Assessing the Country-Level Excess All-Cause Mortality and the Impacts of Air Pollution and Human Activity during the COVID-19 Epidemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Area and Datasets
2.2. Excess Mortality Estimation
2.3. Association Analysis
3. Results
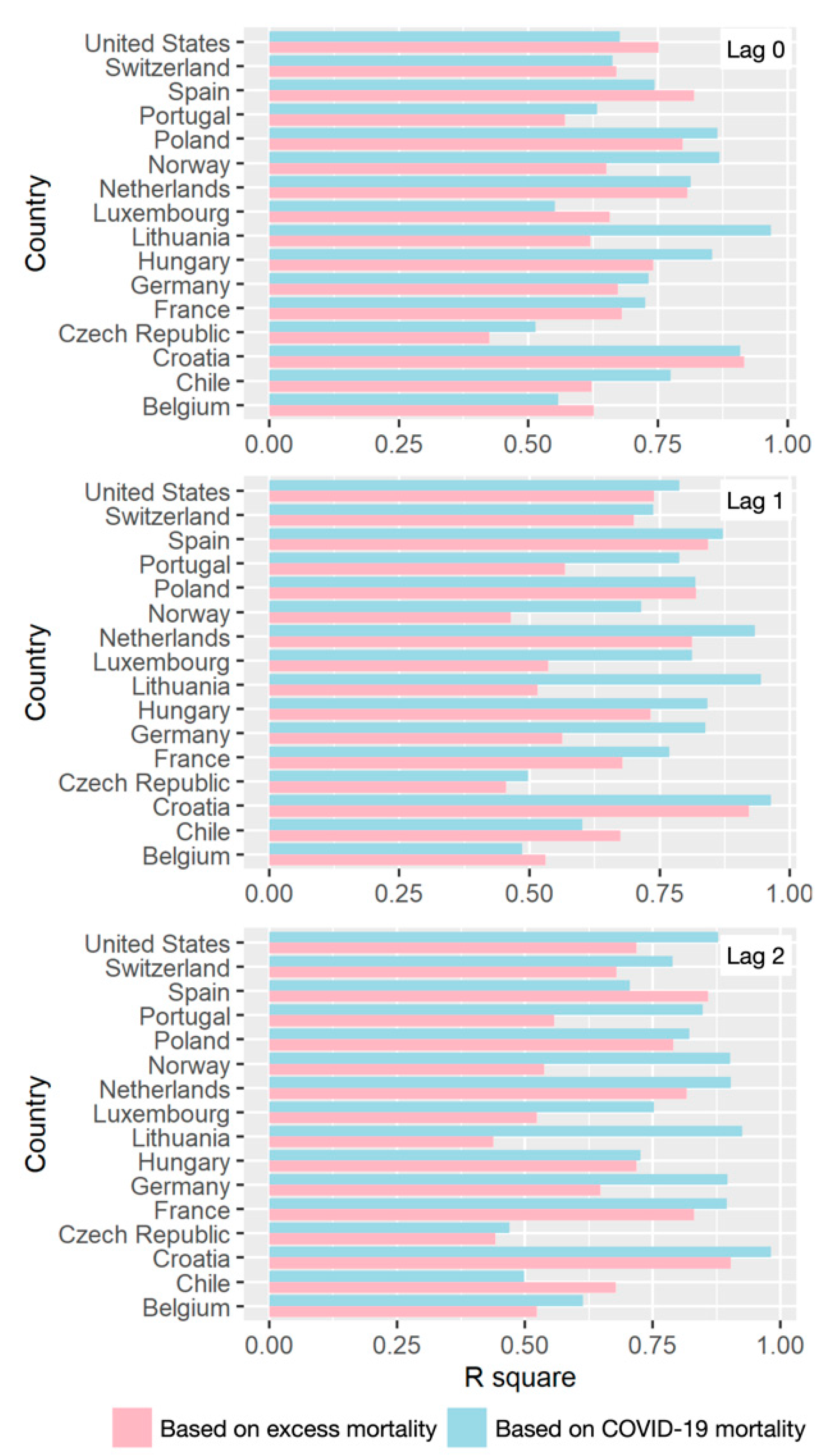
3.1. Excess All-Cause Mortality during COVID-19
3.2. Air Pollution/Human Activity Impacts Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Schlosser, F.; Maier, B.F.; Jack, O.; Hinrichs, D.; Zachariae, A.; Brockmann, D. COVID-19 lockdown induces disease-mitigating structural changes in mobility networks. Proc. Natl. Acad. Sci USA 2020, 117, 32883–32890. [Google Scholar] [CrossRef] [PubMed]
- Fisher, D.; Wilder-Smith, A. The global community needs to swiftly ramp up the response to contain COVID-19. Lancet 2020, 395, 1109–1110. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.J.; Bao, Y.; Huang, X.; Shi, J.; Lu, L. Mental health considerations for children quarantined because of COVID-19. Lancet Child. Adolesc. Health 2020, 4, 347–349. [Google Scholar] [CrossRef] [Green Version]
- Xiang, Y.-T.; Yang, Y.; Li, W.; Zhang, L.; Zhang, Q.; Cheung, T.; Ng, C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020, 7, 228–229. [Google Scholar] [CrossRef] [Green Version]
- Pietrobelli, A.; Pecoraro, L.; Ferruzzi, A.; Heo, M.; Faith, M.; Zoller, T.; Antoniazzi, F.; Piacentini, G.; Fearnbach, S.N.; Heymsfield, S.B. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: A longitudinal study. Obesity 2020, 28, 1382–1385. [Google Scholar] [CrossRef] [PubMed]
- Lai, A.G.; Pasea, L.; Banerjee, A.; Denaxas, S.; Katsoulis, M.; Chang, W.H.; Williams, B.; Pillay, D.; Noursadeghi, M.; Linch, D. Estimating excess mortality in people with cancer and multimorbidity in the COVID-19 emergency. MedRxiv 2020. [Google Scholar] [CrossRef]
- Bilinski, A.; Emanuel, E.J. COVID-19 and excess all-cause mortality in the US and 18 comparison countries. JAMA 2020, 324, 2100–2102. [Google Scholar] [CrossRef]
- Arolas, H.P.; Acosta, E.; López-Casasnovas, G.; Lo, A.; Nicodemo, C.; Riffe, T.; Myrskylä, M. Years of life lost to COVID-19 in 81 countries. Sci. Rep. 2021, 11, 3504. [Google Scholar] [CrossRef]
- Leon, D.A.; Shkolnikov, V.M.; Smeeth, L.; Magnus, P.; Pechholdová, M.; Jarvis, C.I. COVID-19: A need for real-time monitoring of weekly excess deaths. Lancet 2020, 395, e81. [Google Scholar] [CrossRef]
- Modi, C.; Boehm, V.; Ferraro, S.; Stein, G.; Seljak, U. Total covid-19 mortality in Italy: Excess mortality and age dependence through time-series analysis. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Rivera, R.; Rosenbaum, J.E.; Quispe, W. Excess mortality in the United States during the first three months of the COVID-19 pandemic. Epidemiol. Infect. 2020, 148, e264. [Google Scholar] [CrossRef]
- Stang, A.; Standl, F.; Kowall, B.; Brune, B.; Böttcher, J.; Brinkmann, M.; Dittmer, U.; Jöckel, K.-H. Excess mortality due to COVID-19 in Germany. J. Infect. 2020, 81, 797–801. [Google Scholar] [CrossRef]
- Nogueira, P.J.; de Araújo Nobre, M.; Nicola, P.J.; Furtado, C.; Carneiro, A.V. Excess mortality estimation during the COVID-19 pandemic: Preliminary data from Portugal. Acta Med. Port. 2020, 33, 376–383. [Google Scholar] [CrossRef]
- Gibertoni, D.; Adja, K.Y.C.; Golinelli, D.; Reno, C.; Regazzi, L.; Lenzi, J.; Sanmarchi, F.; Fantini, M.P. Patterns of COVID-19 related excess mortality in the municipalities of Northern Italy during the first wave of the pandemic. Health Place 2021, 67, 102508. [Google Scholar] [CrossRef]
- Krieger, N.; Chen, J.T.; Waterman, P.D. Excess mortality in men and women in Massachusetts during the COVID-19 pandemic. Lancet 2020, 395, 1829. [Google Scholar] [CrossRef]
- Lancet, T. The gendered dimensions of COVID-19. Lancet 2020, 395, 1168. [Google Scholar] [CrossRef]
- Sinnathamby, M.A.; Whitaker, H.; Coughlan, L.; Bernal, J.L.; Ramsay, M.; Andrews, N. All-cause excess mortality observed by age group and regions in the first wave of the COVID-19 pandemic in England. Eurosurveillance 2020, 25, 2001239. [Google Scholar] [CrossRef] [PubMed]
- Blangiardo, M.; Cameletti, M.; Pirani, M.; Corsetti, G.; Battaglini, M.; Baio, G. Estimating weekly excess mortality at sub-national level in Italy during the COVID-19 pandemic. PLoS ONE 2020, 15, e0240286. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, A.; Pasea, L.; Harris, S.; Gonzalez-Izquierdo, A.; Torralbo, A.; Shallcross, L.; Noursadeghi, M.; Pillay, D.; Sebire, N.; Holmes, C. Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: A population-based cohort study. Lancet 2020, 395, 1715–1725. [Google Scholar] [CrossRef]
- Dong, Z.; Fan, X.; Wang, J.; Mao, Y.; Luo, Y.; Tang, S. Data-related and methodological obstacles to determining associations between temperature and COVID-19 transmission. Environ. Res. Lett. 2021, 16, 034016. [Google Scholar] [CrossRef]
- Chang, S.; Pierson, E.; Koh, P.W.; Gerardin, J.; Redbird, B.; Grusky, D.; Leskovec, J. Mobility network models of COVID-19 explain inequities and inform reopening. Nature 2021, 589, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Pullano, G.; Valdano, E.; Scarpa, N.; Rubrichi, S.; Colizza, V. Evaluating the effect of demographic factors, socioeconomic factors, and risk aversion on mobility during the COVID-19 epidemic in France under lockdown: A population-based study. Lancet Digit. Health 2020, 2, e638–e649. [Google Scholar] [CrossRef]
- Grantz, K.H.; Meredith, H.R.; Cummings, D.A.; Metcalf, C.J.E.; Grenfell, B.T.; Giles, J.R.; Mehta, S.; Solomon, S.; Labrique, A.; Kishore, N. The use of mobile phone data to inform analysis of COVID-19 pandemic epidemiology. Nat. Commun. 2020, 11, 4961. [Google Scholar] [CrossRef] [PubMed]
- Burnett, R.; Chen, H.; Szyszkowicz, M.; Fann, N.; Hubbell, B.; Pope, C.A.; Apte, J.S.; Brauer, M.; Cohen, A.; Weichenthal, S. Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proc. Natl. Acad. Sci USA 2018, 115, 9592–9597. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Achakulwisut, P.; Brauer, M.; Hystad, P.; Anenberg, S.C. Global, national, and urban burdens of paediatric asthma incidence attributable to ambient NO2 pollution: Estimates from global datasets. Lancet Planet. Health 2019, 3, e166–e178. [Google Scholar] [CrossRef] [Green Version]
- Venter, Z.S.; Aunan, K.; Chowdhury, S.; Lelieveld, J. Air pollution declines during COVID-19 lockdowns mitigate the global health burden. Environ. Res. 2021, 192, 110403. [Google Scholar] [CrossRef]
- Barnett-Itzhaki, Z.; Levi, A. Effects of chronic exposure to ambient air pollutants on COVID-19 morbidity and mortality-A lesson from OECD countries. Environ. Res. 2021, 195, 110723. [Google Scholar] [CrossRef]
- Domingo, J.L.; Rovira, J. Effects of air pollutants on the transmission and severity of respiratory viral infections. Environ. Res. 2020, 109650. [Google Scholar] [CrossRef]
- Wu, X.; Nethery, R.C.; Sabath, B.M.; Braun, D.; Dominici, F. Exposure to air pollution and COVID-19 mortality in the United States. MedRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Liu, L. Emerging study on the transmission of the Novel Coronavirus (COVID-19) from urban perspective: Evidence from China. Cities 2020, 103, 102759. [Google Scholar] [CrossRef]
- Ugolini, F.; Massetti, L.; Calaza-Martínez, P.; Cariñanos, P.; Dobbs, C.; Ostoić, S.K.; Marin, A.M.; Pearlmutter, D.; Saaroni, H.; Šaulienė, I. Effects of the COVID-19 pandemic on the use and perceptions of urban green space: An international exploratory study. Urban. For. Urban. Green. 2020, 56, 126888. [Google Scholar] [CrossRef]
- Venter, Z.S.; Barton, D.N.; Gundersen, V.; Figari, H.; Nowell, M. Urban nature in a time of crisis: Recreational use of green space increases during the COVID-19 outbreak in Oslo, Norway. Environ. Res. Lett. 2020, 15, 104075. [Google Scholar] [CrossRef]
- Brynjolfsson, E.; Horton, J.J.; Ozimek, A.; Rock, D.; Sharma, G.; TuYe, H.-Y. COVID-19 and Remote Work: An Early Look at US Data; 0898-2937; National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar]
- Bishop, G.; Welch, G. An introduction to the kalman filter. Proc. SiggraphCourse 2001, 8, 41. [Google Scholar]
- Rugge, M.; Zorzi, M.; Guzzinati, S. SARS-CoV-2 infection in the Italian Veneto region: Adverse outcomes in patients with cancer. Nat. Cancer 2020, 1, 784–788. [Google Scholar] [CrossRef]
- Albiges, L.; Foulon, S.; Bayle, A.; Gachot, B.; Pommeret, F.; Willekens, C.; Stoclin, A.; Merad, M.; Griscelli, F.; Lacroix, L. Determinants of the outcomes of patients with cancer infected with SARS-CoV-2: Results from the Gustave Roussy cohort. Nat. Cancer 2020, 1, 965–975. [Google Scholar] [CrossRef]
- Subbiah, V. A global effort to understand the riddles of COVID-19 and cancer. Nat. Cancer 2020, 1, 943–945. [Google Scholar] [CrossRef]
- Iftimie, S.; López-Azcona, A.F.; Vicente-Miralles, M.; Descarrega-Reina, R.; Hernández-Aguilera, A.; Riu, F.; Simó, J.M.; Garrido, P.; Joven, J.; Camps, J. Risk factors associated with mortality in hospitalized patients with SARS-CoV-2 infection. A prospective, longitudinal, unicenter study in Reus, Spain. PLoS ONE 2020, 15, e0234452. [Google Scholar] [CrossRef] [PubMed]
- Geng, D.C.; Innes, J.; Wu, W.; Wang, G. Impacts of COVID-19 pandemic on urban park visitation: A global analysis. J. For. Res. 2021, 32, 553–567. [Google Scholar] [CrossRef]
- Kwok, C.Y.T.; Wong, M.S.; Chan, K.L.; Kwan, M.-P.; Nichol, J.E.; Liu, C.H.; Wong, J.Y.H.; Wai, A.K.C.; Chan, L.W.C.; Xu, Y. Spatial analysis of the impact of urban geometry and socio-demographic characteristics on COVID-19, a study in Hong Kong. Sci. Total Environ. 2021, 764, 144455. [Google Scholar] [CrossRef]
- De Angelis, E.; Renzetti, S.; Volta, M.; Donato, F.; Calza, S.; Placidi, D.; Lucchini, R.G.; Rota, M. COVID-19 incidence and mortality in Lombardy, Italy: An ecological study on the role of air pollution, meteorological factors, demographic and socioeconomic variables. Environ. Res. 2021, 195, 110777. [Google Scholar] [CrossRef] [PubMed]
- Zoran, M.A.; Savastru, R.S.; Savastru, D.M.; Tautan, M.N. Assessing the relationship between ground levels of ozone (O3) and nitrogen dioxide (NO2) with coronavirus (COVID-19) in Milan, Italy. Sci. Total Environ. 2020, 740, 140005. [Google Scholar] [CrossRef] [PubMed]
- Villeneuve, P.J.; Goldberg, M.S. Methodological considerations for epidemiological studies of air pollution and the SARS and COVID-19 coronavirus outbreaks. Environ. Health Perspect. 2020, 128, 095001. [Google Scholar] [CrossRef] [PubMed]


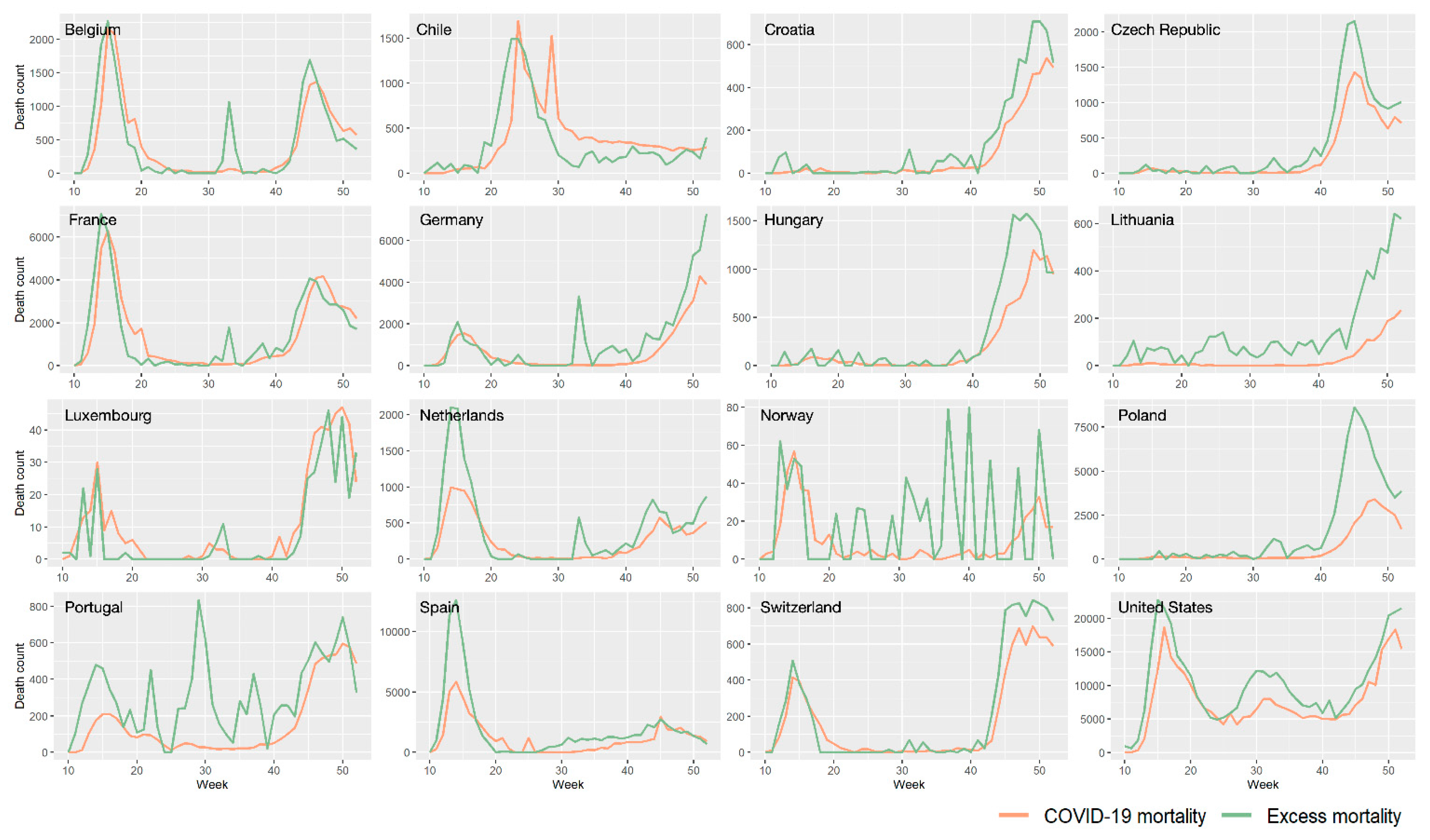




| Country | COVID-19 Mortality | Excess All-Cause Mortality | Variation |
|---|---|---|---|
| Belgium | 19,317 | 19,956 | 3.31% |
| Chile | 16,443 | 14,315 | −12.94% |
| Croatia | 3671 | 5640 | 53.64% |
| Czech Republic | 11,058 | 17,224 | 55.76% |
| France | 62,634 | 63,767 | 1.81% |
| Germany | 30,366 | 50,385 | 65.93% |
| Hungary | 9047 | 13,905 | 53.70% |
| Lithuania | 1254 | 5939 | 373.60% |
| Luxembourg | 460 | 338 | −26.52% |
| Netherland | 11,095 | 17,538 | 58.07% |
| Norway | 421 | 829 | 96.91% |
| Poland | 27,118 | 71,237 | 162.69% |
| Portugal | 6619 | 13,352 | 101.72% |
| Spain | 51,744 | 82,355 | 59.16% |
| Switzerland | 7316 | 9106 | 24.47% |
| United States | 333,278 | 445,242 | 33.59% |
| Min. | Max. | Mean | SD | |
|---|---|---|---|---|
| Weekly NO2 (μg/m3) | 0.000 | 227.039 | 117.327 | 35.680 |
| Weekly PM2.5 (μg/m3) | 0.000 | 204.573 | 66.256 | 32.085 |
| Weekly park visits | −582.000 | 2859.000 | 250.076 | 483.875 |
| Weekly workplace visits | −526.000 | 86.000 | −191.499 | 102.288 |
| Daily precipitation (inch) | 0.000 | 2.616 | 0.517 | 0.492 |
| Daily temperature () | 27.313 | 80.231 | 55.111 | 11.324 |
| Weekly excess death count | 0 | 1.29 × 108 | 3.61 × 106 | 1.25 × 107 |
| Weekly NO2 | Weekly PM2.5 | Weekly Park Visits | Weekly Workplace Visits | ||
|---|---|---|---|---|---|
| Lag 0 | COVID-19 mortality | 1.0166 | 0.9979 | 0.9987 | 0.9968 |
| Excess mortality | 1.0155 | 0.9983 | 0.998 | 0.9968 | |
| Lag 1 | COVID-19 mortality | 1.0162 | 0.9985 | 0.9982 | 0.9979 |
| Excess mortality | 1.0145 | 0.9983 | 0.9975 | 0.9983 | |
| Lag 2 | COVID-19 mortality | 1.0185 | 0.9977 | 0.9976 | 0.999 |
| Excess mortality | 1.0162 | 0.9977 | 0.9976 | 0.9979 | |
| Mean | COVID-19 mortality | 1.0171 | 0.998 | 0.9981 | 0.9979 |
| Excess mortality | 1.0154 | 0.9981 | 0.9977 | 0.9977 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meng, Y.; Wong, M.S.; Xing, H.; Kwan, M.-P.; Zhu, R. Assessing the Country-Level Excess All-Cause Mortality and the Impacts of Air Pollution and Human Activity during the COVID-19 Epidemic. Int. J. Environ. Res. Public Health 2021, 18, 6883. https://doi.org/10.3390/ijerph18136883
Meng Y, Wong MS, Xing H, Kwan M-P, Zhu R. Assessing the Country-Level Excess All-Cause Mortality and the Impacts of Air Pollution and Human Activity during the COVID-19 Epidemic. International Journal of Environmental Research and Public Health. 2021; 18(13):6883. https://doi.org/10.3390/ijerph18136883
Chicago/Turabian StyleMeng, Yuan, Man Sing Wong, Hanfa Xing, Mei-Po Kwan, and Rui Zhu. 2021. "Assessing the Country-Level Excess All-Cause Mortality and the Impacts of Air Pollution and Human Activity during the COVID-19 Epidemic" International Journal of Environmental Research and Public Health 18, no. 13: 6883. https://doi.org/10.3390/ijerph18136883
APA StyleMeng, Y., Wong, M. S., Xing, H., Kwan, M.-P., & Zhu, R. (2021). Assessing the Country-Level Excess All-Cause Mortality and the Impacts of Air Pollution and Human Activity during the COVID-19 Epidemic. International Journal of Environmental Research and Public Health, 18(13), 6883. https://doi.org/10.3390/ijerph18136883










