The Ecology of Unsheltered Homelessness: Environmental and Social-Network Predictors of Well-Being among an Unsheltered Homeless Population
Abstract
:1. Introduction
1.1. Biophysical Dimensions of the Homeless Environment
1.2. Social Dimensions of the Homeless Environment
2. Materials and Methods
2.1. Nashville Unsheltered PEH Data
2.2. NOAA Global Historical Climatology Network (GHCN) Data
2.3. Statistical Models
3. Results
3.1. Characteristics of Sample Population
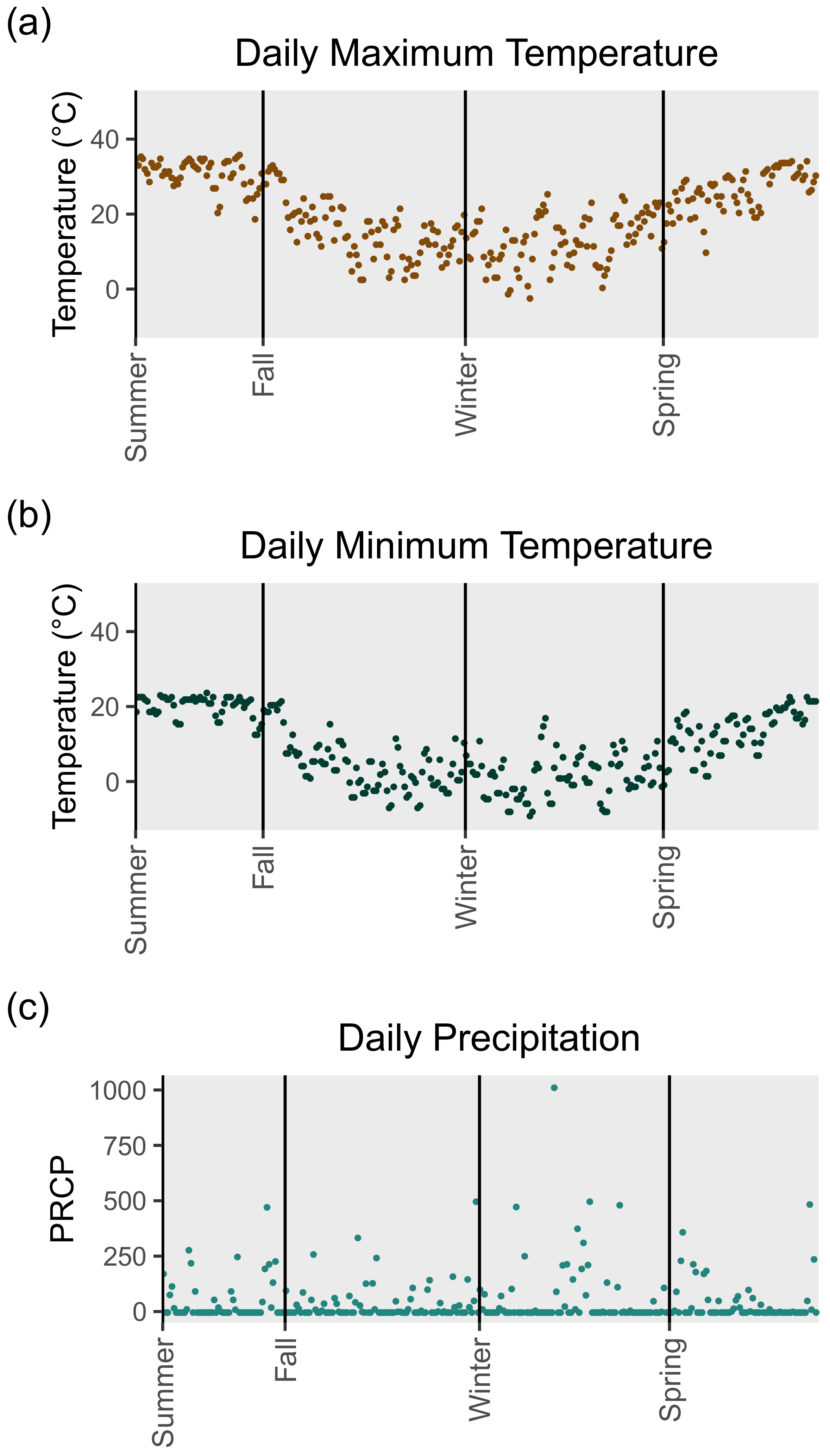
3.2. Nashville Weather Data
3.3. Sample Population Social Network Characteristics
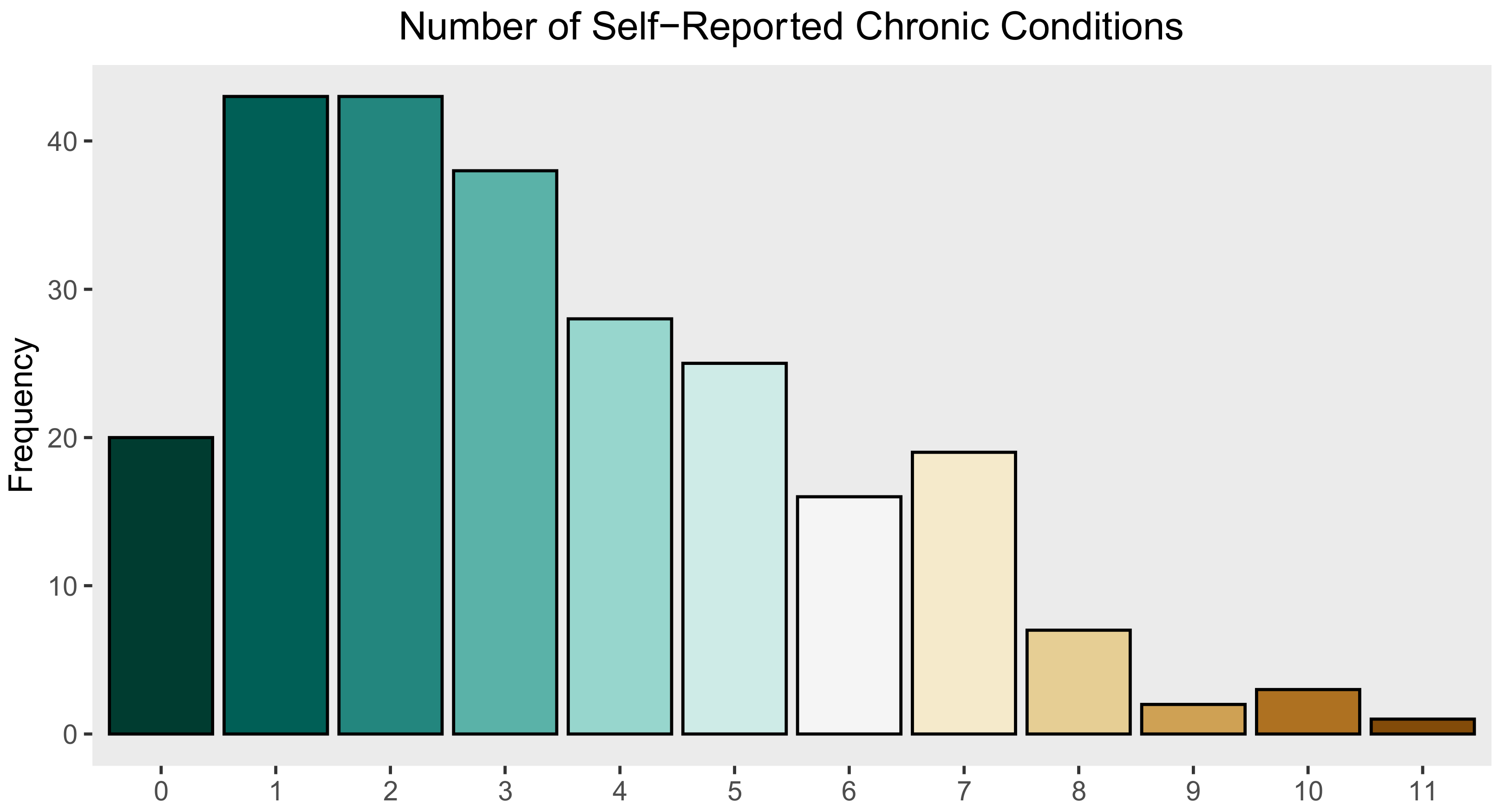
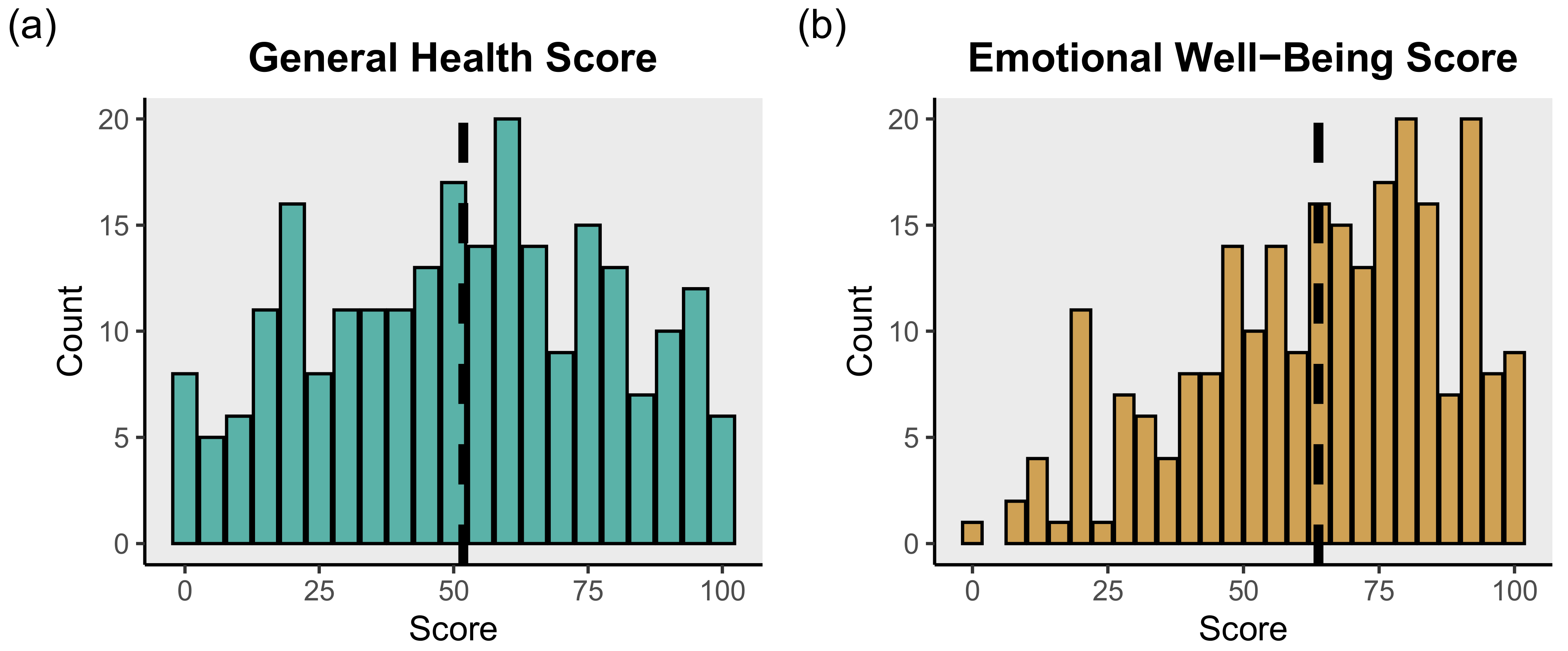
3.4. Sample Population Health Characteristics
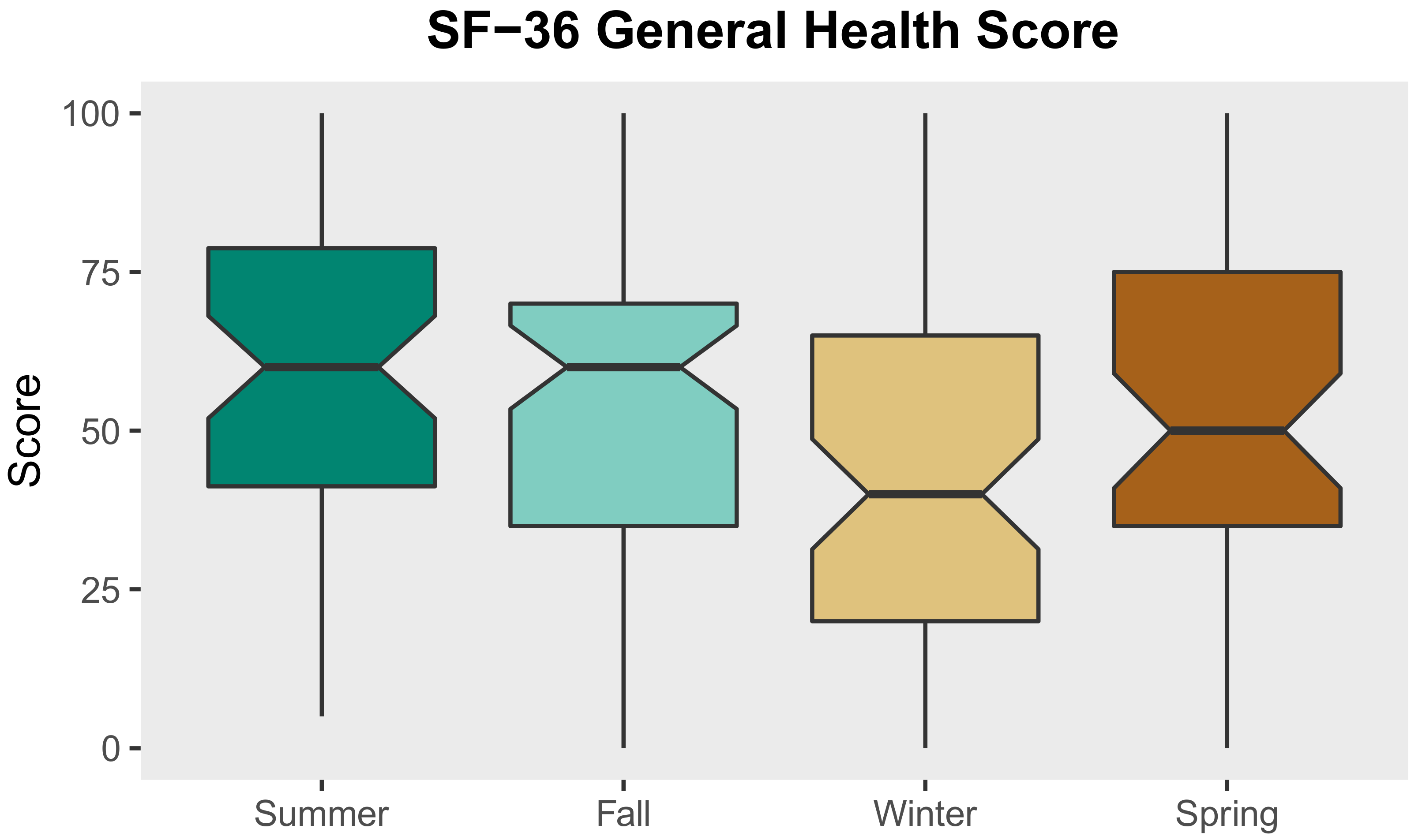
3.5. Fixed Effects Linear Regression Models: Social and Environmental Factors Associated with SF-36 General Health Scale Score
3.6. Fixed Effects Linear Regression Models: Social and Environmental Factors Associated with SF-36 Emotional Well-Being Scale Score
4. Discussion
4.1. Biophysical and Social Dimensions of the Unsheltered Homeless Environment
4.2. Implications for Health Impacts Due to Climate Change Among Homeless Populations
4.3. Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Baggett, T.P.; Hwang, S.W.; O’Connell, J.J.; Porneala, B.C.; Stringfellow, E.J.; Orav, E.J.; Singer, D.E.; Rigotti, N.A. Mortality among homeless adults in Boston: Shifts in causes of death over a 15-year period. JAMA Intern. Med. 2013, 173, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Baggett, T.P.; Chang, Y.; Singer, D.E.; Porneala, B.C.; Gaeta, J.M.; O’Connell, J.J.; Rigotti, N.A. Tobacco-, alcohol-, and drug-attributable deaths and their contribution to mortality disparities in a cohort of homeless adults in Boston. Am. J. Public Health 2015, 105, 1189–1197. [Google Scholar] [CrossRef]
- Fazel, S.; Geddes, J.R.; Kushel, M. The health of homeless people in high-income countries: Descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet 2014, 384, 1529–1540. [Google Scholar] [CrossRef] [Green Version]
- Hwang, S.W.; Orav, E.J.; O’Connell, J.J.; Lebow, J.M.; Brennan, T.A. Causes of Death in Homeless Adults in Boston. Ann. Intern. Med. 1997, 126, 625–628. [Google Scholar] [CrossRef] [PubMed]
- Kushel, M.B.; Vittinghoff, E.; Haas, J.S. Factors Associated With the Health Care Utilization of Homeless Persons. JAMA 2001, 285, 200–206. [Google Scholar] [CrossRef] [Green Version]
- North, C.S.; Eyrich, K.M.; Pollio, D.E.; Spitznagel, E.L. Are Rates of Psychiatric Disorders in the Homeless Population Changing? Am. J. Public Health 2004, 94, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Leibler, J.H.; Nguyen, D.D.; León, C.; Gaeta, J.M.; Perez, D. Personal Hygiene Practices among Urban Homeless Persons in Boston, MA. Int. J. Environ. Res. Public Health 2017, 14, 928. [Google Scholar] [CrossRef]
- Department of Housing and Urban Development. HUD 2020 Continuum of Care Homeless Assistance Programs Homeless Populations and Subpopulations; Department of Housing and Urban Development: Washington, DC, USA, 2020.
- Department of Housing and Urban Development. HUD’s Homeless Assistance Programs: A Guide to Counting Unsheltered Homeless People; Department of Housing and Urban Development: Washington, DC, USA, 2021.
- Levitt, A.J.; Culhane, D.P.; Degenova, J.; O’Quinn, P.; Bainbridge, J. Health and social characteristics of homeless adults in Manhattan who were chronically or not chronically unsheltered. Psychiatr. Serv. 2009, 60, 978–981. [Google Scholar] [CrossRef]
- Montgomery, A.E.; Szymkowiak, D.; Marcus, J.; Howard, P.; Culhane, D.P. Homelessness, unsheltered status, and risk factors for mortality: Findings from the 100 000 homes campaign. Public Health Rep. 2016, 131, 765–772. [Google Scholar] [CrossRef] [Green Version]
- Nyamathi, A.M.; Leake, B.; Gelberg, L. Sheltered versus nonsheltered homeless women. J. Gen. Intern. Med. 2000, 15, 565–572. [Google Scholar] [CrossRef] [Green Version]
- Harter, L.M.; Berquist, C.; Titsworth, B.S.; Novak, D.; Brokaw, T. The Structuring of Invisibility Among the Hidden Homeless: The Politics of Space, Stigma, and Identity Construction. J. Appl. Commun. Res. 2005, 33, 305–327. [Google Scholar] [CrossRef]
- Lee, B.A.; Tyler, K.A.; Wright, J.D. The New Homelessness Revisited. Annu. Rev. Sociol. 2010, 36, 501–521. [Google Scholar] [CrossRef] [Green Version]
- Snow, D.A.; Mulcahy, M. Space, Politics, and the Survival Strategies of the Homeless. Am. Behav. Sci. 2001, 45, 149–169. [Google Scholar] [CrossRef]
- Wasserman, J.A.; Clair, J.M. Housing Patterns of Homeless People: The Ecology of the Street in the Era of Urban Renewal. J. Contemp. Ethnogr. 2011, 40, 71–101. [Google Scholar] [CrossRef]
- Snow, D.A.; Anderson, L. Down on Their Luck: A Study of Homeless Street People, 1st ed.; University of California Press, Ltd.: London, UK, 1993. [Google Scholar]
- Agans, R.P.; Jefferson, M.T.; Bowling, J.M.; Zeng, D.; Yang, J.; Silverbush, M. Enumerating the hidden homeless: Strategies to estimate the homeless gone missing from a point-in-time count. J. Off. Stat. 2014, 30, 215–229. [Google Scholar] [CrossRef] [Green Version]
- Berry, B. A repeated observation approach for estimating the street homeless population. Eval. Rev. 2007, 31, 166–199. [Google Scholar] [CrossRef] [PubMed]
- Schneider, M.; Brisson, D.; Burnes, D. Do we really know how many are homeless?: An analysis of the point-in-time homelessness count. Fam. Soc. J. Contemp. Soc. Serv. 2016, 97, 321–329. [Google Scholar] [CrossRef]
- Nooe, R.M.; Patterson, D.A. The Ecology of Homelessness. J. Hum. Behav. Soc. Environ. 2010, 20, 105–152. [Google Scholar] [CrossRef]
- Toro, P.A.; Trickett, E.J.; Wall, D.D.; Salem, D.A. Homelessness in the United-States—An Ecological Perspective. Am. Psychol. 1991, 46, 1208–1218. [Google Scholar] [CrossRef] [PubMed]
- Altun, G.; Yilmaz, A.; Azmak, D. Deaths among homeless people in Istanbul. Forensic Sci. Int. 1999, 99, 143–147. [Google Scholar] [CrossRef]
- Romaszko, J.; Cymes, I.; Dragańska, E.; Kuchta, R.; Glińska-Lewczuk, K. Mortality among the homeless: Causes and meteorological relationships. PLoS ONE 2017, 12, e0189938. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tanaka, M.; Tokudome, S. Accidental hypothermia and death from cold in urban areas. Int. J. Biometeorol. 1991, 34, 242–246. [Google Scholar] [CrossRef] [PubMed]
- Harlan, S.L.; Declet-Barreto, J.H.; Stefanov, W.L.; Petitti, D.B. Neighborhood effects on heat deaths: Social and environmental predictors of vulnerability in Maricopa county, Arizona. Environ. Health Perspect. 2013, 121, 197–204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, A.J.; Goodacre, S.W.; Cross, S. Do emergency department attendances by homeless people increase in cold weather? Emerg. Med. J. 2010, 27, 526–529. [Google Scholar] [CrossRef]
- Cusack, L.; Van Loon, A.; Kralik, D.; Arbon, P.; Gilbert, S. Extreme weather-related health needs of people who are homeless. Aust. J. Prim. Health 2013, 19, 250–255. [Google Scholar] [CrossRef]
- Menne, M.J.; Durre, I.; Vose, R.S.; Gleason, B.E.; Houston, T.G. An overview of the global historical climatology network-daily database. J. Atmos. Ocean. Technol. 2012, 29, 897–910. [Google Scholar] [CrossRef]
- Donley, A.M.; Wright, J.D. Safer Outside: A Qualitative Exploration of Homeless People’s Resistance to Homeless Shelters. J. Forensic Psychol. Pr. 2012, 12, 288–306. [Google Scholar] [CrossRef]
- Ha, Y.; Narendorf, S.C.; Maria, D.S.; Bezette-Flores, N. Barriers and facilitators to shelter utilization among homeless young adults. Evaluation Program Plan. 2015, 53, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Henwood, B.; Dzubur, E.; Rhoades, H.; Clair, P.S.; Cox, R. Pet ownership in the unsheltered homeless population in Los Angeles. J. Soc. Distress Homeless 2020, 1–4. [Google Scholar] [CrossRef]
- Coolhart, D.; Brown, M.T. The need for safe spaces: Exploring the experiences of homeless LGBTQ youth in shelters. Child. Youth Serv. Rev. 2017, 82, 230–238. [Google Scholar] [CrossRef]
- De Rosa, C.J.; Montgomery, S.B.; Kipke, M.D.; Iverson, E.; Ma, J.L.; Unger, J. Service utilization among homeless and runaway youth in Los Angeles, California: Rates and reasons. J. Adolesc. Health 1999, 24, 190–200. [Google Scholar] [CrossRef]
- Larsen, L.; Poortinga, E.; Hurdle, D.E. Sleeping rough: Exploring the differences between shelter—Using and non-shelter—Using homeless individuals. Environ. Behav. 2004, 36, 578–591. [Google Scholar] [CrossRef]
- Stark, L.R. The Shelter as “Total Institution”. Am. Behav. Sci. 1994, 37, 553–562. [Google Scholar] [CrossRef]
- McMichael, C.; Barnett, J.; McMichael, A.J. An III wind? Climate change, migration, and health. Environ. Health Perspect. 2012, 120, 646–654. [Google Scholar] [CrossRef]
- McMichael, A.J.; Woodruff, R.E.; Hales, S. Climate change and human health: Present and future risks. Lancet 2006, 367, 859–869. [Google Scholar] [CrossRef]
- Tacoli, C. Crisis or adaptation? Migration and climate change in a context of high mobility. Environ. Urban. 2009, 21, 513–525. [Google Scholar] [CrossRef] [Green Version]
- Bezgrebelna, M.; McKenzie, K.; Wells, S.; Ravindran, A.; Kral, M.; Christensen, J.; Stergiopoulos, V.; Gaetz, S.; Kidd, S. Climate Change, Weather, Housing Precarity, and Homelessness: A Systematic Review of Reviews. Int. J. Environ. Res. Public Health 2021, 18, 5812. [Google Scholar] [CrossRef]
- Lee, B.A.; Shinn, M.; Culhane, D.P. Homelessness as a Moving Target. Ann. Am. Acad. Politi Soc. Sci. 2021, 693, 8–26. [Google Scholar] [CrossRef]
- Ramin, B.; Svoboda, T. Health of the homeless and climate change. J. Hered. 2009, 86, 654–664. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wasserman, S.; Faust, K. Social Network Analysis: Methods and Applications; Cambridge University Press: Cambridge, UK, 1994. [Google Scholar]
- Smith, H. Searching for kinship: The creation of street families among homeless youth. Am. Behav. Sci. 2008, 51, 756–771. [Google Scholar] [CrossRef]
- Glasser, I.; Bridgman, R. Braving the Street: The Anthropology of Homelessness, 1st ed.; Berghahn: New York, NY, USA, 1999. [Google Scholar]
- Rice, E.; Kurzban, S.; Ray, D. Homeless but connected: The role of heterogeneous social network ties and social networking technology in the mental health outcomes of street-living adolescents. Commun. Ment. Health J. 2012, 48, 692–698. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Unger, J.B.; Kipke, M.D.; Simon, T.R.; Johnson, C.J.; Montgomery, S.B.; Iverson, E. Stress, coping, and social support among homeless youth. J. Adolesc. Res. 1998, 13, 134–157. [Google Scholar] [CrossRef]
- Barman-Adhikari, A.; Rice, E.; Winetrobe, H.; Petering, R. Social network correlates of methamphetamine, heroin, and cocaine use in a sociometric network of homeless youth. J. Soc. Soc. Work. Res. 2015, 6, 433–457. [Google Scholar] [CrossRef]
- Green, H.D.; Tucker, J.S.; Golinelli, D.; Wenzel, S.L. Social networks, time homeless, and social support: A study of men on Skid Row. Netw. Sci. 2013, 1, 305–320. [Google Scholar] [CrossRef] [Green Version]
- Ennett, S.T.; Bailey, S.L.; Federman, E.B. Social network characteristics associated with risky behaviors among runaway and homeless youth. J. Health Soc. Behav. 1999, 40, 63. [Google Scholar] [CrossRef]
- Rice, E.; Milburn, N.G.; Monro, W. Social Networking Technology, Social Network Composition, and Reductions in Substance Use Among Homeless Adolescents. Prev. Sci. 2010, 12, 80–88. [Google Scholar] [CrossRef] [Green Version]
- Grigsby, C.; Baumann, N.; Gregorich, S.E.; Roberts-Gray, C. Disaffiliation to Entrenchment: A Model for Understanding Homelessness. J. Soc. Issues 1990, 46, 141–156. [Google Scholar] [CrossRef]
- Osborne, R.E. “I May be Homeless, But I’m Not Helpless”: The Costs and Benefits of Identifying with Homelessness. Self Identit 2002, 1, 43–52. [Google Scholar] [CrossRef]
- O’Malley, A.J.; Arbesman, S.; Steiger, D.M.; Fowler, J.; Christakis, N.A. Egocentric social network structure, health, and pro-social behaviors in a national panel study of Americans. PLoS ONE 2012, 7, e36250. [Google Scholar] [CrossRef] [PubMed]
- Perkins, J.M.; Subramanian, S.; Christakis, N.A. Social networks and health: A systematic review of sociocentric network studies in low- and middle-income countries. Soc. Sci. Med. 2015, 125, 60–78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salathé, M.; Jones, J. Dynamics and control of diseases in networks with community structure. PLoS Comput. Biol. 2010, 6, e1000736. [Google Scholar] [CrossRef] [Green Version]
- Smith, K.P.; Christakis, N.A. Social networks and health. Annu. Rev. Soc. 2008, 34, 405–429. [Google Scholar] [CrossRef] [Green Version]
- Almquist, Z.W. Large-scale spatial network models: An application to modeling information diffusion through the homeless population of San Francisco. Environ. Plan B Urban Anal. City Sci. 2020, 47, 523–540. [Google Scholar] [CrossRef]
- Anderson, M.-C.; Hazel, M.-A.; Perkins, J.M.; Jones, J.H.; Christakis, N.A. Investigation of a Homeless Social Identity: A Field Experiment Examining Prosocial Behavior in a Dictator Game Among People Experiencing Homelessness (Working Paper); Stanford University: Stanford, CA, USA, 2021. [Google Scholar]
- Hwang, S.W.; Kirst, M.J.; Chiu, S.; Tolomiczenko, G.; Kiss, A.; Cowan, L.; Levinson, W. Multidimensional social support and the health of homeless individuals. J. Hered. 2009, 86, 791–803. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trumbetta, S.L.; Mueser, K.T.; Quimby, E.; Bebout, R.; Teague, G.B. Social networks and clinical outcomes of dually diagnosed homeless persons. Behav. Ther. 1999, 30, 407–430. [Google Scholar] [CrossRef]
- Rowe, S.; Wolch, J. Social Networks in Time and Space: Homeless Women in Skid Row, Los Angeles. Ann. Assoc. Am. Geogr. 1990, 80, 184–204. [Google Scholar] [CrossRef]
- Reitzes, D.C.; Crimmins, T.J.; Yarbrough, J.; Parker, J. Social support and social network ties among the homeless in a downtown Atlanta park. J. Commun. Psychol. 2011, 39, 274–291. [Google Scholar] [CrossRef]
- Burt, R.S.; Meltzer, D.O.; Seid, M.; Borgert, A.; Chung, J.W.; Colletti, R.B.; Dellal, G.; A Kahn, S.; Kaplan, H.C.; Peterson, L.E.; et al. What’s in a name generator? Choosing the right name generators for social network surveys in healthcare quality and safety research. BMJ Qual. Saf. 2012, 21, 992–1000. [Google Scholar] [CrossRef]
- Luke, D.A.; Harris, J.K. Network Analysis in Public Health: History, Methods, and Applications. Annu. Rev. Public Health 2007, 28, 69–93. [Google Scholar] [CrossRef] [Green Version]
- Guest, G.; Bunce, A.; Johnson, L. Simplifying the Personal Network Name Generator: Alternatives to Traditional Multiple and Single Name Generators. Field Methods 2006, 18, 59–82. [Google Scholar] [CrossRef]
- O’Malley, A.J.; Marsden, P.V. The analysis of social networks. Health Serv. Outcomes Res. Methodol. 2008, 8, 222–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tarlov, A.R.; Ware, J.E.; Greenfield, S.; Nelson, E.C.; Perrin, E.; Zubkoff, M. The Medical Outcomes Study: An Application of Methods for Monitoring the Results of Medical Care. JAMA 1989, 262, 925–930. [Google Scholar] [CrossRef] [PubMed]
- Cherpitel, C.J. A brief screening instrument for problem drinking in the emergency room: The RAPS4. J. Stud. Alcohol 2000, 61, 447–449. [Google Scholar] [CrossRef] [PubMed]
- Skinner, H.A. The drug abuse screening test. Addict. Behav. 1982, 7, 363–371. [Google Scholar] [CrossRef]
- Chamberlain, S. Rnoaa: “NOAA” Weather Data from R; R Foundation for Statistical Computing: Indianapolis, IN, USA, 2021. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- Benenson, J.F. Gender Differences in Social Networks. J. Early Adolesc. 1990, 10, 472–495. [Google Scholar] [CrossRef]
- Harling, G.; Morris, K.A.; Manderson, L.; Perkins, J.M.; Berkman, L.F. Age and Gender Differences in Social Network Composition and Social Support among Older Rural South Africans: Findings from the HAALSI Study. J. Gerontol. Ser. B 2020, 75, 148–159. [Google Scholar] [CrossRef] [Green Version]
- McLaughlin, D.; Vagenas, D.; Pachana, N.; Begum, N.; Dobson, A. Gender differences in social network size and satisfaction in adults in their 70s. J. Health Psychol. 2010, 15, 671–679. [Google Scholar] [CrossRef] [PubMed]
- Burnham, K.P.; Anderson, D.R. Model Selection and Multimodel Inference, 2nd ed.; Springer: New York, NY, USA, 2002. [Google Scholar]
- Ross, C.E.; Wu, C. The Links Between Education and Health; American Sociological Association: New York, NY, USA, 1995; Volume 60, pp. 719–745. [Google Scholar] [CrossRef]
- Department of Housing and Urban Development. HUD 2016 Continuum of Care Homeless Assistance Programs Homeless Populations and Subpopulations; Department of Housing and Urban Development: Washington, DC, USA, 2016.
- Department of Housing and Urban Development. HUD 2017 Continuum of Care Homeless Assistance Programs Homeless Populations and Subpopulations; Department of Housing and Urban Development: Washington, DC, USA, 2017.
- Department of Housing and Urban Development. HUD 2018 Continuum of Care Homeless Assistance Programs Homeless Populations and Subpopulations; Department of Housing and Urban Development: Washington, DC, USA, 2018.
- Department of Housing and Urban Development. HUD 2019 Continuum of Care Homeless Assistance Programs Homeless Populations and Subpopulations; Department of Housing and Urban Development: Washington, DC, USA, 2019.
- Pleace, N. Exclusion by Definition: The Under-Representation of Women in European Homelessness Statistics; Women’s Homelessness in Europe; Palgrave Macmillan: London, UK, 2017; pp. 105–126. [Google Scholar] [CrossRef]
- North, C.S.; Smith, E.M. A comparison of homeless men and women: Different populations, different needs. Commun. Ment. Health J. 1993, 29, 423–431. [Google Scholar] [CrossRef]
- Lewis, J.H.; Andersen, R.M.; Gelberg, L. Health Care for Homeless Women. J. Gen. Intern. Med. 2003, 18, 921–928. [Google Scholar] [CrossRef] [Green Version]
- Cheung, A.M.; Hwang, S.W. Risk of death among homeless women: A cohort study and review of the literature. CMAJ 2004, 13, 1243. [Google Scholar] [CrossRef] [Green Version]
- Ritchey, F.J.; La Gory, M.; Mullis, J. Gender Differences in Health Risks and Physical Symptoms Among the Homeless. J. Health Soc. Behav. 1991, 32, 33. [Google Scholar] [CrossRef] [PubMed]
- Every, D.; Richardson, J.; Osborn, E. There’s nowhere to go: Counting the costs of extreme weather to the homeless community. Disasters 2019, 43, 799–817. [Google Scholar] [CrossRef]
- Aguilera, R.; Corringham, T.; Gershunov, A.; Benmarhnia, T. Wildfire smoke impacts respiratory health more than fine particles from other sources: Observational evidence from Southern California. Nat. Commun. 2021, 12, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Portmann, R.W.; Solomon, S.; Hegerl, G. Spatial and seasonal patterns in climate change, temperatures, and precipitation across the United States. Proc. Natl. Acad. Sci. USA 2009, 106, 7324–7329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Men | Women | Non-Binary | Total | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Participant Characteristics | ||||||||
| Gender | ||||||||
| Female | --- | --- | --- | --- | --- | --- | 75 | 30.4% |
| Male | --- | --- | --- | --- | --- | --- | 167 | 67.8% |
| Non-Binary | --- | --- | --- | --- | --- | --- | 4 | 1.8% |
| LGBTQI+ | ||||||||
| No | 154 | 92.2% | 67 | 89.3% | 0 | 0.0% | 221 | 89.8% |
| Yes | 13 | 7.8% | 8 | 10.7% | 4 | 100.0% | 25 | 10.2% |
| Ethnicity | ||||||||
| Non-White | 99 | 59.3% | 22 | 29.3% | 2 | 50.0% | 92 | 37.4% |
| White | 68 | 40.7% | 53 | 70.7% | 2 | 50.0% | 154 | 62.6% |
| Highest Level of Education | ||||||||
| K-11th Grade | 55 | 32.9% | 27 | 36.0% | 3 | 75.0% | 85 | 34.6% |
| GED or High School | 75 | 44.9% | 24 | 32.0% | 1 | 25.0% | 100 | 40.7% |
| Trade School or Any Higher Education | 37 | 22.2% | 24 | 32.0% | 0 | 61 | 24.7% | |
| Veteran | ||||||||
| No | 147 | 88.0% | 72 | 96.0% | 4 | 100.0% | 23 | 9.3% |
| Yes | 20 | 12.0% | 3 | 4.0% | 0 | 0.0% | 223 | 90.7% |
| Has Caseworker | ||||||||
| No | 129 | 77.2% | 56 | 74.6% | 1 | 25.0% | 186 | 76.0% |
| Yes | 37 | 22.8% | 19 | 25.4% | 3 | 75.0% | 59 | 24.0% |
| Lifetime Homelessness Duration | ||||||||
| 1 year or less | 31 | 18.6% | 19 | 25.3% | 0 | 0.0% | 50 | 20.3% |
| 1 year—5 years | 50 | 29.9% | 35 | 46.7% | 0 | 0.0% | 85 | 34.6% |
| 5 years—10 years | 48 | 28.7% | 12 | 16.0% | 1 | 25.0% | 61 | 24.8% |
| 10 years + | 38 | 22.8% | 9 | 12.0% | 3 | 75.0% | 50 | 20.3% |
| Sleeps in Encampment with Other PEH | ||||||||
| No | 106 | 63.4% | 40 | 53.3% | 2 | 50.0% | 148 | 60.2% |
| Yes | 59 | 36.6% | 35 | 46.7% | 2 | 50.0% | 96 | 39.8% |
| Interview Season | ||||||||
| Summer | 37 | 22.2% | 15 | 20.0% | 2 | 50.0% | 54 | 22.0% |
| Fall | 46 | 27.5% | 25 | 33.3% | 1 | 25.0% | 72 | 29.2% |
| Winter | 47 | 28.1% | 22 | 29.3% | 1 | 25.0% | 70 | 28.5% |
| Spring | 37 | 22.2% | 13 | 17.4% | 0 | 0.0% | 50 | 20.3% |
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Age (Years) | 46.6 | 10.2 | 41.4 | 9.1 | 39.8 | 16.4 | 44.9 | 10.3 |
| Number of Nights Spent Inside During Past Week | 1.6 | 2.2 | 1.5 | 2.2 | 0.8 | 1.5 | 1.5 | 2.2 |
| HUD Point-in-Time Count | ||||||
|---|---|---|---|---|---|---|
| Study Data n = 242 | 2016 n = 672 | 2017 n = 639 | 2018 n = 613 | 2019 n = 583 | 2020 n = 584 | |
| Gender | ||||||
| Male | 167 | 549 * | 458 | 470 * | 462 * | 448 * |
| Female | 75 | 123 * | 181 | 143 * | 121 * | 136 * |
| HUD Point-in-Time Count | ||||||
| Study Data n = 246 | 2016 n = 673 | 2017 n = 639 | 2018 n = 616 | 2019 n = 585 | 2020 n = 584 | |
| Ethnicity | ||||||
| White | 154 | 434 | 419 | 403 | 379 | 371 |
| Non-white | 92 | 239 | 220 | 213 | 206 | 213 |
| Daily Max. Temp. (°C) | Daily Min. Temp. (°C) | Daily Precipitation (mm) | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| Season | ||||||
| Summer | 30.4 | 4.1 | 20.8 | 2.1 | 50.9 | 81.8 |
| Fall | 16.7 | 5.8 | 4.8 | 5.6 | 45.4 | 97.6 |
| Winter | 12.9 | 7.9 | 1.0 | 5.5 | 70.1 | 140.0 |
| Spring | 26.0 | 5.2 | 12.6 | 6.2 | 7.6 | 32.8 |
| Men n = 167 | Women n = 74 | Non-Binary n = 4 | Total n = 245 | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Network Size | 4.8 | 2.7 | 5.3 | 2.7 | 4.8 | 2.4 | 5.0 | 2.7 |
| Number of Family in Network | 1.9 | 1.8 | 2.3 | 2.1 | 1.5 | 1.3 | 2.0 | 1.9 |
| Number of Friends in Network | 2.5 | 1.9 | 2.7 | 1.9 | 2.8 | 2.2 | 2.6 | 1.9 |
| Number of Emotional Supports in Network | 4.0 | 2.6 | 4.5 | 2.8 | 4.8 | 2.4 | 4.2 | 2.6 |
| Number of Material Supports in Network | 4.0 | 2.6 | 4.5 | 2.6 | 4.3 | 2.5 | 4.2 | 2.6 |
| Number of Financial Supports in Network | 3.3 | 2.6 | 3.7 | 2.3 | 2.8 | 3.5 | 3.4 | 2.5 |
| Number of Network Members with Whom Participant Uses Alcohol | 1.7 | 2.1 | 1.1 | 1.5 | 1.8 | 2.9 | 1.6 | 2.0 |
| Number of Network Members with Whom Participant Uses Drugs | 0.9 | 1.5 | 0.7 | 1.0 | 1.5 | 2.4 | 0.9 | 1.4 |
| Number of Trusted Network Members | 4.3 | 2.6 | 4.4 | 2.8 | 4.5 | 1.9 | 4.3 | 2.6 |
| Number of Network Members Who Upset Participant in Past 30 Days | 0.9 | 1.3 | 1.4 | 1.4 | 2.0 | 3.4 | 1.1 | 1.4 |
| Number of Housed Network Members | 3.2 | 2.3 | 3.0 | 2.3 | 2.5 | 1.3 | 3.1 | 2.3 |
| Number of Unhoused Network Members | 1.6 | 1.7 | 2.1 | 1.6 | 2.0 | 2.8 | 1.7 | 1.7 |
| Health Condition | n | % Prevalence |
|---|---|---|
| Diabetes | 24 | 9.8% |
| Anemia | 35 | 14.2% |
| Cancer | 17 | 6.9% |
| High blood pressure | 84 | 34.1% |
| Heart problems | 31 | 12.6% |
| Stroke (has experienced) | 19 | 7.7% |
| Lung problems | 50 | 20.3% |
| Asthma | 76 | 30.9% |
| Liver problems | 24 | 9.8% |
| Epilepsy | 42 | 17.1% |
| Mobility problems | 72 | 29.3% |
| Osteoporosis | 4 | 1.6% |
| Kidney problems | 19 | 7.7% |
| Dental problems | 110 | 44.7% |
| Eye problems (excluding vision) | 21 | 8.5% |
| Disability | 14 | 5.7% |
| Hepatitis | 37 | 15.0% |
| HIV | 5 | 2.1% |
| Mental health diagnosis | 145 | 59.9% |
| Men | Women | Non-Binary | Total | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Substance Use | ||||||||
| Alcohol Abuse | ||||||||
| No | 89 | 53.4% | 47 | 62.7% | 0 | 0.0% | 136 | 55.3% |
| Yes | 78 | 46.6% | 28 | 37.3% | 4 | 100.0% | 110 | 44.7% |
| Drug Abuse | ||||||||
| No | 90 | 53.9% | 45 | 60.0% | 2 | 50.0% | 137 | 55.7% |
| Yes | 77 | 46.1% | 30 | 40.0% | 2 | 50.0% | 109 | 44.3% |
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| β | 95% CI | β | 95% CI | β | 95% CI | β | 95% CI | |
| Biophysical Environment | ||||||||
| Season | ||||||||
| Summer | 57.4 *** | (50.1, 64.8) | 42.8 *** | (32.6, 53.0) | 49.5 *** | (40.1, 58.9) | 70.1 *** | (61.5, 78.6) |
| Fall | 53.5 *** | (47.2, 50.9) | 40.1 *** | (31.1, 49.1) | 44.8 *** | (36.4, 53.2) | 67.1 *** | (59.0, 75.2) |
| Winter | 44.4 *** | (37.9, 50.9) | 31.5 *** | (22.6, 40.4) | 33.3 *** | (24.3, 42.3) | 59.3 *** | (50.4, 68.3) |
| Spring | 53.3 *** | (45.7, 60.8) | 38.5 *** | (28.2, 48.8) | 41.1 *** | (30.9, 51.3) | 60.1 *** | (51.1, 69.1) |
| Sociodemographic Factors | ||||||||
| Gender | ||||||||
| Female (reference) | --- | --- | --- | --- | --- | --- | --- | |
| Male | --- | --- | 13.5 *** | (6.2, 20.8) | 12.6 *** | (5.4, 19.8) | 8.6 ** | (2.6, 14.6) |
| Education | ||||||||
| K-11th Grade (reference) | --- | --- | --- | --- | --- | --- | --- | |
| GED or HS Diploma | --- | --- | 6.2 | (−1.6, 14.1) | --- | --- | --- | --- |
| Any Higher Education | --- | --- | 7.7 | (−1.2, 16.5) | --- | --- | --- | --- |
| Exposure | ||||||||
| Number of nights spent inside during past 7 days | --- | --- | --- | --- | 2.3 ** | (0.8, 3.8) | 1.8 ** | (0.5, 3.1) |
| Social Network Factors | ||||||||
| Number of social network members causing upset to participant in past 30 days | --- | --- | --- | --- | −2.1 | (−4.6, 0.4) | --- | --- |
| Chronic Health Conditions | ||||||||
| Number of chronic health conditions (excluding mental health diagnosis) | --- | --- | --- | --- | --- | --- | −6.2 *** | (−7.4, −5.0) |
| Adjusted | 0.79 | 0.80 | 0.81 | 0.87 | ||||
| Model 5 | Model 6 | Model 7 | Model 8 | |||||
|---|---|---|---|---|---|---|---|---|
| β | 95% CI | β | 95% CI | β | 95% CI | β | 95% CI | |
| Sociodemographic Factors | ||||||||
| Gender | ||||||||
| Female | 59.0 *** | (53.7, 64.4) | 56.2 *** | (49.0, 63.4) | 78.4 *** | (70.8, 86.0) | 75.8 *** | (68.9, 82.9) |
| Male | 65.9 *** | (62.4, 69.5) | 61.6 *** | (55.8, 67.4) | 81.3 *** | (75.7, 87.0) | 79.4 *** | (74.4, 84.5) |
| Social Network Factors | ||||||||
| Number of perceived financial supports | --- | --- | 1.6 | (−0.1, 3.4) | --- | --- | --- | --- |
| Number of trusted social network members | --- | --- | 1.1 | (−0.9, 3.0) | --- | --- | --- | --- |
| Number of social network members who upset participant in past 30 days | --- | --- | −5.3 *** | (−7.6, −3.0) | −2.4 * | (−4.7, −0.3) | −2.3 * | (−4.4, −0.1) |
| Number of housed network members | --- | --- | −0.3 | (−2.3, 1.8) | --- | --- | --- | --- |
| Health Conditions | ||||||||
| Alcohol abuse | ||||||||
| No (reference) | --- | --- | --- | --- | --- | --- | --- | --- |
| Yes | --- | --- | --- | --- | −9.3 ** | (−5.2, 6.5) | −10.1 *** | (−15.8, −4.4) |
| Drug abuse | ||||||||
| No (reference) | --- | --- | --- | --- | --- | --- | --- | --- |
| Yes | --- | --- | --- | --- | 0.7 | (−5.2, 6.5) | --- | --- |
| Chronic Health Conditions | ||||||||
| Number of Chronic Health Conditions (Excluding Mental Health Diagnosis) | --- | --- | --- | --- | −1.1 | (−2.5, 0.2) | --- | --- |
| Mental Health Diagnosis | ||||||||
| No (reference) | --- | --- | --- | --- | --- | --- | --- | --- |
| Yes | --- | --- | --- | --- | −10.8 ** | (−17.2, −4.4) | −13.2 *** | (−18.9, −7.4) |
| Adjusted | 0.88 | 0.89 | 0.90 | 0.90 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anderson, M.-C.; Hazel, A.; Perkins, J.M.; Almquist, Z.W. The Ecology of Unsheltered Homelessness: Environmental and Social-Network Predictors of Well-Being among an Unsheltered Homeless Population. Int. J. Environ. Res. Public Health 2021, 18, 7328. https://doi.org/10.3390/ijerph18147328
Anderson M-C, Hazel A, Perkins JM, Almquist ZW. The Ecology of Unsheltered Homelessness: Environmental and Social-Network Predictors of Well-Being among an Unsheltered Homeless Population. International Journal of Environmental Research and Public Health. 2021; 18(14):7328. https://doi.org/10.3390/ijerph18147328
Chicago/Turabian StyleAnderson, Mary-Catherine, Ashley Hazel, Jessica M. Perkins, and Zack W. Almquist. 2021. "The Ecology of Unsheltered Homelessness: Environmental and Social-Network Predictors of Well-Being among an Unsheltered Homeless Population" International Journal of Environmental Research and Public Health 18, no. 14: 7328. https://doi.org/10.3390/ijerph18147328
APA StyleAnderson, M.-C., Hazel, A., Perkins, J. M., & Almquist, Z. W. (2021). The Ecology of Unsheltered Homelessness: Environmental and Social-Network Predictors of Well-Being among an Unsheltered Homeless Population. International Journal of Environmental Research and Public Health, 18(14), 7328. https://doi.org/10.3390/ijerph18147328






