Analyses of Child and Youth Self-Poisoning Hospitalizations by Substance and Socioeconomic Status
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Overview
2.2. Data Sources and Characteristics
2.3. Data Analysis
3. Results
3.1. Overview of Self-Poisoning Hospitalizations
3.2. Self-Poisoning by Substance
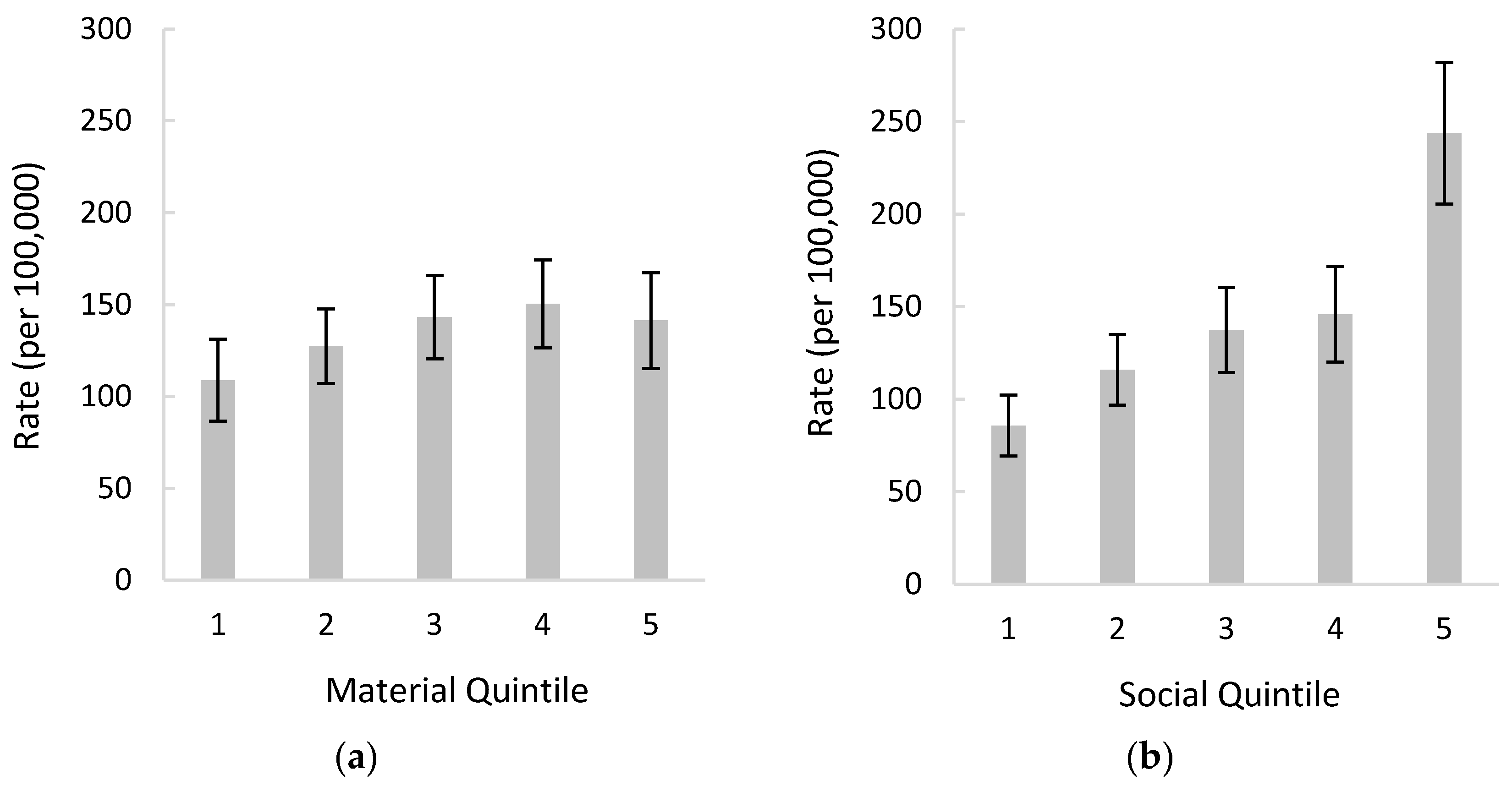
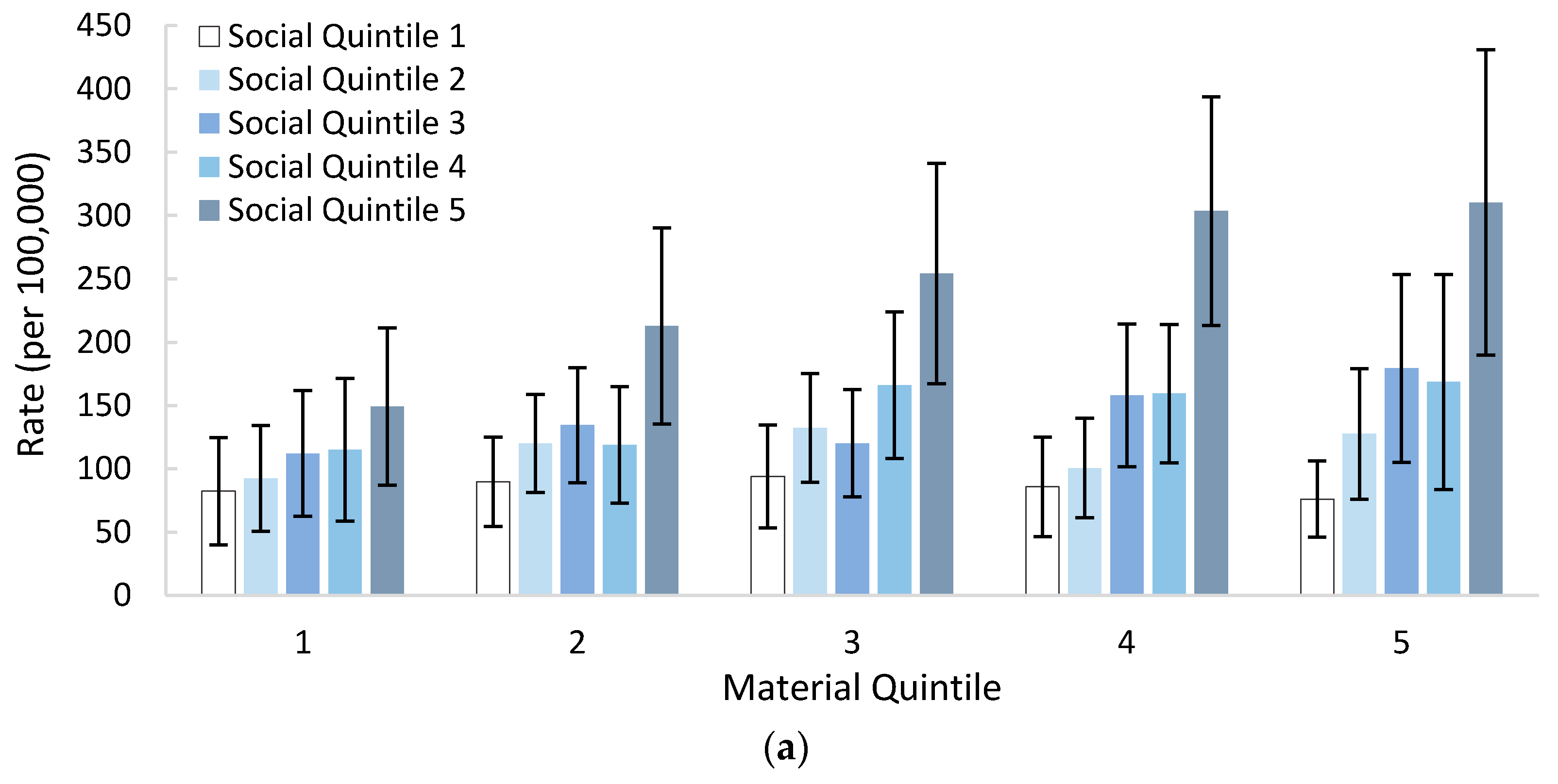
3.3. Self-Poisoning by Material and Social Deprivation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Patton, G.C.; Coffey, C.; Sawyer, S.M.; Viner, R.M.; Haller, D.; Bose, K.; Vos, T.; Ferguson, J.; Mathers, C.D. Global patterns of mortality in young people: A systematic analysis of population health data. Lancet 2009, 374, 881–892. [Google Scholar] [CrossRef]
- Canner, J.K.; Giuliano, K.; Selvarajah, S.; Hammond, E.R.; Schneider, E.B. Emergency department visits for attempted suicide and self harm in the USA: 2006–2013. Epidemiol. Psychiatr. Sci. 2018, 27, 94–102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hawton, K.; Bale, L.; Brand, F.; Townsend, E.; Ness, J.; Waters, K.; Clements, C.; Kapur, N.; Geulayov, G. Mortality in children and adolescents following presentation to hospital after non-fatal self-harm in the Multicentre Study of Self-harm: A prospective observational cohort study. Lancet Child Adolesc. Health 2020, 4, 111–120. [Google Scholar] [CrossRef]
- Mars, B.; Heron, J.; Crane, C.; Hawton, K.; Lewis, G.; Macleod, J.; Tilling, K.; Gunnell, D. Clinical and social outcomes of adolescent self harm: Population based birth cohort study. BMJ 2014, 349, g5954. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Geulayov, G.; Casey, D.; McDonald, K.; Foster, P.; Pritchard, K.; Wells, C.; Clements, C.; Kapur, N.; Ness, J.; Waters, K.; et al. Incidence of suicide, hospital-presenting non-fatal self-harm, and community-occurring non-fatal self-harm in adolescents in England (the iceberg model of self-harm): A retrospective study. Lancet Psychiatry 2018, 5, 167–174. [Google Scholar] [CrossRef] [Green Version]
- Cairns, R.; Karanges, E.A.; Wong, A.; Brown, J.A.; Robinson, J.; Pearson, S.-A.; Dawson, A.H.; Buckley, N.A. Trends in self-poisoning and psychotropic drug use in people aged 5–19 years: A population-based retrospective cohort study in Australia. BMJ Open 2019, 9, e026001. [Google Scholar] [CrossRef] [PubMed]
- Spiller, H.A.; Ackerman, J.P.; Spiller, N.E.; Casavant, M.J. Sex- and Age-specific Increases in Suicide Attempts by Self-Poisoning in the United States among Youth and Young Adults from 2000 to 2018. J. Pediatr. 2019, 210, 201–208. [Google Scholar] [CrossRef]
- Pawer, S.; Rajabali, F.; Smith, J.; Zheng, A.; Dhatt, A.; Purssell, R.; Pike, I. Self-poisoning among British Columbian children and youth: Demographic and geographic characteristics. BC Med. J. 2021, 63, 158–164. [Google Scholar]
- Schreier, H.M.C.; Chen, E. Socioeconomic status and the health of youth: A multilevel, multidomain approach to conceptualizing pathways. Psychol. Bull. 2013, 139, 606–654. [Google Scholar] [CrossRef] [PubMed]
- Jablonska, B.; Lindberg, L.; Lindblad, F.; Hjern, A. Ethnicity, socio-economic status and self-harm in Swedish youth: A national cohort study. Psychol. Med. 2008, 39, 87–94. [Google Scholar] [CrossRef]
- Kokkevi, A.; Rotsika, V.; Arapaki, A.; Richardson, C. Adolescents’ self-reported suicide attempts, self-harm thoughts and their correlates across 17 European countries. J. Child Psychol. Psychiatry 2011, 53, 381–389. [Google Scholar] [CrossRef]
- Lodebo, B.T.; Möller, J.; Larsson, J.-O.; Engström, K. Socioeconomic position and self-harm among adolescents: A population-based cohort study in Stockholm, Sweden. Child Adolesc. Psychiatry Ment. Health 2017, 11, 46. [Google Scholar] [CrossRef] [PubMed]
- Settipani, C.A.; Hawke, L.; Virdo, G.; Yorke, E.; Mehra, K.; Henderson, J. Social Determinants of Health among Youth Seeking Substance Use and Mental Health Treatment. J. Can. Acad. Child Adolesc. Psychiatry 2018, 27, 213–221. [Google Scholar]
- Gamache, P.; Hamel, D.; Blaser, C. The Material and Social Deprivation Index: A Summary. 2019. Available online: https://www.inspq.qc.ca/sites/default/files/publications/2639_material_social_deprivation_index.pdf (accessed on 15 April 2021).
- Institut National de Sante Publique du Quebec. The Challenges of Updating the Deprivation Index with Data from the 2011 Census and the National Household Survey (NHS); Institut National de Sante Publique du Quebec: Montreal, QC, Canada, 2016. [Google Scholar]
- Rajabali, F.; Zheng, A.; Turcotte, K.; Zhang, L.R.; Kao, D.; Rasali, D.; Oakey, M.; Pike, I. The association of material deprivation component measures with injury hospital separations in British Columbia, Canada. Inj. Epidemiol. 2019, 6, 20. [Google Scholar] [CrossRef]
- Zuijdwijk, C.S.; Cuerden, M.; Mahmud, F.H. Social Determinants of Health on Glycemic Control in Pediatric Type 1 Diabetes. J. Pediatr. 2013, 162, 730–735. [Google Scholar] [CrossRef] [PubMed]
- Tørmoen, A.J.; Rossow, I.; Larsson, B.; Mehlum, L. Nonsuicidal self-harm and suicide attempts in adolescents: Differences in kind or in degree? Soc. Psychiatry Psychiatr. Epidemiol. 2013, 48, 1447–1455. [Google Scholar] [CrossRef]
- Klonsky, E.D. Non-suicidal self-injury in United States adults: Prevalence, sociodemographics, topography and functions. Psychol. Med. 2011, 41, 1981–1986. [Google Scholar] [CrossRef] [PubMed]
- Canadian Institute for Health Information. Canadian Coding Standards for Version 2018 ICD-10-CA and CCI. 2018; Canadian Institute for Health Information: Montreal, QC, Canada, 2018. [Google Scholar]
- Census Profile, 2011 Census [Internet]. Statistics Canada. 2011. Available online: https://www12.statcan.gc.ca/census-recensement/2011/dp-pd/prof/index.cfm?Lang=E (accessed on 18 December 2019).
- Census Profile, 2016 Census [Internet]. Statistics Canada. 2016. Available online: https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/index.cfm?Lang=E (accessed on 18 December 2019).
- Kordrostami, R.; Akhgari, M.; Ameri, M.; Ghadipasha, M.; Aghakhani, K. Forensic toxicology analysis of self-poisoning suicidal deaths in Tehran, Iran; trends between 2011–2015. DARU J. Pharm. Sci. 2017, 25, 15. [Google Scholar] [CrossRef] [Green Version]
- Chafe, R.; Aslanova, R.; Hamud, O.; Gregory, P.; Newhook, L.A. Hospitalizations due to self-poisoning at a Canadian paediatric hospital. Paediatr. Child Health 2017, 23, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Jiang, A.; Smith, J.; Rajabali, F.; Zheng, A.; Purssell, R.; Pike, I. Patterns in poisoning hospitalizations and deaths in British Columbia, 2008 to 2013. BC Med. J. 2018, 60, 495–502. Available online: https://www.bcmj.org/articles/patterns-poisoning-hospitalizations-and-deaths-british-columbia-2008-2013 (accessed on 31 August 2019).
- Tyrrell, E.G.; Kendrick, D.; Sayal, K.; Orton, E. Poisoning substances taken by young people: A population-based cohort study. Br. J. Gen. Pract. 2018, 68, e703–e710. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spiller, H.A.; Ackerman, J.P.; Smith, G.A.; Kistamgari, S.; Funk, A.R.; McDermott, M.R.; Casavant, M.J. Suicide attempts by self-poisoning in the United States among 10–25 year olds from 2000 to 2018: Substances used, temporal changes and demographics. Clin. Toxicol. 2019, 58, 676–687. [Google Scholar] [CrossRef] [PubMed]
- Zakharov, S.; Navratil, T.; Pelclova, D. Suicide attempts by deliberate self-poisoning in children and adolescents. Psychiatry Res. 2013, 210, 302–307. [Google Scholar] [CrossRef]
- Rotermann, M.; Sanmartin, C.; Hennessy, D.; Arthur, M. Prescription medication use by Canadians aged 6 to 79. Health Rep. 2014, 25, 3. [Google Scholar]
- Qin, P.; Jepsen, P.; Nørgård, B.; Agerbo, E.; Mortensen, P.B.; Vilstrup, H.; Sørensen, H.T. Hospital admission for non-fatal poisoning with weak analgesics and risk for subsequent suicide: A population study. Psychol. Med. 2009, 39, 1867–1873. [Google Scholar] [CrossRef] [PubMed]
- Partnership for a Drug Free America. Generation Rx: National Study Confirms Abuse of Prescription and Over-the-Counter Drugs; Partnership for a Drug Free America: Washington, DC, USA, 2006. [Google Scholar]
- Hawton, K.; Bergen, H.; Simkin, S.; Dodd, S.; Pocock, P.; Bernal, W.; Gunnell, D.; Kapur, N. Long term effect of reduced pack sizes of paracetamol on poisoning deaths and liver transplant activity in England and Wales: Interrupted time series analyses. BMJ 2013, 346, f403. [Google Scholar] [CrossRef] [Green Version]
- Bridge, S. Suicide prevention-targeting the patient at risk. Aust. Fam. Physician 2006, 35, 335–338. [Google Scholar] [PubMed]
- O’Connor, P.J.; Martin, B.; Weeks, C.S.; Ong, L. Factors that influence young people’s mental health help-seeking behaviour: A study based on the Health Belief Model. J. Adv. Nurs. 2014, 70, 2577–2587. [Google Scholar] [CrossRef]
- Foundry Virtual BC [Internet]. Available online: https://foundrybc.ca/virtual (accessed on 14 May 2020).
- Muehlenkamp, J.J.; Walsh, B.W.; McDade, M. Preventing Non-Suicidal Self-Injury in Adolescents: The Signs of Self-Injury Program. J. Youth Adolesc. 2009, 39, 306–314. [Google Scholar] [CrossRef]
- BC Coroner. Supporting Youth and Health Professionals: A Report on Youth Suicides; 2019. Available online: https://www2.gov.bc.ca/assets/gov/birth-adoption-death-marriage-and-divorce/deaths/coroners-service/child-death-review-unit/reports-publications/youth_suicide_drp_report_2018.pdf (accessed on 10 May 2020).
- Smith, A.; Peled, M. Talking About Youth Health: An Example of Engaging Youth to Improve Child and Youth Health Indicators in British Columbia, Canada. Child Indic. Res. 2017, 10, 353–362. [Google Scholar] [CrossRef]
- Blane, D.; Townsend, P.; Phillimore, P.; Beattie, A. Health and Deprivation: Inequality and the North. Br. J. Sociol. 1989, 40, 344. [Google Scholar] [CrossRef]
- Statistics Canada. Census family-2011 Census Dictionary [Internet]. 2011. Available online: https://www12.statcan.gc.ca/census-recensement/2011/ref/dict/fam004-eng.cfm (accessed on 8 May 2020).
- Butler, C.; Joiner, R.; Bradley, R.; Bowles, M.; Bowes, A.; Russell, C.; Roberts, V. Self-harm prevalence and ideation in a community sample of cis, trans and other youth. Int. J. Transgend. 2019, 20, 447–458. [Google Scholar] [CrossRef] [PubMed]
- Rimes, K.A.; Goodship, N.; Ussher, G.; Baker, D.; West, E. Non-binary and binary transgender youth: Comparison of mental health, self-harm, suicidality, substance use and victimization experiences. Int. J. Transgend. 2019, 20, 230–240. [Google Scholar] [CrossRef] [PubMed]
- WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19-11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 5 March 2021).

| Age Group | Substance | Male | Female | Overall |
|---|---|---|---|---|
| 10–14 | Nonopioid analgesics, antipyretics, and antirheumatics | 2.9 (1.8–4.0) | 53.4 (48.7–58.2) | 27.6 (25.2–30.0) |
| Antiepileptic, sedative–hypnotic, antiparkinsonism, and psychotropic drugs | 3.5 (2.3–4.7) | 37.7 (33.7–41.6) | 20.2 (18.1–22.2) | |
| Unspecified drugs, medicaments, and biological substances | 1.4 (0.7–2.2) | 9.4 (7.4–11.3) | 5.3 (4.3–6.3) | |
| Other drugs acting on the autonomic nervous system | 0.7 (0.2–1.3) | 3.6 (2.4–4.8) | 2.1 (1.5–2.8) | |
| Narcotics and psychodysleptics | 0.2 (0.0–0.5) | 1.7 (0.9–2.6) | 1.0 (0.5–1.4) | |
| Other and unspecified chemical and noxious substances | 0.5 (0.1–1.0) | 3.4 (2.2–4.6) | 1.9 (1.3–2.5) | |
| Organic solvents and hallogenated hydrocarbons and their vapours | 0.7 (0.2–1.3) | 1.4 (0.6–2.2) | 1.1 (0.6–1.5) | |
| Alcohol | 0.0 (0.0–0.0) | 1.0 (0.3–1.6) | 0.5 (0.2–0.8) | |
| Gases and vapours | 0.0 (0.0–0.0) | 0.5 (0.1–1.0) | 0.3 (0.0–0.5) | |
| Other substances ^ | 0.0 (0.0–0.0) | 1.1 (0.4–1.8) | 0.5 (0.2–0.9) | |
| 15–19 | Nonopioid analgesics, antipyretics, and antirheumatics | 24.9 (22.0–27.8) | 127.2 (120.5–134.0) | 74.3 (70.7–77.9) |
| Antiepileptic, sedative–hypnotic, antiparkinsonism, and psychotropic drugs | 28.9 (25.8–32.0) | 110.2 (103.9–116.5) | 68.1 (64.7–71.5) | |
| Unspecified drugs, medicaments, and biological substances | 4.9 (3.6–6.1) | 16.0 (13.6–18.4) | 10.2 (8.9–11.6) | |
| Other drugs acting on the autonomic nervous system | 2.0 (1.2–2.8) | 10.4 (8.5–12.4) | 6.1 (5.0–7.1) | |
| Narcotics and psychodysleptics | 2.9 (1.9–3.8) | 5.4 (4.0–6.8) | 4.1 (3.2–4.9) | |
| Other and unspecified chemical and noxious substances | 1.0 (0.5–1.6) | 5.6 (4.2–7.0) | 3.2 (2.5–4.0) | |
| Organic solvents and hallogenated hydrocarbons and their vapours | 1.0 (0.5–1.6) | 3.0 (1.9–4.0) | 2.0 (1.4–2.6) | |
| Alcohol | 1.2 (0.6–1.9) | 2.9 (1.9–3.9) | 2.0 (1.4–2.6) | |
| Gases and vapours | 0.3 (0.0–0.7) | 0.8 (0.3–1.4) | 0.6 (0.3–0.9) | |
| Other substances ^ | 0.2 (0.0–0.4) | 2.0 (1.2–2.9) | 1.1 (0.6–1.5) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pawer, S.; Rajabali, F.; Zheng, A.; Smith, J.; Purssell, R.; Pike, I. Analyses of Child and Youth Self-Poisoning Hospitalizations by Substance and Socioeconomic Status. Int. J. Environ. Res. Public Health 2021, 18, 7003. https://doi.org/10.3390/ijerph18137003
Pawer S, Rajabali F, Zheng A, Smith J, Purssell R, Pike I. Analyses of Child and Youth Self-Poisoning Hospitalizations by Substance and Socioeconomic Status. International Journal of Environmental Research and Public Health. 2021; 18(13):7003. https://doi.org/10.3390/ijerph18137003
Chicago/Turabian StylePawer, Samantha, Fahra Rajabali, Alex Zheng, Jennifer Smith, Roy Purssell, and Ian Pike. 2021. "Analyses of Child and Youth Self-Poisoning Hospitalizations by Substance and Socioeconomic Status" International Journal of Environmental Research and Public Health 18, no. 13: 7003. https://doi.org/10.3390/ijerph18137003
APA StylePawer, S., Rajabali, F., Zheng, A., Smith, J., Purssell, R., & Pike, I. (2021). Analyses of Child and Youth Self-Poisoning Hospitalizations by Substance and Socioeconomic Status. International Journal of Environmental Research and Public Health, 18(13), 7003. https://doi.org/10.3390/ijerph18137003






