Mental Health during COVID-19 Pandemic among Caregivers of Young Children in Kenya’s Urban Informal Settlements. A Cross-Sectional Telephone Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Data Sources
2.2. Study Setting
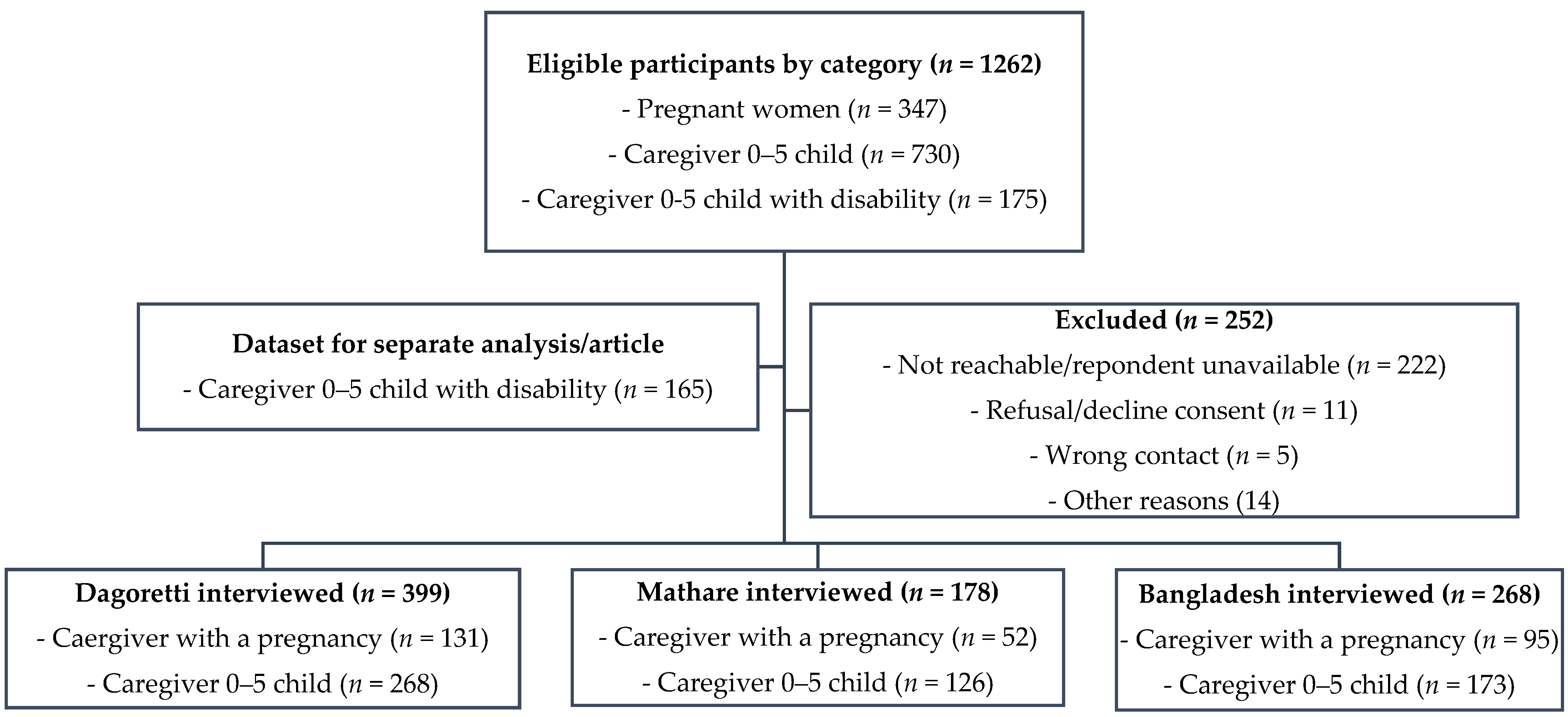
2.3. Participants and Procedures
2.4. Measures and Data Collection Procedures
2.5. Statistical Analysis
3. Results
3.1. Socio-Demographic Characteristics and Mental Health Status
3.2. COVID-19-Related Consequences on Psychosocial Aspects
3.3. Correlates of Mental Health Outcomes
3.3.1. Univariate Analysis
3.3.2. Multivariate Analysis
4. Discussion
4.1. Key Findings
4.2. Implication of Findings and Proposed Recommendations
4.3. Methodological Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
List of Abbreviations
| AdjOR | Adjusted Odds Ratio |
| CAS | COVID-19 Anxiety Scale |
| CHVs | Community Health Volunteers |
| CI | Confidence Interval |
| COVID-19 | Coronavirus–19 |
| GAD | General Anxiety Disorder |
| LMICs | Low-and Middle-Income Countries |
| ODK | Open Data Kit |
| OR | Odds Ratio |
| PHQ | Patient Health Questionnaire |
| PPE | Personal Protective Equipment |
| SD | Standard Deviation |
| UnadjOR | Unadjusted Odds Ratio |
| WHO | World Health Organization |
References
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- World Health Organisation. WHO Corona Virus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 12 March 2021).
- World Health Organisation. WHO COVID-19 Prepardness and Progress Report (February–June 2020); World Health Organisation: Geneva, Switzerland, 2020. [Google Scholar]
- Kola, L.; Kohrt, B.A.; Hanlon, C.; Naslund, J.A.; Sikander, S.; Balaji, M.; Benjet, C.; Cheung, E.Y.L.; Eaton, J.; Gonsalves, P. COVID-19 mental health impact and responses in low-income and middle-income countries: Reimagining global mental health. Lancet Psychiatry 2021, 8, 535–550. [Google Scholar] [CrossRef]
- Semo, B.-W.; Frissa, S.M. The mental health impact of the COVID-19 pandemic: Implications for sub-Saharan Africa. Psychol. Res. Behav. Manag. 2020, 13, 713. [Google Scholar] [CrossRef] [PubMed]
- Fiorillo, A.; Gorwood, P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry 2020, 63, e32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tyrer, P. COVID-19 health anxiety. World Psychiatry 2020, 19, 307. [Google Scholar] [CrossRef] [PubMed]
- Banna, M.H.A.; Sayeed, A.; Kundu, S.; Christopher, E.; Hasan, M.T.; Begum, M.R.; Kormoker, T.; Dola, S.T.I.; Hassan, M.M.; Chowdhury, S. The impact of the COVID-19 pandemic on the mental health of the adult population in Bangladesh: A nationwide cross-sectional study. Int. J. Environ. Health Res. 2020, 1–12. [Google Scholar] [CrossRef]
- Otu, A.; Charles, C.H.; Yaya, S. Mental health and psychosocial well-being during the COVID-19 pandemic: The invisible elephant in the room. Int. J. Ment. Health Syst. 2020, 14, 1–5. [Google Scholar] [CrossRef]
- Ghebreyesus, T.A. Addressing mental health needs: An integral part of COVID-19 response. World Psychiatry 2020, 19, 129. [Google Scholar] [CrossRef]
- Kibe, P.M.; Kisia, L.; Bakibinga, P. COVID-19 and community healthcare: Perspectives from Nairobi’s informal settlements. Pan Afr. Med. J. 2020, 35, 106. [Google Scholar] [CrossRef]
- Quaife, M.; Van Zandvoort, K.; Gimma, A.; Shah, K.; McCreesh, N.; Prem, K.; Barasa, E.; Mwanga, D.; Kangwana, B.; Pinchoff, J. The impact of COVID-19 control measures on social contacts and transmission in Kenyan informal settlements. BMC Med. 2020, 18, 316. [Google Scholar] [CrossRef]
- Chandra, P.S.; Nanjundaswamy, M.H. Pregnancy specific anxiety: An under-recognized problem. World Psychiatry 2020, 19, 336. [Google Scholar] [CrossRef]
- Shorey, S.Y.; Ng, E.D.; Chee, C.Y. Anxiety and depressive symptoms of women in the perinatal period during the COVID-19 pandemic: A systematic review and meta-analysis. Scand. J. Public Health 2021, 14034948211011793. [Google Scholar] [CrossRef]
- Brown, S. Perinatal mental health and the COVID-19 pandemic. World Psychiatry 2020, 19, 333. [Google Scholar] [CrossRef] [PubMed]
- Kotlar, B.; Gerson, E.; Petrillo, S.; Langer, A.; Tiemeier, H. The impact of the COVID-19 pandemic on maternal and perinatal health: A scoping review. Reprod. Health 2021, 18, 10. [Google Scholar] [CrossRef] [PubMed]
- Austin, M.-P. Psychosocial assessment and management of depression and anxiety in pregnancy. Key aspects of antenatal care for general practice. Aust. Fam. Physician 2003, 32, 119–120, 122–126. [Google Scholar]
- Howard, L.M.; Khalifeh, H. Perinatal mental health: A review of progress and challenges. World Psychiatry 2020, 19, 313–327. [Google Scholar] [CrossRef]
- Creswell, J.W. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches; Sage Publications: Thousand Oaks, CA, USA, 2014. [Google Scholar]
- United Nations Human Settlements Programme. Habitat III Issue Papers 22—Informal Settlements. Available online: https://uploads.habitat3.org/hb3/Habitat-III-Issue-Paper-22_Informal-Settlements-2.0.pdf (accessed on 17 August 2021).
- Kostelny, K.; Wessells, M.; Chabeda-Barthe, J.; Ondoro, K. Learning about Children in Urban Slums: A Rapid Ethnographic Study in Two Urban Slums in Mombasa of Community Based Child Protection Mechanisms and Their Linkage with the Kenyan National Child Protection System. N. Y. Columbia Group Child. Advers. 2013, 1–144. Available online: http://www.cpcnetwork.org/wp-content/uploads/2015/03/6.-Kenya-CBCPM-in-Mombasa-2013.pdf (accessed on 5 May 2021).
- Kenya National Bureau of Statistics. Kenya Population and Housing Census Volume I: Population by County and Sub-County; Kenya National Bureau of Statistics: Nairobi, Kenya, 2019. [Google Scholar]
- Kamau, N.; Njiru, H. Water, Sanitation and Hygiene Situation in Kenya’s Urban Slums. J. Health Care Poor Underserved 2018, 29, 321–336. [Google Scholar] [CrossRef] [Green Version]
- Abubakar, A.; Angwenyi, V.; Kabue, M.; Zhang, L.; AKU-AHD Research Group. Parenting programme in an informal settlement in Nairobi, Kenya: Priority needs and identification of delivery platforms. Int. J. Birth Parent Educ. 2019, 6, 11–14. [Google Scholar]
- Mwangi, P.; Nyongesa, M.K.; Koot, H.M.; Cuijpers, P.; Newton, C.R.; Abubakar, A. Validation of a Swahili version of the 9-item Patient Health Questionnaire (PHQ-9) among adults living with HIV compared to a community sample from Kilifi, Kenya. J. Affect. Disord. Rep. 2020, 1, 100013. [Google Scholar] [CrossRef]
- Nyongesa, M.K.; Mwangi, P.; Koot, H.M.; Cuijpers, P.; Newton, C.R.; Abubakar, A. The reliability, validity and factorial structure of the Swahili version of the 7-item generalized anxiety disorder scale (GAD-7) among adults living with HIV from Kilifi, Kenya. Ann. Gen. Psychiatry 2020, 19, 62. [Google Scholar] [CrossRef]
- Lee, S.A. Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety. Death Stud. 2020, 44, 393–401. [Google Scholar] [CrossRef]
- Silva, W.A.D.; de Sampaio Brito, T.R.; Pereira, C.R. COVID-19 anxiety scale (CAS): Development and psychometric properties. Curr. Psychol. 2020, 1–10. [Google Scholar] [CrossRef]
- Ahmed, O.; Faisal, R.A.; Sharker, T.; Lee, S.A.; Jobe, M.C. Adaptation of the Bangla version of the COVID-19 Anxiety Scale. Int. J. Ment. Health Addict. 2020, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Bellows, N.; Weinberger, M.; Reidy, M. Using the Demographic Health Survey wealth index to create family planning market segments based on absolute income levels. BMJ Glob. Health 2020, 5, e002450. [Google Scholar] [CrossRef] [PubMed]
- Kenya National Bureau of Statistics. Kenya Demographic and Health Survey 2014; Institute for Resource Development/Westinghouse: Nairobi, Kenya, 2015. [Google Scholar]
- World Bank. Kenya Economic Update: Navigating the Pandemic. Available online: http://documents1.worldbank.org/curated/en/957121606226133134/pdf/Kenya-Economic-Update-Navigating-the-Pandemic.pdf (accessed on 12 April 2021).
- Nyadera, I.N.; Onditi, F. COVID-19 experience among slum dwellers in Nairobi: A double tragedy or useful lesson for public health reforms? Int. Soc. Work. 2020, 63, 838–841. [Google Scholar] [CrossRef]
- Pinchoff, J.; Austrian, K.; Rajshekhar, N.; Abuya, T.; Kangwana, B.; Ochako, R.; Tidwell, J.B.; Mwanga, D.; Muluve, E.; Mbushi, F. Gendered economic, social and health effects of the COVID-19 pandemic and mitigation policies in Kenya: Evidence from a prospective cohort survey in Nairobi informal settlements. BMJ Open 2021, 11, e042749. [Google Scholar] [CrossRef]
- Corburn, J.; Vlahov, D.; Mberu, B.; Riley, L.; Caiaffa, W.T.; Rashid, S.F.; Ko, A.; Patel, S.; Jukur, S.; Martínez-Herrera, E. Slum health: Arresting COVID-19 and improving well-being in urban informal settlements. J. Urban Health 2020, 97, 348–357. [Google Scholar] [CrossRef] [Green Version]
- Mamun, M.A.; Sakib, N.; Gozal, D.; Bhuiyan, A.I.; Hossain, S.; Bodrud-Doza, M.; Al Mamun, F.; Hosen, I.; Safiq, M.B.; Abdullah, A.H. The COVID-19 pandemic and serious psychological consequences in Bangladesh: A population-based nationwide study. J. Affect. Disord. 2021, 279, 462–472. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.W.; Nyengerai, T.; Mendenhall, E. Evaluating the mental health impacts of the COVID-19 pandemic in urban South Africa: Perceived risk of COVID-19 infection and childhood trauma predict adult depressive symptoms. Psychol. Med. 2020, 1–13. [Google Scholar] [CrossRef]
- Winter, S.C.; Obara, L.M.; McMahon, S. Intimate partner violence: A key correlate of women’s physical and mental health in informal settlements in Nairobi, Kenya. PLoS ONE 2020, 15, e0230894. [Google Scholar] [CrossRef]
- Lambert, J.E.; Denckla, C. Posttraumatic stress and depression among women in Kenya’s informal settlements: Risk and protective factors. Eur. J. Psychotraumatology 2021, 12, 1865671. [Google Scholar] [CrossRef]
- Laurenzi, C.A.; Hunt, X.; Skeen, S.; Sundin, P.; Weiss, R.E.; Kosi, V.; Rotheram-Borus, M.J.; Tomlinson, M. Associations between caregiver mental health and young children’s behaviour in a rural Kenyan sample. Glob. Health Action 2021, 14, 1861909. [Google Scholar] [CrossRef]
- Russell, B.; Hutchison, M.; Tambling, R.; Tomkunas, A.; Horton, A. Initial challenges of caregiving during COVID-19: Caregiver burden, mental health, and the parent–child relationship. Child Psychiatry Hum. Dev. 2020, 51, 671–682. [Google Scholar] [CrossRef]
- Zhang, S.; Dang, R.; Yang, N.; Bai, Y.; Wang, L.; Abbey, C.; Rozelle, S. Effect of Caregiver’s mental health on early childhood development across different rural communities in China. Int. J. Environ. Res. Public Health 2018, 15, 2341. [Google Scholar] [CrossRef] [Green Version]
- Shumba, C.; Maina, R.; Mbuthia, G.; Kimani, R.; Mbugua, S.; Shah, S.; Abubakar, A.; Luchters, S.; Shaibu, S.; Ndirangu, E. Reorienting Nurturing Care for Early Childhood Development during the COVID-19 Pandemic in Kenya: A Review. Int. J. Environ. Res. Public Health 2020, 17, 7028. [Google Scholar] [CrossRef] [PubMed]
- Kimani, R.W.; Maina, R.; Shumba, C.; Shaibu, S. Maternal and newborn care during the COVID-19 pandemic in Kenya: Re-contextualising the community midwifery model. Hum. Resour. Health 2020, 18, 75. [Google Scholar] [CrossRef]
- Oluoch-Aridi, J.; Chelagat, T.; Nyikuri, M.M.; Onyango, J.; Guzman, D.; Makanga, C.; Miller-Graff, L.; Dowd, R. COVID-19 Effect on access to maternal health services in Kenya. Front. Glob. Women’s Health 2020, 1, 19. [Google Scholar]
- Jaguga, F.; Kwobah, E. Mental health response to the COVID-19 pandemic in Kenya: A review. Int. J. Ment. Health Syst. 2020, 14, 68. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health Kenya. A Comprehensive Guide on Mental Health & Psychosocial Support during the COVID-19 Pandemic. Available online: https://www.health.go.ke/wp-content/uploads/2020/05/GUIDE-ON-MENTAL-HEALTH-AND-PSYCHOSOCIAL-SUPPORT-DURING-THE-COVID-19-PANDEMIC-compressed.pdf (accessed on 18 March 2021).
- Ministry of Health Kenya. Interim Guidance on Mental Health Services During the COVID-19 Pandemic; Ministry of Health Kenya: Nairobi, Kenya, 2020; Available online: https://www.health.go.ke/wp-content/uploads/2020/05/INTERIM-GUIDANCE-ON-CONTINUITY-OF-MENTAL-HEALTH-SERVICES-DURING-THE-COVID-19-PANDEMIC_compressed-2.pdf (accessed on 12 March 2021).
- Ahmed, S.A.S.; Ajisola, M.; Azeem, K.; Bakibinga, P.; Chen, Y.-F.; Choudhury, N.N.; Fayehun, O.; Griffiths, F.; Harris, B.; Kibe, P. Impact of the societal response to COVID-19 on access to healthcare for non-COVID-19 health issues in slum communities of Bangladesh, Kenya, Nigeria and Pakistan: Results of pre-COVID and COVID-19 lockdown stakeholder engagements. BMJ Glob. Health 2020, 5, e003042. [Google Scholar] [CrossRef] [PubMed]
- Hussein, S.; Otiso, L.; Kimani, M.; Olago, A.; Wanyungu, J.; Kavoo, D.; Njiraini, R.; Kimanzi, S.; Karuga, R. Institutionalizing community health services in Kenya: A policy and practice journey. Glob. Health Sci. Pract. 2021, 9, S25–S31. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | All Participants | PHQ-9 | CAS (COVID-19 Anxiety Scale) | GAD-7 (General Anxiety Disorder) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | p-Value | No | Yes | p-Value | No | Yes | p-Value | ||
| Age (years) mean (SD) | 29.00 (7.15) | |||||||||
| <30 | 516 (61.07) | 351 (63.02) | 165 (57.29) | 0.106 | 446 (61.35) | 70 (59.32) | 0.675 | 418 (61.65) | 98 (58.68) | 0.481 |
| 30 and above | 329 (38.93) | 206 (36.98) | 123 (42.71) | 281 (38.65) | 48(40.68) | 260 (38.35) | 69 (41.32) | |||
| Gender | ||||||||||
| Female | 801 (94.79) | 531 (95.33) | 270 (93.75) | 0.326 | 686 (94.36) | 115 (97.46) | 0.160 | 645 (95.13) | 156 (93.41) | 0.370 |
| Male | 44 (5.21) | 26 (4.67) | 18 (6.25) | 41 (5.64) | 3 (2.54) | 33 (4.87) | 11 (6.59) | |||
| Marital status | ||||||||||
| Married or cohabiting | 597 (71.17) | 406 (73.15) | 191 (67.25) | 0.012 | 511 (70.68) | 86 (74.14) | 0.604 | 482 (71.30) | 115 (70.55) | 0.187 |
| Single | 119 (14.18) | 82 (14.77) | 37 (13.03) | 106 (14.66) | 13 (11.21) | 101 (14.94) | 18 (11.04) | |||
| Separated/Divorced/Widowed | 123 (14.66) | 67 (12.07) | 56 (16.72) | 106 (14.66) | 17 (14.66) | 93 (13.76) | 30 (18.40) | |||
| Education level | ||||||||||
| Primary school and below | 376 (44.50) | 233 (41.83) | 143 (49.65) | 0.086 | 315 (43.33) | 61 (51.69) | 0.098 | 301 (44.40) | 75 (44.91) | 0.975 |
| Secondary School | 379 (44.85) | 260 (46.68) | 119 (41.32) | 329 (45.25) | 50 (42.37) | 304 (44.84) | 75 (44.91) | |||
| Tertiary | 90 (10.65) | 64 (11.49) | 26 (9.03) | 83 (11.42) | 7 (5.93) | 73 (10.77) | 17 (10.18) | |||
| Occupation | ||||||||||
| Formal | 42 (4.97) | 30 (5.39) | 12 (4.17) | 0.32 | 40 (5.50) | 2 (1.69) | 0.08 | 30 (4.42) | 12 (7.19) | 0.32 |
| Informal | 388 (45.92) | 246 (44.17) | 142 (49.31) | 325 (44.70) | 63 (53.39) | 311 (45.87) | 77 (46.11) | |||
| Unemployed | 415 (49.11) | 281 (50.45) | 134 (46.53) | 362 (49.79) | 53 (443.92) | 337 (49.710 | 78 (46.71) | |||
| Household asset index | ||||||||||
| Mean (SD) | (2.52) 1.19 | 2.65 (1.23) | 2.26 (1.07) | <0.001 | 2.55 (1.22) | 2.30 (1.02) | 0.030 | 2.56 (1.21) | 2.35 (1.09) | 0.047 |
| Survey site | ||||||||||
| Dagoretti | 396 (47.26) | 284 (51.45) | 112 (39.16) | <0.001 | 358 (49.72) | 38 (32.20) | <0.001 | 327 (48.59) | 69 (41.82) | 0.006 |
| Mathare | 177 (21.12) | 122 (22.10) | 55 (19.23) | 159 (22.08) | 18 (15.25) | 150 (22.29) | 27 (16.36) | |||
| Bangladesh | 265 (31.62) | 146 (26.45) | 119 (41.61) | 203 (28.19) | 62 (52.54) | 196 (29.12) | 69 (41.82) | |||
| Pregnancy | ||||||||||
| Not pregnant | 567 (67.10) | 384 (68.94) | 183 (63.54) | 0.113 | 489 (67.26) | 78 (66.10) | 0.803 | 453 (66.81) | 114 (68.26) | 0.721 |
| Pregnant | 278 (32.90) | 173 (31.06) | 105 (36.46) | 238 (32.74) | 40 (33.90) | 225 (33.19) | 53 (31.74) | |||
| Number of children + | ||||||||||
| 0–3 | 623 (79.97) | 406 (79.92) | 217 (80.07) | 0.960 | 536 (80.72) | 87 (75.65) | 0.210 | 506 (81.48) | 117 (74.05) | 0.037 |
| >3 | 156 (20.03) | 102 (20.08) | 54 (19.93) | 128 (19.28) | 28 (24.35) | 115 (18.52) | 41 (25.95) | |||
| Characteristics | All Participants | PHQ-9 | CAS (COVID-19 Anxiety Scale) | GAD-7 (General Anxiety Disorder) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | p-Value | No | Yes | p-Value | No | Yes | p-Value | ||
| Experienced violence (COVID period) | ||||||||||
| Yes | 107 (12.66) | 47 (8.44) | 60 (20.83) | <0.001 | 82 (11.28) | 25 (21.19) | 0.003 | 73 (10.77) | 34 (20.36) | 0.001 |
| No | 738 (87.34) | 510 (91.56) | 228 (79.17) | 645 (88.72) | 93 (78.81) | 605 (89.23) | 133 (79.64) | |||
| COVID-19 perceived as a serious threat | ||||||||||
| No | 46 (5.46) | 36 (6.47) | 10 (3.48) | 0.070 | 45 (6.20) | 1 (0.58) | 0.018 | 43 (6.35) | 3 (1.81) | 0.021 |
| Yes | 797 (94.54) | 520 (93.53) | 277 (96.52) | 681 (93.80) | 116 (99.15) | 634 (93.65) | 163 (98.19) | |||
| Experienced discrimination (COVID period) | ||||||||||
| Yes | 129 (15.27) | 57 (10.23) | 72 (25.00) | <0.001 | 96 (13.20) | 33 (27.97) | <0.001 | 79 (11.65) | 50 (29.94) | <0.001 |
| No | 716 (84.73) | 500 (89.77) | 216 (75.00) | 631 (86.80) | 85 (72.03) | 599 (88.35) | 117 (70.06) | |||
| Experienced job loss (COVID period) | ||||||||||
| No or to a less extent | 133 (17.69) | 114 (23.41) | 19 (7.17) | <0.001 | 123 (19.19) | 10 (9.01) | 0.009 | 115 (19.20) | 18 (11.76) | 0.031 |
| Very much | 619 (82.31) | 373 (76.59) | 246 (92.83) | 518 (80.81) | 101 (90.99) | 484 (80.80) | 135 (88.24) | |||
| Loss of income generation (COVID period) | ||||||||||
| No | 129 (18.38) | 102 (22.27) | 27 (11.01) | <0.001 | 118 (19.80) | 11 (10.38) | 0.021 | 112 (20.04) | 17 (11.89) | 0.025 |
| Yes | 573 (81.62) | 356 (77.73) | 217 (88.93) | 478 (80.20) | 95 (89.62) | 447 (79.96) | 126 (88.11) | |||
| Ability to pay utilities affected (COVID period) | ||||||||||
| Not affected or affected to a less extent | 135 (16.13) | 92 (16.70) | 43 (15.03) | 0.535 | 111 (15.42) | 24 (20.51) | 0.165 | 107 (15.97) | 28 (16.77) | 0.802 |
| Very much affected | 702 (83.87) | 459 (83.30) | 243 (84.97) | 609 (84.58) | 93 (79.49) | 563 (84.03) | 139 (83.23) | |||
| Ability to repay loans affected (COVID period) | ||||||||||
| Not affected or affected to a less extent | 158 (22.77) | 99 (22.86) | 59 (22.61) | 0.937 | 131 (22.32) | 27 (25.23) | 0.508 | 124 (22.42) | 34 (24.11) | 0.669 |
| Very much affected | 536 (77.23) | 334 (77.14) | 202 (77.39) | 456 (77.68) | 80 (74.77) | 429 (77.58) | 107 (75.89) | |||
| Ability to meet basic childcare affected (COVID period) | ||||||||||
| Not affected or affected to a less extent | 218 (27.39) | 166 (31.98) | 52 (18.77) | <0.001 | 193 (28.34) | 25 (21.74) | 0.142 | 188 (29.51) | 30 (18.87) | 0.007 |
| Very much affected | 578 (72.61) | 353 (68.02) | 225 (81.23) | 488 (71.66) | 90 (78.26) | 449 (70.49) | 129 (81.13) | |||
| Interaction outside households affected (COVID period) | ||||||||||
| Not affected or affected to a less extent | 364 (43.23) | 258 (46.40) | 106 (37.06) | 0.010 | 326 (44.97) | 38 (32.48) | 0.011 | 307 (45.41) | 57 (34.34) | 0.010 |
| Very much affected | 478 (56.77) | 298 (53.60) | 180 (62.94) | 399 (55.03) | 79 (67.52) | 369 (54.59) | 109 (65.66) | |||
| Family interactions affected (COVID period) | ||||||||||
| Not affected or affected to a less extent | 290 (34.44) | 212 (38.20) | 78 (27.18) | 0.001 | 259 (35.77) | 31 (26.27) | 0.044 | 248 (36.74) | 42 (25.15) | 0.005 |
| Very much affected | 552 (65.56) | 343 (61.80) | 209 (72.82) | 465 (64.23) | 87 (73.73) | 427 (63.26) | 125 (74.85) | |||
| Characteristics | PHQ-9 | CAS | GAD-7 | |||
|---|---|---|---|---|---|---|
| Odds Ratio (95% CI) | p-Value | Odds Ratio (95% CI) | p-Value | Odds Ratio (95% CI) | p-Value | |
| Age | ||||||
| <30 | 1 | 1 | 1 | |||
| 30 and above | 1.15 (0.78–1.68) | 0.487 | 0.80 (0.49–1.30) | 0.360 | 0.77 (0.48–1.25) | 0.291 |
| Sex | ||||||
| Female | 1 | 1 | 1 | |||
| Male | 1.18 (0.52–2.67) | 0.686 | 0.44 (0.12–1.57) | 0.205 | 1.37 (0.57–3.25) | 0.482 |
| Marital status | ||||||
| Married or cohabiting | 1 | 1 | 1 | |||
| Single | 1.56 (0.88–2.76) | 0.130 | 1.41 (0.70–2.86) | 0.342 | 1.58 (0.82–3.04) | 0.167 |
| Separated/Divorced/Widowed | 0.98 (0.57–1.71) | 0.956 | 0.51 (0.24–1.08) | 0.078 | 0.83 (0.44–1.55) | 0.558 |
| Education Level | ||||||
| Tertiary | 1 | 1 | ||||
| Primary and below | 1.39 (0.70–2.72) | 0.345 | 2.79 (1.06–7.36) | 0.038 | 0.99 (0.46–2.12) | 0.984 |
| Secondary School | 1.22 (0.63–2.37) | 0.563 | 2.24 (0.85–5.93) | 0.103 | 1.02 (0.49–2.15) | 0.952 |
| Occupation | ||||||
| Unemployed | 1 | 1 | 1 | |||
| Formal | 1.34 (0.58–3.12) | 0.491 | 0.56 (0.12–2.58) | 0.460 | 2.84 (1.21–6.63) | 0.016 |
| Informal | 1.04 (0.70–1.54) | 0.847 | 1.26 (0.78–2.05) | 0.347 | 0.93 (0.59–1.49) | 0.776 |
| Pregnancy | ||||||
| Not pregnant | 1 | 1 | 1 | |||
| Pregnant | 1.44 (0.96–2.16) | 0.074 | 0.98 (0.59–1.63) | 0.939 | 1.04 (0.63–1.69) | 0.890 |
| No. of children | ||||||
| 0–3 | 1 | 1 | 1 | |||
| >3 | 1.02 (0.61–1.68) | 0.948 | 1.27 (0.72–2.25) | 0.402 | 1.55 (0.93–2.57) | 0.090 |
| Experienced violence(COVID period) | ||||||
| No | 1 | 1 | 1 | |||
| Yes | 1.89 (1.12–3.18)) | 0.016 | 1.83 (1.01–3.32) | 0.048 | 1.80 (1.03–3.13) | 0.037 |
| Perceived COVID-19 as a serious threat | ||||||
| No | 1 | 1 | 1 | |||
| Yes | 0.77 (0.31–1.88) | 0.561 | 3.79 (0.49–29.43) | 0.203 | 2.27 (0.51–10.10) | 0.282 |
| Experienced discrimination(COVID period) | ||||||
| No | 1 | 1 | 1 | |||
| Yes | 3.12 (1.91–5.10) | <0.001 | 2.35 (1.35–4.09) | 0.002 | 3.62 (2.19–5.98) | <0.001 |
| Experienced job loss(COVID period) | ||||||
| Not affected or affected to a less extent | 1 | 1 | 1 | |||
| Very much affected | 2.88 (1.51–5.48) | 0.001 | 1.60 (0.69–3.70) | 0.272 | 1.17 (0.58–2.39) | 0.661 |
| Loss of income generation(COVID period) | ||||||
| No | 1 | 1 | 1 | |||
| Yes | 1.19 (0.68–2.15) | 0.564 | 1.50 (0.67–3.38) | 0.325 | 1.26 (0.63–2.53) | 0.519 |
| Ability to pay utilities affected(COVID period) | ||||||
| Not affected or affected to a less extent | 1 | 1 | 1 | |||
| Very much affected | 0.45 (0.22–0.91) | 0.026 | 0.31 (0.12–0.78) | 0.013 | 0.34 (0.14–0.82) | 0.016 |
| Ability to repay loans affected(COVID period) | ||||||
| Not affected or affected to a less extent | 1 | 1 | 1 | |||
| Very much affected | 0.64 (0.37–1.11) | 0.112 | 0.87 (0.40–1.87) | 0.721 | 0.48 (0.25–0.91) | 0.024 |
| Ability to meet basic childcare affected(COVID period) | ||||||
| Not affected or affected to a less extent | 1 | 1 | 1 | |||
| Very much affected | 1.41 (0.88–2.24) | 0.149 | 2.08 (0.87–4.98) | 0.101 | 1.58 (0.90–2.75) | 0.109 |
| Household asset index | 0.83 (0.69–0.99) | 0.041 | 1.02 (0.81–1.28) | 0.874 | 0.94 (0.76–1.16) | 0.562 |
| Movement outside household affected(COVID period) | ||||||
| Not affected or affected to a less extent | 1 | 1 | 1 | |||
| Very much affected | 1.50 (0.98–2.31) | 0.062 | 1.68 (0.96–2.93) | 0.070 | 1.38 (0.84–2.29) | 0.207 |
| Family interaction affected(COVID period) | ||||||
| Not affected or affected to a less extent | 1 | 1 | 1 | |||
| Very much affected | 1.16 (0.73–1.85) | 0.518 | 1.11 (0.61–2.01) | 0.739 | 1.17 (0.68–2.04) | 0.565 |
| Survey study site | ||||||
| Dagoretti | 1 | 1 | 1 | |||
| Mathare | 1.02 (0.61–1.72) | 0.934 | 1.11 (0.55–2.24) | 0.772 | 0.56 (0.28–1.11) | 0.098 |
| Bangladesh | 1.93 (1.26–2.98) | 0.003 | 2.12 (1.23–3.65) | 0.007 | 1.52 (0.93–2.48) | 0.093 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Angwenyi, V.; Kabue, M.; Chongwo, E.; Mabrouk, A.; Too, E.K.; Odhiambo, R.; Nasambu, C.; Marangu, J.; Ssewanyana, D.; Njoroge, E.; et al. Mental Health during COVID-19 Pandemic among Caregivers of Young Children in Kenya’s Urban Informal Settlements. A Cross-Sectional Telephone Survey. Int. J. Environ. Res. Public Health 2021, 18, 10092. https://doi.org/10.3390/ijerph181910092
Angwenyi V, Kabue M, Chongwo E, Mabrouk A, Too EK, Odhiambo R, Nasambu C, Marangu J, Ssewanyana D, Njoroge E, et al. Mental Health during COVID-19 Pandemic among Caregivers of Young Children in Kenya’s Urban Informal Settlements. A Cross-Sectional Telephone Survey. International Journal of Environmental Research and Public Health. 2021; 18(19):10092. https://doi.org/10.3390/ijerph181910092
Chicago/Turabian StyleAngwenyi, Vibian, Margaret Kabue, Esther Chongwo, Adam Mabrouk, Ezra Kipngetich Too, Rachel Odhiambo, Carophine Nasambu, Joyce Marangu, Derrick Ssewanyana, Eunice Njoroge, and et al. 2021. "Mental Health during COVID-19 Pandemic among Caregivers of Young Children in Kenya’s Urban Informal Settlements. A Cross-Sectional Telephone Survey" International Journal of Environmental Research and Public Health 18, no. 19: 10092. https://doi.org/10.3390/ijerph181910092
APA StyleAngwenyi, V., Kabue, M., Chongwo, E., Mabrouk, A., Too, E. K., Odhiambo, R., Nasambu, C., Marangu, J., Ssewanyana, D., Njoroge, E., Ombech, E., Mokaya, M. M., Obulemire, E. K., Khamis, A., & Abubakar, A. (2021). Mental Health during COVID-19 Pandemic among Caregivers of Young Children in Kenya’s Urban Informal Settlements. A Cross-Sectional Telephone Survey. International Journal of Environmental Research and Public Health, 18(19), 10092. https://doi.org/10.3390/ijerph181910092






