Motivation, Usability, and Credibility of an Intelligent Activity-Based Client-Centred Training System to Improve Functional Performance in Neurological Rehabilitation: An Exploratory Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Protocol
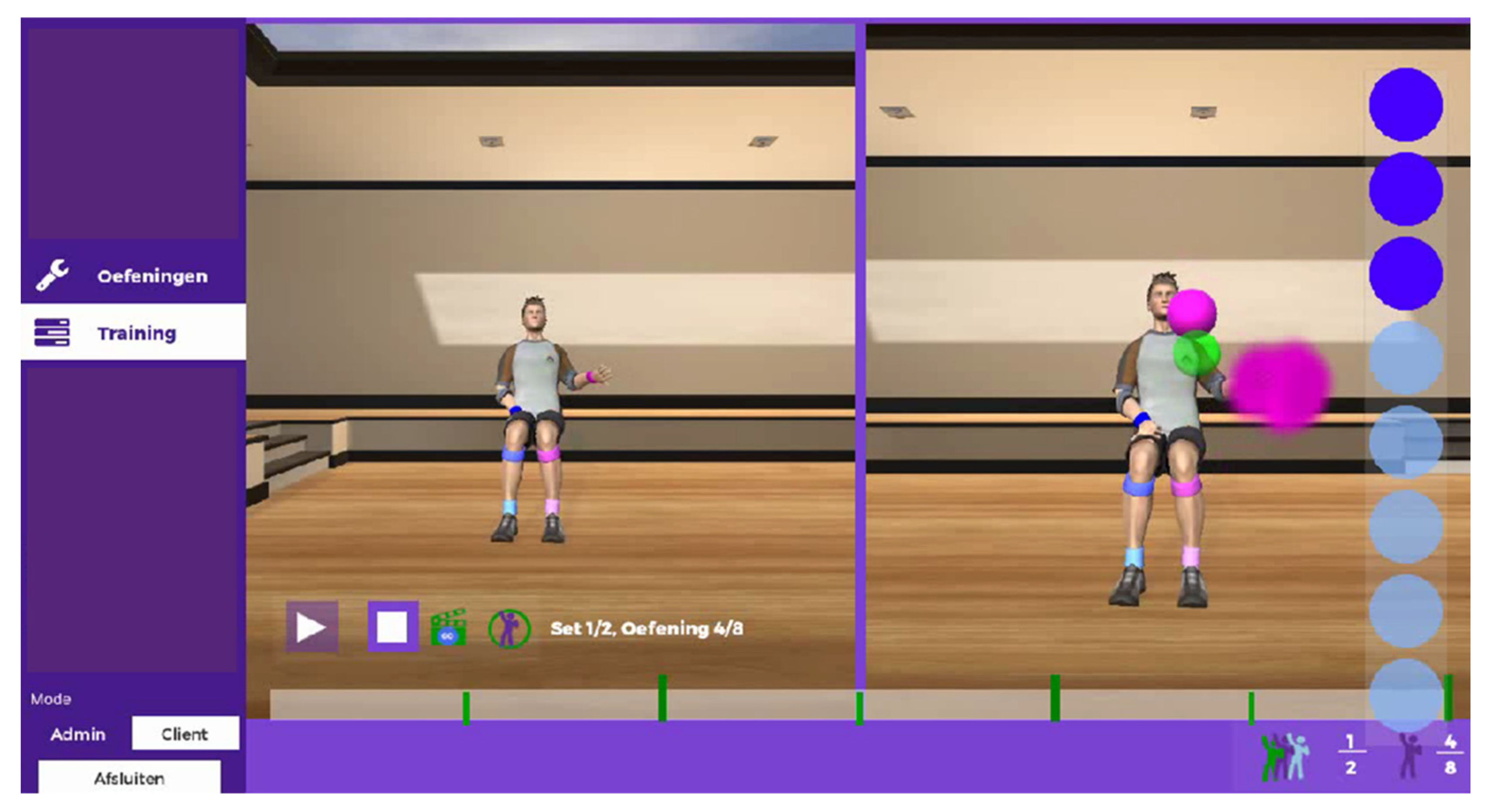
2.3. Apparatus
2.4. Outcome Measures
2.5. Ethics Statement
2.6. Statistical Analysis
3. Results
3.1. Quantitative Results
3.2. Qualitative results
“I learned other stuff than in my regular therapy… I really believe that this in combination with my normal therapies, helped me regain arm functionality”(Patient with stroke)
“Technology is the future, but we are still needed. Patients still want a human standing beside them who tells them what is good and what is wrong, or give them tips and tricks”(occupational therapist)
“If I’m honest, I secretly liked it (i.e., i-ACT training)”(Person with MS)
“Patients tell a lot about their training with i-ACT. They all like doing it, just because it’s something different, something new”(occupational therapist)
“You have to do your exercises really well, otherwise you get a red dot. If you do your therapy exercises at home, you never know whether you do them correctly or not”(person with stroke)
“It looks like the little guy is shivering most of the time. It distracts me sometimes”(person with spinal cord injury)
“After the first workshop, I thought it would be easy. But after that I did not have enough time to get myself acquainted with i-ACT, let alone practice with a patient, and then you forget about certain steps. (…) We need a very intuitive system or more time for training with the system with a professional”(occupational therapist)
“At least one therapist who works here, should become a specialist in using the i-ACT, then he or she can motivate the colleagues, provide assistance when needed and give workshops every now and then.”(occupational therapist)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Users | Observers | |
|---|---|---|
| Introduction question | What are the shortcomings of the i-ACT? What are the positive aspects of i-ACT? | Why did you not actively use the i-ACT? |
| Transition question | How could we improve the i-ACT in the future? | What changes are needed for you to actively use i-ACT? |
| Main question 1 | Would you use i-ACT in your rehabilitation? Why (not)? | Would you use i-ACT if the patient asks to use it? Why (not)? |
| Main question 2 | In how far do you believe i-ACT is effective for you/your patient? | Would you use i-ACT if there is an educational program (e.g., workshop, training)? Why (not)? |
| Final question | Would you recommend i-ACT for use in neurological rehabilitation? Why (not)? | |
References
- Domínguez-Téllez, P.; Moral-Muñoz, J.A.; Salazar, A.; Casado-Fernández, E.; Lucena-Anton, D. Game-Based Virtual Reality Interventions to Improve Upper Limb Motor Function and Quality of Life After Stroke: Systematic Review and Meta-analysis. Games Health J. 2020, 9, 1–10. [Google Scholar] [CrossRef] [PubMed]
- De Heredia-Torres, M.P.; Huertas-Hoyas, E.; Sánchez-Camarero, C.; Máximo-Bocanegra, N.; Alegre-Ayala, J.; Sánchez-Herrera-Baeza, P.; Martínez-Piédrola, R.M.; García-Bravo, C.; Mayoral-Martín, A.; Serrada-Tejeda, S. Occupational performance in multiple sclerosis and its relationship with quality of life and fatigue. Eur. J. Phys. Rehabil. Med. 2020, 56, 148–154. [Google Scholar] [CrossRef]
- De Araújo, A.V.L.; Neiva, J.F.D.O.; Monteiro, C.B.D.M.; Magalhães, F.H. Efficacy of Virtual Reality Rehabilitation after Spinal Cord Injury: A Systematic Review. BioMed Res. Int. 2019, 2019. [Google Scholar] [CrossRef] [PubMed]
- Kwakkel, G.; van Peppen, R.; Wagenaar, R.C.; Wood Dauphinee, S.; Richards, C.; Ashburn, A.; Miller, K.; Lincoln, N.; Partridge, C.; Wellwood, I.; et al. Effects of augmented exercise therapy time after stroke: A meta-analysis. Stroke 2004, 35, 2529–2539. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rietberg, M.B.; Brooks, D.; Uitdehaag, B.M.; Kwakkel, G. Exercise therapy for multiple sclerosis. Cochrane Database Syst. Rev. 2005, 2005, CD003980. [Google Scholar] [CrossRef]
- Smidt, N.; de Vet, H.C.; Bouter, L.M.; Dekker, J.; Arendzen, J.H.; de Bie, R.A.; Bierma-Zeinstra, S.M.; Helders, P.J.; Keus, S.H.; Kwakkel, G.; et al. Effectiveness of exercise therapy: A best-evidence summary of systematic reviews. Aust. J. Physiother. 2005, 51, 71–85. [Google Scholar] [CrossRef] [Green Version]
- Van Peppen, R.; Kwakkel, G.; Wood-Dauphinee, S.; Hendriks, H.; Van der Wees, P.; Dekker, J. The impact of physical therapy on functional outcomes after stroke: What’s the evidence? Clin. Rehabil. 2004, 18, 833–862. [Google Scholar] [CrossRef]
- Timmermans, A.; Spooren, A.I.F.; Kingma, H.H.; Seelen, H.A.M. Influence of Task-Oriented Training Content on Skilled Arm-Hand Performance in Stroke: A Systematic Review. Neurorehabilit. Neural Repair 2010, 24, 858–870. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spooren, A.I.; Timmermans, A.; Seelen, H.A. Motor training programs of arm and hand in patients with MS according to different levels of the ICF: A systematic review. BMC Neurol. 2012, 12, 49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spooren, A.I.F.; Janssen-Potten, Y.J.M.; Kerckhofs, E.; Bongers, H.M.H.; Seelen, H.A.M. Evaluation of a task-oriented client-centered upper extremity skilled performance training module in persons with tetraplegia. Spinal Cord 2011, 49, 1049–1054. [Google Scholar] [CrossRef] [Green Version]
- Veerbeek, J.M.; van Wegen, E.; van Peppen, R.; van der Wees, P.J.; Hendriks, E.; Rietberg, M.; Kwakkel, G. What is the evidence for physical therapy poststroke? A systematic review and meta-analysis. PLoS ONE 2014, 9, e87987. [Google Scholar] [CrossRef] [Green Version]
- Saposnik, G.; Levin, M. Virtual reality in stroke rehabilitation a meta-analysis and implications for clinicians. Stroke 2011, 42, 1380–1386. [Google Scholar] [CrossRef]
- Timmermans, A.A.; Lemmens, R.J.; Monfrance, M.; Geers, R.P.; Bakx, W.; Smeets, R.J.; Seelen, H.A. Effects of task-oriented robot training on arm function, activity, and quality of life in chronic stroke patients: A randomized controlled trial. J. Neuroeng. Rehabil. 2014, 11, 45. [Google Scholar] [CrossRef] [Green Version]
- Prange, G.B.; Jannink, M.J.; Groothuis-Oudshoorn, C.G.; Hermens, H.J.; Ijzerman, M.J. Systematic review of the effect of robot-aided therapy on recovery of the hemiparetic arm after stroke. J. Rehabil. Res. Dev. 2006, 43, 171–184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feys, P.; Coninx, K.; Kerkhofs, L.; De Weyer, T.; Truyens, V.; Maris, A.; Lamers, I. Robot-supported upper limb training in a virtual learning environment: A pilot randomized controlled trial in persons with MS. J. Neuroeng. Rehabil. 2015, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fasoli, S.E.; Krebs, H.I.; Hogan, N. Robotic Technology and Stroke Rehabilitation: Translating Research into Practice. Top. Stroke Rehabil. 2004, 11, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Mehrholz, J.; Pollock, A.; Pohl, M.; Kugler, J.; Elsner, B. Systematic review with network meta-analysis of randomized controlled trials of robotic-assisted arm training for improving activities of daily living and upper limb function after stroke. J. Neuroeng. Rehabil. 2020, 17, 83. [Google Scholar] [CrossRef] [PubMed]
- Veerbeek, J.M.; Langbroek-Amersfoort, A.C.; van Wegen, E.E.; Meskers, C.G.; Kwakkel, G. Effects of Robot-Assisted Therapy for the Upper Limb After Stroke. Neurorehabilit. Neural Repair 2017, 31, 107–121. [Google Scholar] [CrossRef] [PubMed]
- Vanmulken, D.A.; Spooren, A.I.; Bongers, H.M.; Seelen, H.A. Robot-assisted task-oriented upper extremity skill training in cervical spinal cord injury: A feasibility study. Spinal Cord 2015, 53, 547–551. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mubin, O.; Alnajjar, F.; Jishtu, N.; Alsinglawi, B.; Al Mahmud, A. Exoskeletons With Virtual Reality, Augmented Reality, and Gamification for Stroke Patients’ Rehabilitation: Systematic Review. JMIR Rehabil. Assist. Technol. 2019, 6, e12010. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Knippenberg, E.; Verbrugghe, J.; Lamers, I.; Palmaers, S.; Timmermans, A.; Spooren, A. Markerless motion capture systems as training device in neurological rehabilitation: A systematic review of their use, application, target population and efficacy. J. Neuroeng. Rehabil. 2017, 14, 61. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Lo, W.L.; Mao, Y.R.; Ding, M.H.; Lin, Q.; Li, H.; Zhao, J.L.; Xu, Z.Q.; Bian, R.H.; Huang, D.F. Effect of Virtual Reality on Postural and Balance Control in Patients with Stroke: A Systematic Literature Review. BioMed Res. Int. 2016, 2016, 7309272. [Google Scholar] [CrossRef] [PubMed]
- Sin, H.; Lee, G. Additional virtual reality training using Xbox Kinect in stroke survivors with hemiplegia. Am. J. Phys. Med. Rehabil. 2013, 92, 871–880. [Google Scholar] [CrossRef] [PubMed]
- Paquin, K.; Crawley, J.; Harris, J.E.; Horton, S. Survivors of chronic stroke—Participant evaluations of commercial gaming for rehabilitation. Disabil. Rehabil. 2016, 38, 2144–2152. [Google Scholar] [CrossRef]
- Gamito, P.; Oliveira, J.; Coelho, C.; Morais, D.; Lopes, P.; Pacheco, J.; Brito, R.; Soares, F.; Santos, N.; Barata, A.F. Cognitive training on stroke patients via virtual reality-based serious games. Disabil. Rehabil. 2017, 39, 385–388. [Google Scholar] [CrossRef]
- Webster, D.; Celik, O. Systematic review of Kinect applications in elderly care and stroke rehabilitation. J. Neuroeng. Rehabil. 2014, 11, 108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lozano-Quilis, J.A.; Gil-Gomez, H.; Gil-Gomez, J.A.; Albiol-Perez, S.; Palacios-Navarro, G.; Fardoun, H.M.; Mashat, A.S. Virtual rehabilitation for multiple sclerosis using a kinect-based system: Randomized controlled trial. JMIR Serious Games 2014, 2, e12. [Google Scholar] [CrossRef]
- Knippenberg, E.; Spooren, A. Opportunities of markerless motion detection systems for use in neurological rehabilitation: A qualitative study on patient and therapist perspective. Austin J. Robot. Autom. 2016, 3, 1–5. [Google Scholar]
- Jager, J.; Putnick, D.; Bornstein, M.H., II. MORE THAN JUST CONVENIENT: THE SCIENTIFIC MERITS OF HOMOGENEOUS CONVENIENCE SAMPLES. Monogr. Soc. Res. Child Dev. 2017, 82, 13–30. [Google Scholar] [CrossRef] [Green Version]
- Knippenberg, E.; Van Hout, L.; Smeets, W.; Palmaers, S.; Timmermans, A.; Spooren, A. Developing an intelligent activity-based client-centred training system with a user-centred approach. Technol. Health Care 2019, 28, 1–14. [Google Scholar] [CrossRef]
- Deci, E.L.; Eghrari, H.; Patrick, B.C.; Leone, D.R. Facilitating internalization: The self-determination theory perspective. J. Personal. 1994, 62, 119–142. [Google Scholar] [CrossRef] [PubMed]
- Ryan, R.M.; Mims, V.; Koestner, R. Relation of reward contingency and interpersonal context to intrinsic motivation: A review and test using cognitive evaluation theory. J. Personal. Soc. Psychol. 1983, 45, 736. [Google Scholar] [CrossRef]
- Tsigilis, N.; Theodosiou, A. Temporal stability of the intrinsic motivation inventory. Percept. Mot. Ski. 2003, 97, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Bangor, A.; Kortum, P.T.; Miller, J.T. An empirical evaluation of the system usability scale. Int. J. Hum. Comput. Interact. 2008, 24, 574–594. [Google Scholar] [CrossRef]
- Lewis, J.R.; Sauro, J. The factor structure of the system usability scale. In Proceedings of the International Conference on Human Centered Design, San Diego, CA, USA, 19–24 July 2009; pp. 94–103. [Google Scholar]
- Borkovec, T.D.; Nau, S.D. Credibility of analogue therapy rationales. J. Behav. Ther. Exp. Psychiatry 1972, 3, 257–260. [Google Scholar] [CrossRef]
- Devilly, G.J.; Borkovec, T.D. Psychometric properties of the credibility/expectancy questionnaire. J. Behav. Ther. Exp. Psychiatry 2000, 31, 73–86. [Google Scholar] [CrossRef]
- Bodiam, C. The use of the Canadian Occupational Performance Measure for the assessment of outcome on a neurorehabilitation unit. Br. J. Occup. Ther. 1999, 62, 123–126. [Google Scholar] [CrossRef]
- Wressle, E.; Eeg-Olofsson, A.M.; Marcusson, J.; Henriksson, C. Improved client participation in the rehabilitation process using a client-centred goal formulation structure. J. Rehabil. Med. 2002, 34, 5–11. [Google Scholar] [CrossRef] [Green Version]
- Lamers, I.; Kelchtermans, S.; Baert, I.; Feys, P. Upper limb assessment in multiple sclerosis: A systematic review of outcome measures and their psychometric properties. Arch. Phys. Med. Rehabil. 2014, 95. [Google Scholar] [CrossRef]
- Wolf, S.L.; Catlin, P.A.; Ellis, M.; Archer, A.L.; Morgan, B.; Piacentino, A. Assessing Wolf motor function test as outcome measure for research in patients after stroke. Stroke 2001, 32, 1635–1639. [Google Scholar] [CrossRef] [Green Version]
- Finley, J.M.; Gotsis, M.; Lympouridis, V.; Jain, S.; Kim, A.; Fisher, B.E. Design and Development of a Virtual Reality-Based Mobility Training Game for People With Parkinson’s Disease. Front. Neurol. 2021, 11, 577713. [Google Scholar] [CrossRef] [PubMed]
- Bangor, A.; Kortum, P.; Miller, J. Determining what individual SUS scores mean: Adding an adjective rating scale. J. Usability Stud. 2009, 4, 114–123. [Google Scholar]
- Carswell, A.; McColl, M.A.; Baptiste, S.; Law, M.; Polatajko, H.; Pollock, N. The Canadian Occupational Performance Measure: A Research and Clinical Literature Review. Can. J. Occup. Ther. 2004, 71, 210–222. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.C.; Lee, T. Validity of the Canadian occupational performance measure. Occup. Ther. Int. 1997, 4, 231–249. [Google Scholar] [CrossRef]
- Phipps, S.; Richardson, P. Occupational therapy outcomes for clients with traumatic brain injury and stroke using the Canadian Occupational Performance Measure. Am. J. Occup. Ther. 2007, 61, 328–334. [Google Scholar] [CrossRef] [Green Version]
- Chen, C.C.; Bode, R.K. Psychometric validation of the Manual Ability Measure-36 (MAM-36) in patients with neurologic and musculoskeletal disorders. Arch. Phys. Med. Rehabil. 2010, 91, 414–420. [Google Scholar] [CrossRef] [PubMed]
- Kos, D.; Kerckhofs, E.; Carrea, I.; Verza, R.; Ramos, M.; Jansa, J. Evaluation of the Modified Fatigue Impact Scale in four different European countries. Mult. Scler. J. 2005, 11, 76–80. [Google Scholar] [CrossRef]
- Kos, D.; Kerckhofs, E.; Nagels, G.; D’Hooghe, B.D.; Duquet, W.; Duportail, M.; Ketelaer, P. Assessing fatigue in multiple sclerosis: Dutch modified fatigue impact scale. Acta Neurol. Belg. 2003, 103, 185–191. [Google Scholar] [PubMed]
- Verheyden, G.; Hughes, J.; Jelsma, J.; Nieuwboer, A.; De Weerdt, W. Assesing motor impairment of the trunk in patients with traumatic brain injury: Reliability and validity of the trunk impairment scale. S. Afr. J. Physiother. 2006, 62, 23–27. [Google Scholar] [CrossRef] [Green Version]
- Verheyden, G.; Nieuwboer, A.; Mertin, J.; Preger, R.; Kiekens, C.; De Weerdt, W. The Trunk Impairment Scale: A new tool to measure motor impairment of the trunk after stroke. Clin. Rehabil. 2004, 18, 326–334. [Google Scholar] [CrossRef]
- Laver, K.E.; Lange, B.; George, S.; Deutsch, J.E.; Saposnik, G.; Crotty, M. Virtual reality for stroke rehabilitation. Cochrane Database Syst. Rev. 2017, 11. [Google Scholar] [CrossRef] [Green Version]
- Lloréns, R.; Noé, E.; Colomer, C.; Alcañiz, M. Effectiveness, Usability, and Cost-Benefit of a Virtual Reality–Based Telerehabilitation Program for Balance Recovery After Stroke: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2015, 96, 418–425.e412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levin, M.F.; Snir, O.; Liebermann, D.G.; Weingarden, H.; Weiss, P.L. Virtual Reality Versus Conventional Treatment of Reaching Ability in Chronic Stroke: Clinical Feasibility Study. Neurol. Ther. 2012, 1, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duff, M.; Chen, Y.; Cheng, L.; Liu, S.-M.; Blake, P.; Wolf, S.L.; Rikakis, T. Adaptive Mixed Reality Rehabilitation Improves Quality of Reaching Movements More Than Traditional Reaching Therapy Following Stroke. Neurorehabilit. Neural Repair 2013, 27, 306–315. [Google Scholar] [CrossRef]
- Stinear, C.M.; Lang, C.E.; Zeiler, S.; Byblow, W.D. Advances and challenges in stroke rehabilitation. Lancet Neurol. 2020, 19, 348–360. [Google Scholar] [CrossRef]

| T0 | T1 | T2 | T3 | T4 | |||
|---|---|---|---|---|---|---|---|
| T0a | T0b | T0c | |||||
| −2 Weeks | −1 Week | Week 0 | Week 2 | Week 4 | Week 6 | Week 15 | |
| Primary outcome measures | COPM | COPM | COPM | ||||
| IMI 1 | IMI | IMI | IMI | IMI | |||
| SUS 1 | SUS | SUS | SUS | SUS | |||
| CEQ 1 | CEQ | CEQ | CEQ | CEQ | |||
| WMFT | WMFT | WMFT | WMFT | WMFT | WMFT | WMFT | |
| Secondary outcome measures | MAM-36 | MAM-36 | MAM-36 | MAM-36 | MAM-36 | MAM-36 | MAM-36 |
| TIS | TIS | TIS | TIS | TIS | TIS | TIS | |
| MFIS | MFIS | MFIS | MFIS | MFIS | MFIS | MFIS | |
| AROM | AROM | AROM | AROM | AROM | AROM | AROM | |
| Patients | Therapists | |
|---|---|---|
| N | 17 | 8 |
| Age (years) 1 Gender (male/female) Diagnosis (time (months) since diagnosis) 1 Stroke Multiple sclerosis Spinal cord injury Craniocerebral trauma Parsonage Turner syndrome | 57.2 ± 16.3 13/4 11 (5.00 ± 2.14) 2 (289.00 ± 151.32) 1 (5.00) 2 (16.00 ± 9.90) 1 (3.00) | 35.6 ± 4.7 0/8 |
| Baseline | Training Period | Follow-Up | Within Group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T0 | T1 | T2 | T3 | T4 | Over Time * | T0–T3 £ | Effect Size | T0–T4£ | Effect Size | T3–T4 £ | Effect Size | |
| n = 17 | n = 17 | n = 17 | n = 13 | n = 14 | T0–T4 | T0–T3 | T0–T4 | T3–T4 | ||||
| IMI (range 1–7) | ||||||||||||
| Interest/enjoyment | 6.00 (5.07–6.64) | 5.86 (4.43–6.50) | 6.00 (5.15–6.50) | 6.00 (5.22–6.29) | 5.93 (5.54–6.50) | p = 0.413 | p = 0.875 | p = 0.506 | p = 0.400 | |||
| Perceived competence | 5.17 (3.75–5.83) | 5.33 (4.33–5.67) | 5.67 (4.84–6.00) | 5.83 (4.59–6.17) | 5.67 (5.13–6.04) | p = 0.025 | p = 0.017 | r = 0.434 | p = 0.035 | r = 0.378 | p = 0.789 | |
| Effort | 6.00 (5.50–6.70) | 6.00 (5.40–6.40) | 6.00 (5.40–6.70) | 6.20 (5.20–6.70) | 6.4 (5.70–7.00) | p = 0.543 | p = 0.345 | p = 0.806 | p = 0.232 | |||
| Felt pressure/tension | 2.00 (1.10–3.50) | 2.20 (1.50–2.80) | 1.80 (1.20–2.80) | 2.00 (1.10–2.30) | 2.20 (1.35–2.85) | p = 0.682 | p = 0.142 | p = 0.325 | p = 0.422 | |||
| Value/usefulness | 6.00 (5.15–6.64) | 6.00 (5.22–6.57) | 6.29 (5.72–6.71) | 6.00 (4.86–6.79) | 6.36 (5.36–6.78) | p = 0.086 | p = 0.484 | p = 0.099 | p = 0.247 | |||
| Relatedness | 5.80 (5.10–6.20) | 5.80 (4.90–6.80) | 6.00 (5.80–6.60) | 6.00 (5.30–6.60) | 5.70 (5.20–7.00) | p = 0.884 | p = 0.972 | p = 0.504 | p = 0.944 | |||
| SUS (range 0–100) | 77.50 (71.25–85.00) | 77.50 (61.25–81.25) | 75.00 (58.75–86.25) | 75.00 (63.75–90.00) | 73.75 (64.38–92.50) | p = 0.174 | p = 0.562 | p = 0.975 | p = 0.858 | |||
| CEQ (range 0–27) | ||||||||||||
| Credibility | 22.00 (18.00–25.00) | 23.00 (17.00–25.00) | 23.00 (18.00–25.50) | 23.00 (16.00–24.50) | 24.00 (20.25–25.00) | p = 0.176 | p = 0.655 | p = 0.302 | p = 0.020 | r = 0.447 | ||
| Expectancy | 16.90 (10.80–20.10) | 16.00 (12.80–22.45) | 18.80 (13.15–21.85) | 17.70 (11.25–21.00) | 15.85 (10.30–19.83) | p = 0.563 | p = 0.959 | p = 0.529 | p = 0.308 | |||
| WMFT | ||||||||||||
| Functional ability (range 0–75) | 63.67 (37.25–71.00) | 63.00 (46.00–72.50) | 68.00 (44.00–74.00) | 70.00 (43.00–74.00) | 67.00 (53.50–74.25) | p = 0.000 | p = 0.004 | r = 0.523 | p = 0.002 | r = 0.547 | p = 0.018 | r = 0.455 |
| Performance time (sec) | 65.82 (40.72–390.78) | 59.91 (31.95–180.27) | 49.01 (28.76–269.16) | 136.53 (24.34–309.56) | 57.96 (23.23–177.30) | p = 0.000 | p = 0.039 | r = −0.376 | p = 0.001 | r = −0.581 | p = 0.046 | r = −0.383 |
| COPM (range 0–10) | ||||||||||||
| Performance | 3.00 (0.85–3.75) | 7.00 (5.15–7.80) | 7.00 (4.68–8.00) | p = 0.000 | p = 0.002 | r = 0.559 | p = 0.001 | r = 0.581 | p = 0.969 | |||
| Satisfaction | 3.00 (0.15–4.30) | 6.00 (4.00–7.80) | 7.10 (5.20–8.50) | p = 0.000 | p = 0.003 | r = 0.536 | p = 0.001 | r = 0.592 | p = 0.071 | |||
| MAM-36 (range 0–144) | 73.00 (35.15–102.85) | 79.00 (34.00–109.00) | 87.00 (44.00–118.50) | 79.00 (39.50–122.0) | 97.00 (38.50–127.00) | p = 0.000 | p = 0.007 | r = 0.493 | p = 0.001 | r = 0.592 | p = 0.052 | |
| MFIS (range 0–84) | 19.00 (4.50–41.50) | 30.00 (6.00–53.50) | 24.00 (3.00–42.00) | 24.00 (5.50–43.50) | 15.50 (2.75–41.75) | p = 0.254 | p = 0.824 | p = 0.432 | p = 0.160 | |||
| TIS (range 0–23) | 19.00 (13.85–21.85) | 21.00 (12.50–22.00) | 21.00 (16.00–23.00) | 21.00 (11.00–23.00) | 20.50 (6.00–23.00) | p = 0.342 | p = 0.514 | p = 0.514 | p = 0.833 | |||
| AROM (degrees) | ||||||||||||
| Shoulder abduction | 88.30 (67.50–162.50) | 90.00 (70.00–150.00) | 100.00 (75.00–155.00) | 100.00 (70.00–170.00) | 102.50 (68.75–160.00) | p = 0.000 | p = 0.109 | p = 0.100 | p = 0.167 | |||
| Shoulder anteflexion | 95.00 (80.00–147.50) | 100.00 (80.00–137.50) | 115.00 (82.50–147.50) | 100.00 (82.50–157.50) | 112.50 (80.50–162.50) | p = 0.001 | p = 0.071 | p = 0.011 | r = 0.459 | p = 0.019 | r = 0.453 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Knippenberg, E.; Lamers, I.; Timmermans, A.; Spooren, A. Motivation, Usability, and Credibility of an Intelligent Activity-Based Client-Centred Training System to Improve Functional Performance in Neurological Rehabilitation: An Exploratory Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 7641. https://doi.org/10.3390/ijerph18147641
Knippenberg E, Lamers I, Timmermans A, Spooren A. Motivation, Usability, and Credibility of an Intelligent Activity-Based Client-Centred Training System to Improve Functional Performance in Neurological Rehabilitation: An Exploratory Cohort Study. International Journal of Environmental Research and Public Health. 2021; 18(14):7641. https://doi.org/10.3390/ijerph18147641
Chicago/Turabian StyleKnippenberg, Els, Ilse Lamers, Annick Timmermans, and Annemie Spooren. 2021. "Motivation, Usability, and Credibility of an Intelligent Activity-Based Client-Centred Training System to Improve Functional Performance in Neurological Rehabilitation: An Exploratory Cohort Study" International Journal of Environmental Research and Public Health 18, no. 14: 7641. https://doi.org/10.3390/ijerph18147641
APA StyleKnippenberg, E., Lamers, I., Timmermans, A., & Spooren, A. (2021). Motivation, Usability, and Credibility of an Intelligent Activity-Based Client-Centred Training System to Improve Functional Performance in Neurological Rehabilitation: An Exploratory Cohort Study. International Journal of Environmental Research and Public Health, 18(14), 7641. https://doi.org/10.3390/ijerph18147641







