (7.5) | 319 (10.9) | <0.001 |
| 50–67 | 351 (11.1) | 735 (22.6) | <0.001 | 488 (15.6) | 754 (23.4) | <0.001 | 352 (11.2) | 706 (21.7) | <0.001 |
| >67 | 221 (12.0) | 692 (28.6) | <0.001 | 308 (17.2) | 686 (29.2) | <0.001 | 325 (17.7) | 908 (37.5) | <0.001 |
| Nationality a,b,c | |||||||||
| Spanish | 911 (9.6) | 1932 (19.7) | <0.001 | 1392 (14.9) | 2188 (22.6) | <0.001 | 948 (10.0) | 1925 (19.6) | <0.001 |
| Other | 47 (3.6) | 165 (10.6) | <0.001 | 123(9.2) | 304 (19.8) | <0.001 | 56 (4.3) | 139 (8.9) | <0.001 |
| Marital status a,b,c | |||||||||
| Married | 530 (7.6) | 1117 (16.9) | <0.001 | 900 (13.1) | 1352 (20.6) | <0.001 | 652 (9.4) | 1127 (17.0) | <0.001 |
| Others | 428 (11.2) | 980 (20.6) | <0.001 | 615 (16.3) | 1140 (24.5) | <0.001 | 352 (9.2) | 937 (19.7) | <0.001 |
| Education level a,b,c | |||||||||
| Primary | 346 (13.9) | 877 (28.9) | <0.001 | 446 (18.3) | 862 (29.1) | <0.001 | 378 (15.2) | 963 (31.7) | <0.001 |
| Secondary | 487 (7.9) | 913 (16.1) | <0.001 | 832 (13.5) | 1177 (20.9) | <0.001 | 483 (7.8) | 798 (14.1) | <0.001 |
| University | 95 (4.9) | 216(8.9) | <0.001 | 208 (10.7) | 357 (14.8) | <0.001 | 118 (6.1) | 188(7.8) | 0.032 |
| Social Class a,b,c | |||||||||
| Upper | 117 (5.7) | 238 (11.4) | <0.001 | 227 (11.2) | 300 (14.4) | <0.001 | 145 (7.1) | 230 (11.0) | <0.001 |
| Middle | 313 (8.5) | 622 (17.5) | <0.001 | 494 (13.6) | 735 (20.9) | <0.001 | 336 (9.2) | 635 (17.8) | <0.001 |
| Low | 516 (10.5) | 1157 (21.3) | <0.001 | 782 (16.1) | 1382 (25.9) | <0.001 | 513 (10.4) | 1112 (20.5) | <0.001 |
| Mental Disorders | Psychological Distress | Psychotropic Drug Consumption | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | Men | Women | p Value | Men | Women | p Value | Men | Women | p Value |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||||
| Self-rated health a,b,c | |||||||||
| Very good, good | 288 (3.6) | 614 (8.2) | <0.001 | 602 (7.6) | 854 (11.5) | <0.001 | 276 (3.5) | 564 (7.6) | <0.001 |
| Fair, poor, very poor | 670 (23.9) | 1483 (37.8) | <0.001 | 913 (33.3) | 1637 (42.8) | <0.001 | 728 (25.9) | 1500 (38.2) | <0.001 |
| Hypertension a,b,c | 335 (13.1) | 798 (29.9) | <0.001 | 484 (19.2) | 821 (31.4) | <0.001 | 405 (15.9) | 927 (34.8) | <0.001 |
| Heart diseases a,b,c | 159 (15.9) | 326 (38.9) | <0.001 | 233 (23.8) | 346 (42.6) | <0.001 | 216 (21.6) | 344 (41.1) | <0.001 |
| Arthrosis a,b,c | 261 (19.0) | 1010 (34.7) | <0.001 | 356 (26.4) | 1016 (35.6) | <0.001 | 309 (22.5) | 1142 (39.2) | <0.001 |
| Permanent injuries a,b,c | 159 (18.2) | 219 (37.4) | <0.001 | 238 (27.8) | 243 (42.5) | <0.001 | 147 (16.8) | 193 (32.9) | <0.001 |
| Stroke a,b,c | 63 (27.9) | 74 (43.3) | <0.001 | 74 (35.1) | 72 (45.3) | 0.040 | 81 (35.8) | 79 (46.2) | 0.040 |
| Diabetes mellitus a,b | 145 (14.7) | 300 (33.7) | <0.001 | 219 (22.6) | 327 (37.8) | <0.001 | 180 (18.3) | 348 (39.0) | 0.040 |
| Malignant Tumors a,b,c | 68 (17.4) | 228 (38.1) | <.001 | 112 (29.5) | 217 (37.5) | 0.010 | 87 (22.3) | 226 (37.7) | <0.001 |
| Respiratory diseases a,b,c | 156 (16.7) | 308 (29.1) | <0.001 | 239 (26.0) | 358 (34.5) | <0.001 | 166 (12.7) | 309 (29.2) | <0.001 |
| Chronic pain a,b,c | 466 (18.1) | 1413 (31.1) | <0.001 | 665 (26.0) | 1521 (33.9) | <0.001 | 508 (19.7) | 1375 (30.2) | <0.001 |
| Mental disorders b,c | 958 (100) | 2097 (100) | NA | 505 (55.3) | 1081 (53.6) | <0.001 | 578 (60.3) | 1334 (63.6) | 0.070 |
| Psychological distress a,c | 505 (33.3) | 1081 (43.4) | <0.001 | 1515 (100) | 2492 (100) | NA | 476 (31.4) | 1028 (41.3) | <0.001 |
| Mental Disorders | Psychological Distress | Psychotropic Drug Consumption | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | Men | Women | p Value | Men | Women | p Value | Men | Women | p Value |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||||
| Emergency services a,b,c | 381 (12.8) | 956 (26.2) | <0.001 | 650 (22.3) | 1147 (32.1) | <0.001 | 455 (15.3) | 981 (26.9) | <0.001 |
| Hospital admission a,b,c | 137 (15.8) | 289 (31.2) | <0.001 | 260 (31.1) | 366 (40.6) | <0.001 | 197 (22.8) | 346 (37.2) | <0.001 |
| Visit to physiotherapist a,b,c | 168 (10.0) | 450 (21.2) | <0.001 | 296 (17.7) | 518 (24.6) | <0.001 | 210 (12.4) | 405 (19.1) | <0.001 |
| Visit to psychologist a,b,c | 301 (70.3) | 507 (69.5) | 0.750 | 238 (58.0) | 404 (57.0) | 0.720 | 273 (63.9) | 443 (60.6) | 0.260 |
| Psychotropic drug use a,b | 578 (57.7) | 1334 (64.7) | <0.001 | 476 (49.1) | 1028 (51.6) | 0.210 | 1004 (100) | 2064 (100) | NA |
| Obesity a,b,c | 208 (10.9) | 508 (28.0) | <0.001 | 312 (16.5) | 515 (28.9) | <0.001 | 208 (32.2) | 475 (53.8) | <0.001 |
| Alcohol consumption a,b,c | 581 (7.0) | 937 (14.6) | <0.001 | 1065 (12.8) | 1195 (18.7) | <0.001 | 618 (7.4) | 872 (13.6) | <0.001 |
| Smoking habit a,b,c | 344 (11.0) | 480 (19.8) | <0.001 | 513 (16.6) | 559 (23.1) | <0.001 | 300 (9.6) | 386 (15.9) | <0.001 |
| Physical inactivity a,b,c | 511 (7.2) | 993 (15.1) | <0.001 | 744 (20.5) | 1348 (28.7) | <0.001 | 549 (7.8) | 923 (14.0) | <0.001 |
| Variables | Categories | Mental Disorders | Psychological Distress | Psychotropic Drug Consumption | |||
|---|---|---|---|---|---|---|---|
| OR (CI 95%) | p Value | OR (CI 95%) | p Value | OR (CI 95%) | p Value | ||
| Gender | Male | 1 | 1 | 1 | |||
| Female | 1.74 (1.54–1.96) | <0.001 | 1.26 (1.15–1.37) | <0.001 | 1.29 (1.15–1.45) | <0.001 | |
| Age (years) | 18–37 | 1 | 1 | 1 | |||
| 38–49 | 1.25 (1.05–1.50) | 0.013 | 0.97 (0.86–1.10) | 0.670 | 2.31 (1.87–2.85) | <0.001 | |
| 50–67 | 1.41 (1.17–1.70) | <0.001 | 0.78 (0.68–0.89) | <0.001 | 3.61 (2.92–4.46) | <0.001 | |
| >67 | 0.87 (0.69–1.10) | 0.247 | 0.57 (0.48–0.68) | <0.001 | 6.13 (4.79–7.83) | <0.001 | |
| Nationality | Spanish | 1 | 1 | 1 | |||
| Other | 0.67 (0.55–0.82) | <0.001 | 0.96 (0.84–1.09) | 0.514 | 0.77 (0.62–0.95) | 0.013 | |
| Marital status | Married | 1 | 1 | 1 | |||
| Other | 1.40 (1.25–1.58) | <0.001 | 1.25 (1.14–1.36) | <0.001 | 1.06 (0.94–1.19) | 0.325 | |
| Level of education | University | 1 | 1 | 1 | |||
| Secondary | 1.29 (1.07–1.56) | <0.001 | 0.88 (0.75–1.04) | 0.126 | 1.24 (0.99–1.53) | 0.051 | |
| Primary | 1.60 (1.31–2.02) | 0.007 | 0.93 (0.82–1.06) | 0.273 | 1.23 (1.02–1.48) | 0.029 | |
| Social class | Upper | 1 | 1 | 1 | |||
| Middle | 1.01 (0.84–1.22) | 0.882 | 1.12 (0.97–1.27) | 0.139 | 1.03 (0.86–1.23) | 0.749 | |
| Low | 1.10 (0.91–1.33) | 0.331 | 1.21 (1.06–1.39) | 0.006 | 0.93 (0.77–1.12) | 0.429 | |
| Self-rated health | Good | 1 | 1 | 1 | |||
| Poor | 2.17 (1.91–1.33) | <0.001 | 2.92 (2.64–3.22) | <0.001 | 1.87 (1.64–2.12) | <0.001 | |
| Emergency services | Yes | 0.95 (0.84–1.07) | 0.399 | 1.31 (1.20–1.44) | <0.001 | 1.46 (1.30–1.65) | <0.001 |
| Hospital admission | Yes | 0.64 (0.53–0.77) | <0.001 | 1.26 (1.10–1.45) | 0.001 | 1.29 (1.09–1.52) | 0.003 |
| Physiotherapist visit | Yes | 0.91 (0.79–1.05) | 0.219 | 0.98 (0.88–1.09) | 0.707 | 1.08 (0.94–1.24) | 0.294 |
| Psychologist visit | Yes | 7.50 (6.21–9.06) | <0.001 | 1.98 (1.68–2.32) | <0.001 | 5.10 (4.21–6.17) | <0.001 |
| Hypertension | Yes | 1.02 (0.88–1.16) | 0.826 | 1.05 (0.94–1.17) | 0.402 | 1.24 (1.09–1.41) | 0.001 |
| Heart diseases | Yes | 1.13 (0.94–1.35) | 0.185 | 1.22 (1.05–1.40) | 0.007 | 1.07 (0.91–1.26) | 0.411 |
| Arthrosis | Yes | 1.09 (0.94–1.26) | 0.252 | 1.11 (0.99–1.25) | 0.073 | 1.39 (1.22–1.59) | 0.000 |
| Permanent injuries | Yes | 1.33 (1.10–1.61) | 0.003 | 1.63 (1.42–1.88) | <0.001 | 0.87 (0.72–1.06) | 0.166 |
| Stroke | Yes | 1.49 (1.06–2.09) | 0.021 | 1.45 (1.11–1.91) | 0.007 | 1.39 (1.02–1.89) | 0.036 |
| Diabetes mellitus | Yes | 0.98 (0.82–1.18) | 0.873 | 1.15 (1.00–1.33) | 0.056 | 0.95 (0.80–1.12) | 0.533 |
| Malignant tumors | Yes | 1.28 (1.03–1.58) | 0.025 | 1.31 (1.10–1.56) | 0.002 | 1.04 (0.85–1.28) | 0.690 |
| Respiratory diseases | Yes | 1.03 (0.87–1.22) | 0.732 | 1.26 (1.10–1.43) | <0.001 | 1.05 (0.90–1.24) | 0.578 |
| Chronic pain | Yes | 1.72 (1.52–1.95) | <0.001 | 1.43 (1.30–1.57) | <0.001 | 1.42 (1.26–1.60) | <0.001 |
| Obesity | Yes | 1.23 (1.07–1.41) | 0.004 | 0.93 (0.83–1.03 | 0.176 | 0.88 (0.76–1.00) | 0.062 |
| Alcohol consumption | Yes | 0.85 (0.75–0.95) | 0.007 | 0.93 (0.85–1.02) | 0.126 | 0.87 (0.77–0.97) | 0.017 |
| Smoking habit | Yes | 1.47 (1.29–1.68) | <0.001 | 1.13 (1.02–1.24) | 0.017 | 1.17 (1.02–1.34) | 0.021 |
| Physical activity | Yes | 0.99 (0.89–1.12) | 0.959 | 0.68 (0.62–0.73) | <0.001 | 0.93 (0.83–1.04) | 0.196 |
| Psychotropic drugs | Yes | 10.35 (9.15–11.69) | <0.001 | 1.77 (1.57–2.00) | <0.001 | - | |
| Psychological distress | Yes | 2.80 (2.48–3.15) | <0.001 | - | 1.81 (1.59–2.04) | <0.001 | |
| Mental disorders | Yes | - | 2.72 (2.41–3.06) | <0.001 | 10.46 (9.26–11.82) | <0.001 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maestre-Miquel, C.; López-de-Andrés, A.; Ji, Z.; de Miguel-Diez, J.; Brocate, A.; Sanz-Rojo, S.; López-Farre, A.; Carabantes-Alarcon, D.; Jiménez-García, R.; Zamorano-León, J.J. Gender Differences in the Prevalence of Mental Health, Psychological Distress and Psychotropic Medication Consumption in Spain: A Nationwide Population-Based Study. Int. J. Environ. Res. Public Health 2021, 18, 6350. https://doi.org/10.3390/ijerph18126350
Maestre-Miquel C, López-de-Andrés A, Ji Z, de Miguel-Diez J, Brocate A, Sanz-Rojo S, López-Farre A, Carabantes-Alarcon D, Jiménez-García R, Zamorano-León JJ. Gender Differences in the Prevalence of Mental Health, Psychological Distress and Psychotropic Medication Consumption in Spain: A Nationwide Population-Based Study. International Journal of Environmental Research and Public Health. 2021; 18(12):6350. https://doi.org/10.3390/ijerph18126350
Chicago/Turabian StyleMaestre-Miquel, Clara, Ana López-de-Andrés, Zichen Ji, Javier de Miguel-Diez, Arturo Brocate, Sara Sanz-Rojo, Antonio López-Farre, David Carabantes-Alarcon, Rodrigo Jiménez-García, and José J. Zamorano-León. 2021. "Gender Differences in the Prevalence of Mental Health, Psychological Distress and Psychotropic Medication Consumption in Spain: A Nationwide Population-Based Study" International Journal of Environmental Research and Public Health 18, no. 12: 6350. https://doi.org/10.3390/ijerph18126350
APA StyleMaestre-Miquel, C., López-de-Andrés, A., Ji, Z., de Miguel-Diez, J., Brocate, A., Sanz-Rojo, S., López-Farre, A., Carabantes-Alarcon, D., Jiménez-García, R., & Zamorano-León, J. J. (2021). Gender Differences in the Prevalence of Mental Health, Psychological Distress and Psychotropic Medication Consumption in Spain: A Nationwide Population-Based Study. International Journal of Environmental Research and Public Health, 18(12), 6350. https://doi.org/10.3390/ijerph18126350








