Diagnosis of Fetal Alcohol Spectrum Disorders (FASDs): Guidelines of Interdisciplinary Group of Polish Professionals
Abstract
:1. Introduction
2. Materials and Methods
2.1. Work on the FASD Diagnostic Recommendations Included Several Steps
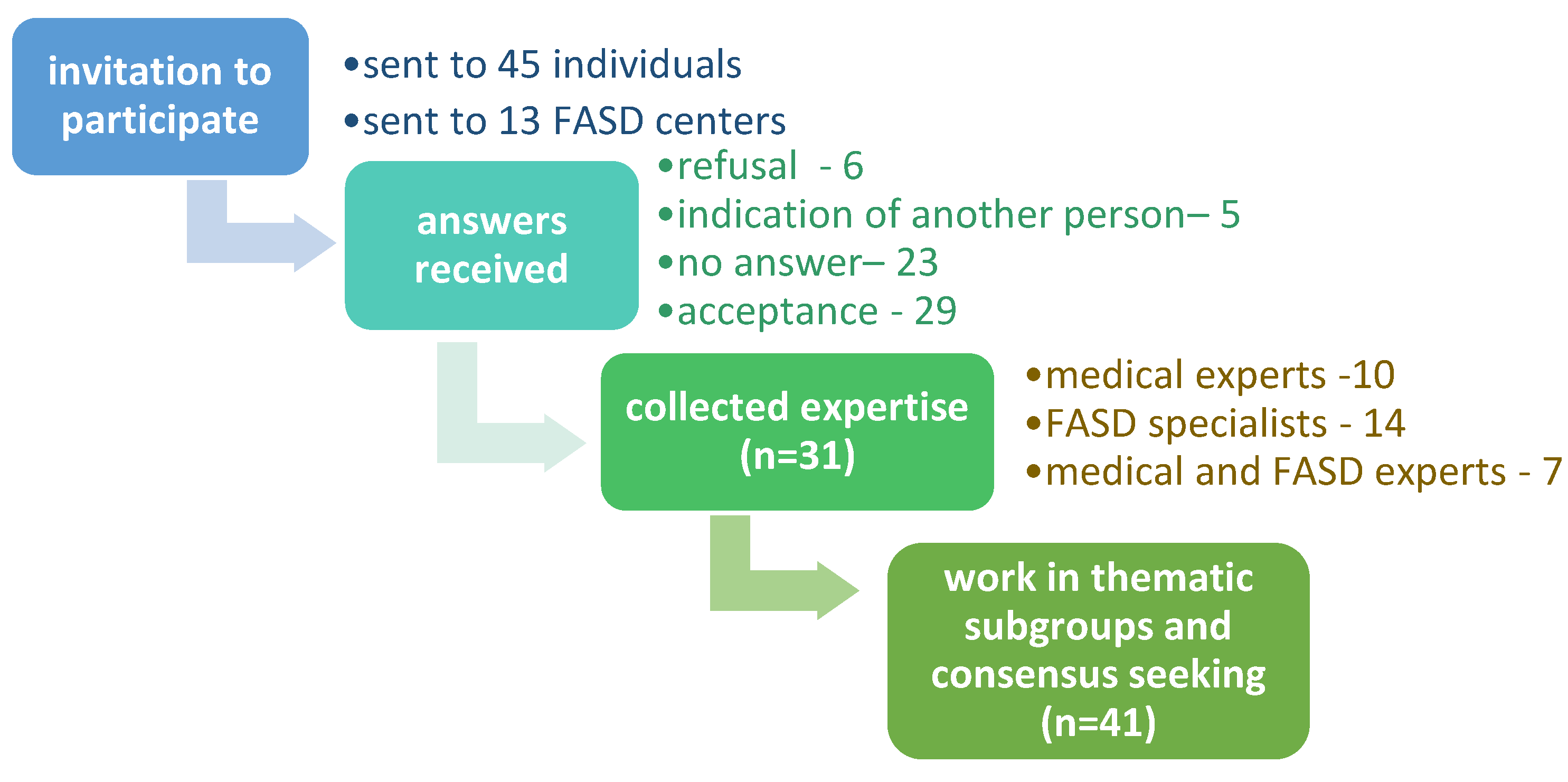
2.1.1. Step 1. Formation of a Team of Professionals
2.1.2. Step 2. Gathering the Opinions of Professionals on the Three (U.S./Canadian) FASD Diagnostic Systems
- scope and purpose of the recommendation,
- scope of consultation,
- methodological rigor of developing recommendations,
- clarity of presentation,
- utility,
- authors’ independence, and
- overall assessment.
- featured categories/units under the FASD term,
- diagnostic procedure,
- assessment of prenatal exposure to alcohol,
- assessment of neurodevelopmental disorders,
- assessment of key facial dysmorphias,
- assessment of height/weight, and
- formulating the diagnosis and the action plan.
- clarity of presentation,
- methodological rigor in developing recommendations,
- utility in Poland, and
- overall assessment.
2.1.3. Step 3. Four Rounds of Consultation and Work in Subgroups
- Group 1—recommendations for neurodevelopmental assessment,
- Group 2—recommendations regarding prenatal exposure to alcohol,
- Group 3—recommendations for the diagnostic procedure, and
- Group 4—recommendations for the assessment of growth and dysmorphia.
2.1.4. Step 4. Adoption of the Recommendation
3. Results
3.1. Evaluation of U.S./Canadian FASD Diagnostic Guidelines
- Dysmorphology and growth assessment are not very controversial. The key task is to select growth charts to be used in Poland, as at present, the practice in this area significantly differs across specialists and diagnostic centers.
- The research evidence on the usefulness of various methods to assess prenatal alcohol exposure among Polish women of childbearing age and during pregnancy is missing.
- In-depth understanding of biological mechanisms and factors determining structural and functional development of the central nervous system is needed to develop standards of neurodevelopmental assessment.
- The neurodevelopmental assessment is probably the most challenging element of FASD diagnosis. However, the general consensus was achieved that the scope of assessment has to be broad—covering all cognitive, emotional, and social functions, acknowledging environmental factors (family, school).
- In the area of neurodevelopmental assessment, further discussion is needed to determine:
- ■
- selection of psychological and neuropsychological tools (the first list of validated tests will be elaborated by the work group soon),
- ■
- selection of the cutoff point (1.5 or 2 SD) for test results,
- ■
- interpretation of the general IQ scores,
- ■
- whether other neurodevelopmental disorders should be recognized in a patient with FASD or whether an individual cognitive profile should be prepared, and
- ■
- inter-sectoral cooperation of mental health specialists (between education and healthcare systems) and educational judicature (How psychologists working out of the healthcare system should be involved in FASD diagnosis?).
- In Poland, a three-stage diagnostic algorithm (including basic screening in primary healthcare, social-care, and educational units; proper assessment by the interdisciplinary team; consultations with a highly specialized medical center for genetic, neuroimaging, and neurometabolic assessment) might be useful.
3.2. Polish Guidelines for Diagnosing Fetal Alcohol Spectrum Disorders
- distinguished diagnostic categories,
- diagnostic procedure,
- assessment of prenatal exposure to alcohol,
- assessment of sentinel facial dysmorphias,
- assessment of body weight, height, and head circumference, and
- neurodevelopmental assessment.
3.2.1. Distinguished Diagnostic Categories
- FAS (Q86.0 in the ICD-10 classification)
- ND–PAE (neurodevelopmental disorder associated with prenatal alcohol exposure)—although ND-PAE is not recognized in the ICD-10 classification, it is recommended to register this as G96.8: Other specified disorders of the central nervous system.
3.2.2. Diagnostic Procedure
- FASD is in general underdiagnosed especially among individuals staying in biological families.
- The doctor has very little time for the patient (the regulations set by the National Health Fund limit consultations to 20 min, including the time devoted to administrative duties).
- The diagnosis once entered into the patient’s file is rarely verified by consecutive doctors. Most often, the consecutive consultants of the patient prescribe the previous diagnoses and add their own.
- The current system of financing outpatient specialist care by the National Health Fund does not create the possibility of organizing multispecialist consultations and referring the patient to other specialists, radically extends the process of diagnosis (queues to specialists). Multispecialist consultations are most often offered by private or public centers thanks to the funds from other sources—e.g., municipal budgets.
- (1)
- Screening—to enhance early identification of risk and referrals to the proper diagnosis of FASD.
- (2)
- Proper diagnosis—to check whether a person meets the FAS or ND–PAE diagnostic criteria, or whether he/she should be classified as at risk of FASD; to formulate functional diagnosis; and to indicate the necessary tests to complement the differential diagnosis.
- (3)
- Differential and functional diagnosis—to rule out causes of neurodevelopmental disorders other than prenatal exposure to alcohol, and thereby ultimately confirm a diagnosis of FAS or ND–PAE. It may also exclude a patient from the FASD risk group.
- (4)
- Formulation of conclusions and recommendations and their presentation to a patient and/or family/caregivers.
- In obstetrics and pediatric clinics—based on an interview with the mother or other data indicating alcohol consumption during pregnancy.
- In obstetrics and neonatal departments—based on the observation of neurological disorders or congenital abnormalities in the newborn, including dysmorphia.
- By pediatricians or nurses, in various healthcare facilities—based on the observation of any neurodevelopmental abnormalities or growth restriction or dysmorphia in the child (Tools supporting professionals in observing feeding problems in a child under 2 years of age and approximate assessment of the functions of the nervous system for non-physicians in order to make a decision about referring a child over 2 years of age to a neurologist are included, as appendixes, in the Polish recommendations).
- according to what criteria the diagnosis was made;
- findings of the diagnostic team in the scope of the performed tests (assessments);
- recommendations for further steps, including follow-up visits (it must be adjusted to the actual needs identified as a result of the functional diagnosis and the real possibilities of providing them to the patient and their family); and
- in the case of children at risk of FASD—information about the need to contact the diagnostic team at a specific time for the reassessment as well as information on the areas of the child’s functioning that should be observed by parents/caregivers in the meantime.
3.2.3. Assessment of Prenatal Exposure to Alcohol
- ≥8 standard alcohol doses per week for ≥2 weeks of pregnancy or
- ≥2 heavy drinking episodes (having on one occasion ≥4 doses of alcohol).
- (1)
- Direct interview—reliable information can only be obtained from the mother herself if an interviewer is in good contact with her and creates an atmosphere of security and trust. Therefore, it is recommended to
- introduce questions about drinking alcohol to a broader medical interview (an example of such an interview is provided in the attachments);
- avoid closed questions, i.e., those to which the patient only answers YES or NO;
- asking about the period of 3 months before pregnancy (or learning about pregnancy) may be a better predictor of drinking alcohol during pregnancy than a direct question about drinking alcohol during pregnancy [34].
- (2)
- Indirect interview—based on information from other people who have contact with the mother during pregnancy.
- It should be remembered that the persons providing the information should be reliable, and there should be no conflict of interest between them and the mother.
- Indirect information (e.g., about a woman’s lifestyle in general or the use of alcohol in other pregnancies) by itself cannot be taken as a significant indicator of PAE.
- (3)
- Medical, judicial, or employee records as well from broadly understood social welfare
- documented social or legal problems related to drinking alcohol during pregnancy (e.g., driving under the influence of alcohol); and
- documented alcohol intoxication during pregnancy (study alcohol content in blood, exhaled air, urine).
3.2.4. Assessment of Sentinel Facial Dysmorphias
3.2.5. Anthropometry
Growth Impairment
Occipitofrontal Circumference (OFC) Evaluation
3.2.6. Neurodevelopmental Assessment
- cognitive functions (gnosis, praxis, attention, language and communication, visual-spatial functions, memory and learning, executive functions, graphomotor skills, general intelligence);
- emotional and social functioning (adequacy and compassion of emotions, mentalization ability, theory of mind, understanding and observance of social norms, implementation of developmental tasks, relationships with peers);
- adaptive difficulties (physiological processes: sleep, eating, symptoms of the autonomic nervous system, self-regulation processes, sensory sensitivity); and
- psychopathological symptoms (anxiety, behavioral disorders, personality development disorders).
- The presence of deficits in at least three cognitive areas. In the case of neurological symptoms—deficits in two areas.
- The occurrence of abnormalities in at least three areas from the emotional and social sphere, adaptation disorders, or psychopathological symptoms.
- Significant impact of the identified deficits and symptoms on everyday life activities and school functioning (in the case of people who have completed their education, the data from the interview are to be taken into account).
- at 4 years of age;
- about 6–7 years of age (in Poland, this is the age of starting school education);
- around 11–12 years of age; and
- around 18 years of age.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Statement
References
- Popova, S.; Lange, S.; Probst, C.; Gmel, G.; Rehm, J. Estimation of National, Regional, and Global Prevalence of Alcohol Use during Pregnancy and Fetal Alcohol Syndrome: A Systematic Review and Meta-Analysis. Lancet Glob. Health 2017, 5, e290–e299. [Google Scholar] [CrossRef] [Green Version]
- Roozen, S.; Peters, G.-J.Y.; Kok, G.; Townend, D.; Nijhuis, J.; Curfs, L. Worldwide Prevalence of Fetal Alcohol Spectrum Disorders: A Systematic Literature Review Including Meta-Analysis. Alcohol. Clin. Exp. Res. 2016, 40, 18–32. [Google Scholar] [CrossRef]
- Okulicz-Kozaryn, K.; Borkowska, M.; Brzózka, K. FASD Prevalence among Schoolchildren in Poland. J. Appl. Res. Intellect. Disabil. 2017, 30, 61–70. [Google Scholar] [CrossRef] [Green Version]
- Popova, S.; Lange, S.; Shield, K.; Mihic, A.; Chudley, A.E.; Mukherjee, R.A.S.; Bekmuradov, D.; Rehm, J. Comorbidity of Fetal Alcohol Spectrum Disorder: A Systematic Review and Meta-Analysis. Lancet 2016, 387, 978–987. [Google Scholar] [CrossRef]
- Hoyme, H.E.; May, P.A.; Kalberg, W.O.; Kodituwakku, P.; Gossage, J.P.; Trujillo, P.M.; Buckley, D.G.; Miller, J.H.; Aragon, A.S.; Khaole, N.; et al. A Practical Clinical Approach to Diagnosis of Fetal Alcohol Spectrum Disorders: Clarification of the 1996 Institute of Medicine Criteria. Pediatrics 2005, 115, 39–47. [Google Scholar] [CrossRef] [Green Version]
- Hoyme, H.E.; Kalberg, W.O.; Elliott, A.J.; Blankenship, J.; Buckley, D.; Marais, A.-S.; Manning, M.A.; Robinson, L.K.; Adam, M.P.; Abdul-Rahman, O.; et al. Updated Clinical Guidelines for Diagnosing Fetal Alcohol Spectrum Disorders. Pediatrics 2016, 138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cook, J.L.; Green, C.R.; Lilley, C.M.; Anderson, S.M.; Baldwin, M.E.; Chudley, A.E.; Conry, J.L.; LeBlanc, N.; Loock, C.A.; Lutke, J.; et al. Fetal Alcohol Spectrum Disorder: A Guideline for Diagnosis across the Lifespan. CMAJ 2016, 188, 191–197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Astley, S.J. Validation of the Fetal Alcohol Spectrum Disorder (FASD) 4-Digit Diagnostic Code. J. Popul. Ther. Clin. Pharmacol. 2013, 20, e416–e467. [Google Scholar] [PubMed]
- Landgraf, M.N.; Nothacker, M.; Heinen, F. Diagnosis of Fetal Alcohol Syndrome (FAS): German Guideline Version 2013. Eur. J. Paediatr. Neurol. 2013, 17, 437–446. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Watkins, R.E.; Elliott, E.J.; Wilkins, A.; Mutch, R.C.; Fitzpatrick, J.P.; Payne, J.M.; O’Leary, C.M.; Jones, H.M.; Latimer, J.; Hayes, L.; et al. Recommendations from a Consensus Development Workshop on the Diagnosis of Fetal Alcohol Spectrum Disorders in Australia. BMC Pediatr. 2013, 13, 156. [Google Scholar] [CrossRef] [Green Version]
- Coles, C.D.; Gailey, A.R.; Mulle, J.G.; Kable, J.A.; Lynch, M.E.; Jones, K.L. A Comparison Among 5 Methods for the Clinical Diagnosis of Fetal Alcohol Spectrum Disorders. Alcohol. Clin. Exp. Res. 2016, 40, 1000–1009. [Google Scholar] [CrossRef]
- Okulicz-Kozaryn, K.; Terlikowska, J.; Brzózka, K.; Borkowska, M. Prevention and Intervention for FASD in Poland. J. Pediatr. Neuropsychol. 2017, 3, 79–92. [Google Scholar] [CrossRef]
- Brown, J.M.; Bland, R.; Jonsson, E.; Greenshaw, A.J. The Standardization of Diagnostic Criteria for Fetal Alcohol Spectrum Disorder (FASD): Implications for Research, Clinical Practice and Population Health. Can. J. Psychiatry 2019, 64, 169–176. [Google Scholar] [CrossRef] [Green Version]
- Brouwers, M.C.; Kho, M.E.; Browman, G.P.; Burgers, J.S.; Cluzeau, F.; Feder, G.; Fervers, B.; Graham, I.D.; Grimshaw, J.; Hanna, S.E.; et al. AGREE II: Advancing Guideline Development, Reporting and Evaluation in Health Care. CMAJ 2010, 182, E839–E842. [Google Scholar] [CrossRef] [Green Version]
- Okulicz-Kozaryn, K.; Szymańska, K.; Maryniak, A.; Dyląg, K.; Śmigiel, R.; Helwich, E.; Domin, A.; Borkowska, M. Rozpoznawanie Spektrum Płodowych Zaburzeń Alkoholowych. 2020. Available online: https://www.ciazabezalkoholu.pl/images/Rozpoznawanie_FASD_Pediatria_2020_FASD.pdf (accessed on 20 May 2021).
- Stratton, K.R.; Howe, C.J.; Battaglia, F.C. (Eds.) Fetal Alcohol Syndrome: Diagnosis, Epidemiology, Prevention, and Treatment; National Academy Press: Washington, DC, USA, 1999. [Google Scholar]
- Sampson, P.D.; Streissguth, A.P.; Bookstein, F.L.; Barr, H.M. On Categorizations in Analyses of Alcohol Teratogenesis. Environ. Health Perspect. 2000, 108 (Suppl. 3), 421–428. [Google Scholar] [CrossRef]
- Wozniak, D.F.; Hartman, R.E.; Boyle, M.P.; Vogt, S.K.; Brooks, A.R.; Tenkova, T.; Young, C.; Olney, J.W.; Muglia, L.J. Apoptotic Neurodegeneration Induced by Ethanol in Neonatal Mice Is Associated with Profound Learning/Memory Deficits in Juveniles Followed by Progressive Functional Recovery in Adults. Neurobiol. Dis. 2004, 17, 403–414. [Google Scholar] [CrossRef]
- Memo, L.; Gnoato, E.; Caminiti, S.; Pichini, S.; Tarani, L. Fetal Alcohol Spectrum Disorders and Fetal Alcohol Syndrome: The State of the Art and New Diagnostic Tools. Early Hum. Dev. 2013. [Google Scholar] [CrossRef]
- Perkins, A.; Lehmann, C.; Lawrence, R.C.; Kelly, S.J. Alcohol Exposure during Development: Impact on the Epigenome. Int. J. Dev. Neurosci. 2013, 31, 391–397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Warzycha, J.; Baryła, M.; Halkiewicz, M.; Warzycha, E.; Rakowska, M. Wpływ Alkoholu Na Rozwój Dziecka—Współczesne Poglądy. Post. Neonatol. 2013, 2, 64–68. [Google Scholar]
- Messina, M.P.; D’Angelo, A.; Battagliese, G.; Coriale, G.; Tarani, L.; Pichini, S.; Rasio, D.; Parlapiano, G.; Fiore, M.; Petrella, C.; et al. Fetal Alcohol Spectrum Disorders Awareness in Health Professionals: Implications for Psychiatry. Riv. Psichiatr. 2020, 55, 79–89. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, J.L.; Jacobson, S.W.; Sokol, R.J.; Martier, S.S.; Ager, J.W.; Kaplan-Estrin, M.G. Teratogenic Effects of Alcohol on Infant Development. Alcohol. Clin. Exp. Res. 1993, 17, 174–183. [Google Scholar] [CrossRef]
- O’Leary, C.M.; Nassar, N.; Zubrick, S.R.; Kurinczuk, J.J.; Stanley, F.; Bower, C. Evidence of a Complex Association between Dose, Pattern and Timing of Prenatal Alcohol Exposure and Child Behaviour Problems. Addiction 2010, 105, 74–86. [Google Scholar] [CrossRef]
- Patra, J.; Bakker, R.; Irving, H.; Jaddoe, V.W.V.; Malini, S.; Rehm, J. Dose-Response Relationship between Alcohol Consumption before and during Pregnancy and the Risks of Low Birthweight, Preterm Birth and Small for Gestational Age (SGA)-a Systematic Review and Meta-Analyses. BJOG Int. J. Obstet. Gynaecol. 2011, 118, 1411–1421. [Google Scholar] [CrossRef] [PubMed]
- Larkby, C.A.; Goldschmidt, L.; Hanusa, B.H.; Day, N.L. Prenatal Alcohol Exposure Is Associated with Conduct Disorder in Adolescence: Findings from a Birth Cohort. J. Am. Acad. Child Adolesc. Psychiatry 2011, 50, 262–271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sawada Feldman, H.; Lyons Jones, K.; Lindsay, S.; Slymen, D.; Klonoff-Cohen, H.; Kao, K.; Rao, S.; Chambers, C. Prenatal Alcohol Exposure Patterns and Alcohol-Related Birth Defects and Growth Deficiencies: A Prospective Study. Alcohol. Clin. Exp. Res. 2012, 36, 670–676. [Google Scholar] [CrossRef] [PubMed]
- May, P.A.; Blankenship, J.; Marais, A.S.; Gossage, J.P.; Kalberg, W.O.; Joubert, B.; Cloete, M.; Barnard, R.; De Vries, M.; Hasken, J.; et al. Maternal Alcohol Consumption Producing Fetal Alcohol Spectrum Disorders (FASD): Quantity, Frequency, and Timing of Drinking. Drug Alcohol Depend. 2013, 133, 502–512. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flak, A.L.; Su, S.; Bertrand, J.; Denny, C.H.; Kesmodel, U.S.; Cogswell, M.E. The Association of Mild, Moderate, and Binge Prenatal Alcohol Exposure and Child Neuropsychological Outcomes: A Meta-Analysis. Alcohol. Clin. Exp. Res. 2014, 38, 214–226. [Google Scholar] [CrossRef]
- May, P.A.; Gossage, J.P. Maternal Risk Factors for Fetal Alcohol Spectrum Disorders: Not as Simple as It Might Seem. Alcohol Res. Health 2011, 34, 15–26. [Google Scholar]
- Bradley, K.A.; Debenedetti, A.F.; Volk, R.J.; Williams, E.C.; Frank, D.; Kivlahan, D.R. AUDIT-C as a Brief Screen for Alcohol Misuse in Primary Care. Alcohol. Clin. Exp. Res. 2007, 31, 1208–1217. [Google Scholar] [CrossRef] [PubMed]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; De la Fuente, J.R.; Grant, M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption-II. Addiction 1993, 88, 791–804. [Google Scholar] [CrossRef]
- Klimkiewicz, A.; Jakubczyk, A.; Mach, A.; Abramowska, M.; Szczypiński, J.; Berndt, D.; Skrzeszewski, J.; Witkowski, G.; Wojnar, M. Adaptacja i Walidacja Testu Rozpoznawania Zaburzeń Związanych z Używaniem Alkoholu (AUDIT) w Warunkach Polskich PARPA Raport; Warszawa, Poland, 2020; unpublished report; Available online: https://www.parpa.pl/images/Adaptacja_i_walidacja_testu_AUDIT_do_warunk%C3%B3w_polskich.pdf (accessed on 12 May 2021).
- Symon, A.; Rankin, J.; Sinclair, H.; Butcher, G.; Barclay, K.; Gordon, R.; MacDonald, M.; Smith, L. Peri-Conceptual and Mid-Pregnancy Drinking: A Cross-Sectional Assessment in Two Scottish Health Board Areas Using a 7-Day Retrospective Diary. J. Adv. Nurs. 2017, 73, 375–385. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, K.; Smith, D. Recognition of the Fetal Alcohol Syndrome in Early Infancy. Lancet 1973, 302, 999–1001. [Google Scholar] [CrossRef]
- Lemoine, P.; Harouseau, H.; Borteryu, J.; Menuet, J. Les Enfants Des Parents Alcooliques. Anomalies Observées à Propos de 127 Cas. Quest Med. 1968. [Google Scholar] [CrossRef]
- Astley, S.J.; Clarren, S.K. Measuring the Facial Phenotype of Individuals with Prenatal Alcohol Exposure: Correlations with Brain Dysfunction. Alcohol Alcohol. 2001, 36, 147–159. [Google Scholar] [CrossRef] [Green Version]
- Cranston, M.E.; Mhanni, A.A.; Marles, S.L.; Chudley, A.E. Concordance of Three Methods for Palpebral Fissure Length Measurement in the Assessment of Fetal Alcohol Spectrum Disorder. Can. J. Clin. Pharmacol. 2009, 16, e234–e241. [Google Scholar]
- Astley, S.J. Canadian Palpebral Fissure Length Growth Charts Reflect a Good Fit for Two School and FASD Clinic-Based U.S. Populations. J. Popul. Ther. Clin. Pharmacol. = J. Ther. Popul. Pharmacol. Clin. 2011, 18, e231–e241. [Google Scholar]
- Astley, S.J. Palpebral Fissure Length Measurement: Accuracy of the FAS Facial Photographic Analysis Software and Inaccuracy of the Ruler. J. Popul. Ther. Clin. Pharmacol. 2015, 22, e9–e26. [Google Scholar]
- Strömland, K.; Chen, Y.; Norberg, T.; Wennerström, K.; Michael, G. Reference Values of Facial Features in Scandinavian Children Measured with a Range-Camera Technique. Scand. J. Plast. Reconstr. Surg. Hand Surg. 1999, 33, 59–65. [Google Scholar] [CrossRef]
- Del Campo, M.; Jones, K.L. A Review of the Physical Features of the Fetal Alcohol Spectrum Disorders. Eur. J. Med. Genet. 2017, 60, 55–64. [Google Scholar] [CrossRef]
- Jones, K.; Smith, D.; Ulleland, C.; Streissguth, A. Pattern of Malformation in Offspring of Chronic Alcoholic Mothers. Lancet 1973, 301, 1267–1271. [Google Scholar] [CrossRef]
- Kuehn, D.; Aros, S.; Cassorla, F.; Avaria, M.; Unanue, N.; Henriquez, C.; Kleinsteuber, K.; Conca, B.; Avila, A.; Carter, T.C.; et al. A Prospective Cohort Study of the Prevalence of Growth, Facial, and Central Nervous System Abnormalities in Children with Heavy Prenatal Alcohol Exposure. Alcohol. Clin. Exp. Res. 2012, 36, 1811–1819. [Google Scholar] [CrossRef] [Green Version]
- Carter, R.C.; Jacobson, J.L.; Molteno, C.D.; Jiang, H.; Meintjes, E.M.; Jacobson, S.W.; Duggan, C. Effects of Heavy Prenatal Alcohol Exposure and Iron Deficiency Anemia on Child Growth and Body Composition through Age 9 Years. Alcohol. Clin. Exp. Res. 2012, 36, 1973–1982. [Google Scholar] [CrossRef] [Green Version]
- Carter, R.C.; Jacobson, J.L.; Sokol, R.J.; Avison, M.J.; Jacobson, S.W. Fetal Alcohol-Related Growth Restriction from Birth through Young Adulthood and Moderating Effects of Maternal Prepregnancy Weight. Alcohol. Clin. Exp. Res. 2013, 37, 452–462. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lumeng, J.C.; Cabral, H.J.; Gannon, K.; Heeren, T.; Frank, D.A. Pre-Natal Exposures to Cocaine and Alcohol and Physical Growth Patterns to Age 8 Years. Neurotoxicol. Teratol. 2007, 29, 446–457. [Google Scholar] [CrossRef] [Green Version]
- Day, N.L.; Leech, S.L.; Richardson, G.A.; Cornelius, M.D.; Robles, N.; Larkby, C. Prenatal Alcohol Exposure Predicts Continued Deficits in Offspring Size at 14 Years of Age. Alcohol. Clin. Exp. Res. 2002, 26, 1584–1591. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, C.M.; Nassar, N.; Kurinczuk, J.J.; Bower, C. The Effect of Maternal Alcohol Consumption on Fetal Growth and Preterm Birth. BJOG Int. J. Obstet. Gynaecol. 2009, 116, 390–400. [Google Scholar] [CrossRef]
- Astley, S.J.; Bledsoe, J.M.; Davies, J.K. The Essential Role of Growth Deficiency in the Diagnosis of Fetal Alcohol Spectrum Disorder. Adv. Pediatr. Res. 2016, 3. [Google Scholar] [CrossRef]
- Battaglia, F.C.; Lubchenco, L.O. A Practical Classification of Newborn Infants by Weight and Gestational Age. J. Pediatr. 1967, 71, 159–163. [Google Scholar] [CrossRef]
- WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards Based on Length/Height, Weight and Age. Acta Paediatr. Suppl. 2006, 450, 76–85. [Google Scholar]
- Fenton, T.R.; Kim, J.H. A Systematic Review and Meta-Analysis to Revise the Fenton Growth Chart for Preterm Infants. BMC Pediatr. 2013, 13, 59. [Google Scholar] [CrossRef] [Green Version]
- Jones, K.L.; Hoyme, H.E.; Robinson, L.K.; del Campo, M.; Manning, M.A.; Bakhireva, L.N.; Prewitt, L.M.; Chambers, C.D. Developmental Pathogenesis of Short Palpebral Fissure Length in Children with Fetal Alcohol Syndrome. Birth Defects Res. Part A Clin. Mol. Teratol. 2009, 85, 695–699. [Google Scholar] [CrossRef] [Green Version]
- Treit, S.; Zhou, D.; Chudley, A.E.; Andrew, G.; Rasmussen, C.; Nikkel, S.M.; Samdup, D.; Hanlon-Dearman, A.; Loock, C.; Beaulieu, C. Relationships between Head Circumference, Brain Volume and Cognition in Children with Prenatal Alcohol Exposure. PLoS ONE 2016, 11, e0150370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- NHANES Anthropometry Procedures Manual. Available online: https://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_an.pdf (accessed on 12 May 2021).
- Palczewska, I.; Niedzwiedzka, Z. Somatic Development Indices in Children and Youth of Warsaw. Med. Wieku Rozwoj. 2001, 5, 18–118. [Google Scholar] [PubMed]
- Fuglestad, A.J.; Whitley, M.L.; Carlson, S.M.; Boys, C.J.; Eckerle, J.K.; Fink, B.A.; Wozniak, J.R. Executive Functioning Deficits in Preschool Children with Fetal Alcohol Spectrum Disorders. Child Neuropsychol. 2015, 21, 716–731. [Google Scholar] [CrossRef] [Green Version]
- Ase, F.; Ilona, A.R.; Mirjam, K.; Pekka, S.; Eugene, H.H.; Sarah, M.N.; Marit, K. Adaptive Behaviour in Children and Adolescents with Foetal Alcohol Spectrum Disorders: A Comparison with Specific Learning Disability and Typical Development. Eur. Child Adolesc. Psychiatry 2012, 21, 221–231. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vaurio, L.; Riley, E.P.; Mattson, S.N. Neuropsychological Comparison of Children with Heavy Prenatal Alcohol Exposure and an IQ-Matched Comparison Group. J. Int. Neuropsychol. Soc. 2011, 17, 463–473. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mattson, S.N.; Roesch, S.C.; Glass, L.; Deweese, B.N.; Coles, C.D.; Kable, J.A.; May, P.A.; Kalberg, W.O.; Sowell, E.R.; Adnams, C.M.; et al. Further Development of a Neurobehavioral Profile of Fetal Alcohol Spectrum Disorders. Alcohol. Clin. Exp. Res. 2013, 37, 517–528. [Google Scholar] [CrossRef] [Green Version]
- American Academy of Pediatrics. 2016 Coding for Fetal Alcohol Spectrum Disorder. Available online: https://www.aap.org/en-us/professional-resources/practice-transformation/getting-paid/Coding-at-%0Athe-AAP/Pages/Fetal-Alcohol-Syndrome.aspx (accessed on 12 May 2021).
- Bager, H.; Christensen, L.P.; Husby, S.; Bjerregaard, L. Biomarkers for the Detection of Prenatal Alcohol Exposure: A Review. Alcohol. Clin. Exp. Res. 2017, 41, 251–261. [Google Scholar] [CrossRef]
- Chabenne, A.; Moon, C.; Ojo, C.; Khogali, A.; Nepal, B.; Sharma, S. Biomarkers in Fetal Alcohol Syndrome. Biomark. Genom. Med. 2014, 6, 12–22. [Google Scholar] [CrossRef] [Green Version]
- Chiandetti, A.; Hernandez, G.; Mercadal-Hally, M.; Alvarez, A.; Andreu-Fernandez, V.; Navarro-Tapia, E.; Bastons-Compta, A.; Garcia-Algar, O. Prevalence of Prenatal Exposure to Substances of Abuse: Questionnaire versus Biomarkers. Reprod. Health 2017. [Google Scholar] [CrossRef]
- Gomez-Roig, M.D.; Marchei, E.; Sabra, S.; Busardò, F.P.; Mastrobattista, L.; Pichini, S.; Gratacós, E.; Garcia-Algar, O. Maternal Hair Testing to Disclose Self-Misreporting in Drinking and Smoking Behavior during Pregnancy. Alcohol 2018, 67, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Kodituwakku, P.; Kodituwakku, E. Cognitive and Behavioral Profiles of Children with Fetal Alcohol Spectrum Disorders. Curr. Dev. Disord. Rep. 2014, 1, 149–160. [Google Scholar] [CrossRef] [Green Version]
- Mattson, S.N.; Bernes, G.A.; Doyle, L.R. Fetal Alcohol Spectrum Disorders: A Review of the Neurobehavioral Deficits Associated With Prenatal Alcohol Exposure. Alcohol. Clin. Exp. Res. 2019, 43, 1046–1062. [Google Scholar] [CrossRef] [PubMed]



| The Recommendation Is Precise—Clearly Indicates How to Differentiate between Various Sub-Categories of FASD | |||||
|---|---|---|---|---|---|
| 1 I Definitely Do Not Agree | 2 I Rather Do Not Agree | 3 It Is Hard to Say | 4 I Rather Agree | 5 I Definitely Agree | |
| IOM guidelines | |||||
| Canadian guidelines | |||||
| 4-Digit Code | |||||
| Substantiation/Comments | |||||
| FASD | At Risk of FASD—Non-Diagnostic Category | ||
|---|---|---|---|
| FAS | ND–PAE | ||
| Prenatal alcohol exposure | Yes or unknown | Yes | Yes or, in the presence of 3 sentinel facial features, unknown |
| Pre- and/orpostnatal growth deficits | Yes | N/A | To be observed |
| Sentinel facial features |
| N/A | To be observed |
| Neurodevelopmental disorders |
| To be observed | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okulicz-Kozaryn, K.; Maryniak, A.; Borkowska, M.; Śmigiel, R.; Dylag, K.A. Diagnosis of Fetal Alcohol Spectrum Disorders (FASDs): Guidelines of Interdisciplinary Group of Polish Professionals. Int. J. Environ. Res. Public Health 2021, 18, 7526. https://doi.org/10.3390/ijerph18147526
Okulicz-Kozaryn K, Maryniak A, Borkowska M, Śmigiel R, Dylag KA. Diagnosis of Fetal Alcohol Spectrum Disorders (FASDs): Guidelines of Interdisciplinary Group of Polish Professionals. International Journal of Environmental Research and Public Health. 2021; 18(14):7526. https://doi.org/10.3390/ijerph18147526
Chicago/Turabian StyleOkulicz-Kozaryn, Katarzyna, Agnieszka Maryniak, Magdalena Borkowska, Robert Śmigiel, and Katarzyna Anna Dylag. 2021. "Diagnosis of Fetal Alcohol Spectrum Disorders (FASDs): Guidelines of Interdisciplinary Group of Polish Professionals" International Journal of Environmental Research and Public Health 18, no. 14: 7526. https://doi.org/10.3390/ijerph18147526
APA StyleOkulicz-Kozaryn, K., Maryniak, A., Borkowska, M., Śmigiel, R., & Dylag, K. A. (2021). Diagnosis of Fetal Alcohol Spectrum Disorders (FASDs): Guidelines of Interdisciplinary Group of Polish Professionals. International Journal of Environmental Research and Public Health, 18(14), 7526. https://doi.org/10.3390/ijerph18147526






