The Role of Myofunctional Therapy in Treating Sleep-Disordered Breathing: A State-of-the-Art Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Literature Search: Inclusion and Exclusion Criteria
- Population: Adults experiencing SDB, including snoring, upper airway resistance syndrome, or sleep apnoea.
- Intervention: Any type of MFT, although following Camacho et al. [5], we did not consider the range of MFT to include singing exercises or playing wind instruments.
- Comparison: From before to after MFT in uncontrolled studies (quasi experimental studies) or between intervention and no-intervention cohorts in controlled studies (cohort and clinical trials).
- Outcome: Six research questions were defined. (1) Is MFT useful for treating SDB? (2) Which patients benefit most from MFT? (3) What are the secondary effects of MFT? (4) Which type of MFT is best? (5) How should the effects of MFT be assessed? (6) How long do the effects of MFT last?
- Types of studies: Clinical trials, case series, and prospective and retrospective cohort studies published in peer-reviewed journals. We did not include case reports, theses, narrative reviews, or meeting communications. There were no restrictions by date or publication type. The search was last updated in February 2021. We included studies published in English, Spanish, German, French, Italian, or Portuguese.
- Exclusion criteria: (1) Studies that included syndromic patients, (2) duplicated publications, (3) studies in which the individual effect of MFT was not explored, (4) studies that did not answer any of the research questions, and (5) studies that included both adults and children without subgroup analysis.
2.2. Search Strategy
2.3. Data Extraction and Analysis
2.4. Level of Evidence
2.5. Statistical Analysis
3. Results
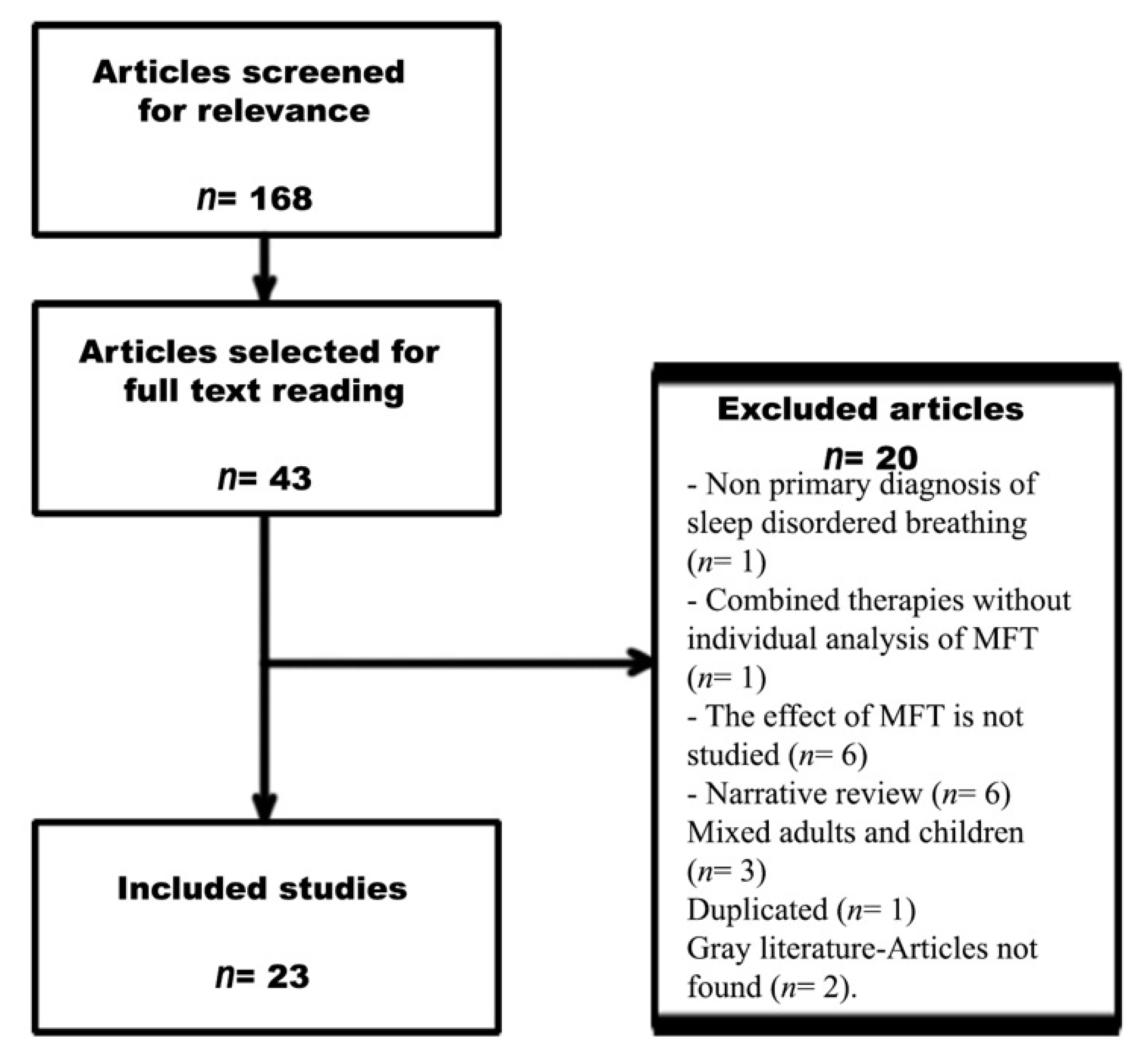
Search Results
4. Discussion
4.1. Question 1a: Is MFT Useful for Treating SDB—OSA?
4.1.1. Polysomnographic Variables
4.1.2. Clinical Variables
4.2. Question 1b: Is MFT Useful for Treating SDB?—Snoring
4.3. Question 1c: Is MFT Useful for Treating SDB?—Upper Airway Resistance Syndrome
4.4. Question 2: Which Patients Benefit Most from MFT?
4.4.1. Tongue and Lip Strength
4.4.2. Lingual Fraenulum
4.4.3. Severity
4.4.4. Malocclusion and Craniofacial Anomalies
4.4.5. Body Mass Index
4.4.6. Positional Apnoea
4.4.7. Nasal Patency
4.4.8. Tonsillar Hypertrophy
4.4.9. Scales
4.4.10. Age, Sex, and Tongue Volume
4.5. Question 3: What Are the Secondary Effects of MFT?
4.6. Question 4: Which Type of MFT Is Best?
4.7. Question 5: How Should the Effects of MFT Be Assessed?
4.8. Question 6: How Long Does the Effect Last?
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mediano, O.; González Mangado, N.; Montserrat, J.M.; Alonso-Álvarez, M.L.; Almendros, I.; Alonso-Fernández, A.; Barbé, F.; Borsini, E.; Caballero-Eraso, C.; Cano-Pumarega, I.; et al. International Consensus Document on Obstructive Sleep Apnea. Arch. Bronconeumol. 2021. [Google Scholar] [CrossRef]
- Eckert, D.J.; White, D.P.; Jordan, A.S.; Malhotra, A.; Wellman, A. Defining Phenotypic Causes of Obstructive Sleep Apnea. Identification of Novel Therapeutic Targets. Am. J. Respir. Crit. Care Med. 2013, 188, 996–1004. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puhan, M.A.; Suarez, A.; Lo Cascio, C.; Zahn, A.; Heitz, M.; Braendli, O. Didgeridoo Playing as Alternative Treatment for Obstructive Sleep Apnoea Syndrome: Randomised Controlled Trial. BMJ 2006, 332, 266–270. [Google Scholar] [CrossRef] [Green Version]
- O’Sullivan, D.; Wilk, S.; Michalowski, W.; Farion, K. Using PICO to Align Medical Evidence with MDs Decision Making Models. Stud. Health Technol. Inform. 2013, 192, 1057. [Google Scholar] [PubMed]
- Camacho, M.; Certal, V.F.; Abdullatif, J.; Zaghi, S.; Ruoff, C.M.; Capasso, R.; Kushida, C.A.; Landau, L. Myofunctional Therapy to Treat Obstructive Sleep Apnea: A Systematic Review and Meta-Analysis. Sleep 2015, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- OCEBM Levels of Evidence—Centre for Evidence-Based Medicine (CEBM), University of Oxford. Available online: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence (accessed on 9 June 2021).
- Atilgan, E.; Kunter, E.; Algun, Z.C. Are Oropharyngeal Exercises Effective in Obstructive Sleep Apnea Syndrome? J. Back Musculoskelet. Rehabil. 2020, 33, 209–216. [Google Scholar] [CrossRef]
- Suzuki, M.; Okamoto, T.; Akagi, Y.; Matsui, K.; Sekiguchi, H.; Satoya, N.; Inoue, Y.; Tatsuta, A.; Hagiwara, N. Efficacy of Oral Myofunctional Therapy in Middle-Aged to Elderly Patients with Obstructive Sleep Apnoea Treated with Continuous Positive Airway Pressure. J. Oral Rehabil. 2021, 48, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Hsu, B.; Emperumal, C.P.; Grbach, V.X.; Padilla, M.; Enciso, R. Effects of Respiratory Muscle Therapy on Obstructive Sleep Apnea: A Systematic Review and Meta-Analysis. J. Clin. Sleep Med. JCSM Off. Publ. Am. Acad. Sleep Med. 2020, 16, 785–801. [Google Scholar] [CrossRef] [PubMed]
- Erturk, N.; Calik-Kutukcu, E.; Arikan, H.; Savci, S.; Inal-Ince, D.; Caliskan, H.; Saglam, M.; Vardar-Yagli, N.; Firat, H.; Celik, A.; et al. The Effectiveness of Oropharyngeal Exercises Compared to Inspiratory Muscle Training in Obstructive Sleep Apnea: A Randomized Controlled Trial. Heart Lung J. Crit. Care 2020, 49, 940–948. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Oh, E.G.; Choi, M.; Choi, S.J.; Joo, E.Y.; Lee, H.; Kim, H.Y. Development and Evaluation of Myofunctional Therapy Support Program (MTSP) Based on Self-Efficacy Theory for Patients with Obstructive Sleep Apnea. Sleep Breath. 2020, 24, 1051–1058. [Google Scholar] [CrossRef]
- O’Connor-Reina, C.; Ignacio Garcia, J.M.; Rodriguez Ruiz, E.; Morillo Dominguez, M.D.C.; Ignacio Barrios, V.; Baptista Jardin, P.; Casado Morente, J.C.; Garcia Iriarte, M.T.; Plaza, G. Myofunctional Therapy App for Severe Apnea-Hypopnea Sleep Obstructive Syndrome: Pilot Randomized Controlled Trial. JMIR MHealth UHealth 2020, 8, e23123. [Google Scholar] [CrossRef]
- O’Connor Reina, C.; Plaza, G.; Ignacio-Garcia, J.M.; Baptista Jardin, P.; Garcia-Iriarte, M.T.; Casado-Morente, J.C.; De Vicente Gonzalez, E.; Rodriguez-Reina, A.; O’Connor Reina, C.; Plaza, G.; et al. New MHealth Application Software Based on Myofunctional Therapy Applied to Sleep-Disordered Breathing in Non-Compliant Subjects. Sleep Sci. Pract. 2020, 4, 3. [Google Scholar] [CrossRef]
- Camacho, M.; Guilleminault, C.; Wei, J.M.; Song, S.A.; Noller, M.W.; Reckley, L.K.; Fernandez-Salvador, C.; Zaghi, S. Oropharyngeal and Tongue Exercises (Myofunctional Therapy) for Snoring: A Systematic Review and Meta-Analysis. Eur. Arch. Oto-Rhino-Laryngol. 2018, 275, 849–855. [Google Scholar] [CrossRef] [PubMed]
- Verma, R.K.; Johnson, J.J.R.; Goyal, M.; Banumathy, N.; Goswami, U.; Panda, N.K. Oropharyngeal Exercises in the Treatment of Obstructive Sleep Apnoea: Our Experience. Sleep Breath. 2016, 20, 1193–1201. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, A.S.; Sharshar, R.S.; Elkolaly, R.M.; Serageldin, S.M. Upper Airway Muscle Exercises Outcome in Patients with Obstructive Sleep Apnea Syndrome. Egypt. J. Chest Dis. Tuberc. 2017, 66, 121–125. [Google Scholar] [CrossRef] [Green Version]
- Nemati, S.; Gerami, H.; Soltanipour, S.; Saberi, A.; Moghadam, S.K.; Setva, F. The Effects of Oropharyngeal-Lingual Exercises in Patients with Primary Snoring. Eur. Arch. Oto-Rhino-Laryngol. 2015, 272, 1027–1031. [Google Scholar] [CrossRef] [PubMed]
- Ieto, V.; Kayamori, F.; Montes, M.I.; Hirata, R.P.; Gregório, M.G.; Alencar, A.M.; Drager, L.F.; Genta, P.R.; Lorenzi-Filho, G. Effects of Oropharyngeal Exercises on Snoring: A Randomized Trial. Chest 2015, 148, 683–691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsumura, E.; Tonisi, G.A.B.R.; Vecina, A.L.C.; Inocêncio, L.B.; Guimarães, K.C.C.; Nemr, N.K. A percepção do acompanhante e do indivíduo com ronco/saos antes e após fonoterapia. Rev. CEFAC 2014, 16, 907–916. [Google Scholar] [CrossRef]
- Diaferia, G.; Badke, L.; Santos-Silva, R.; Bommarito, S.; Tufik, S.; Bittencourt, L. Effect of Speech Therapy as Adjunct Treatment to Continuous Positive Airway Pressure on the Quality of Life of Patients with Obstructive Sleep Apnea. Sleep Med. 2013, 14, 628–635. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, H.; Watanabe, A.; Akihiro, Y.; Takao, M.; Ikematsu, T.; Kimoto, S.; Asano, T.; Kawara, M. Pilot Study to Assess the Potential of Oral Myofunctional Therapy for Improving Respiration during Sleep. J. Prosthodont. Res. 2013, 57, 195–199. [Google Scholar] [CrossRef]
- Valbuza, J.S.; de Oliveira, M.M.; Conti, C.F.; Prado, L.B.F.; de Carvalho, L.B.C.; do Prado, G.F. Methods for Increasing Upper Airway Muscle Tonus in Treating Obstructive Sleep Apnea: Systematic Review. Sleep Breath. 2010, 14, 299–305. [Google Scholar] [CrossRef]
- Guimarães, K.C.; Drager, L.F.; Genta, P.R.; Marcondes, B.F.; Lorenzi-Filho, G. Effects of Oropharyngeal Exercises on Patients with Moderate Obstructive Sleep Apnea Syndrome. Am. J. Respir. Crit. Care Med. 2009, 179, 962–966. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Randerath, W.J.; Galetke, W.; Domanski, U.; Weitkunat, R.; Ruhle, K.-H. Tongue-Muscle Training by Intraoral Electrical Neurostimulation in Patients with Obstructive Sleep Apnea. Sleep 2004, 27, 254–259. [Google Scholar] [CrossRef] [Green Version]
- Goswami, U.; Black, A.; Krohn, B.; Meyers, W.; Iber, C. Smartphone-Based Delivery of Oropharyngeal Exercises for Treatment of Snoring: A Randomized Controlled Trial. Sleep Breath. 2019, 23, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Díaz, M.; Salazar, A.; Bravo, F.; Ocampo-Garcés, A. Tratamiento Del Síndrome de Apneas e Hipopneas Obstructivas Del Sueño Con Terapia Miofuncional Orofaríngea: Experiencia En Hospital Público de Chile. Rev. Otorrinolaringol. Cir. Cabeza Cuello 2019, 79, 395–403. [Google Scholar] [CrossRef] [Green Version]
- Kayamori, F.; Bianchini, E.M.G. Effects of Orofacial Myofunctional Therapy on the Symptoms and Physiological Parameters of Sleep Breathing Disorders in Adults: A Systematic Review. Rev. CEFAC 2017, 19, 868–878. [Google Scholar] [CrossRef] [Green Version]
- Baz, H.; Elshafey, M.; Elmorsy, S.; Abu-Samra, M. The Role of Oral Myofunctional Therapy in Managing Patients with Mild to Moderate Obstructive Sleep Apnea. PAN Arab. J. Rhinol. 2012, 2, 17–22. [Google Scholar]
- Weaver, T.E. Outcome Measurement in Sleep Medicine Practice and Research. Part 1: Assessment of Symptoms, Subjective and Objective Daytime Sleepiness, Health-Related Quality of Life and Functional Status. Sleep Med. Rev. 2001, 5, 103–128. [Google Scholar] [CrossRef] [PubMed]
- O’Connor-Reina, C.; Plaza, G.; Garcia-Iriarte, M.T.; Ignacio-Garcia, J.M.; Baptista, P.; Casado-Morente, J.C.; De Vicente, E. Tongue Peak Pressure: A Tool to Aid in the Identification of Obstruction Sites in Patients with Obstructive Sleep Apnea/Hypopnea Syndrome. Sleep Breath. 2019. [Google Scholar] [CrossRef]
- De Felício, C.M.; da Silva Dias, F.V.; Trawitzki, L.V.V. Obstructive Sleep Apnea: Focus on Myofunctional Therapy. Nat. Sci. Sleep 2018, 10, 271–286. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Engelke, W.; Engelhardt, W.; Mendoza-Gärtner, M.; Deccó, O.; Barrirero, J.; Knösel, M. Functional Treatment of Snoring Based on the Tongue-Repositioning Manoeuvre. Eur. J. Orthod. 2010, 32, 490–495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Folha, G.A.; Valera, F.C.P.; de Felício, C.M. Validity and Reliability of a Protocol of Orofacial Myofunctional Evaluation for Patients with Obstructive Sleep Apnea. Eur. J. Oral Sci. 2015, 123, 165–172. [Google Scholar] [CrossRef] [PubMed]
| Question | Available Evidence | Level of Evidence | Conclusions |
|---|---|---|---|
| Is MFT useful for treating SDB? (PSG variables) | 2 meta-analyses [5,10], 2 systematic reviews [23,28], 7 RCTs [11,12,14,19,21,24,25], 1 cohort [14], 5 quasi-experimental [9,16,17,22,29], and 1 case series [27] | Level 1a | Available evidence demonstrates a positive effect of MFT in reducing sleep apnoea as measured by PSG variables. |
| Is MFT useful for treating SDB? (sleepiness and QoL) | 2 meta-analyses [5,10], 2 systematic reviews [23,28], 8 RCTs [8,9,12,13,19,21,24,25], 1 cohort [14], 5 quasi-experimental [9,16,17,20,29], and 1 case series [27] | Level 1a | Available evidence demonstrates a positive effect of MFT in reducing self-reported sleepiness and increasing QoL. |
| Is MFT useful for treating SDB? (snoring) | 1 meta-analysis [15], 1 systematic review [28], 7 RCTs [8,11,12,19,24,25,26,29], 6 quasi-experimental [9,16,17,18,20] | Level 1a | Available evidence demonstrates a positive effect of MFT in reducing snoring as measured by objective (PSG) and subjective (scales) evaluation. |
| Is MFT useful for treating upper airway resistance syndrome? | None | None | There is no evidence regarding the use of MFT for upper airway resistance syndrome. |
| Which patients benefit most from MFT? | 1 RCT [11] and 1 quasi-experimental [17] | None | There is no evidence regarding the optimal method for patient selection for MFT. |
| What are the secondary effects of MFT? | 1 meta-analysis [10], 3 RCTs [8,11,12,13,19,21,24,25,26], and 1 cohort [14] | Level 1b | Available evidence suggests that MFT is a safe therapy. |
| Which type of MFT is best? | 1 RCT [11] | Level 2b | Available evidence has important flaws, and there is no evidence for making solid conclusions. |
| How well do patients adhere to MFT? | 9 RCTs [8,11,12,13,19,21,24,25,26], 7 quasi-experimental [9,16,17,18,20,22,29], and 1 case series [27] | Not applicable | Several variables can influence adherence to MFT. Available evidence is too heterogeneous to make solid conclusions about adherence. |
| How long do the effects of MFT last? | 1 RCT [21] and 1 case series [27] | Not applicable | There is no evidence. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carrasco-Llatas, M.; O’Connor-Reina, C.; Calvo-Henríquez, C. The Role of Myofunctional Therapy in Treating Sleep-Disordered Breathing: A State-of-the-Art Review. Int. J. Environ. Res. Public Health 2021, 18, 7291. https://doi.org/10.3390/ijerph18147291
Carrasco-Llatas M, O’Connor-Reina C, Calvo-Henríquez C. The Role of Myofunctional Therapy in Treating Sleep-Disordered Breathing: A State-of-the-Art Review. International Journal of Environmental Research and Public Health. 2021; 18(14):7291. https://doi.org/10.3390/ijerph18147291
Chicago/Turabian StyleCarrasco-Llatas, Marina, Carlos O’Connor-Reina, and Christian Calvo-Henríquez. 2021. "The Role of Myofunctional Therapy in Treating Sleep-Disordered Breathing: A State-of-the-Art Review" International Journal of Environmental Research and Public Health 18, no. 14: 7291. https://doi.org/10.3390/ijerph18147291
APA StyleCarrasco-Llatas, M., O’Connor-Reina, C., & Calvo-Henríquez, C. (2021). The Role of Myofunctional Therapy in Treating Sleep-Disordered Breathing: A State-of-the-Art Review. International Journal of Environmental Research and Public Health, 18(14), 7291. https://doi.org/10.3390/ijerph18147291







