A Comprehensive Community-Based Prevalence Study on Nocturia in Hong Kong Male Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design & Subject Recruitment
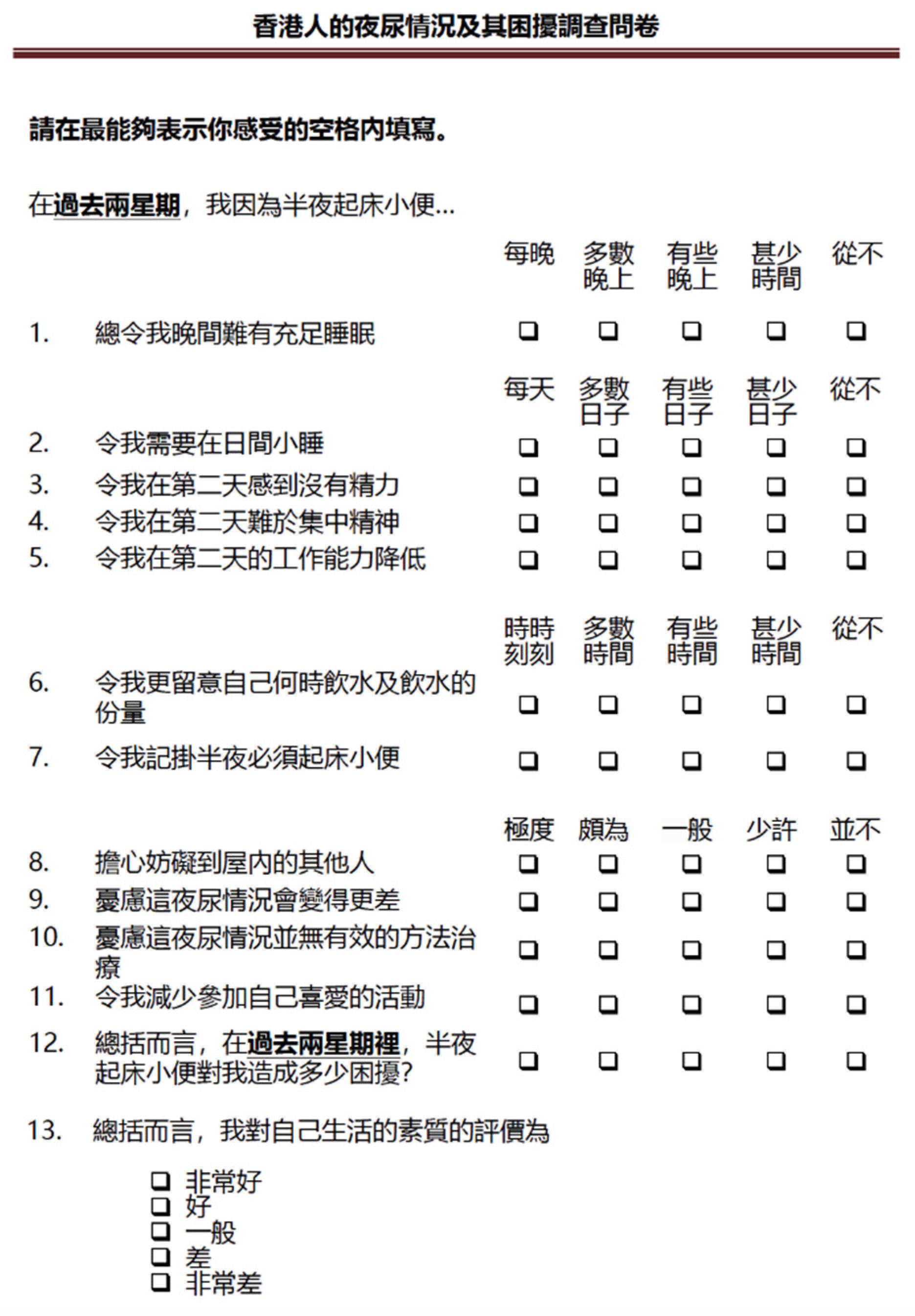
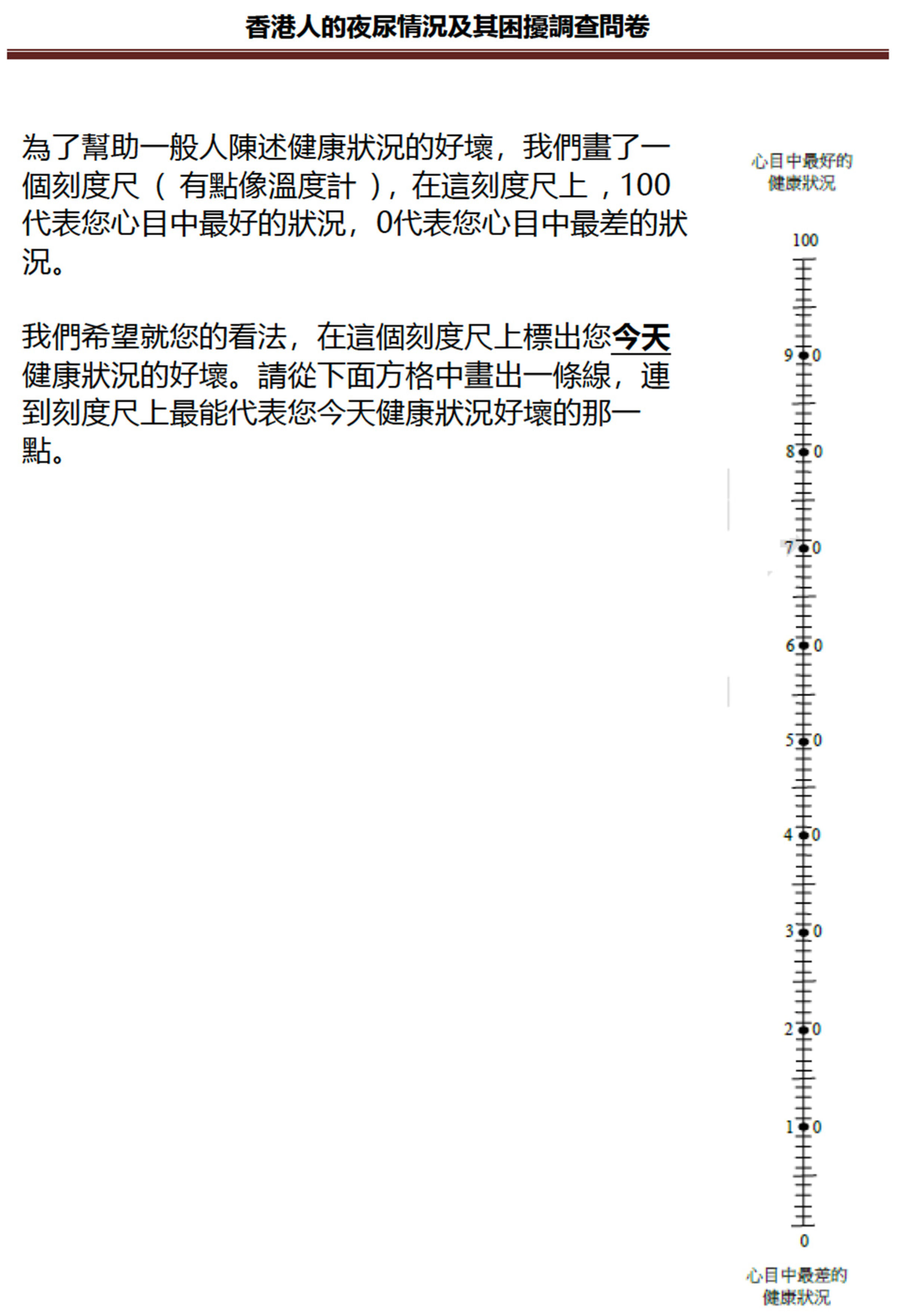
2.2. The Instruments and Measurements
2.3. Date Processing and Statistical Analysis
3. Results
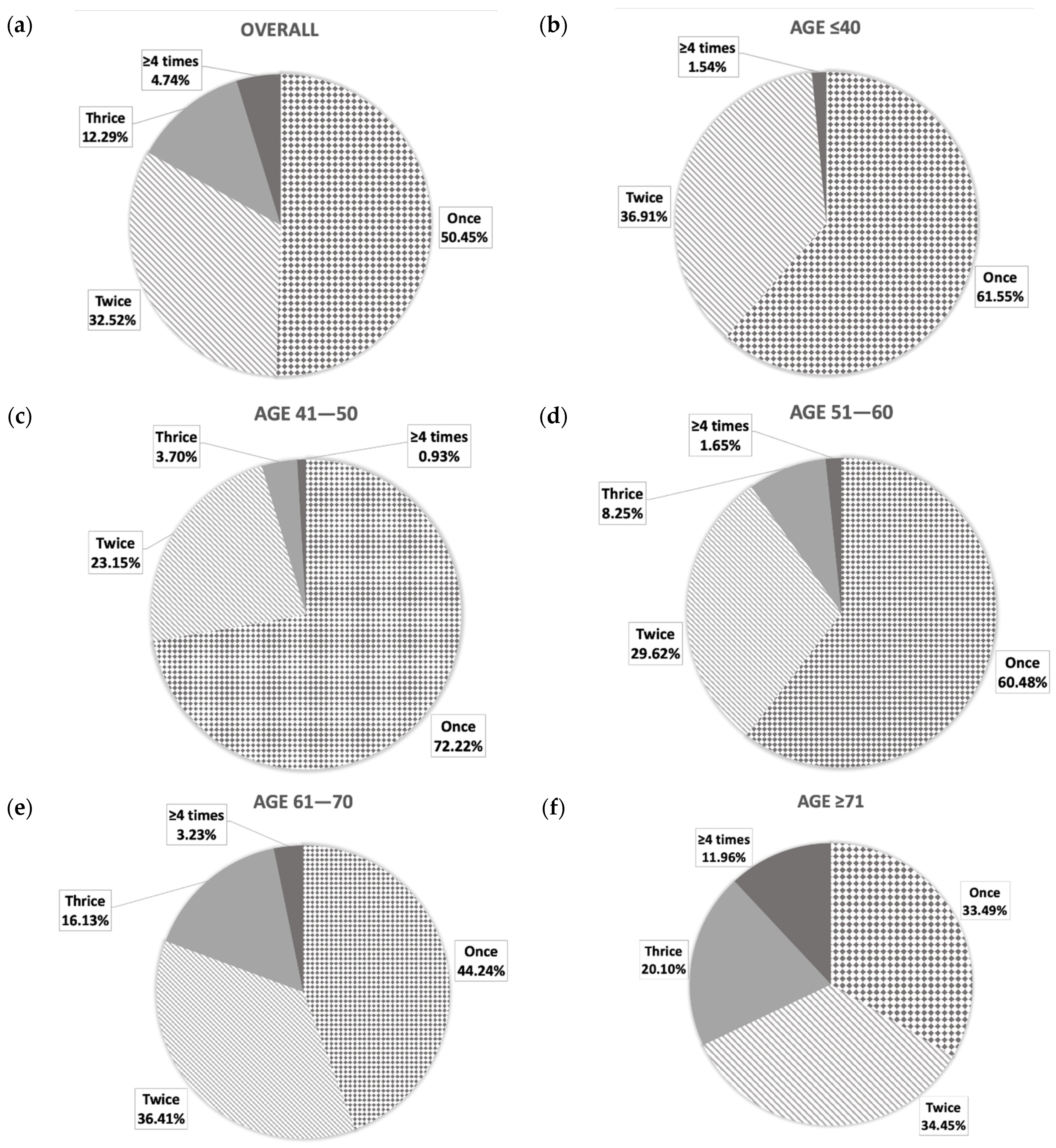
3.1. Prevalence and Characteristics of Nocturia
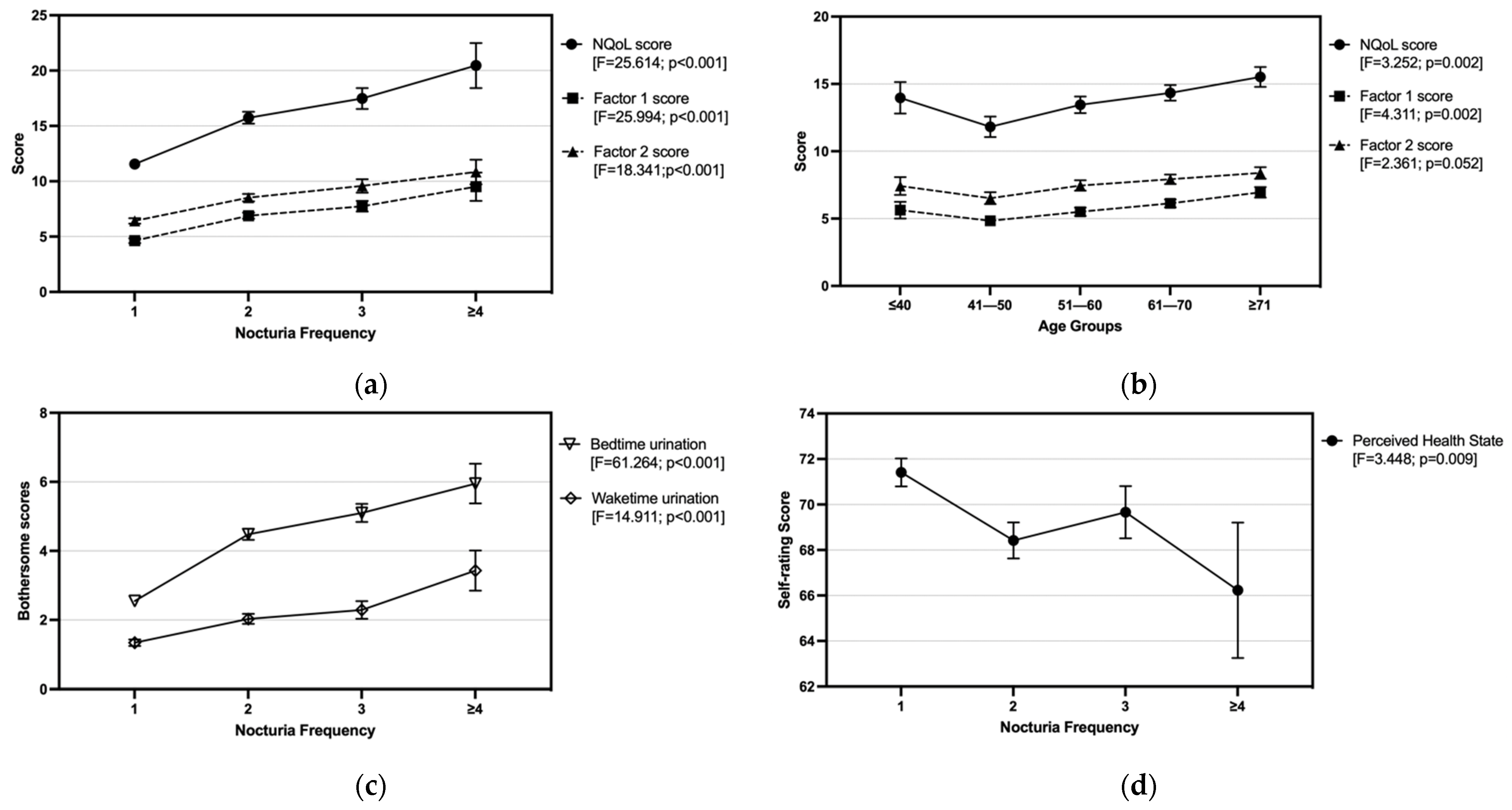
3.2. Nocturia-Related QoL and Bothersome
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- van Kerrebroeck, P.; Abrams, P.; Chaikin, D.; Donovan, J.; Fonda, D.; Jackson, S.; Jennum, P.; Johnson, T.; Lose, G.; Mattiasson, A.; et al. Standardisation Sub-committee of the International Continence Society. The standardisation of terminology in nocturia: Report from the Standardisation Sub-committee of the International Continence Society. Neurourol. Urodyn. 2002, 21, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J. Insomnia. J. Am. Med. Assoc. 2013, 309, 706–716. [Google Scholar] [CrossRef]
- Kobelt, G.; Borgström, F.; Mattiasson, A. Productivity, vitality and utility in a group of healthy professionally active individuals with nocturia. BJU Int. 2003, 91, 190–195. [Google Scholar] [CrossRef] [PubMed]
- Hunter, P. To sleep, perchance to live. Sleeping is vital for health, cognitive function, memory and long life. EMBO Rep. 2008, 9, 1070–1073. [Google Scholar] [CrossRef][Green Version]
- Choi, E.P.H.; Wan, E.Y.F.; Kwok, J.Y.Y.; Chin, W.Y.; Lam, C.L.K. The mediating role of sleep quality in the association between nocturia and health-related quality of life. Health Qual. Life Outcomes 2019, 17, 181. [Google Scholar] [CrossRef] [PubMed]
- Schneider, T.; de la Rosette, J.J.; Michel, M.C. Nocturia: A non-specific but important symptom of urological disease. Int. J. Urol. 2009, 16, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Gulur, D.M.; Mevcha, A.M.; Drake, M.J. Nocturia as a manifestation of systemic disease. BJU Int. 2011, 107, 702–713. [Google Scholar] [CrossRef] [PubMed]
- Weiss, J.P.; Blaivas, J.G.; Jones, M.; Wang, J.T.; Guan, Z.; 037 Study Group. Age related pathogenesis of nocturia in patients with overactive bladder. J. Urol. 2007, 178, 548–551. [Google Scholar] [CrossRef]
- Homma, Y. Classification of nocturia in the adult and elderly patient: A review of clinical criteria and selected literature. BJU Int. 2005, 96, 8–14. [Google Scholar] [CrossRef]
- Um, Y.H.; Oh, J.; Kim, T.; Seo, H.; Kim, S.; Chung, J.; Jeong, J.; Hong, S. Nocturia and sleep: Focus on common comorbidies and their association with obstructive sleep apnea. Sleep Med. Res. 2020, 11, 59–64. [Google Scholar] [CrossRef]
- Ali, A.; Snape, J. Nocturia in older people: A review of causes, consequences, assessment and management. Int. J. Clin. Pract. 2004, 58, 366–373. [Google Scholar] [CrossRef]
- Van Kerrebroeck, P.E.; Dmochowski, R.; FitzGerald, M.P.; Hashim, H.; Norgaard, J.P.; Robinson, D.; Weiss, J.P. Nocturia research: Current status and future perspectives. Neurourol. Urodyn. 2010, 29, 623–628. [Google Scholar] [CrossRef]
- Wyndaele, J.J. Nocturia and quality of life. Eur. Urol. 2012, 61, 85–87. [Google Scholar] [CrossRef]
- Furtado, D.; Hachul, H.; Andersen, M.L.; Castro, R.A.; Girão, M.B.; Tufik, S. Nocturia × disturbed sleep: A review. Int. Urogynecol. J. 2012, 23, 255–267. [Google Scholar] [CrossRef]
- Bosch, J.L.; Weiss, J.P. The prevalence and causes of nocturia. J. Urol. 2010, 184, 440–446. [Google Scholar] [CrossRef]
- Wang, J.Y.; Liao, L.; Liu, M.; Sumarsono, B.; Cong, M. Epidemiology of lower urinary tract symptoms in a cross-sectional, population-based study: The status in China. Medicine 2018, 97, e11554. [Google Scholar] [CrossRef] [PubMed]
- Li, M.K.; Garcia, L.A.; Rosen, R. Lower urinary tract symptoms and male sexual dysfunction in Asia: A survey of ageing men from five Asian countries. BJU Int. 2005, 96, 1339–1354. [Google Scholar] [CrossRef] [PubMed]
- Yee, C.H.; Chan, C.K.; Teoh, J.Y.C.; Chiu, P.K.F.; Wong, J.H.M.; Chan, E.S.Y.; Hou, S.S.M.; Ng, C.F. Survey on prevalence of lower urinary tract symptoms in an Asian population. Hong Kong Med. J. 2019, 25, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Ho, L.Y.; Chan, C.K.; Chu, P.S. Patient opinion of lower urinary tract symptoms and their treatment: A cross-sectional survey in Hong Kong public urology clinics. Hong Kong Med. J. 2017, 23, 562–569. [Google Scholar] [CrossRef][Green Version]
- Wong, M.K.T.; Leung, S.Y.L. Cross-sectional population based study on nocturia in Hong Kong: Prevalence, impacts, and treatment seeking behaviours. BJU Int. 2016, 117, 11. [Google Scholar]
- Tam, P.C. Nocturia survey in Hong Kong. HK Med. D 2005, 10, 13. [Google Scholar]
- Chiu, M.Y.L.; Wong, H.T.; Yang, X. Distress Due to Urinary Problems and Psychosocial Correlates among Retired Men in Hong Kong. Int. J. Environ. Res. Public Health 2020, 17, 2533. [Google Scholar] [CrossRef]
- Census & Statistics Department. Hong Kong Population By-Census. 2017. Available online: www.censtatd.gov.hk/hkstat/sub/sp459.jsp?productCode=B112160A (accessed on 4 August 2021).
- Abraham, L.; Hareendran, A.; Mills, I.W.; Martin, M.L.; Abrams, P.; Drake, M.J.; MacDonagh, R.P.; Noble, J.G. Development and validation of a quality-of-life measure for men with nocturia. Urology 2004, 63, 481–486. [Google Scholar] [CrossRef]
- Feng, Y.; Parkin, D.; Devlin, N.J. Assessing the performance of the EQ-VAS in the NHS PROMs programme. Qual. Life Res. 2014, 23, 977–989. [Google Scholar] [CrossRef]
- Irwin, D.E.; Milsom, I.; Hunskaar, S.; Reilly, K.; Kopp, Z.; Herschorn, S.; Coyne, K.; Kelleher, C.; Hampel, C.; Artibani, W.; et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: Results of the EPIC study. Eur. Urol. 2006, 50, 1306–1314. [Google Scholar] [CrossRef] [PubMed]
- Kageyama, T.; Kabuto, M.; Nitta, H.; Kurokawa, Y.; Taira, K.; Suzuki, S.; Takemoto, T. Prevalence of nocturia among Japanese adults. Psychiatry Clin. Neurosci. 2000, 54, 299–300. [Google Scholar] [CrossRef]
- Liew, L.C.; Tiong, H.Y.; Wong, M.L.; Png, D.C.; Tan, J.K. A population study of nocturia in Singapore. BJU Int. 2006, 97, 109–112. [Google Scholar] [CrossRef]
- Wang, Y.; Hu, H.; Xu, K.; Zhang, X.; Wang, X.; Na, Y.; Kang, X. Prevalence, risk factors, and symptom bother of nocturia: A population-based survey in China. World J. Urol. 2015, 33, 677–683. [Google Scholar] [CrossRef] [PubMed]
- Kalejaiye, O.; Persad, R.; Rees, J. Assessment of lower urinary tract symptoms in younger men. Br. J. Fam. Med. 2013, 1, 24–27. [Google Scholar]
- Jeong, S.J.; Yeon, J.S.; Lee, J.K.; Jeong, J.W.; Lee, B.K.; Park, Y.H.; Lee, S.C.; Jeong, C.W.; Kim, J.H.; Hong, S.K.; et al. Chronic lower urinary tract symptoms in young men without symptoms of chronic prostatitis: Urodynamic analyses in 308 men aged 50 years or younger. Korean J. Urol. 2014, 55, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.C.; Lin, A.T.; Chen, K.K.; Chang, L.S. Multifactorial nature of male nocturia. Urology 2006, 67, 541–544. [Google Scholar] [CrossRef] [PubMed]
- Asplund, R. Nocturia: Consequences for sleep and daytime activities and associated risks. Eur. Urol. Suppl. 2005, 3, 24–32. [Google Scholar] [CrossRef]
- Kupelian, V.; Wei, J.T.; O’Leary, M.P.; Norgaard, J.P.; Rosen, R.C.; McKinlay, J.B. Nocturia and quality of life: Results from the Boston area community health survey. Eur. Urol. 2012, 61, 78–84. [Google Scholar] [CrossRef]
- Bruce, E.S.; Lunt, L.; McDonagh, J.E. Sleep in adolescents and young adults. Clin. Med. 2017, 17, 422–428. [Google Scholar] [CrossRef] [PubMed]
- Lam, C.T.; Tse, S.H.; Chan, S.T.; Tam, J.K.; Yuen, J.W.M. A survey on the prevalence and utilization characteristics of gua sha in the Hong Kong community. Complement. Ther. Med. 2015, 23, 46–54. [Google Scholar] [CrossRef] [PubMed]

| Variables | Total | Non-Nocturia | Nocturia | χ2 |
|---|---|---|---|---|
| N = 1239 | N = 458 | N = 781 | p-Value | |
| Number (Percentage; Confidence Interval 95%) | ||||
| Demographics | ||||
| Mean age ± SD, years | 56.57 ± 15.22 | 49.83 ± 14.84 | 60.52 ± 14.01 | <0.001 # |
| Married/cohabited | 822 (66.3; 63.6–69.0) | 306 (66.8; 62.3–71.1) | 516 (66.1; 62.6–69.4) | 0.789 |
| Education < college | 750 (60.5; 57.7–63.3) | 217 (47.4; 42.7–52.1) | 533 (68.2; 64.9–71.5) | <0.001 |
| Current smoker | 610 (49.2; 46.4–52.1) | 202 (44.1; 40.7–47.7) | 452 (57.9; 53.2–62.4) | <0.001 |
| Daily drinker | 312 (25.2; 22.8–27.7) | 107 (23.4; 19.6–27.5) | 205 (26.2; 23.2–29.5) | 0.489 |
| Waketime Urination | ||||
| Every hour | 56 (4.5; 3.4–5.8) | 13 (2.8; 1.5–4.8) | 43 (5.5; 4.0–7.3) | <0.001 |
| Every 2 h | 330 (26.6; 24.2–29.2) | 81 (17.7; 14.3–21.5) | 249 (31.9; 28.6–35.3) | |
| Every 3 h | 485 (39.1; 36.4–41.9) | 173 (37.8; 33.3–42.4) | 312 (40.0; 36.5–43.5) | |
| ≥Every 4 h | 368 (29.7; 27.2–32.3) | 191 (41.7; 37.1–46.4) | 177 (22.7; 19.8–25.8) | |
| Bothersome (0–10), mean ± SD | 1.67 ± 2.20 | 0.93 ± 1.53 | 1.78 ± 2.27 | <0.001 # |
| Health & Illnesses | ||||
| Diabetes Mellitus | 181 (14.6; 12.7–16.7) | 34 (7.4; 5.2–10.2) | 147 (18.8; 16.1–21.7) | <0.001 |
| Hypertension | 448 (36.2; 33.5–38.9) | 98 (21.4; 17.7–25.4) | 350 (44.8; 41.3–48.4) | <0.001 |
| Diabetes Mellitus + Hypertension | 153 (12.3; 10.6–14.3) | 30 (6.6; 4.5–9.2) | 123 (15.7; 13.3–18.5) | <0.001 |
| Benign prostatic hyperplasia | 96 (7.8; 6.3–9.4) | 9 (2.0; 0.9–3.7) | 87 (11.1; 0.9–13.6) | <0.001 |
| Prostate cancer | 5 (0.4; 0.1–0.9) | 0 (0; 0–0.8) | 5 (0.6; 0.2–1.5) | 0.086 |
| On Benign prostatic hyperplasia medication | 65 (5.3; 431–6.6) | 7 (1.5; 0.6–3.1) | 58 (7.4; 5.7–9.5) | <0.001 |
| Health state (0–100), mean ± SD | 72.85 ± 12.57 | 76.79 ± 11.41 | 70.17 ± 12.64 | <0.001 # |
| Nocturia Episodes | Frequency | Percentage | Age (Mean ± SD, Years) |
|---|---|---|---|
| 1 | 394 | 50.4 | 57.01 ± 13.53 |
| 2 | 254 | 32.5 | 61.06 ± 14.20 |
| 3 | 96 | 12.3 | 68.65 ± 9.11 |
| ≥4 | 37 | 4.7 | 73.00 ± 12.01 |
| Variables | NQoL Factor 2 Score | NQoL Factor 1 Score | NQoL Score | Nocturia Frequency | Waketime Urination Frequency |
|---|---|---|---|---|---|
| Pearson Correlation Coefficient (r); p-Value | |||||
| Age | 0.088; 0.014 | 0.137; <0.001 | 0.103; 0.004 | 0.329; <0.001 | 0.045; 0.206 |
| Waketime urination frequency | −0.117; 0.001 | −0.207; <0.001 | −0.178; <0.001 | −0.294; <0.001 | |
| Nocturia frequency | 0.253; <0.001 | 0.301; <0.001 | 0.294; <0.001 | ||
| NQoL score | 0.954; <0.001 | 0.928; <0.001 | |||
| NQoL Factor 1 score | 0.787; <0.001 | ||||
| NQoL Items | Nocturia Frequency | χ2 | |||
|---|---|---|---|---|---|
| 1 Time | 2 Times | 3 Times | ≥4 Times | p-Value | |
| N = 391 | N = 254 | N = 96 | N = 37 | ||
| Number (Percentage) # | |||||
| Rated the overall QoL poor/very poor | 51 (13.0) | 38 (15.0) | 16 (16.7) | 11 (29.7) | <0.001 |
| Factor 1 (Sleep/Energy) | |||||
| Difficult to concentrate the next day | 50 (12.8) | 81 (31.9) | 33 (34.4) | 14 (37.8) | <0.001 |
| Feel no energy the next day | 73 (18.7) | 103 (40.6) | 51 (53.1) | 18 (48.7) | <0.001 |
| Required to nap at day time | 92 (23.5) | 124 (48.8) | 59 (61.5) | 17 (46.0) | <0.001 |
| Lowered next day’s productivity | 41 (10.5) | 53 (20.9) | 19 (19.8) | 11 (29.7) | <0.001 |
| Participate less in favorite activities | 42 (10.7) | 37 (14.6) | 22 (22.9) | 14 (37.8) | <0.001 |
| Difficult to get enough sleep at night ^ | 121 (31.0) | 123 (48.4) | 61 (63.5) | 19 (51.4) | <0.001 |
| Factor 2 (Bother/Concern) | |||||
| Pay more attention of when and how much to drink | 168 (43.0) | 117 (46.1) | 37 (38.5) | 12 (32.4) | 0.012 |
| Difficult to get enough sleep at night ^ | 121 (31.0) | 123 (48.4) | 61 (63.5) | 19 (51.4) | <0.001 |
| Worried disturbing others in the house because of having to get up in the middle of night to urinate | 81 (20.7) | 75 (29.5) | 28 (29.2) | 16 (43.2) | 0.007 |
| Concerned that must get up in the middle of the night to urinate | 85 (21.7) | 99 (39.0) | 55 (57.3) | 20 (54.1) | <0.001 |
| Worried that the condition of night urination will get worse | 73 (18.7) | 81 (31.9) | 38 (39.6) | 21 (56.8) | <0.001 |
| Worried that there is no effective treatment for the condition of night urination | 59 (15.1) | 73 (28.7) | 37 (38.5) | 17 (46.0) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yuen, J.W.-M.; Wong, I.Y.-P.; Chiu, P.K.-F.; Teoh, J.Y.-C.; Chan, C.-K.; Yee, C.-H.; Ng, C.-F. A Comprehensive Community-Based Prevalence Study on Nocturia in Hong Kong Male Adults. Int. J. Environ. Res. Public Health 2021, 18, 9112. https://doi.org/10.3390/ijerph18179112
Yuen JW-M, Wong IY-P, Chiu PK-F, Teoh JY-C, Chan C-K, Yee C-H, Ng C-F. A Comprehensive Community-Based Prevalence Study on Nocturia in Hong Kong Male Adults. International Journal of Environmental Research and Public Health. 2021; 18(17):9112. https://doi.org/10.3390/ijerph18179112
Chicago/Turabian StyleYuen, John Wai-Man, Ivy Yuen-Ping Wong, Peter Ka-Fung Chiu, Jeremy Yuen-Chun Teoh, Chi-Kwok Chan, Chi-Hang Yee, and Chi-Fai Ng. 2021. "A Comprehensive Community-Based Prevalence Study on Nocturia in Hong Kong Male Adults" International Journal of Environmental Research and Public Health 18, no. 17: 9112. https://doi.org/10.3390/ijerph18179112
APA StyleYuen, J. W.-M., Wong, I. Y.-P., Chiu, P. K.-F., Teoh, J. Y.-C., Chan, C.-K., Yee, C.-H., & Ng, C.-F. (2021). A Comprehensive Community-Based Prevalence Study on Nocturia in Hong Kong Male Adults. International Journal of Environmental Research and Public Health, 18(17), 9112. https://doi.org/10.3390/ijerph18179112







