The Depression Anxiety Stress Scale 21: Development and Validation of the Depression Anxiety Stress Scale 8-Item in Psychiatric Patients and the General Public for Easier Mental Health Measurement in a Post COVID-19 World
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Participants, and Procedure
2.2. Study Instruments
2.3. Ethical Considerations
2.4. Statistical Analysis
3. Results
3.1. Participants’ Characteristics
3.2. Results of Exploratory Factor Analysis
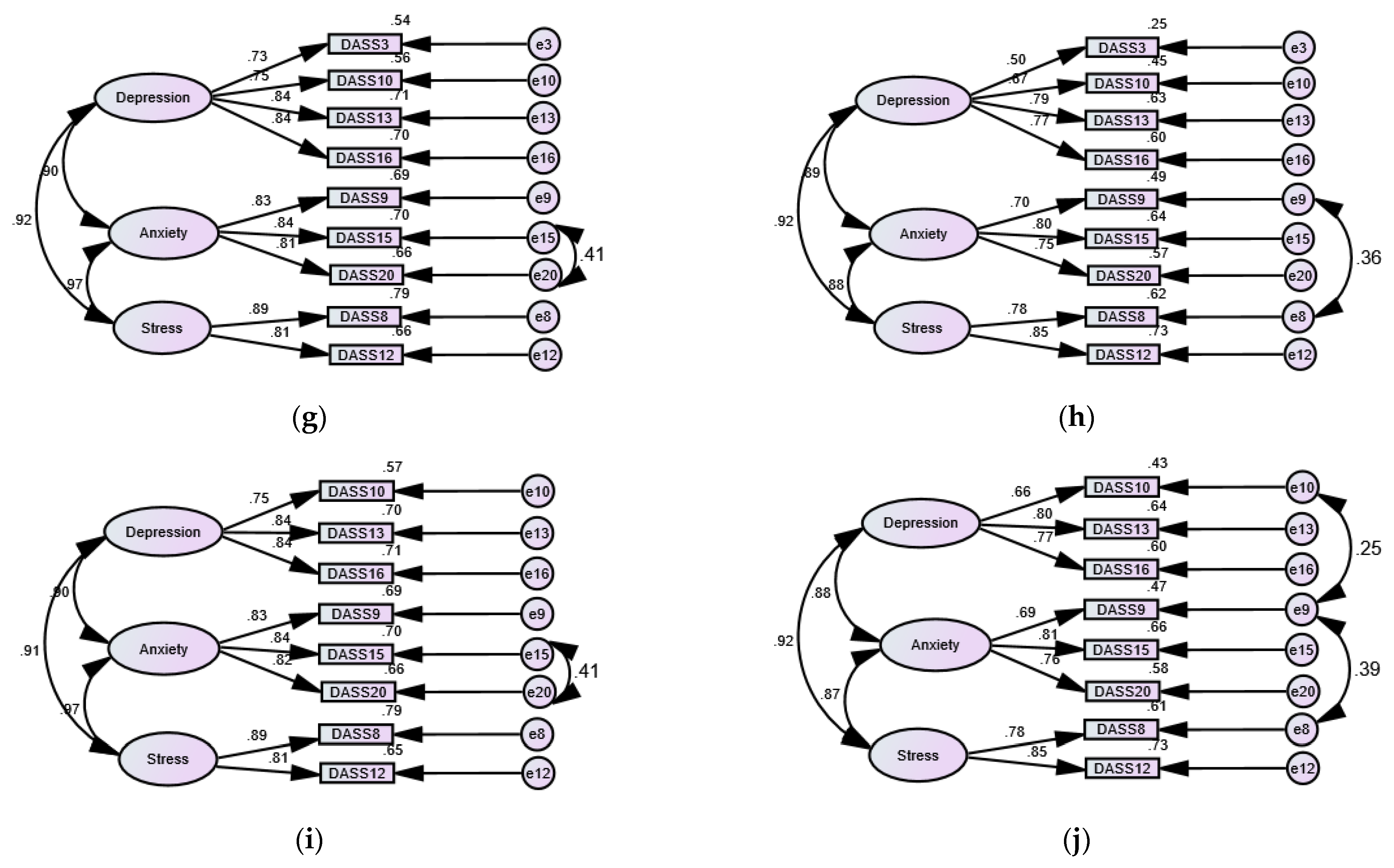
3.3. Results of Confirmatory Factor Analysis
3.4. Results of Invariance Analysis
3.5. Normality of the DASS-21 and Its Shortened Versions
3.6. Internal Consistency, Item Coverage, and Predictive Validity of Shortened Versions of the DASS-21
3.7. Discriminant Validity of the DASS-21 and Its Shortened Versions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kan, F.P.; Raoofi, S.; Rafiei, S.; Khani, S.; Hosseinifard, H.; Tajik, F.; Raoofi, N.; Ahmadi, S.; Aghalou, S.; Torabi, F.; et al. A systematic review of the prevalence of anxiety among the general population during the COVID-19 pandemic. J. Affect. Disord. 2021, 293, 391–398. [Google Scholar] [CrossRef]
- Lee, S.A. Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety. Death Stud. 2020, 44, 393–401. [Google Scholar] [CrossRef]
- Ali, A.M.; Hendawy, A.O.; Kunugi, H. The Internet Addiction Test: Its factor structure, measurement invariance, and psychometric properties of a six-item version among Spanish women with eating disorders. Res. Sq. 2021, 1. [Google Scholar] [CrossRef]
- Ali, A.M.; Kunugi, H. Corona Virus Disease 2019 (COVID-19): A pandemic that threatens physical and mental health by promoting physical inactivity. Sports Med. Health Sci. 2020, 2, 221–223. [Google Scholar] [CrossRef]
- Ali, A.M.; Kunugi, H. Apitherapy for age-related skeletal muscle dysfunction (sarcopenia): A review on the effects of royal jelly, propolis, and bee pollen. Foods 2020, 9, 1362. [Google Scholar] [CrossRef]
- Ali, A.M.; Kunugi, H. Approaches to nutritional screening in patients with Coronavirus Disease 2019 (COVID-19). Int. J. Environ. Res. Public Health 2021, 18, 2772. [Google Scholar] [CrossRef]
- Ali, A.M.; Ali, E.M.; Mousa, A.A.; Ahmed, M.E.; Hendawy, A.O. Bee honey and exercise for improving physical performance, reducing fatigue, and promoting an active lifestyle during COVID-19. Sports Med. Health Sci. 2021, 3, 177–180. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.M.; Kunugi, H. The effects of royal jelly acid, 10-hydroxy-trans-2-decenoic acid, on neuroinflammation and oxidative stress in astrocytes stimulated with lipopolysaccharide and hydrogen peroxide. Immuno 2021, 1, 13. [Google Scholar] [CrossRef]
- Ali, A.M.; Kunugi, H.; Abdelmageed, H.A.; Mandour, A.S.; Ahmed, M.E.; Ahmad, S.; Hendawy, A.O. Vitamin K in COVID-19—potential anti-covid-19 properties of fermented milk fortified with bee honey as a natural source of vitamin K and probiotics. Fermentation 2021, 7, 202. [Google Scholar]
- Ali, A.M.; Kunugi, H. Apitherapy for Parkinson’s disease: A focus on the effects of propolis and royal jelly. Oxid Med. Cell Longev. 2020, 2020, 1727142. [Google Scholar] [CrossRef]
- Ali, A.M.; Kunugi, H. Royal jelly as an intelligent anti-aging—a focus on cognitive aging and Alzheimer’s disease: A review. Antioxidants 2020, 9, 937. [Google Scholar] [CrossRef] [PubMed]
- Tran, T.D.; Tran, T.; Fisher, J. Validation of the depression anxiety stress scales (DASS) 21 as a screening instrument for depression and anxiety in a rural community-based cohort of northern Vietnamese women. BMC Psychiatry 2013, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ali, A.M.; Kunugi, H. Intermittent fasting, dietary modifications, and exercise for the control of gestational diabetes and maternal mood dysregulation: A review and a case report. Int. J. Environ. Res. Public Health 2020, 17, 9379. [Google Scholar] [CrossRef] [PubMed]
- Ter Meulen, W.G.; Draisma, S.; van Hemert, A.M.; Schoevers, R.A.; Kupka, R.W.; Beekman, A.T.F.; Penninx, B.W.J.H. Depressive and anxiety disorders in concert–A synthesis of findings on comorbidity in the NESDA study. J. Affect. Disord. 2021, 284, 85–97. [Google Scholar] [CrossRef]
- Ali, A.M.; Green, J. Factor structure of the depression anxiety stress Scale-21 (DASS-21): Unidimensionality of the Arabic version among Egyptian drug users. Subst. Abus. Treat. Prev. Policy 2019, 14, 40. [Google Scholar] [CrossRef]
- Janiri, D.; Moser, D.A.; Doucet, G.E.; Luber, M.J.; Rasgon, A.; Lee, W.H.; Murrough, J.W.; Sani, G.; Eickhoff, S.B.; Frangou, S. Shared Neural Phenotypes for Mood and Anxiety Disorders: A Meta-analysis of 226 Task-Related Functional Imaging Studies. JAMA Psychiatry 2020, 77, 172–179. [Google Scholar] [CrossRef] [Green Version]
- Dale, L.P.; Vanderloo, L.; Moore, S.; Faulkner, G. Physical activity and depression, anxiety, and self-esteem in children and youth: An umbrella systematic review. Mental. Health Physical. Act. 2019, 16, 66–79. [Google Scholar] [CrossRef]
- Racine, N.; McArthur, B.A.; Cooke, J.E.; Eirich, R.; Zhu, J.; Madigan, S. Global Prevalence of Depressive and Anxiety Symptoms in Children and Adolescents During COVID-19: A Meta-analysis. JAMA Pediatr. 2021. [Google Scholar] [CrossRef]
- Ma, L.; Mazidi, M.; Li, K.; Li, Y.; Chen, S.; Kirwan, R.; Zhou, H.; Yan, N.; Rahman, A.; Wang, W.; et al. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2021, 293, 78–89. [Google Scholar] [CrossRef]
- Narmandakh, A.; Roest, A.M.; de Jonge, P.; Oldehinkel, A.J. Psychosocial and biological risk factors of anxiety disorders in adolescents: A TRAILS report. Eur. Child. Adolesc. Psychiatry 2020. [Google Scholar] [CrossRef] [PubMed]
- Womersley, J.S.; Martin, L.; van der Merwe, L.; Seedat, S.; Hemmings, S.M.J. Genetic variation in neuropeptide Y interacts with childhood trauma to influence anxiety sensitivity. Anxiety Stress Coping 2021, 34, 450–464. [Google Scholar] [CrossRef]
- Wickersham, A.; Leightley, D.; Archer, M.; Fear, N.T. The association between paternal psychopathology and adolescent depression and anxiety: A systematic review. J. Adolesc. 2020, 79, 232–246. [Google Scholar] [CrossRef]
- Saraceno, L.; Munafó, M.; Heron, J.; Craddock, N.; van den Bree, M.B. Genetic and non-genetic influences on the development of co-occurring alcohol problem use and internalizing symptomatology in adolescence: A review. Addiction 2009, 104, 1100–1121. [Google Scholar] [CrossRef]
- Glynn, L.M.; Howland, M.A.; Fox, M. Maternal programming: Application of a developmental psychopathology perspective. Dev. Psychopathol. 2018, 30, 905–919. [Google Scholar] [CrossRef]
- Ali, A.M.; Hori, H.; Kim, Y.; Kunugi, H. Predictors of nutritional status, depression, internet addiction, Facebook addiction, and tobacco smoking among women with eating disorders in Spain. Front. Psychiatry 2021. under review. [Google Scholar]
- Weissman, M.M.; Warner, V.; Wickramaratne, P.J.; Kandel, D.B. Maternal smoking during pregnancy and psychopathology in offspring followed to adulthood. J. Am. Acad. Child. Adolesc. Psychiatry 1999, 38, 892–899. [Google Scholar] [CrossRef]
- Huizink, A.C.; de Rooij, S.R. Prenatal stress and models explaining risk for psychopathology revisited: Generic vulnerability and divergent pathways. Dev. Psychopathol. 2018, 30, 1041–1062. [Google Scholar] [CrossRef] [PubMed]
- Goodman, S.H.; Gotlib, I.H. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychol. Rev. 1999, 106, 458–490. [Google Scholar] [CrossRef] [PubMed]
- Nelson, C.A.; Scott, R.D.; Bhutta, Z.A.; Harris, N.B.; Danese, A.; Samara, M. Adversity in childhood is linked to mental and physical health throughout life. BMJ 2020, 371, m3048. [Google Scholar] [CrossRef] [PubMed]
- Rasing, S.P.A.; Braam, M.W.G.; Brunwasser, S.M.; Janssens, J.; Creemers, D.H.M.; Scholte, R.H.J. Depression and Anxiety Symptoms in Female Adolescents: Relations with Parental Psychopathology and Parenting Behavior. J. Res. Adolesc. 2020, 30, 298–313. [Google Scholar] [CrossRef]
- Hastings, P.D.; Ugarte, E.; Mashash, M.; Marceau, K.; Natsuaki, M.N.; Shirtcliff, E.A.; Zahn-Waxler, C.; Klimes-Dougan, B. The codevelopment of adolescents’ and parents’ anxiety and depression: Moderating influences of youth gender and psychophysiology. Depress. Anxiety 2021. [Google Scholar] [CrossRef]
- Lee, E.H.; Moon, S.H.; Cho, M.S.; Park, E.S.; Kim, S.Y.; Han, J.S.; Cheio, J.H. The 21-Item and 12-Item Versions of the Depression Anxiety Stress Scales: Psychometric Evaluation in a Korean Population. Asian. Nurs. Res. 2019, 13, 30–37. [Google Scholar] [CrossRef] [Green Version]
- Gurley, D.; Cohen, P.; Pine, D.S.; Brook, J. Discriminating depression and anxiety in youth: A role for diagnostic criteria. J. Affect. Disord. 1996, 39, 191–200. [Google Scholar] [CrossRef]
- Waszczuk, M.A.; Zavos, H.M.; Gregory, A.M.; Eley, T.C. The phenotypic and genetic structure of depression and anxiety disorder symptoms in childhood, adolescence, and young adulthood. JAMA Psychiatry 2014, 71, 905–916. [Google Scholar] [CrossRef]
- Watson, D.; Clark, L.A.; Weber, K.; Assenheimer, J.S.; Strauss, M.E.; McCormick, R.A. Testing a Tripartite Model: II. Exploring the Symptom Structure of Anxiety and Depression in Student, Adult, and Patient Sample. J. Abnorm. Psychol. 1995, 104, 15–25. [Google Scholar] [CrossRef]
- Zhang, F.; Rao, S.; Cao, H.; Zhang, X.; Wang, Q.; Xu, Y.; Sun, J.; Wang, C.; Chen, J.; Xu, X.; et al. Genetic evidence suggests posttraumatic stress disorder as a subtype of major depressive disorder. J. Clin. Investig. 2021. [Google Scholar] [CrossRef]
- Vaughan, R.S.; Edwards, E.J.; MacIntyre, T.E. Mental Health Measurement in a Post Covid-19 World: Psychometric Properties and Invariance of the DASS-21 in Athletes and Non-athletes. Front. Psychol. 2020, 11, 590559. [Google Scholar] [CrossRef]
- Bottesi, G.; Ghisi, M.; Altoè, G.; Conforti, E.; Melli, G.; Sica, C. The Italian version of the Depression Anxiety Stress Scales-21: Factor structure and psychometric properties on community and clinical samples. Compr. Psychiatry 2015, 60, 170–181. [Google Scholar] [CrossRef] [PubMed]
- Henry, J.D.; Crawford, J.R. The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2005, 44, 227–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yıldırım, A.; Boysan, M.; Kefeli, M.C. Psychometric properties of the Turkish version of the Depression Anxiety Stress Scale-21 (DASS-21). Br. J. Guid. Couns. 2018, 46, 1–14. [Google Scholar] [CrossRef]
- Silva, H.A.; Passos, M.H.; Oliveira, V.M.; Palmeira, A.C.; Pitangui, A.C.; Araújo, R.C. Short version of the Depression Anxiety Stress Scale-21: Is it valid for Brazilian adolescents? Einstein 2016, 14, 486–493. [Google Scholar] [CrossRef] [Green Version]
- Zanon, C.; Brenner, R.E.; Baptista, M.N.; Vogel, D.L.; Rubin, M.; Al-Darmaki, F.R.; Gonçalves, M.; Heath, P.J.; Liao, H.Y.; Mackenzie, C.S.; et al. Examining the Dimensionality, Reliability, and Invariance of the Depression, Anxiety, and Stress Scale-21 (DASS-21) Across Eight Countries. Assessment 2020, 28, 1531–1544. [Google Scholar] [CrossRef] [PubMed]
- Camacho, Á.; Cordero, E.D.; Perkins, T. Psychometric Properties of the DASS-21 Among Latina/o College Students by the US-Mexico Border. J. Immigr. Minor Health 2016, 18, 1017–1023. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.M.; Ahmed, A.; Sharaf, A.; Kawakami, N.; Abdeldayem, S.M.; Green, J. The Arabic Version of The Depression Anxiety Stress Scale-21: Cumulative scaling and discriminant-validation testing. Asian J. Psychiatr. 2017, 30, 56–58. [Google Scholar] [CrossRef] [PubMed]
- Teo, Y.C.; Hj Yusuf, A.; Alice Lim, W.P.; Ghazali, N.B.; Abd Rahman, H.; Lin, N.; Koh, D. Validation of DASS-21 among nursing and midwifery students in Brunei. J. Public Health 2019, 27, 387–391. [Google Scholar] [CrossRef]
- Patrick, J.; Dyck, M.; Bramston, P. Depression anxiety stress scale (DASS): Is it valid for children and adolescents? J. Clin. Psychol. 2010, 66, 996–1007. [Google Scholar] [CrossRef] [Green Version]
- Jafari, P.; Nozari, F.; Ahrari, F.; Bagheri, Z. Measurement invariance of the Depression Anxiety Stress Scales-21 across medical student genders. Int. J. Med. Educ. 2017, 8, 116–122. [Google Scholar] [CrossRef] [Green Version]
- Scholten, S.; Velten, J.; Bieda, A.; Zhang, X.C.; Margraf, J. Testing measurement invariance of the Depression, Anxiety, and Stress Scales (DASS-21) across four countries. Psychol. Assess. 2017, 29, 1376–1390. [Google Scholar] [CrossRef]
- Bibi, A.; Lin, M.; Zhang, X.C.; Margraf, J. Psychometric properties and measurement invariance of Depression, Anxiety and Stress Scales (DASS-21) across cultures. Int. J. Psychol. 2020, 55, 916–925. [Google Scholar] [CrossRef]
- Caetano, A.C.; Oliveira, D.; Gomes, Z.; Mesquita, E.; Rolanda, C. Psychometry and Pescatori projective test in coloproctological patients. Ann. Gastroenterol. 2017, 30, 433–437. [Google Scholar] [CrossRef]
- Osman, A.; Wong, J.L.; Bagge, C.L.; Freedenthal, S.; Gutierrez, P.M.; Lozano, G. The Depression Anxiety Stress Scales-21 (DASS-21): Further examination of dimensions, scale reliability, and correlates. J. Clin. Psychol. 2012, 68, 1322–1338. [Google Scholar] [CrossRef]
- Page, A.C.; Hooke, G.R.; Morrison, D.L. Psychometric properties of the Depression Anxiety Stress Scales (DASS) in depressed clinical samples. Br. J. Clin. Psychol. 2007, 46, 283–297. [Google Scholar] [CrossRef] [PubMed]
- Garin, O. Ceiling Effect. In Encyclopedia of Quality of Life and Well-Being Research; Michalos, A.C., Ed.; Springer: Dordrecht, The Netherlands, 2014; pp. 631–633. [Google Scholar]
- Obeid, S.; Akel, M.; Haddad, C.; Fares, K.; Sacre, H.; Salameh, P.; Hallit, S. Factors associated with alcohol use disorder: The role of depression, anxiety, stress, alexithymia and work fatigue- a population study in Lebanon. BMC Public Health 2020, 20, 245. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ali, A.M. The relationship between emotional intelligence, distress disclosure and psychological distress among egyptian illicit substance users. J. Addict Recovery 2018, 1, 1–5. [Google Scholar]
- Cooke, J.E.; Eirich, R.; Racine, N.; Madigan, S. Prevalence of posttraumatic and general psychological stress during COVID-19: A rapid review and meta-analysis. Psychiatry Res. 2020, 292, 113347. [Google Scholar] [CrossRef] [PubMed]
- Briere, J.; Gil, E. Self-mutilation in clinical and general population samples: Prevalence, correlates, and functions. Am. J. Orthopsychiatry 1998, 68, 609–620. [Google Scholar] [CrossRef] [Green Version]
- Ibrahim, Z.M.A. Egyptian and Lebanese Written Modern Standard Arabic: Are They One and the Same? Doctorate Thesis, Georgetown University, Washington, DC, USA, 1997. [Google Scholar]
- Al-Kabi, M.; Al-Ayyoub, M.; Alsmadi, I.; Wahsheh, H. A Prototype for a Standard Arabic Sentiment Analysis Corpus. Int. Arab. J. Inf. Technol. 2016, 13, 163–170. [Google Scholar]
- Alkhamees, A.A.; Aljohani, M.S.; Alghesen, M.A.; Alhabib, A.T. Psychological Distress in Quarantine Designated Facility During COVID-19 Pandemic in Saudi Arabia. Risk Manag. Healthc Policy 2020, 13, 3103–3120. [Google Scholar] [CrossRef]
- Ali, A.M.; Ahmed, A.H.; Smail, L. Psychological Climacteric Symptoms and Attitudes toward Menopause among Emirati Women. Int. J. Environ. Res. Public Health 2020, 17, 5028. [Google Scholar] [CrossRef]
- Ali, A.M.; Hendawy, A.O.; Ahmad, O.; Sabbah, H.A.; Smail, L.; Kunugi, H. The Arabic version of the Cohen perceived stress scale: Factorial validity and measurement invariance. Brain Sci. 2021, 11, 419. [Google Scholar] [CrossRef]
- Goetz, C.; Coste, J.; Lemetayer, F.; Rat, A.C.; Montel, S.; Recchia, S.; Debouverie, M.; Pouchot, J.; Spitz, E.; Guillemin, F. Item reduction based on rigorous methodological guidelines is necessary to maintain validity when shortening composite measurement scales. J. Clin. Epidemiol. 2013, 66, 710–718. [Google Scholar] [CrossRef]
- Seel, R.T.; Kreutzer, J.S.; Rosenthal, M.; Hammond, F.M.; Corrigan, J.D.; Black, K. Depression after traumatic brain injury: A National Institute on Disability and Rehabilitation Research Model Systems multicenter investigation. Arch. Phys. Med. Rehabil. 2003, 84, 177–184. [Google Scholar] [CrossRef]
- Ren, L.; Wang, Y.; Wu, L.; Wei, Z.; Cui, L.-B.; Wei, X.; Hu, X.; Peng, J.; Jin, Y.; Li, F.; et al. Network structure of depression and anxiety symptoms in Chinese female nursing students. BMC Psychiatry 2021, 21, 279. [Google Scholar] [CrossRef]
- Ohayon, M.M. Specific characteristics of the pain/depression association in the general population. J. Clin. Psychiatry 2004, 65, 5–9. [Google Scholar] [PubMed]
- Pedrelli, P.; Baer, L.; Iosifescu, D.V.; Fava, M. Relationship Between Residual Symptoms of Depression and Self-reported Cognitive Impairment. CNS Spectr. 2014, 15, 46–51. [Google Scholar] [CrossRef]
- Liu, Y.; Yin, H.; Ma, H.; Yu, X.; Liu, G.; Guo, L.; Geng, Q. The salivary-α-amylase level after stroop test in anxious patients can predict the severity of anxiety. Neurosci. Lett. 2020, 715, 134613. [Google Scholar] [CrossRef] [PubMed]
- Altamura, M.; Iuso, S.; Balzotti, A.; Francavilla, G.; Dimitri, A.; Cibelli, G.; Bellomo, A.; Petito, A. Salivary alpha-amylase and cortisol responsiveness to stress in first episode, drug-naïve patients with panic disorder. Neurosci. Res. 2018, 137, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Gorman, J.M.; Sloan, R.P. Heart rate variability in depressive and anxiety disorders. Am. Heart J. 2000, 140, S77–S83. [Google Scholar] [CrossRef] [PubMed]
- Horowitz, M.J. Stress-Response Syndromes. In International Handbook of Traumatic Stress Syndromes. The Plenum Series on Stress and Coping; Wilson, J.P., Raphael, B., Eds.; Springer: Boston, MA, USA, 1993. [Google Scholar]
- Peirce, A.G. From Intrusive to Oscillating Thoughts. Arch. Psychiatr. Nurs. 2007, 21, 278–286. [Google Scholar] [CrossRef]
- Kähäri, K.; Zachau, G.; Eklöf, M.; Möller, C. The influence of music and stress on musicians’ hearing. J. Sound Vib. 2004, 277, 627–631. [Google Scholar] [CrossRef]
- Shrout, P.E.; Yager, T.J. Reliability and validity of screening scales: Effect of reducing scale length. J. Clin. Epidemiol. 1989, 42, 69–78. [Google Scholar] [CrossRef]
- Sariçam, H. The Psychometric Properties of Turkish Version of Depression Anxiety Stress Scale-21 (DASS-21) in Health Control and Clinical Samples. JCBPR 2018, 7, 19–30. [Google Scholar] [CrossRef]
- Ali, A.M.; Alkhamees, A.A.; Hendawy, A. The psychological impact of COVID-19 among psychiatric patients. Mendeley Data 2021, V1. [Google Scholar] [CrossRef]

| Items | Extracted Factors | ||||
|---|---|---|---|---|---|
| Factor 1 | Factor 2 | Factor 3 | Factor 4 | ||
| 1 | I found it hard to wind down | 0.242 | 0.178 | 0.206 | 0.616 |
| 2 | I was aware of dryness of my mouth | 0.573 | 0.182 | 0.149 | 0.136 |
| 3 | I couldn’t seem to experience any positive feeling at all | 0.265 | 0.278 | 0.365 | 0.284 |
| 4 | I experienced breathing difficulty (e.g., excessively rapid breathing, breathlessness in the absence of physical exertion) | 0.451 | 0.162 | 0.285 | 0.078 |
| 5 | I found it difficult to work up the initiative to do things | 0.246 | 0.206 | 0.474 | 0.022 |
| 6 | I tended to over-react to situations | 0.251 | 0.587 | 0.194 | 0.141 |
| 7 | I experienced trembling (e.g., in the hands) | 0.584 | 0.320 | 0.121 | 0.225 |
| 8 | I felt that I was using a lot of nervous energy | 0.257 | 0.659 | 0.270 | 0.439 |
| 9 | I was worried about situations in which I might panic and make a fool of myself | 0.345 | 0.695 | 0.160 | 0.179 |
| 10 | I felt that I had nothing to look forward to | 0.124 | 0.244 | 0.604 | 0.205 |
| 11 | I found myself getting agitated | 0.348 | 0.552 | 0.390 | 0.427 |
| 12 | I found it difficult to relax | 0.250 | 0.364 | 0.258 | 0.800 |
| 13 | I felt down-hearted and blue | 0.293 | 0.531 | 0.531 | 0.194 |
| 14 | I was intolerant of anything that kept me from getting on with what I was doing | 0.100 | 0.496 | 0.465 | 0.315 |
| 15 | I felt I was close to panic | 0.745 | 0.331 | 0.181 | 0.292 |
| 16 | I was unable to become enthusiastic about anything | 0.342 | 0.166 | 0.701 | 0.267 |
| 17 | I felt I wasn’t worth much as a person | 0.364 | 0.156 | 0.555 | 0.257 |
| 18 | I felt that I was rather touchy | 0.298 | 0.562 | 0.389 | 0.151 |
| 19 | I was aware of the action of my heart in the absence of physical exertion (e.g., sense of heart rate increase, heart missing a beat) | 0.624 | 0.092 | 0.312 | 0.092 |
| 20 | I felt scared without any good reason | 0.699 | 0.296 | 0.234 | 0.223 |
| 21 | I felt that life was meaningless | 0.548 | 0.257 | 0.461 | 0.160 |
| Models | Samples | χ2 | P | Df | CFI | TLI | RMSEA | RMSEA 90% CI | SRMR |
|---|---|---|---|---|---|---|---|---|---|
| Model 1 1F DASS-21 | Sample 1 (C) | 433.259 | 0.000 | 189 | 0.902 | 0.891 | 0.088 | 0.077 to 0.099 | 0.0504 |
| Sample 2 (C) | 1399.543 | 0.000 | 189 | 0.889 | 0.877 | 0.080 | 0.076 to 0.084 | 0.0464 | |
| Sample 1 (E) | 351.518 | 0.000 | 186 | 0.934 | 0.925 | 0.073 | 0.061 to 0.085 | 0.0460 | |
| Sample 2 (E) | 964.340 | 0.000 | 183 | 0.929 | 0.918 | 0.066 | 0.062 to 0.070 | 0.0412 | |
| Model 2 2F DASS-21 | Sample 1 (C) | 410.409 | 0.000 | 188 | 0.911 | 0.901 | 0.084 | 0.073 to 0.095 | 0.0498 |
| Sample 2 (C) | 1305.573 | 0.000 | 188 | 0.898 | 0.886 | 0.077 | 0.074 to 0.081 | 0.0447 | |
| Sample 1 (E) | 328.718 | 0.000 | 185 | 0.942 | 0.935 | 0.068 | 0.056 to 0.080 | 0.0452 | |
| Sample 2 (E) | 819.684 | 0.000 | 179 | 0.941 | 0.931 | 0.060 | 0.056 to 0.064 | 0.0373 | |
| Model 3 3F DASS-21 | Sample 1 (C) | 396.040 | 0.000 | 186 | 0.916 | 0.905 | 0.082 | 0.071 to 0.093 | 0.0489 |
| Sample 2 (C) | 1205.022 | 0.000 | 186 | 0.907 | 0.895 | 0.074 | 0.070 to 0.078 | 0.0427 | |
| Sample 1 (E) | 360.727 | 0.000 | 184 | 0.929 | 0.919 | 0.076 | 0.064 to 0.087 | 0.0460 | |
| Sample 2 (E) | 818.366 | 0.000 | 179 | 0.942 | 0.931 | 0.060 | 0.056 to 0.064 | 0.0366 | |
| Model 4 Bifactor DASS-21 | Sample 1 (C) | 838.898 | 0.000 | 184 | 0.938 | 0.929 | 0.071 | 0.059 to 0.083 | -- |
| Sample 2 (C) | 1207.798 | 0.000 | 184 | 0.906 | 0.893 | 0.075 | 0.071 to 0.079 | -- | |
| Model 5 1F DASS-17 item | Sample 1 (C) | 311.184 | 0.000 | 119 | 0.905 | 0.898 | 0.098 | 0.085 to 0.112 | 0.0510 |
| Sample 2 (C) | 1957.672 | 0.000 | 119 | 0.892 | 0.877 | 0.089 | 0.084 to 0.094 | 0.0477 | |
| Sample 1 (E) | 249.932 | 0.000 | 117 | 0.934 | 0.924 | 0.082 | 0.068 to 0.097 | 0.0458 | |
| Sample 2 (E) | 329.896 | 0.000 | 60 | 0.948 | 0.932 | 0.067 | 0.060 to 0.075 | ||
| Model 6 1F Korean DASS-12 | Sample 1 (C) | 161.031 | 0.000 | 65 | 0.924 | 0.908 | 0.094 | 0.076 to 0.112 | 0.0561 |
| Sample 2 (C) | 598.906 | 0.000 | 65 | 0.903 | 0.884 | 0.091 | 0.084 to 0.098 | 0.0529 | |
| Sample 1 (E) | 139.024 | 0.000 | 64 | 0.940 | 0.927 | 0.084 | 0.065 to 0.103 | 0.0522 | |
| Sample 2 (E) | 399.349 | 0.000 | 62 | 0.939 | 0.923 | 0.074 | 0.067 to 0.081 | 0.0465 | |
| Model 7 3F Korean DASS-12 | Sample 1 (C) | 81.966 | 0.004 | 51 | 0.971 | 0.962 | 0.060 | 0.034 to 0.084 | 0.0388 |
| Sample 2 (C) | 375.549 | 0.000 | 51 | 0.930 | 0.910 | 0.080 | 0.073 to 0.088 | 0.0423 | |
| Sample 2 (E) | 214.140 | 0.000 | 49 | 0.965 | 0.952 | 0.058 | 0.050 to 0.066 | 0.0348 | |
| Model 8 1F Osman’s DASS-13 | Sample 1 (C) | 154.117 | 0.000 | 65 | 0.927 | 0.912 | 0.091 | 0.072 to 0.109 | 0.0560 |
| Sample 2 (C) | 585.667 | 0.000 | 65 | 0.899 | 0.879 | 0.090 | 0.083 to 0.097 | 0.0535 | |
| Sample 1 (E) | 133.026 | 0.000 | 64 | 0.943 | 0.931 | 0.080 | 0.061 to 0.100 | 0.0525 | |
| Sample 2 (E) | 329.896 | 0.000 | 60 | 0.948 | 0.932 | 0.067 | 0.060 to 0.075 | 0.0442 | |
| Model 9 3F Osman’s DASS-13 | Sample 1 (C) | 95.869 | 0.004 | 62 | 0.972 | 0.965 | 0.057 | 0.033 to 0.079 | 0.0413 |
| Sample 2 (C) | 297.251 | 0.000 | 62 | 0.954 | 0.943 | 0.062 | 0.055 to 0.069 | 0.0380 | |
| Sample 2 (E) | 251.989 | 0.000 | 61 | 0.963 | 0.953 | 0.056 | 0.049 to 0.064 | 0.0347 | |
| Model 10 Osman’s DASS-9 | Sample 1 (C) | 80.404 | 0.000 | 27 | 0.917 | 0.889 | 0.106 | 0.082 to 0.137 | 0.0585 |
| Sample 2 (C) | 366.421 | 0.000 | 27 | 0.875 | 0.833 | 0.113 | 0.103 to 0.123 | 0.0586 | |
| Sample 1 (E) | 64.291 | 0.000 | 26 | 0.940 | 0.917 | 0.094 | 0.065 to 0.123 | 0.0535 | |
| Sample 2 (E) | 162.073 | 0.000 | 25 | 0.938 | 0.911 | 0.082 | 0.072 to 0.093 | 0.0505 | |
| Model 11 Osman’s DASS-9 | Sample 1 (C) | 53.590 | 0.000 | 27 | 0.954 | 0.931 | 0.086 | 0.055 to 0.117 | 0.0468 |
| Sample 2 (C) | 366.421 | 0.000 | 27 | 0.875 | 0.833 | 0.113 | 0.103 to 0.123 | 0.0586 | |
| Sample 1 (E) | 41.339 | 0.011 | 23 | 0.971 | 0.955 | 0.069 | 0.033 to 0.102 | 0.0419 | |
| Sample 2 (E) | 72.478 | 0.000 | 22 | 0.981 | 0.969 | 0.048 | 0.036 to 0.061 | 0.0283 | |
| Model 12 A modified 3F DASS-9 | Sample 1 (C) | 38.653 | 0.030 | 24 | 0.987 | 0.980 | 0.060 | 0.019 t0 0.094 | 0.0302 |
| Sample 2 (C) | 225.860 | 0.000 | 24 | 0.955 | 0.933 | 0.092 | 0.081 to 0.103 | 0.0323 | |
| Sample 1 (E) | 24.835 | 0.359 | 23 | 0.998 | 0.997 | 0.022 | 0.000 to 0.069 | 0.0219 | |
| Sample 2 (E) | 134.101 | 0.000 | 23 | 0.976 | 0.962 | 0.070 | 0.059 to 0.081 | 0.0265 | |
| Model 13 3F DASS-8 | Sample 1 (C) | 30.003 | 0.026 | 17 | 0.987 | 0.979 | 0.068 | 0.023 to 0.107 | 0.0275 |
| Sample 2 (C) | 217.990 | 0.000 | 17 | 0.953 | 0.923 | 0.109 | 0.097 to 0.122 | 0.0351 | |
| Sample 1 (E) | 16.483 | 0.420 | 16 | 1.000 | 0.999 | 0.013 | 0.000 to 0.073 | 0.0186 | |
| Sample 2 (E) | 67.047 | 0.000 | 15 | 0.988 | 0.977 | 0.059 | 0.045 to 0.074 | 0.0203 |
| Samples | DASS-21 | DASS-21 Depression | DASS-21 Anxiety | DASS-21 Stress | DASS-9 | DASS-9 Depression | DASS-9 Anxiety ▲ | DASS-9 Stress ▲ | DASS-8 | DASS-8 Depression | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Shapiro–Wilks’ W | Sample 1 | 0.93 | 0.93 | 0.90 | 0.94 | 0.92 | 0.92 | 0.85 | 0.88 | 0.91 | 0.90 |
| Sample 2 | 0.83 | 0.83 | 0.72 | 0.84 | 0.82 | 0.86 | 0.67 | 0.75 | 0.80 | 0.82 |
| DASS versions | Samples | MD | Q1–Q3 | Coefficient Alpha | Alpha-If-Item-Deleted | Item-Total Correlations | Correlation with the DASS-21 | U | W | z |
|---|---|---|---|---|---|---|---|---|---|---|
| DASS-21 | Sample 1 | 21 | 6–39.8 | 0.959 | 0.956–0.959 | 0.364–0.784 | -- | 51,198.5 | 542,734.5 | −8.098 |
| Sample 2 | 7 | 2–17 | 0.939 | 0.933–0.940 | 0.172–0.696 | -- | ||||
| Korean DASS-12 | Sample 1 | 12 | 5–21 | 0.920 | 0.906–0.919 | 0.503–0.817 | 0.977 | 50,933.5 | 542,469.5 | −8.178 |
| Sample 2 | 5 | 1–10 | 0.879 | 0.856–0.881 | 0.366–0.765 | 0.970 | ||||
| Osman’s DASS-13 | Sample 1 | 12 | 4.3–24 | 0.928 | 0.918–0.927 | 0.512–0.794 | 0.984 | 50,478.5 | 542,014.5 | −8.290 |
| Sample 2 | 5 | 1–10 | 0.890 | 0.872–0.893 | 0.331–0.766 | 0.971 | ||||
| Osman’s DASS-9 | Sample 1 | 9 | 3–16 | 0.886 | 0.868–0.884 | 0.491–0.708 | 0.967 | 50,506.0 | 542,042.0 | −8.314 |
| Sample 2 | 3 | 1–7 | 0.829 | 0.789–0.831 | 0.335–0.708 | 0.921 | ||||
| Modified DASS-9 | Sample 1 | 10 | 3–19 | 0.939 | 0.928–0.936 | 0.683–0.830 | 0.977 | 51,697.0 | 543,233.0 | −8.009 |
| Sample 2 | 3 | 1–8 | 0.901 | 0.883–0.905 | 0.471–0.757 | 0.949 | ||||
| DASS-8 | Sample 1 | 9 | 2–17 | 0.936 | 0.924–0.934 | 0.688–0.826 | 0.972 | 50,965.0 | 542,501.0 | −8.229 |
| Sample 2 | 2 | 0–7 | 0.905 | 0.888–0.900 | 0.625–0.756 | 0.929 |
| Criteria | Samples | DASS-21 | Korean DASS-12 | DASS-13 | Osman’s DASS-9 | DASS-9 | DASS-8 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Depression | Anxiety | Stress | Depression | Anxiety ▲ | Stress | Depression | Stress | Depression | Anxiety | Stress | Depression | Anxiety △ | Stress △ | Depression | ||
| Coefficient alpha | Sample 1 | 0.902 | 0.872 | 0.908 | 0.850 | 0.772 | 0.852 | 0.898 | 0.824 | 0.833 | 0.731 | 0.695 | 0.869 | 0.888 | 0.835 | 0.854 |
| Sample 2 | 0.854 | 0.795 | 0.891 | 0.742 | 0.626 | 0.828 | 0.846 | 0.814 | 0.753 | 0.554 | 0.766 | 0.777 | 0.789 | 0.801 | 0.793 | |
| Range of corrected item-total correlations | Sample 1 | 0.607–0.797 | 0.496–0.748 | 0.577–0.820 | 0.653–0.741 | 0.497–0.641 | 0.579–0.766 | 0.665–0.793 | 0.599–0.780 | 0.604–0.708 | 0.484–0.611 | 0.533- | 0.667–0.765 | 0.720–0.829 | All 0.717 | 0.706–0.740 |
| Sample 2 | 0.468–0.707 | 0.349–0.667 | 0.574–0.788 | 0.416–0.606 | 0.350–0.459 | 0.561–0.768 | 0.443–0.707 | 0.614–0.744 | 0.404–0.631 | 0.319–0.400 | 0.623 | 0.443–0.659 | 0.580–0.696 | All 0.668 | 0.595–0.673 | |
| Range of alpha if-item-deleted | Sample 1 | 0.877–0.898 | 0.840–0.873 | 0.884–0.910 | 0.788–0.826 | 0.680–0.755 | 0.779–0.856 | 0.869–0.889 | 0.695–0.835 | 0.770–0.815 | 0.580–0.722 | -- | 0.820–0.845 | 0.801–0.895 | - | 0.782–0.814 |
| Sample 2 | 0.820–0.856 | 0.740–0.801 | 0.862–0.889 | 0.641–0.751 | 0.516–0.602 | 0.734–0.827 | 0.805–0.857 | 0.667–0.801 | 0.650–0.778 | 0.409–0.528 | -- | 0.682–0.793 | 0.647–0.780 | - | 0.676–0.759 | |
| Correlation with the corresponding scale on the DASS-21 | Sample 1 | -- | -- | -- | 0.970 | 0.897 | 0.969 | 0.991 | 0.943 | 0.963 | 0.866 | 0.884 | 0.967 | 0.924 | 0.921 | 0.949 |
| Sample 2 | -- | -- | -- | 0.947 | 0.828 | 0.955 | 0.979 | 0.899 | 0.906 | 0.799 | 0.832 | 0.958 | 0.837 | 0.863 | 0.899 | |
| Correlation with the DASS-21 | Sample 1 | 0.952 | 0.935 | 0.958 | 0.918 | 0.796 | 0.926 | 0.943 | 0.895 | 0.911 | 0.769 | 0.830 | 0.918 | 0.902 | 0.881 | 0.904 |
| Sample 2 | 0.914 | 0.823 | 0.939 | 0.866 | 0.613 | 0.900 | 0.898 | 0.828 | 0.805 | 0.587 | 0.766 | 0.881 | 0.770 | 0.808 | 0.854 | |
| DASS Subscales | Samples | Korean DASS-12 | DASS-13 | Osman’s DASS-9 | Modified DASS-9 | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MD | Q1–Q3 | U | W | z | MD | Q1–Q3 | U | W | z | MD | Q1–Q3 | U | W | z | MD | Q1–Q3 | U | W | z | ||
| Depression | Sample 1 | 5 | 2–9 | 53,363.0 | 544,899.0 | −7.659 | 7 | 2–13 | 51,796.0 | 543,332.0 | −8.014 | 4 | 1–8 | 53,045.0 | 544,581.0 | −7.826 | 5 | 2–9 | 54,378.5 | 545,914.5 | −7.384 |
| Sample 2 | 2 | 0–4 | 3 | 0–5 | 1 | 0–3 | 2 | 0–4 | |||||||||||||
| Anxiety | Sample 1 | 2 | 0–5 | 55,078.5 | 546,614.5 | −7.724 | 2 | 0–5 | 55,078.5 | 546,614.5 | −7.724 | 2 | 0–4 | 55,800.0 | 547,336.0 | −7.609 | 3 | 0–6 | 54,555.0 | 546,091.0 | −7.940 |
| Sample 2 | 0 | 0–2 | 0 | 0–2 | 0 | 0–1 | 0 | 0–2 | |||||||||||||
| Stress | Sample 1 | 5 | 2–8 | 54,327.5 | 545,863.5 | −7.424 | 4 | 1–6 | 56,008.5 | 547,544.5 | −7.096 | 3 | 1–4 | 57,678.5 | 549,214.5 | −6.780 | 2 | 0–4 | 56,053.5 | 547,586.5 | −7.316 |
| Sample 2 | 2 | 0–5 | 1 | 0–3 | 1 | 0–3 | 0 | 0–2 | |||||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ali, A.M.; Alkhamees, A.A.; Hori, H.; Kim, Y.; Kunugi, H. The Depression Anxiety Stress Scale 21: Development and Validation of the Depression Anxiety Stress Scale 8-Item in Psychiatric Patients and the General Public for Easier Mental Health Measurement in a Post COVID-19 World. Int. J. Environ. Res. Public Health 2021, 18, 10142. https://doi.org/10.3390/ijerph181910142
Ali AM, Alkhamees AA, Hori H, Kim Y, Kunugi H. The Depression Anxiety Stress Scale 21: Development and Validation of the Depression Anxiety Stress Scale 8-Item in Psychiatric Patients and the General Public for Easier Mental Health Measurement in a Post COVID-19 World. International Journal of Environmental Research and Public Health. 2021; 18(19):10142. https://doi.org/10.3390/ijerph181910142
Chicago/Turabian StyleAli, Amira Mohammed, Abdulmajeed A. Alkhamees, Hiroaki Hori, Yoshiharu Kim, and Hiroshi Kunugi. 2021. "The Depression Anxiety Stress Scale 21: Development and Validation of the Depression Anxiety Stress Scale 8-Item in Psychiatric Patients and the General Public for Easier Mental Health Measurement in a Post COVID-19 World" International Journal of Environmental Research and Public Health 18, no. 19: 10142. https://doi.org/10.3390/ijerph181910142
APA StyleAli, A. M., Alkhamees, A. A., Hori, H., Kim, Y., & Kunugi, H. (2021). The Depression Anxiety Stress Scale 21: Development and Validation of the Depression Anxiety Stress Scale 8-Item in Psychiatric Patients and the General Public for Easier Mental Health Measurement in a Post COVID-19 World. International Journal of Environmental Research and Public Health, 18(19), 10142. https://doi.org/10.3390/ijerph181910142







