Determination of the Strongest Factor and Component in a Relationship between Lower-Extremity Assessment Protocol and Patient-Oriented Outcomes in Individuals with Anterior Cruciate Ligament Reconstruction: A Pilot Study
Abstract
:1. Introduction
2. Method
2.1. Participants
- Aged 19 to 40 years;
- Verified history of ACLR surgery; and
- ACLR surgery with autograft.
- A history of lower-extremity injuries within the past 3 months;
- A history of surgery in the lower extremities except for ACLR;
- A history of ACL re-injury (only patients who underwent ACLR due to an initial injury were included); and
- Damage or impairment affecting the muscle and nerve function.
2.2. Procedure
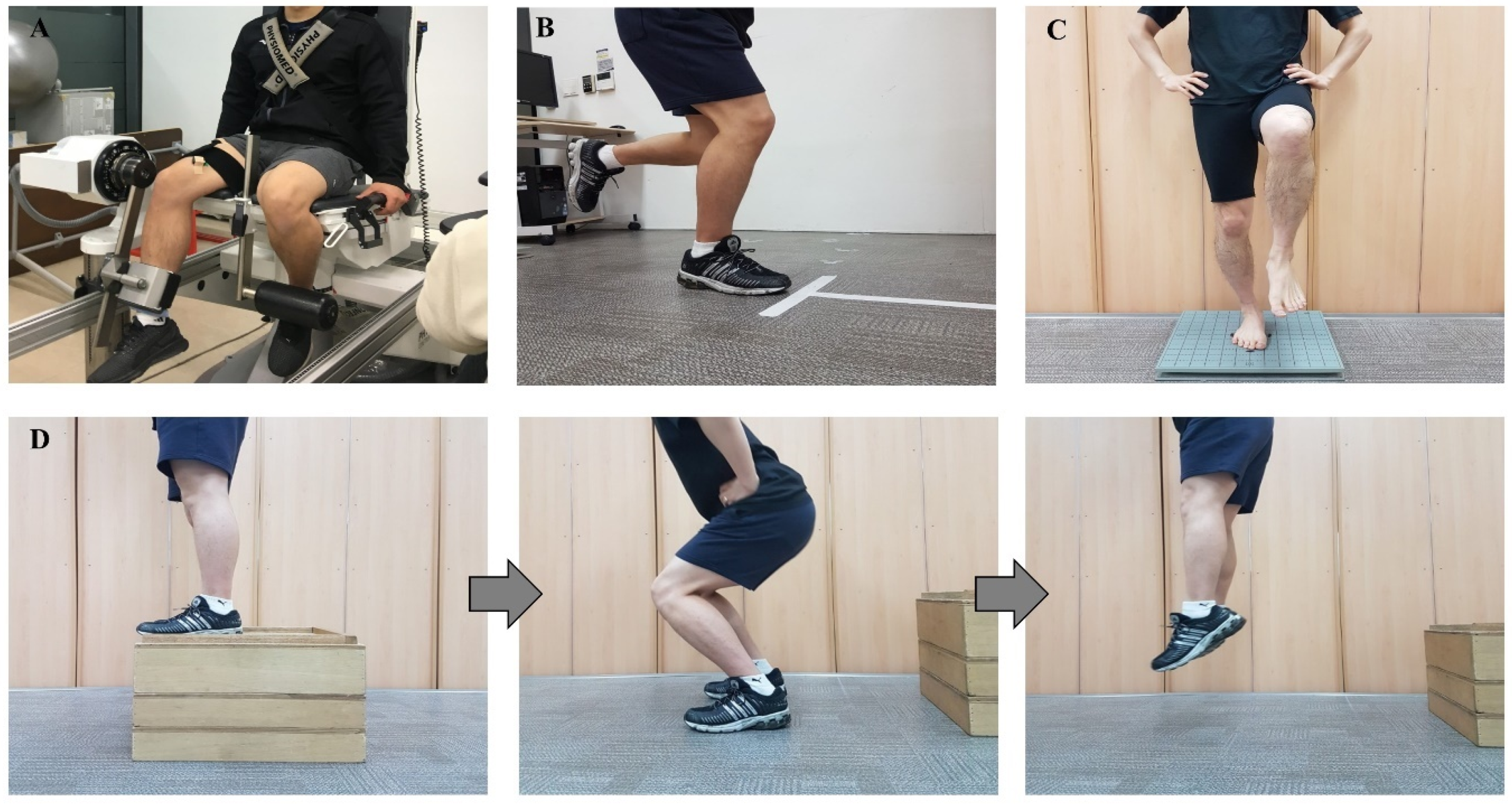
2.3. Strength Assessment and Fatigue Index
2.4. Functional Assessment
2.5. Balance Assessment
2.6. Jump Landing Assessment
2.7. Statistical Analysis
3. Results
3.1. Categorizing Results of the Lower-Extremity Assessment Protocol
3.2. The Strongest Factor of the Lower-Extremity Assessment Protocol
3.3. The Strongest Component of the Lower-Extremity Assessment Protocol
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Moses, B.; Orchard, J.; Orchard, J. Systematic review: Annual incidence of acl injury and surgery in various populations. Res. Sports Med. 2012, 20, 157–179. [Google Scholar] [CrossRef]
- Dönmez, G.; Korkusuz, F.; Özçakar, L.; Karanfil, Y.; Dursun, E.; Kudaş, S.; Doral, M.N. Injuries among recreational football players: Results of a prospective cohort study. Clin. J. Sport Med. 2018, 28, 249–254. [Google Scholar] [CrossRef] [PubMed]
- Griffin, L.Y.; Agel, J.; Albohm, M.J.; Arendt, E.A.; Dick, R.W.; Garrett, W.E.; Garrick, J.G.; Hewett, T.E.; Huston, L.; Ireland, M.L.; et al. Noncontact anterior cruciate ligament injuries: Risk factors and prevention strategies. J. Am. Acad. Orthop. Surg. 2000, 8, 141–150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hootman, J.M.; Dick, R.; Agel, J. Epidemiology of collegiate injuries for 15 sports: Summary and recommendations for injury prevention initiatives. J. Athl. Train. 2007, 42, 311–319. [Google Scholar]
- Orchard, J.; Seward, H.; McGivern, J.; Hood, S. Intrinsic and extrinsic risk factors for anterior cruciate ligament injury in Australian footballers. Am. J. Sports Med. 2001, 29, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.; Garrett, W.E. Mechanisms of non-contact acl injuries. Br. J. Sports Med. 2007, 41, i47–i51. [Google Scholar] [CrossRef] [Green Version]
- Fitzgerald, G.K.; Axe, M.J.; Snyder-Mackler, L. A decision-making scheme for returning patients to high-level activity with nonoperative treatment after anterior cruciate ligament rupture. Knee Surg. Sports Traumatol. Arthrosc. 2000, 8, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Petersen, W.; Taheri, P.; Forkel, P.; Zantop, T. Return to play following acl reconstruction: A systematic review about strength deficits. Arch. Orthop. Trauma Surg. 2014, 134, 1417–1428. [Google Scholar] [CrossRef]
- Diermann, N.; Schumacher, T.; Schanz, S.; Raschke, M.J.; Petersen, W.; Zantop, T. Rotational instability of the knee: Internal tibial rotation under a simulated pivot shift test. Arch. Orthop. Trauma Surg. 2009, 129, 353–358. [Google Scholar] [CrossRef]
- Paterno, M.V. Non-operative care of the patient with an acl-deficient knee. Curr. Rev. Musculoskelet. Med. 2017, 10, 322–327. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ardern, C.L.; Taylor, N.F.; Feller, J.A.; Webster, K.E. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: An updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br. J. Sports Med. 2014, 48, 1543–1552. [Google Scholar] [CrossRef] [Green Version]
- Ardern, C.L.; Webster, K.E.; Taylor, N.F.; Feller, J.A. Return to sport following anterior cruciate ligament reconstruction surgery: A systematic review and meta-analysis of the state of play. Br. J. Sports Med. 2011, 45, 596–606. [Google Scholar] [CrossRef] [PubMed]
- Daniel, D.M.; Stone, M.L.; Dobson, B.E.; Fithian, D.C.; Rossman, D.J.; Kaufman, K.R. Fate of the acl-injured patient. A prospective outcome study. Am. J. Sports Med. 1994, 22, 632–644. [Google Scholar] [CrossRef]
- Lee, D.Y.; Karim, S.A.; Chang, H.C. Return to sports after anterior cruciate ligament reconstruction—A review of patients with minimum 5-year follow-up. Ann. Acad. Med. Singap. 2008, 37, 273–278. [Google Scholar] [PubMed]
- Marx, R.G.; Jones, E.C.; Angel, M.; Wickiewicz, T.L.; Warren, R.F. Beliefs and attitudes of members of the American Academy of Orthopaedic Surgeons regarding the treatment of anterior cruciate ligament injury. Arthroscopy 2003, 19, 762–770. [Google Scholar] [CrossRef]
- Nakayama, Y.; Shirai, Y.; Narita, T.; Mori, A.; Kobayashi, K. Knee functions and a return to sports activity in competitive athletes following anterior cruciate ligament reconstruction. J. Nippon Med. Sch. 2000, 67, 172–176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petersen, W.; Forkel, P.; Achtnich, A.; Metzlaff, S.; Zantop, T. Technique of anatomical footprint reconstruction of the acl with oval tunnels and medial portal aimers. Arch. Orthop. Trauma Surg. 2013, 133, 827–833. [Google Scholar] [CrossRef]
- Wilk, K.E. Anterior cruciate ligament injury prevention and rehabilitation: Let’s get it right. J. Orthop. Sports Phys. Ther. 2015, 45, 729–730. [Google Scholar] [CrossRef]
- Dienst, M.; Burks, R.T.; Greis, P.E. Anatomy and biomechanics of the anterior cruciate ligament. Orthop. Clin. N. Am. 2002, 33, 605–620. [Google Scholar] [CrossRef]
- Baugher, W.H.; Warren, R.F.; Marshall, J.L.; Joseph, A. Quadriceps atrophy in the anterior cruciate insufficient knee. Am. J. Sports Med. 1984, 12, 192–195. [Google Scholar] [CrossRef]
- Arvidsson, I.; Eriksson, E.; Häggmark, T.; Johnson, R.J. Isokinetic thigh muscle strength after ligament reconstruction in the knee joint: Results from a 5–10 year follow-up after reconstructions of the anterior cruciate ligament in the knee joint. Int. J. Sports Med. 1981, 2, 7–11. [Google Scholar] [CrossRef]
- Knezevic, O.M.; Mirkov, D.M.; Kadija, M.; Nedeljkovic, A.; Jaric, S. Asymmetries in explosive strength following anterior cruciate ligament reconstruction. Knee 2014, 21, 1039–1045. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smeets, A.; Verschueren, S.; Staes, F.; Vandenneucker, H.; Claes, S.; Vanrenterghem, J. Athletes with an acl reconstruction show a different neuromuscular response to environmental challenges compared to uninjured athletes. Gait Posture 2021, 83, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Han, S.B.; Park, J.H.; Choi, J.H.; Suh, D.K.; Jang, K.M. Impaired neuromuscular control up to postoperative 1 year in operated and nonoperated knees after anterior cruciate ligament reconstruction. Medicine 2019, 98, e15124. [Google Scholar] [CrossRef]
- Paterno, M.V.; Rauh, M.J.; Schmitt, L.C.; Ford, K.R.; Hewett, T.E. Incidence of second acl injuries 2 years after primary acl reconstruction and return to sport. Am. J. Sports Med. 2014, 42, 1567–1573. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DiFabio, M.; Slater, L.V.; Norte, G.; Goetschius, J.; Hart, J.M.; Hertel, J. Relationships of functional tests following acl reconstruction: Exploratory factor analyses of the lower extremity assessment protocol. J. Sport Rehabil. 2018, 27, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, L.C.; Paterno, M.V.; Hewett, T.E. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J. Orthop. Sports Phys. Ther. 2012, 42, 750–759. [Google Scholar] [CrossRef] [Green Version]
- Lepley, L.K. Deficits in quadriceps strength and patient-oriented outcomes at return to activity after acl reconstruction: A review of the current literature. Sports Health 2015, 7, 231–238. [Google Scholar] [CrossRef]
- Kim, B.H.; Jeon, H.G.; Cheo, J.H.; Kang, T.K.; Lee, S.Y. Objective and subjective analysis of the knee joint function using lower extremity assessment protocol after anterior cruciate ligament reconstruction. Korean Soc. Sports Med. 2021, 39, 34–41. [Google Scholar] [CrossRef]
- Bodkin, S.G.; Werner, B.C.; Slater, L.V.; Hart, J.M. Post-traumatic osteoarthritis diagnosed within 5 years following acl reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 790–796. [Google Scholar] [CrossRef]
- Reid, A.; Birmingham, T.B.; Stratford, P.W.; Alcock, G.K.; Giffin, J.R. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys. Ther. 2007, 87, 337–349. [Google Scholar] [CrossRef] [Green Version]
- Padua, D.A.; Marshall, S.W.; Boling, M.C.; Thigpen, C.A.; Garrett, W.E., Jr.; Beutler, A.I. The landing error scoring system (LESS) is a valid and reliable clinical assessment tool of jump-landing biomechanics: The jump-acl study. Am. J. Sports Med. 2009, 37, 1996–2002. [Google Scholar] [CrossRef]
- Logerstedt, D.; Grindem, H.; Lynch, A.; Eitzen, I.; Engebretsen, L.; Risberg, M.A.; Axe, M.J.; Snyder-Mackler, L. Single-legged hop tests as predictors of self-reported knee function after anterior cruciate ligament reconstruction: The Delaware-oslo acl cohort study. Am. J. Sports Med. 2012, 40, 2348–2356. [Google Scholar] [CrossRef] [Green Version]
- Xergia, S.A.; Pappas, E.; Georgoulis, A.D. Association of the single-limb hop test with isokinetic, kinematic, and kinetic asymmetries in patients after anterior cruciate ligament reconstruction. Sports Health 2015, 7, 217–223. [Google Scholar] [CrossRef] [Green Version]
- Sueyoshi, T.; Nakahata, A.; Emoto, G.; Yuasa, T. Single-leg hop test performance and isokinetic knee strength after anterior cruciate ligament reconstruction in athletes. Orthop. J. Sports Med. 2017, 5. [Google Scholar] [CrossRef] [Green Version]
- Arna Risberg, M.; Lewek, M.; Snyder-Mackler, L. A systematic review of evidence for anterior cruciate ligament rehabilitation: How much and what type? Phys. Ther. Sport 2004, 5, 125–145. [Google Scholar] [CrossRef]
- Czuppon, S.; Racette, B.A.; Klein, S.E.; Harris-Hayes, M. Variables associated with return to sport following anterior cruciate ligament reconstruction: A systematic review. Br. J. Sports Med. 2014, 48, 356–364. [Google Scholar] [CrossRef] [PubMed]
- Kocher, M.S.; Steadman, J.R.; Briggs, K.; Zurakowski, D.; Sterett, W.I.; Hawkins, R.J. Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstruction. Bone Jt. Surg. Am. 2002, 84, 1560–1572. [Google Scholar] [CrossRef]
- Pietrosimone, B.; Lepley, A.S.; Harkey, M.S.; Luc-Harkey, B.A.; Blackburn, J.T.; Gribble, P.A.; Spang, J.T.; Sohn, D.H. Quadriceps Strength Predicts Self-reported Function Post-ACL Reconstruction. Med. Sci. Sports Exerc. 2016, 48, 1671–1677. [Google Scholar] [CrossRef] [PubMed]
- Ageberg, E.; Roos, H.P.; Silbernagel, K.G.; Thomeé, R.; Roos, E.M. Knee extension and flexion muscle power after anterior cruciate ligament reconstruction with patellar tendon graft or hamstring tendons graft: A cross-sectional comparison 3 years post surgery. Knee Surg. Sports Traumatol. Arthrosc. 2009, 17, 162–169. [Google Scholar] [CrossRef]
- Zebis, M.K.; Andersen, L.L.; Bencke, J.; Kjaer, M.; Aagaard, P. Identification of athletes at future risk of anterior cruciate ligament ruptures by neuromuscular screening. Am. J. Sports Med. 2009, 37, 1967–1973. [Google Scholar] [CrossRef]
- Della Villa, F.; Ricci, M.; Perdisa, F.; Filardo, G.; Gamberini, J.; Caminati, D.; Della Villa, S. Anterior cruciate ligament reconstruction and rehabilitation: Predictors of functional outcome. Joints 2015, 3, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Paterno, M.V.; Schmitt, L.C.; Ford, K.R.; Rauh, M.J.; Myer, G.D.; Huang, B.; Hewett, T.E. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am. J. Sports Med. 2010, 38, 1968–1978. [Google Scholar] [CrossRef] [PubMed]
- Hewett, T.E.; Myer, G.D.; Ford, K.R.; Heidt, R.S., Jr.; Colosimo, A.J.; McLean, S.G.; van den Bogert, A.J.; Paterno, M.V.; Succop, P. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. Am. J. Sports Med. 2005, 33, 492–501. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rozzi, S.L.; Lephart, S.M.; Fu, F.H. Effects of muscular fatigue on knee joint laxity and neuromuscular characteristics of male and female athletes. J. Athl. Train. 1999, 34, 106–114. [Google Scholar]
- Hiemstra, L.A.; Lo, I.K.; Fowler, P.J. Effect of fatigue on knee proprioception: Implications for dynamic stabilization. J. Orthop. Sports Phys. Ther. 2001, 31, 598–605. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sakai, H.; Tanaka, S.; Kurosawa, H.; Masujima, A. The effect of exercise on anterior knee laxity in female basketball players. Int. J. Sports Med. 1992, 13, 552–554. [Google Scholar] [CrossRef]
- Skinner, H.B.; Wyatt, M.P.; Hodgdon, J.A.; Conard, D.W.; Barrack, R.L. Effect of fatigue on joint position sense of the knee. J. Orthop. Res. 1986, 4, 112–118. [Google Scholar] [CrossRef]
- Steiner, M.E.; Brown, C.; Zarins, B.; Brownstein, B.; Koval, P.S.; Stone, P. Measurement of anterior–posterior displacement of the knee. A comparison of the results with instrumented devices and with clinical examination. J. Bone Jt. Surg. Am. 1990, 72, 1307–1315. [Google Scholar] [CrossRef]
- Csapo, R.; Pointner, H.; Hoser, C.; Gföller, P.; Raschner, C.; Fink, C. Physical fitness after anterior cruciate ligament reconstruction: Influence of graft, age, and sex. Sports 2020, 8, 30. [Google Scholar] [CrossRef] [Green Version]
- El-Kotob, R.; Giangregorio, L.M. Pilot and feasibility studies in exercise, physical activity, or rehabilitation research. Pilot Feasibility Stud. 2018, 4, 137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuenze, C.M.; Trigsted, S.; Lisee, C.; Post, E.; Bell, D.R. Sex differences on the landing error scoring system among individuals with anterior cruciate ligament reconstruction. J. Athl. Train. 2018, 53, 837–843. [Google Scholar] [CrossRef] [PubMed]
- Hanzlíková, I.; Athens, J.; Hébert-Losier, K. Clinical implications of Landing Error Scoring System calculation methods. Phys. Ther. Sport 2020, 44, 61–66. [Google Scholar] [CrossRef] [PubMed]

| ACLR (n = 15) | |
|---|---|
| Age (years) | 27.87 ± 4.10 |
| Sex (m:f) | 12:3 |
| Height (cm) | 172.56 ± 4.81 |
| Weight (kg) | 75.51 ± 13.03 |
| Time to surgery (months) | 27.11 ± 14.03 |
| IKDC score (percentage) | 71.87 ± 16.60 |
| Tegner activity level (current) | 5.73 ± 1.16 |
| Components | Factor Loading | ||||
| Factor 1 | Factor 2 | Factor 3 | Factor 4 | ||
| Functional task | Single hop | 0.926 | 0.296 | −0.131 | 0.007 |
| Triple hop | 0.900 | 0.374 | −0.184 | 0.031 | |
| Cross-over hop | 0.877 | 0.389 | −0.188 | 0.035 | |
| 6 m timed hop | −0.784 | −0.198 | 0.422 | 0.267 | |
| Muscle strength | Isokinetic knee flexion 180°/s | 0.144 | 0.917 | −0.265 | −0.018 |
| Isokinetic knee extension 180°/s | 0.310 | 0.868 | 0.130 | 0.087 | |
| Isokinetic knee flexion 90°/s | 0.407 | 0.849 | −0.070 | −0.212 | |
| Isokinetic knee extension 90°/s | 0.389 | 0.778 | −0.155 | 0.262 | |
| Isometric knee extension | 0.547 | 0.551 | 0.118 | 0.485 | |
| Isometric knee flexion | 0.497 | 0.504 | −0.177 | 0.254 | |
| Neuromuscular control | Static single-leg balance | −0.208 | −0.122 | 0.892 | −0.106 |
| Landing error scoring system | −0.319 | −0.127 | 0.772 | 0.107 | |
| Fatigue index | Knee flexion fatigue index | −0.147 | −0.047 | −0.079 | 0.854 |
| Knee extension fatigue index | 0.217 | 0.245 | 0.509 | 0.614 | |
| Eigenvalue | 4.247 | 3.989 | 2.084 | 1.625 | |
| Variance (%) | 30.335 | 28.492 | 14.884 | 11.604 | |
| Cumulative variance (%) | 30.335 | 58.827 | 73.710 | 85.315 | |
| KMO = 0.318, Bartlett’s x = 253.318 (p < 0.001). | |||||
| Dependent Variable | B | S.E. | β | t | F | p | VIF | R2 | adjR2 | R2 Change |
| (Constant) | 43.85 | 9.52 | 4.60 | |||||||
| Functional task a | 0.03 | 0.11 | 0.66 | 3.14 | 9.88 * | 0.008 | 1.00 | 0.43 | 0.39 | 0.43 |
| Dependent Variable | B | S.E. | β | t | F | p | VIF | R2 | adjR2 | R2Change |
|---|---|---|---|---|---|---|---|---|---|---|
| (Constant) | 42.82 | 8.78 | 4.88 | |||||||
| Single hop a | 0.26 | 0.08 | 0.70 | 3.55 | 12.57 * | 0.004 | 1.00 | 0.49 | 0.45 | 0.49 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeon, H.G.; Kim, B.H.; Kang, T.K.; Jeong, H.S.; Lee, S.Y. Determination of the Strongest Factor and Component in a Relationship between Lower-Extremity Assessment Protocol and Patient-Oriented Outcomes in Individuals with Anterior Cruciate Ligament Reconstruction: A Pilot Study. Int. J. Environ. Res. Public Health 2021, 18, 8053. https://doi.org/10.3390/ijerph18158053
Jeon HG, Kim BH, Kang TK, Jeong HS, Lee SY. Determination of the Strongest Factor and Component in a Relationship between Lower-Extremity Assessment Protocol and Patient-Oriented Outcomes in Individuals with Anterior Cruciate Ligament Reconstruction: A Pilot Study. International Journal of Environmental Research and Public Health. 2021; 18(15):8053. https://doi.org/10.3390/ijerph18158053
Chicago/Turabian StyleJeon, Hyung Gyu, Byong Hun Kim, Tae Kyu Kang, Hee Seong Jeong, and Sae Yong Lee. 2021. "Determination of the Strongest Factor and Component in a Relationship between Lower-Extremity Assessment Protocol and Patient-Oriented Outcomes in Individuals with Anterior Cruciate Ligament Reconstruction: A Pilot Study" International Journal of Environmental Research and Public Health 18, no. 15: 8053. https://doi.org/10.3390/ijerph18158053






