Psychological Support Interventions for Healthcare Providers and Informal Caregivers during the COVID-19 Pandemic: A Systematic Review of the Literature
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
- -
- (“informal caregiver” OR parent*) AND (“emotional support” OR “psychological support” OR “psychological assistance”) AND (Covid-19) AND (“well-being” OR “mental health” OR “quality of life” OR anxiety OR depression OR distress OR psych*).
- -
- (“health care provider” OR “formal caregiver”) AND (“emotional support” OR “psychological support” OR “psychological assistance”) AND (Covid-19) AND (“well-being” OR “mental health” OR “quality of life” OR anxiety OR depression OR distress OR psych*).
2.2. Inclusion and Exclusion Criteria
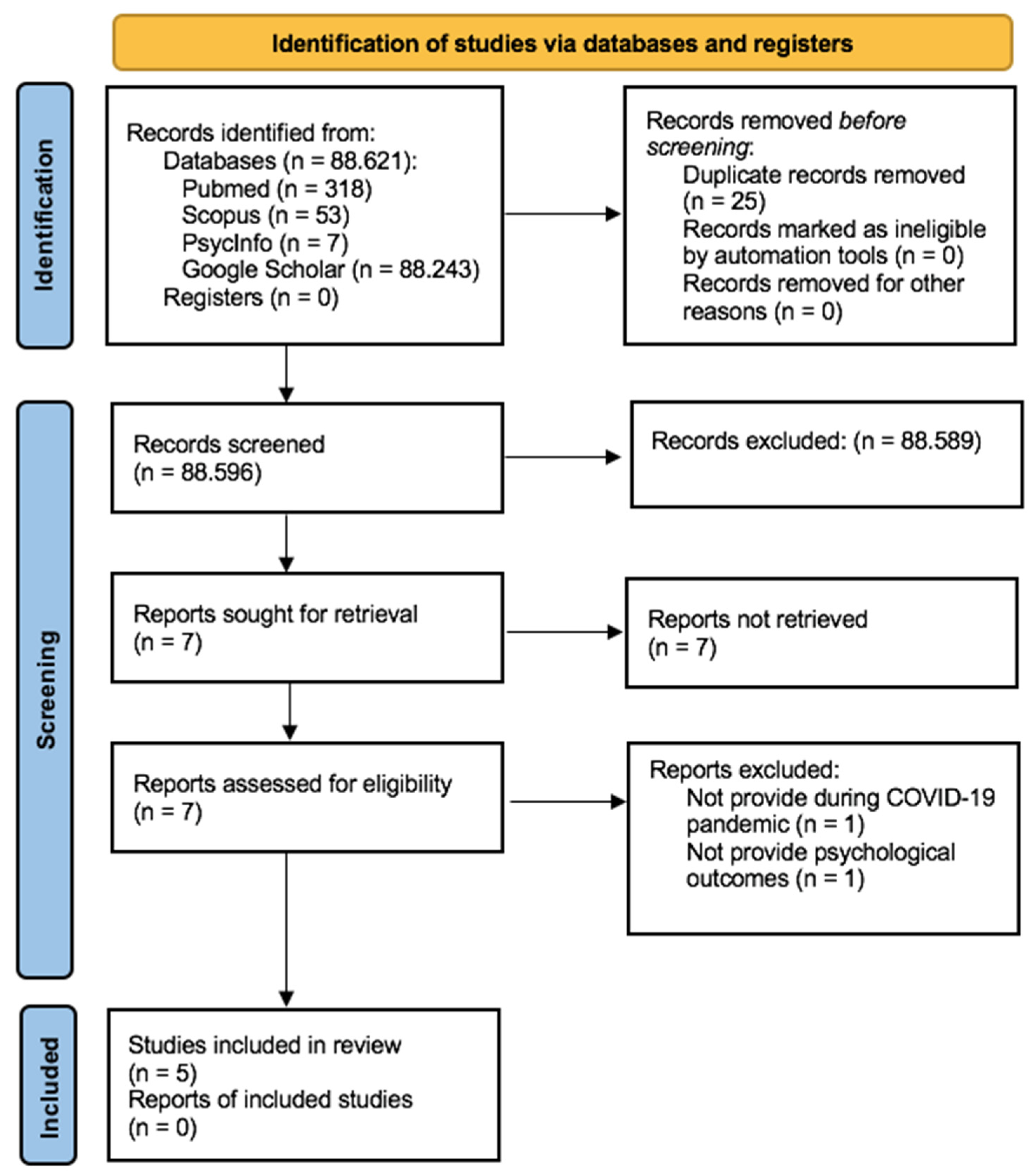
2.3. Study Selection
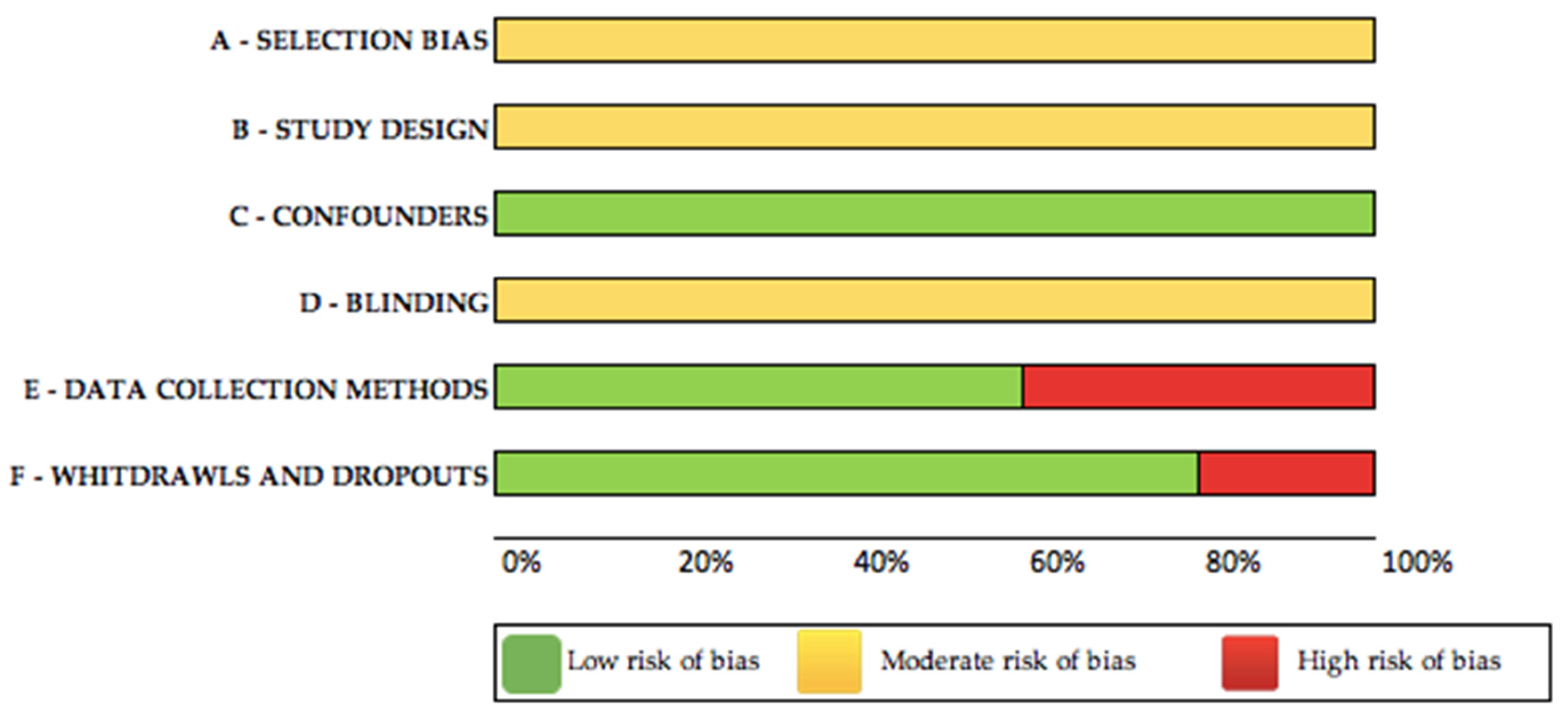
2.4. Assessment of Risk of Bias
2.5. Data Extraction and Synthesis
3. Results
3.1. Characteristics of the Included Studies
3.2. Psychological Support Interventions for HCPs
3.3. Psychological Support Interventions for Informal Caregivers
4. Discussion
4.1. Strengths and Limitations
4.2. Future Research and Practical Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Director-General’s Statement on IHR Emergency Committee on Novel Coronavirus (2019-nCoV). 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-statement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov) (accessed on 6 May 2021).
- Bonaccorsi, G.; Pierri, F.; Cinelli, M.; Flori, A.; Galeazzi, A.; Porcelli, F.; Schmidt, A.L.; Valensise, C.M.; Scala, A.; Quattrociocchi, W.; et al. Economic and social consequences of human mobility restrictions under COVID-19. Proc. Natl. Acad. Sci. USA 2020, 117, 15530–15535. [Google Scholar] [CrossRef]
- Guo, L.; Wu, M.; Zhu, Z.; Zhang, L.; Peng, S.; Li, W.; Chen, H.; Fernández-Aranda, F.; Chen, J. Effectiveness and influencing factors of online education for caregivers of patients with eating disorders during COVID -19 pandemic in China. Eur. Eat. Disord. Rev. 2020, 28, 816–825. [Google Scholar] [CrossRef]
- Nguyen, H.C.; Nguyen, M.H.; Do, B.N.; Tran, C.Q.; Nguyen, T.T.P.; Pham, K.M.; Pham, L.V.; Tran, K.V.; Duong, T.T.; Tran, T.V.; et al. People with Suspected COVID-19 symptoms were more likely depressed and had lower health-related quality of life: The potential benefit of health literacy. J. Clin. Med. 2020, 9, 965. [Google Scholar] [CrossRef] [Green Version]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef]
- Lutgendorf, S.K.; Laudenslager, M.L. Care of the caregiver: Stress and dysregulation of inflammatory control in cancer caregivers. J. Clin. Oncol. 2009, 27, 2894–2895. [Google Scholar] [CrossRef] [PubMed]
- Parola, A.; Rossi, A.; Tessitore, F.; Troisi, G.; Mannarini, S. Mental health through the COVID-19 quarantine: A growth curve analysis on Italian young adults. Front. Psychol. 2020, 11, 567484. [Google Scholar] [CrossRef] [PubMed]
- Pietrabissa, G.; Simpson, S.G. Psychological consequences of social isolation during COVID-19 outbreak. Front. Psychol. 2020, 11, 2201. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Pearman, A.; Hughes, M.; Smith, E.L.; Neupert, S.D. Mental health challenges of United States healthcare professionals during COVID-19. Front. Psychol. 2020, 11, 2065. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.; Panzeri, A.; Pietrabissa, G.; Manzoni, G.M.; Castelnuovo, G.; Mannarini, S. The anxiety-buffer hypothesis in the time of COVID-19: When self-esteem protects from the impact of loneliness and fear on anxiety and depression. Front. Psychol. 2020, 11, 2177. [Google Scholar] [CrossRef]
- Rodrigues, R.; Simmons, C.; Schmidt, A.E.; Steiber, N. Care in times of COVID-19: The impact of the pandemic on informal caregiving in Austria. Eur. J. Ageing 2021, 1–11. [Google Scholar] [CrossRef]
- Li, J.; Song, Y. Formal and informal care. In Encyclopedia of Gerontology and Population Aging; Gu, D., Dupre, M., Eds.; Springer: Cham, Switzerland, 2019. [Google Scholar]
- Diniz, M.A.A.; Melo, B.R.D.S.; Neri, K.H.; Casemiro, F.G.; Figueiredo, L.C.; Gaioli, C.C.L.D.O.; Gratão, A.C.M. Estudo comparativo entre cuidadores formais e informais de idosos. Ciênc. Saúde Colet. 2018, 23, 3789–3798. [Google Scholar] [CrossRef]
- Wang, H.; Li, T.; Barbarino, P.; Gauthier, S.; Brodaty, H.; Molinuevo, J.L.; Xie, H.; Sun, Y.; Yu, E.; Tang, Y.; et al. Dementia care during COVID-19. Lancet 2020, 395, 1190–1191. [Google Scholar] [CrossRef]
- Russell, B.S.; Hutchison, M.; Tambling, R.; Tomkunas, A.J.; Horton, A.L. initial challenges of caregiving during COVID-19: Caregiver burden, mental health, and the parent–child relationship. Child Psychiatry Hum. Dev. 2020, 51, 671–682. [Google Scholar] [CrossRef]
- Giusti, E.M.; Pedroli, E.; D’Aniello, G.E.; Badiale, C.S.; Pietrabissa, G.; Manna, C.; Badiale, M.S.; Riva, G.; Castelnuovo, G.; Molinari, E. The psychological impact of the COVID-19 outbreak on health professionals: A cross-sectional study. Front. Psychol. 2020, 11, 1684. [Google Scholar] [CrossRef]
- Pucciarelli, G.; Vellone, E.; Savini, S.; Simeone, S.; Ausili, D.; Alvaro, R.; Lee, C.; Lyons, K. Roles of changing physical function and caregiver burden on quality of life in stroke. Stroke 2017, 48, 733–739. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.A.; Kunicki, Z.J.; Drohan, M.M.; Greaney, M.L. Exploring changes in caregiver burden and caregiving intensity due to COVID-19. Gerontol. Geriatr. Med. 2021, 7, 2333721421999279. [Google Scholar] [CrossRef]
- Mochari-Greenberger, H.; Mosca, L. caregiver burden and nonachievement of healthy lifestyle behaviors among family caregivers of cardiovascular disease patients. Am. J. Health Promot. 2012, 27, 84–89. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wiles, J. Informal caregivers’ experiences of formal support in a changing context. Health Soc. Care Community 2003, 11, 189–207. [Google Scholar] [CrossRef] [PubMed]
- Shiba, K.; Kondo, N.; Kondo, K. Informal and formal social support and caregiver burden: The AGES caregiver survey. J. Epidemiol. 2016, 26, 622–628. [Google Scholar] [CrossRef] [Green Version]
- Galehdar, N.; Toulabi, T.; Kamran, A.; Heydari, H. Exploring nurses’ perception about the care needs of patients with COVID-19: A qualitative study. BMC Nurs. 2020, 19, 1–8. [Google Scholar] [CrossRef]
- Cheng, W.; Zhang, F.; Liu, Z.; Zhang, H.; Lyu, Y.; Xu, H.; Hua, Y.; Gu, J.; Yang, Z.; Liu, J. A psychological health support scheme for medical teams in COVID-19 outbreak and its effectiveness. Gen. Psychiatry 2020, 33, e100288. [Google Scholar] [CrossRef]
- Cabarkapa, S.; Nadjidai, S.E.; Murgier, J.; Ng, C.H. The psychological impact of COVID-19 and other viral epidemics on frontline healthcare workers and ways to address it: A rapid systematic review. Brain Behav. Immunity Health 2020, 8, 100144. [Google Scholar] [CrossRef]
- Panzeri, A.; Ferrario, S.R.; Cerutti, P. Psychological differences among healthcare workers of a rehabilitation institute during the COVID-19 pandemic: A two-step study. Front. Psychol. 2021, 12, 636129. [Google Scholar] [CrossRef] [PubMed]
- Talevi, D.; Socci, V.; Carai, M.; Carnaghi, G.; Faleri, S.; Trebbi, E.; Di Bernardo, A.; Capelli, F.; Pacitti, F. Mental health outcomes of the CoViD-19 pandemic. Riv. Psichiatr. 2020, 55, 137–144. [Google Scholar]
- Bai, Y.; Lin, C.-C.; Lin, C.-Y.; Chao-Cheng, L.; Chue, C.-M.; Chou, P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr. Serv. 2004, 55, 1055–1057. [Google Scholar] [CrossRef]
- Liu, X.; Kakade, M.; Fuller, C.J.; Fan, B.; Fang, Y.; Kong, J.; Guan, Z.; Wu, P. Depression after exposure to stressful events: Lessons learned from the severe acute respiratory syndrome epidemic. Compr. Psychiatry 2012, 53, 15–23. [Google Scholar] [CrossRef]
- Julliard, K.; Klimenko, E.; Jacob, M.S. Definitions of health among healthcare providers. Nurs. Sci. Q. 2006, 19, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Muhammad, A.; Prince, H.A. Caring for dementia caregivers in times of the COVID-19 crisis: A systematic review. Am. J. Nurs. Res. 2020, 8, 552–561. [Google Scholar] [CrossRef]
- Giordano, F.; Scarlata, E.; Baroni, M.; Gentile, E.; Puntillo, F.; Brienza, N.; Gesualdo, L. Receptive music therapy to reduce stress and improve wellbeing in Italian clinical staff involved in COVID-19 pandemic: A preliminary study. Arts Psychother. 2020, 70, 101688. [Google Scholar] [CrossRef]
- Caillet, A.; Allaouchiche, B. COVID impact: Psychological disorders and COVID-19 among ICU caregivers in April and October 2020. Minerva Anestesiol. 2021. [Google Scholar] [CrossRef]
- Mojtahedzadeh, N.; Wirth, T.; Nienhaus, A.; Harth, V.; Mache, S. Job demands, resources and strains of outpatient caregivers during the COVID-19 pandemic in Germany: A qualitative study. Int. J. Environ. Res. Public Health 2021, 18, 3684. [Google Scholar] [CrossRef]
- Wade, M.; Prime, H.; Johnson, D.; May, S.S.; Jenkins, J.M.; Browne, D.T. The disparate impact of COVID-19 on the mental health of female and male caregivers. Soc. Sci. Med. 2021, 275, 113801. [Google Scholar] [CrossRef]
- Li, Q.; Zhang, H.; Zhang, M.; Li, T.; Ma, W.; An, C.; Chen, Y.; Liu, S.; Kuang, W.; Yu, X.; et al. Prevalence and risk factors of anxiety, depression, and sleep problems among caregivers of people living with neurocognitive disorders during the COVID-19 pandemic. Front. Psychiatry 2020, 11, 590343. [Google Scholar] [CrossRef] [PubMed]
- Pongan, E.; Dorey, J.-M.; Borg, C.; Getenet, J.C.; Bachelet, R.; Lourioux, C.; Laurent, B.; Rey, R.; Rouch, I. COVID-19: Association between increase of behavioral and psychological symptoms of dementia during lockdown and caregivers’ poor mental health. J. Alzheimer Dis. 2021, 80, 1713–1721. [Google Scholar] [CrossRef] [PubMed]
- van Pelt, M.; Morris, T.; Lilly, A.C.; Pian-Smith, M.C.M.; Karasik, L.; van Pelt, F. Supporting caregivers during COVID-19: Transforming compassionate care from a way of doing to being. AANA J. 2021, 89, 1–6. [Google Scholar]
- Li, Q.; Zhang, H.; Zhang, M.; Li, T.; Ma, W.; An, C.; Chen, Y.; Liu, S.; Kuang, W.; Yu, X.; et al. Mental health multimorbidity among caregivers of older adults during the COVID-19 epidemic. Am. J. Geriatr. Psychiatry 2021. [Google Scholar] [CrossRef] [PubMed]
- Lai, F.H.-Y.; Yan, E.W.-H.; Yu, K.K.-Y.; Tsui, W.-S.; Chan, D.T.-H.; Yee, B.K. The protective impact of telemedicine on persons with dementia and their caregivers during the COVID-19 pandemic. Am. J. Geriatr. Psychiatry 2020, 28, 1175–1184. [Google Scholar] [CrossRef]
- De Luca, R.; Rifici, C.; Pollicino, P.; Di Cara, M.; Miceli, S.; Sergi, G.; Sorrenti, L.; Romano, M.; Naro, A.; Billeri, L.; et al. ‘Online therapy’ to reduce caregiver’s distress and to stimulate post-severe acquired brain injury motor and cognitive recovery: A Sicilian hospital experience in the COVID era. J. Telemed. Telecare 2021, 1357633X21990195. [Google Scholar] [CrossRef]
- Khan, K.S.; Kunz, R.; Kleijnen, J.; Antes, G. Five steps to conducting a systematic review. J. R. Soc. Med. 2003, 96, 118–121. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Huang, X.; Lin, J.; Demner-Fushman, D. Evaluation of PICO as a knowledge representation for clinical questions. AMIA Annu. Symp. Proc. 2006, 2006, 359–363. [Google Scholar]
- Smith, V.; DeVane, D.; Begley, C.M.; Clarke, M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med. Res. Methodol. 2011, 11, 15. [Google Scholar] [CrossRef] [Green Version]
- Douglas, S.L.; Mazanec, P.; Lipson, A.R.; Day, K.; Blackstone, E.; Bajor, D.L.; Saltzman, J.; Krishnamurthi, S. Videoconference intervention for distance caregivers of patients with cancer: A randomized controlled trial. JCO Oncol. Pract. 2021, 17, e26–e35. [Google Scholar] [CrossRef] [PubMed]
- Samadi, S.A.; Bakhshalizadeh-Moradi, S.; Khandani, F.; Foladgar, M.; Poursaid-Mohammad, M.; McConkey, R. Using hybrid telepractice for supporting parents of children with ASD during the COVID-19 lockdown: A feasibility study in Iran. Brain Sci. 2020, 10, 892. [Google Scholar] [CrossRef]
- Thomas, B.; Ciliska, D.; Dobbins, M.; Micucci, S. A Process for systematically reviewing the literature: Providing the research evidence for public health nursing interventions. Worldviews Evid. Based Nurs. 2004, 1, 176–184. [Google Scholar] [CrossRef] [PubMed]
- Goulia, P.; Mantas, C.; Dimitroula, D.; Mantis, D.; Hyphantis, T. General hospital staff worries, perceived sufficiency of information and associated psychological distress during the A/H1N1 influenza pandemic. BMC Infect. Dis. 2010, 10, 322. [Google Scholar] [CrossRef] [Green Version]
- Khunti, K.; Griffiths, A.; Majeed, A.; Nagpaul, C.; Rao, M. Assessing risk for healthcare workers during the covid-19 pandemic. BMJ 2021, 372, n602. [Google Scholar] [CrossRef] [PubMed]
- Maunder, R.G.; Leszcz, M.; Savage, D.; Adam, M.A.; Peladeau, N.; Romano, D.; Rose, M.; Schulman, R.B. Applying the lessons of SARS to pandemic influenza. Can. J. Public Health 2008, 99, 486–488. [Google Scholar] [CrossRef]
- Naldi, A.; Vallelonga, F.; Di Liberto, A.; Cavallo, R.; Agnesone, M.; Gonella, M.; Sauta, M.D.; Lochner, P.; Tondo, G.; Bragazzi, N.L.; et al. COVID-19 pandemic-related anxiety, distress and burnout: Prevalence and associated factors in healthcare workers of North-West Italy. BJPsych Open 2021, 7, e27. [Google Scholar] [CrossRef]
- Vaughan, E.; Tinker, T. Effective health risk communication about pandemic influenza for vulnerable populations. Am. J. Public Health 2009, 99, S324–S332. [Google Scholar] [CrossRef] [PubMed]
- Kocsis, B.J.; Yellowlees, P. Telepsychotherapy and the therapeutic relationship: Principles, advantages, and case examples. Telemed. E Health 2018, 24, 329–334. [Google Scholar] [CrossRef]
- Poletti, B.; Tagini, S.; Brugnera, A.; Parolin, L.; Pievani, L.; Ferrucci, R.; Compare, A.; Silani, V. Telepsychotherapy: A leaflet for psychotherapists in the age of COVID-19. A review of the evidence. Couns. Psychol. Q. 2020, 1–16. [Google Scholar] [CrossRef]
- Anderson, G.; Carlbring, P.; Ljótsson, B.; Hedman, E. Guided internet-based CBT for common mental disorders. J. Contemp. Psychother. 2013, 43, 223–233. [Google Scholar] [CrossRef]
- Pietrabissa, G.; Manzoni, G.M.; Algeri, D.; Mazzucchelli, L.; Carella, A.; Pagnini, F.; Castelnuovo, G. Facebook use as access facilitator for consulting psychology. Aust. Psychol. 2015, 50, 299–303. [Google Scholar] [CrossRef]
- Jimison, H.; Gorman, P.; Woods, S.; Nygren, P.; Walker, M.; Norris, S.; Hersh, W. Barriers and drivers of health information technology use for the elderly, chronically ill, and underserved. Évid. Rep. Assess. 2008, 175, 1–1422. [Google Scholar]
- Or, C.K.L.; Karsh, B.-T. A systematic review of patient acceptance of consumer health information technology. J. Am. Med. Inform. Assoc. 2009, 16, 550–560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rubin, J.; Chisnell, D. How to plan, design, and conduct effective tests. In Handbook Of Usability Testing; Wiley: Hoboken, NJ, USA, 2008. [Google Scholar]
| Author, Year | Country | Study Design | Study Aim | Format | Recipients | Type of Intervention | |
|---|---|---|---|---|---|---|---|
| HEALTHCARE PROVIDERS (HCPs) | |||||||
| Cheng et al., 2020 | China | One group pre–post study | To evaluate the efficacy of a psychological support intervention in promoting positive emotion, maintaining teamwork efficiency, and preventing burnout | Digital (online chat) and in person | HCPs | Five cognitive modules | |
| Giordano et al., 2020 | Italy | One group pre–post study | To evaluate the efficacy of a psychological support intervention in reducing distress and improving well-being | Digital (playlist on a mobile phone) | HCPs | Receptive music therapy | |
| INFORMAL CAREGIVERS | |||||||
| De Luca et al., 2021 | Italy | One group pre–post study | To evaluate the efficacy of a psychological support intervention in reducing distress | Digital (online Skype therapy) | Informal caregivers of adults with a SARI | Cognitive and sensory–motor intervention | |
| Guo et al., 2020 | China | Pre–post comparative study | To compare the efficacy of a psychological support intervention in reducing depression and anxiety in caregivers of youth with/without eating disorders | Digital (online using WeChat or e-mail) | Informal caregivers of youths with EDs (IG) vs. informal caregivers of youths without MDs (CG) | Educational program on caregivers’ skills | |
| Lai et al., 2020 | China | Pre–post comparative study | To compare the efficacy of digital psychological support interventions to increase quality of life and self-efficacy | Digital (video conferencing platform (IG), phone calls (CG)) | Informal caregivers of adults with an NCD | Care service telehealth | |
| HEALTHCARE PROVIDERS (HCPs) | |||||||
| Cheng et al., 2020 | 155 | 35, (24–54) | 106 (68.4%) | Daily mood, feelings, gains and issues | DMI, SUF, GIS | T0: baseline, T1: 6 weeks | Mood improved in those who had significantly higher perceived gains (p < 0.001) and positive attitudes, and fewer issues |
| Giordano et al., 2020 | 34 | 31.8 (8.33), 22–59 | 22 (64.7%) | Stress, well-being | MTC | T0: baseline, T1: 1 week, T2: 2 weeks, T3: 3 weeks, T4: 4 weeks, T5: 5 weeks | T0–T1: tiredness, sadness, fear, and worry intensity decreased significantly with the BP (p < 0.05) T0–T1: tiredness, sadness, and worry intensity decreased significantly with the EP (p < 0.05) T0–T5: perceived sadness (p < 0.03), fear (p < 0.001), and worry (p < 0.006) decreased significantly with the BP T0–T5: perceived tiredness (p < 0.0001), sadness (p < 0.002), fear (p < 0.003), and worry intensity (p < 0.04) decreased significantly with the EP |
| INFORMAL CAREGIVERS | |||||||
| De Luca et al., 2021 | 25 | 55 (12); 24–74 | 8 (32%) | Anxiety, perceived care burden | SAS, ZBI-22 | T0: baseline, T1: 12 weeks | Anxiety and perceived care burden reduced significantly (p < 0.0001) |
| Guo et al., 2020 | 508 (IG = 254; CG = 254) | IG = 47.0 (4.3); CG = 46.6 (4.2) | IG = 214 (84.3%) CG = 213 (83.9%) | Depression, anxiety | PHQ-9, GAD-7 | T0: baseline, T1: 4 weeks | T0–T1: no significant effect was observed on depression and anxiety Caregivers of older patients (p = 0.037) and not living with patients (p = 0.006) had lower PHQ-9 scores, caregivers of patients with a shorter duration of illness (p = 0.041) had lower GAD-7 scores |
| Lai et al., 2020 | 60 (IG = 30; CG = 30) | IG = 72.43 (0.80), 66–82; CG = 71.83 (0.80), 66–82 | IG = 17 (56.6%) CG = 18 (60%) | QoL, perceived care burden, self-efficacy | SF-36V2, ZBI; RCSES | T0: baseline, T1: 4 weeks | T0–T1: SF-36v2, ZBI, RCSES scores increased significantly in the IG (p < 0.001) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bertuzzi, V.; Semonella, M.; Bruno, D.; Manna, C.; Edbrook-Childs, J.; Giusti, E.M.; Castelnuovo, G.; Pietrabissa, G. Psychological Support Interventions for Healthcare Providers and Informal Caregivers during the COVID-19 Pandemic: A Systematic Review of the Literature. Int. J. Environ. Res. Public Health 2021, 18, 6939. https://doi.org/10.3390/ijerph18136939
Bertuzzi V, Semonella M, Bruno D, Manna C, Edbrook-Childs J, Giusti EM, Castelnuovo G, Pietrabissa G. Psychological Support Interventions for Healthcare Providers and Informal Caregivers during the COVID-19 Pandemic: A Systematic Review of the Literature. International Journal of Environmental Research and Public Health. 2021; 18(13):6939. https://doi.org/10.3390/ijerph18136939
Chicago/Turabian StyleBertuzzi, Vanessa, Michelle Semonella, Denise Bruno, Chiara Manna, Julian Edbrook-Childs, Emanuele M. Giusti, Gianluca Castelnuovo, and Giada Pietrabissa. 2021. "Psychological Support Interventions for Healthcare Providers and Informal Caregivers during the COVID-19 Pandemic: A Systematic Review of the Literature" International Journal of Environmental Research and Public Health 18, no. 13: 6939. https://doi.org/10.3390/ijerph18136939
APA StyleBertuzzi, V., Semonella, M., Bruno, D., Manna, C., Edbrook-Childs, J., Giusti, E. M., Castelnuovo, G., & Pietrabissa, G. (2021). Psychological Support Interventions for Healthcare Providers and Informal Caregivers during the COVID-19 Pandemic: A Systematic Review of the Literature. International Journal of Environmental Research and Public Health, 18(13), 6939. https://doi.org/10.3390/ijerph18136939








