Community Engagement Practices at Research Centers in U.S. Minority Institutions: Priority Populations and Innovative Approaches to Advancing Health Disparities Research
Abstract
:1. Introduction
1.1. Research Centers in Minority Institutions
1.2. Community Engagement Cores
1.3. Objective
2. Materials and Methods
3. Results
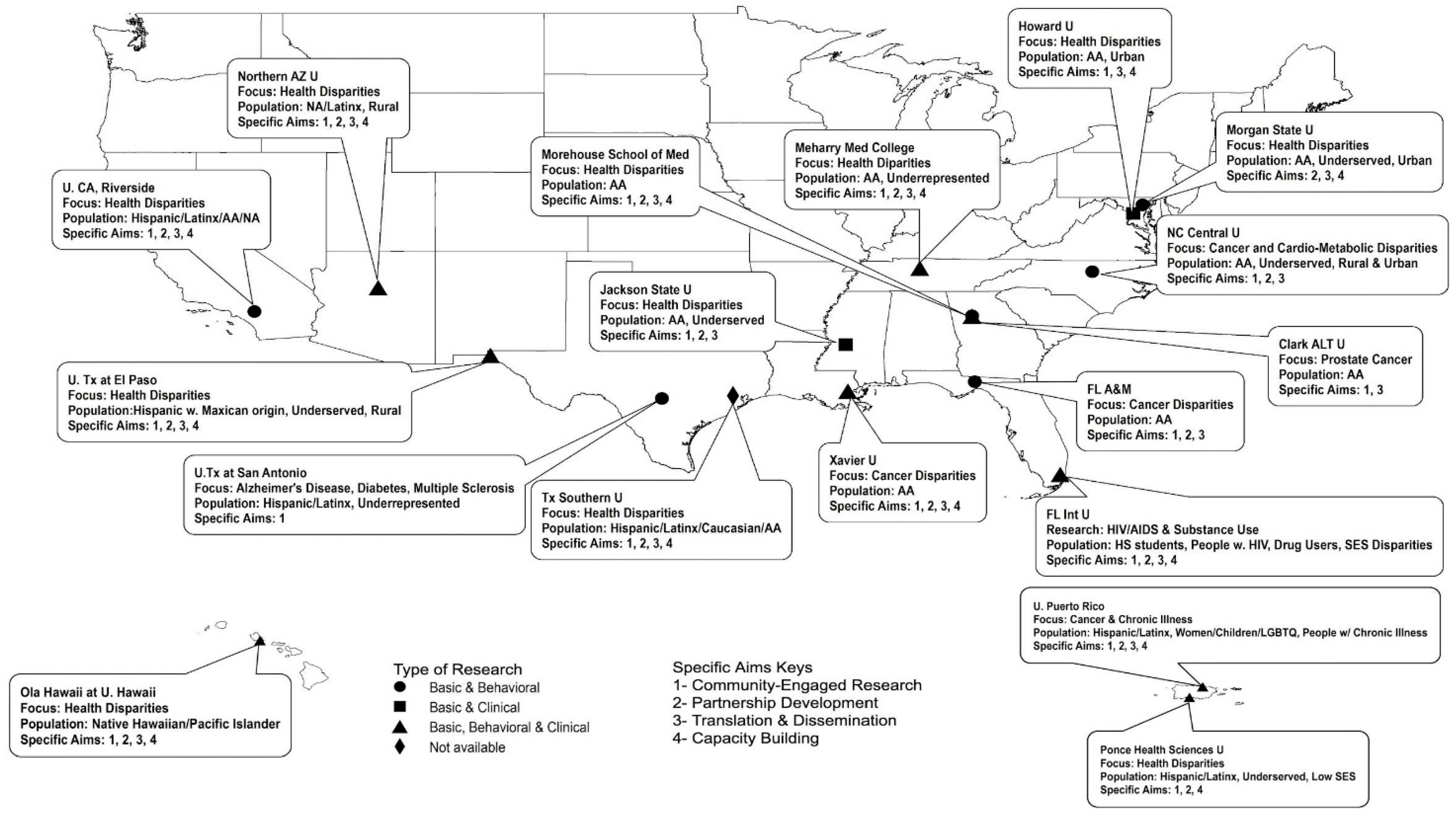
3.1. Demographics, Components, Focus Areas, Specific Aims and Target Populations
3.2. Themes from the Open-Ended Questions
3.3. Establishing Trust between the Community-Academic Collaborators and within the Community
Provide seed funding for small projects to help the partnership develop and strengthen before jumping into a larger project with more funding. Seed funding gives partners a unique opportunity to discuss roles and responsibilities and to negotiate shared decision- making and power early on, which strengthens the partnership in the long-term.
“We support a community-based research group which vets requests from students, instructors, and researchers who want to access the community. Instructors, researchers, and students must attend a few monthly meetings to get to know the group and then present and defend their research, explaining how they will build community capacity, share data [and] share findings, etc.”
3.4. Building Collaborative Relationships
“We use a shared governance model and integrate community partners in leadership of the program. Community partners are co-leaders of the CEC and members of the program advisory committee that assesses progress and outcomes and makes recommendations for improvement.”
4. Discussion
4.1. Strengths of the RCMI CEC Network
4.2. Strengths of Study
4.3. Limitations of Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Research Centers in Minority Institutions Program. Available online: https://www.nimhd.nih.gov/programs/extramural/research-centers/rcmi/ (accessed on 17 February 2021).
- Department of Health and Human Services Part 1. Overview Information. Available online: https://grants.nih.gov/grants/guide/rfa-files/RFA-FD-17-005.html (accessed on 17 February 2021).
- Grumbach, K.; Vargas, R.A.; Fleisher, P.; Aragόn, T.J.; Chung, L.; Chawla, C.; Yant, A.; Garcia, E.R.; Santiago, A.; Lang, P.L.; et al. Achieving health equity through community engagement in translating evidence to policy: The San Francisco Health Improvement Partnership, 2010–2016. Prev. Chronic Dis. 2017, 14, 1–9. [Google Scholar] [CrossRef]
- Committee to Review the Clinical and Translational Science Awards Program at the National Center for Advancing Translational Sciences; Board on Health Sciences Policy; Institute of Medicine. The CTSA Program at NIH: Opportunities for Advancing Clinical and Translational Research; Leshner, A.I., Terry, S.F., Schultz, A.M., Liverman, C.T., Eds.; National Academies Press (US): Washington, DC, USA, 2013. [Google Scholar]
- Sydnor, K.D.; Hawkins, A.S.; Edwards, L.V. Expanding Research Opportunities: Making the Argument for the Fit between HBCUs and Community-based Participatory Research. J. Negro Educ. 2010, 79, 79–86. [Google Scholar]
- Braun, K.L.; Stewart, S.; Baquet, C.; Berry-Bobovski, L.; Blumenthal, D.; Brandt, H.M.; Buchwald, D.S.; Campbell, J.E.; Coe, K.; Cooper, L.C.; et al. The National Cancer Institute’s Community Networks Program initiative to reduce dancer health disparities: Outcomes and lessons learned. Prog. Community Health Partnersh. 2015, 9, 21–32. [Google Scholar] [CrossRef] [Green Version]
- Hébert, J.R.; Braun, K.L.; Meade, C.D.; Bloom, J.; Kobetz, E. Community-based participatory research adds value to the National Cancer Institute’s research portfolio (editorial). Prog. Community Health Partnersh. 2015, 9. [Google Scholar] [CrossRef] [Green Version]
- Leon Guerrero, R.T.; Palafox, N.A.; Hattori-Uchima, M.P.; Robinette, H.R.; Vogel, C.W. Addressing cancer health disparities in the Pacific Peoples of Hawai’i, Guam, and the US Associated Pacific Islands through Pacific-focused research capacity building. JCO Glob. Oncol. 2020, 6, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Institutional Development Award Program Infrastructure for Clinical and Translational Research (IDeA-CTR). Available online: https://www.nigms.nih.gov/Research/DRCB/IDeA/Pages/IDeA-CTR.aspx#:~:text=Institutional%20Development%20Award%20Program%20Infrastructure%20for%20Clinical%20and,and%20coordination%20of%20clinical%20and%20translational%20research (accessed on 17 February 2021).
- Eder, M.; Evans, E.; Funes, M.; Hong, H.; Reuter, K.; Ahmed, S.; Calhoun, K.; Corbie-Smith, G.; Dave, G.; DeFino, M.; et al. Defining and measuring community engagement and community-engaged research: Clinical and Translational Science Institutional Practices. Prog. Community Health Partnersh. 2018, 12, 145–156. [Google Scholar] [CrossRef] [PubMed]
- Goal 2: Engage Patients and Communities in Every Phase of the Translational Process. Available online: https://ncats.nih.gov/ctsa/action/goal2 (accessed on 17 February 2021).
- Braun, K.L.; Tsark, J.; Santos, L.; Aitaoto, N.; Chong, C. Building Native Hawaiian capacity in cancer research and programming: The Legacy of ‘Imi Hale. Cancer 2006, 108, 2082–2090. [Google Scholar] [CrossRef] [PubMed]
- Cunningham-Erves, J.; Joosten, Y.; Hollingsworth, C.P.; Cockroft, J.D.; Murry, V.M.; Lipham, L.; Luther, P.; Vaughn, Y.; Miller, S.T. Implementation and evaluation of a dual-track research training program for community members and community-based organizations. Prog. Community Health Partnersh. 2020, 14, 75–87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cunningham-Erves, J.; Joosten, Y.; Bruce, M.A.; Elzey, J.; Luther, P.; Lipham, L.; Vaughn, Y.; Micah, T.; Wilkins, C.H.; Miller, S.T. Comprehensive strategy for capturing and integrating community input into community research training curricula. J. Clin. Transl. Sci. 2018, 2, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Jenkins, C.; Fagan, H.B.; Passarella, J.; Fournakis, N.; Burshell, D. Training academic and community investigator teams for community-engaged research: Program development, implementation, evaluation and replication. Prog. Community Health Partnersh. 2020, 14, 229–242. [Google Scholar] [CrossRef]
- Drahota, A.; Meza, R.D.; Brikho, B.; Naaf, M.; Estabillo, J.A.; Gomez, E.D.; Vejnoska, S.F.; Dufek, S.; Stahmer, A.C.; Aarons, G.A. Community-Academic Partnerships: A systematic review of the state of the literature and recommendations for fture research. Milbank Q. 2016, 94, 163–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fong, M.; Braun, K.L.; Tsark, J. Improving Native Hawaiian health through community-based participatory research. CJHP 2003, 1, 136–148. [Google Scholar] [CrossRef] [Green Version]
- LeClair, A.; Lim, J.J.; Rubin, C. Lessons learned from developing and sustaining a community-research collaborative through translational research. J. Clin. Transl. Sci. 2018, 2, 79–85. [Google Scholar] [CrossRef] [Green Version]
- Sy, A.; Hayes, T.; Laurila, K.; Noboa, C.; Langwerden, R.J.; Hospital, M.M.; Andújar-Pérez, D.A.; Stevenson, L.; Cunningham, S.M.R.; Rollins, L.; et al. Evaluating Research Centers in Minority Institutions: Framework, metrics, best practices, and challenges. Int. J. Environ. Res. Public Health 2020, 17, 8373. [Google Scholar] [CrossRef]
- Braun, K.L.; Nguyen, T.; Tanjasiri, S.P.; Campbell, J.; Heiney, S.P.; Brandt, H.M.; Smith, S.A.; Blumenthal, D.S.; Hargreaves, M.; Coe, K.; et al. Operationalization of community-based participatory research principles across NCI’s Community Networks Programs. Am. J. Public Health 2012, 102, 1195–1203. [Google Scholar] [CrossRef] [PubMed]
- Wallerstein, N.; Duran, B. Community-based participatory research contributions to intervention research: The intersection of science and practice to improve health equity. Am. J. Public Health 2010, 100, 40–46. [Google Scholar] [CrossRef]
- Oetzel, J.G.; Zhou, C.; Duran, B.; Pearson, C.; Magarati, M.; Lucero, J.; Wallerstein, N.; Villegas, M. Establishing the psychometric properties of constructs in a community-based participatory research conceptual model. Am. J. Health Promot. 2015, 29, 188–202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Charmaz, Z. Constructing Grounded Theory; Sage Publication: London, UK, 2014. [Google Scholar]
- Glaser, B.G.; Strauss, A.L. The Discovery of Grounded Theory: Strategies for Qualitative Research; Aldine: Chicago, IL, USA, 1967. [Google Scholar]
- Centers for Disease Control and Prevention, U.S. Public Health Service Syphilis Study at Tuskegee, The Tuskegee Timeline. Available online: https://www.cdc.gov/tuskegee/timeline.htm (accessed on 17 February 2021).
- Melo, M.M.; Wolf, L.E. The Havasupai Indian Tribe case: Lessons for research involving stored biologic samples. N. Engl. J. Med. 2010, 363, 204–207. [Google Scholar] [CrossRef] [PubMed]
- Hamidreza Babaei, N.A. Bonding, bridging and linking social capital and empowerment among squatter settlements in Tehran, Iran. World App. Sci. J. 2012, 17, 119–126. [Google Scholar]
- Sandel, M.; Faugno, E.; Mingo, A.; Cannon, J.; Byrd, K.; Acevedo Garcia, D.; Collier, S.; McClure, E.; Boynton Jarrett, R. Neighborhood-level interventions to improve childhood opportunity and lift children out of poverty. Acad. Pediatr. 2016, 16, 128–135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Braithwaite, R.; Akintobi, T.; Blumenthal, D.; Langley, M. Morehouse mHEodel: How One School of Medicine Revolutionized Community Engagement and Health Equity; Johns Hopkins University Press: Baltimore, MD, USA, 2020. [Google Scholar]
- Allen, M.; Culhane-Pera, K.; Pergament, S.; Call, T. A Capacity building program to promote CBPR partnerships between academic researchers and community members. Clin. Transl. Sci. 2011, 4, 428–433. [Google Scholar] [CrossRef] [PubMed]
- Staniszewska, S.; Haywood, K.L.; Brett, J.; Tutton, L. Patient and public involvement in developing patient-reported outcome measures: Evolution not revolution. Patient 2012, 5, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Glasgow, R.E.; Lichtenstein, E.; Marcus, A.C. Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. Am. J. Public Health 2003, 93, 1261–1267. [Google Scholar] [CrossRef]
- Henry Akintobi, T.; Hopkins, J.; Holden, K.B.; Hefner, D.; Taylor, H.A., Jr. Tx ™: An Approach and Philosophy to Advance Translation to Transformation. Ethn. Dis. 2019, 29 (Suppl. 2), 349–354. [Google Scholar] [CrossRef]
- Park, J. Historical origins of the Tuskegee Experiment: The dilemma of public health in the United States. Korean J. Med. Hist. 2017, 26, 545–578. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kerpel-Fronius, S. The epoch-changing influence of the Nuremberg Doctor’s Trial on the ethical judgement of human experiments. Orv. Hetilap. 2008, 149, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Jones, B.L.; Vyhlidal, C.A.; Bradley-Ewing, A.; Sherman, A.; Goggin, K. If we would only ask: How Henrietta Lacks continues to teach us about perceptions of research and genetic research among African Americans today. J. Racial Ethn. Health Disparities 2017, 4, 735–745. [Google Scholar] [CrossRef]


| RCMI Characteristic | Number (%) |
|---|---|
| Years RCMI Funded | |
| <10 Years | 8 (47%) |
| 10–20 Years | 2 (12%) |
| 20+ Years | 7 (41%) |
| Years CEC Funded | |
| 1–2 Years | 10 (59%) |
| 3–4 Years | 4 (24%) |
| 5+ Years | 3 (18%) |
| Advisory Committee | |
| Advisory Committee Formed | 15 (88%) |
| Advisory Committee Active | 14 (82%) |
| Specific Aims | |
| Community Engaged Research | 16 (94%) |
| Translation & Dissemination | 15 (88%) |
| Partnership Development | 14 (82%) |
| Capacity Building | 12 (71%) |
| Services | |
| Partnership Linkage/Connection | 13 (77%) |
| Education, Training, Tech Asst., Workshop, Seminar | 12 (71%) |
| Proposal Development, Research Support/Funding | 9 (53%) |
| Dissemination Events/Support | 8 (47%) |
| Consultation | 6 (35%) |
| Engagement Strategies | |
| Skill Building & Learning | 14 (82%) |
| Implementation | 14 (82%) |
| Dissemination Efforts & Support | 12 (71%) |
| Discussion & Dialogue | 10 (59%) |
| Communications | 8 (47%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Henry Akintobi, T.; Sheikhattari, P.; Shaffer, E.; Evans, C.L.; Braun, K.L.; Sy, A.U.; Mancera, B.; Campa, A.; Miller, S.T.; Sarpong, D.; et al. Community Engagement Practices at Research Centers in U.S. Minority Institutions: Priority Populations and Innovative Approaches to Advancing Health Disparities Research. Int. J. Environ. Res. Public Health 2021, 18, 6675. https://doi.org/10.3390/ijerph18126675
Henry Akintobi T, Sheikhattari P, Shaffer E, Evans CL, Braun KL, Sy AU, Mancera B, Campa A, Miller ST, Sarpong D, et al. Community Engagement Practices at Research Centers in U.S. Minority Institutions: Priority Populations and Innovative Approaches to Advancing Health Disparities Research. International Journal of Environmental Research and Public Health. 2021; 18(12):6675. https://doi.org/10.3390/ijerph18126675
Chicago/Turabian StyleHenry Akintobi, Tabia, Payam Sheikhattari, Emma Shaffer, Christina L. Evans, Kathryn L. Braun, Angela U. Sy, Bibiana Mancera, Adriana Campa, Stephania T. Miller, Daniel Sarpong, and et al. 2021. "Community Engagement Practices at Research Centers in U.S. Minority Institutions: Priority Populations and Innovative Approaches to Advancing Health Disparities Research" International Journal of Environmental Research and Public Health 18, no. 12: 6675. https://doi.org/10.3390/ijerph18126675
APA StyleHenry Akintobi, T., Sheikhattari, P., Shaffer, E., Evans, C. L., Braun, K. L., Sy, A. U., Mancera, B., Campa, A., Miller, S. T., Sarpong, D., Holliday, R., Jimenez-Chavez, J., Khan, S., Hinton, C., Sellars-Bates, K., Ajewole, V., Teufel-Shone, N. I., McMullin, J., Suther, S., ... Tchounwou, P. B. (2021). Community Engagement Practices at Research Centers in U.S. Minority Institutions: Priority Populations and Innovative Approaches to Advancing Health Disparities Research. International Journal of Environmental Research and Public Health, 18(12), 6675. https://doi.org/10.3390/ijerph18126675














