Is Loneliness an Undervalued Pathway between Socio-Economic Disadvantage and Health?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data and Sample
2.2. Measures
2.2.1. Dependent Variables
2.2.2. Independent Variables
Loneliness
Confounders
2.3. Statistical Analyses
3. Results
3.1. Descriptive Statistics
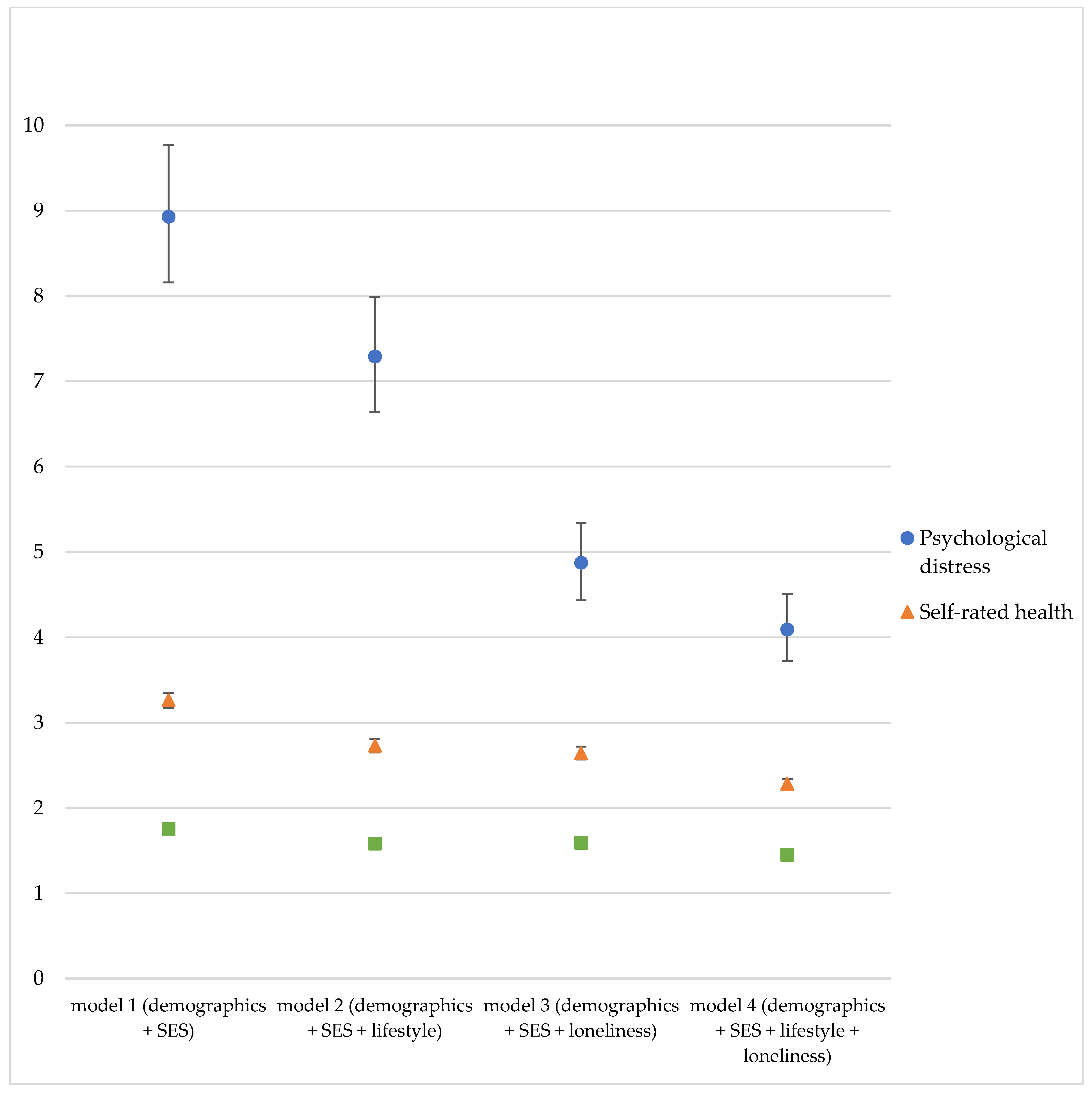
3.2. Socioeconomic Status, Lifestyle, and Loneliness
3.3. Analyses in Age and Gender Strata
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Marmot, M.; Allen, J.; Bell, R.; Bloomer, E.; Goldblatt, P. WHO European review of social determinants of health and the health divide. Lancet 2012, 380, 1011–1029. [Google Scholar] [CrossRef]
- Black, S.D. Inequalities in health: Report of a Research Working Group: Department of Health and Social Security. Achiev. Dis. Child. 1980, 56, 161–162. [Google Scholar] [CrossRef] [Green Version]
- Marmot, M.; Rose, G.; Shipley, M.; Hamilton, P. Employment grade and coronary heart disease in British civil servants. J. Epidemiol. Community Health 1978, 32, 244–249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Braveman, P.G.L. The social determinants of health: It’s time to consider the causes of the causes. Public Health Rep. 2014, 129, 19–31. [Google Scholar] [CrossRef] [Green Version]
- Zajacova, A.; Lawrence, E.M. The relationship between education and health: Reducing disparities through a contextual approach. Annu. Rev. Public Health 2018, 39, 273–278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marengoni, A.; Winblad, B.; Karp, A.; Fratiglioni, L. Prevalence of chronic diseases and multimorbidity among the elderly population in Sweden. Am. J. Public Health 2008, 98, 1198–1200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cockerham, W.C.; Hamby, B.W.; Oates, G.R. The social determinants of chronic disease. Am. J. Prev. Med. 2017, 52, S5–S12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lindström, M.; Hanson, B.S.; Östergren, P.-O. Socioeconomic differences in leisure-time physical activity: The role of social participation and social capital in shaping health related behaviour. Soc. Sci. Med. 2001, 52, 441–451. [Google Scholar] [CrossRef]
- Lantz, P.M.; Lynch, J.W.; House, J.S.; Lepkowski, J.M.; Mero, R.P.; Musick, M.A.; Williams, D.R. Socioeconomic disparities in health change in a longitudinal study of US adults: The role of health-risk behaviors. Soc. Sci. Med. 2001, 53, 29–40. [Google Scholar] [CrossRef]
- Dahlgren, G.; Whitehead, M. European Strategies for Tackling Social Inequities in Health: Levelling Up Part 2. Copenhagen: World Health Organization Regional Office for Europe. 2006. Available online: https://apps.who.int/iris/handle/10665/107791 (accessed on 17 June 2021).
- Molarius, A.; Berglund, K.; Eriksson, C.; Lambe, M.; Nordström, E.; Eriksson, H.G.; Feldman, I. Socioeconomic conditions, lifestyle factors, and self-rated health among men and women in Sweden. Eur. J. Public Health 2006, 17, 125–133. [Google Scholar] [CrossRef] [Green Version]
- Hawkley, L.C.; Cacioppo, J.T. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Ann. Behav. Med. 2010, 40, 218–227. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bosma, H.; Jansen, M.; Schefman, S.; Hajema, K.; Feron, F. Lonely at the bottom: A cross-sectional study on being ill, poor, and lonely. Public Health 2015, 129, 185–187. [Google Scholar] [CrossRef]
- De Jong-Gierveld, J.; Kamphuls, F. The development of a Rasch-type loneliness scale. Appl. Psychol. Meas. 1985, 9, 289–299. [Google Scholar] [CrossRef]
- Zhuori, N.; Cai, Y.; Yan, Y.; Cui, Y.; Zhao, M. Does Social Support Affect the Health of the Elderly in Rural China? A Meta-Analysis Approach. Int. J. Environ. Res. Public Health 2019, 16, 3471. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matud, M.P.; García, M.C.; Fortes, D. Relevance of Gender and Social Support in Self-Rated Health and Life Satisfaction in Elderly Spanish People. Int. J. Environ. Res. Public Health 2019, 16, 2725. [Google Scholar] [CrossRef] [Green Version]
- Mendoza-Núñez, V.M.; González-Mantilla, F.; Correa-Muñoz, E.; Retana-Ugalde, R. Relationship between Social Support Networks and Physical Functioning in Older Community-Dwelling Mexicans. Int. J. Environ. Res. Public Health 2017, 14, 993. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cherry, K. Loneliness: Causes and Health Consequences. Verywell Mind. 2021. Available online: https://www.verywellmind.com/loneliness-causes-effects-and-treatments-2795749#citation-2 (accessed on 6 September 2021).
- DiJulio, B.; Hamel, L.; Muñana, C.; Brodie, M. Loneliness and Social Isolation in the United States, the United Kingdom, and Japan: An International Survey. San Francisco: Kaiser Family Foundation. 2018. Available online: https://www.kff.org/other/report/loneliness-and-social-isolation-in-the-united-states-the-united-kingdom-and-japan-an-international-survey/ (accessed on 17 June 2021).
- Franssen, T.; Stijnen, M.; Hamers, F.; Schneider, F. Age differences in demographic, social and health-related factors associated with loneliness across the adult life span (19–65 years): A cross-sectional study in The Netherlands. BMC Public Health 2020, 20, 1118. [Google Scholar] [CrossRef]
- Elovainio, M.; Hakulinen, C.; Pulkki-Råback, L.; Virtanen, M.; Josefsson, K.; Jokela, M.; Vahtera, J.; Kivimäki, M. Contribution of risk factors to excess mortality in isolated and lonely individuals: An analysis of data from the UK Biobank cohort study. Lancet Public Health 2017, 2, e260–e266. [Google Scholar] [CrossRef] [Green Version]
- Hawkley, L.C.; Burleson, M.H.; Berntson, G.G.; Cacioppo, J.T. Loneliness in everyday life: Cardiovascular activity, psychosocial context, and health behaviors. J. Pers. Soc. Psychol. 2003, 85, 105. [Google Scholar] [CrossRef] [PubMed]
- Rico-Uribe, L.A.; Caballero, F.F.; Olaya, B.; Tobiasz-Adamczyk, B.; Koskinen, S.; Leonardi, M.; Haro, J.M.; Chatterji, S.; Ayuso-Mateos, J.L.; Miret, M. Loneliness, social networks, and health: A cross-sectional study in three countries. PLoS ONE 2016, 11, e0145264. [Google Scholar] [CrossRef] [Green Version]
- Lauder, W.; Mummery, K.; Jones, M.; Caperchione, C. A comparison of health behaviours in lonely and non-lonely populations. Psychol. Health Med. 2006, 11, 233–245. [Google Scholar] [CrossRef] [PubMed]
- Beutel, M.E.; Klein, E.M.; Brähler, E.; Reiner, I.; Jünger, C.; Michal, M.; Wiltink, J.; Wild, P.S.; Münzel, T.; Lackner, K.J. Loneliness in the general population: Prevalence, determinants and relations to mental health. BMC Psychiatry 2017, 17, 97. [Google Scholar] [CrossRef] [Green Version]
- Meisters, R.; Westra, D.; Putrik, P.; Bosma, H.; Ruwaard, D.; Jansen, M. Does loneliness have a cost? A population-wide study of the association between loneliness and healthcare expenditure. Int. J. Public Health 2021, 66. [Google Scholar] [CrossRef]
- Pinquart, M. Loneliness in Married, Widowed, Divorced, and Never-Married Older Adults. J. Soc. Pers. Relatsh. 2003, 20, 31–53. [Google Scholar] [CrossRef]
- Ten Kate, R.L.F.; Bilecen, B.; Steverink, N. A Closer Look at Loneliness: Why Do First-Generation Migrants Feel More Lonely Than Their Native Dutch Counterparts? Gerontologist 2020, 60, 291–301. [Google Scholar] [CrossRef]
- Van den Brink, C.L.; van Herten, M.H.; Boeker, S. Gezondheidsmonitor 2012 The Dutch public health monitor 2012. Tijdschr. Voor Gezondh. 2017, 95, 222–227. [Google Scholar] [CrossRef]
- Documentatie Gezondheidsmonitor Volwassenen en Ouderen 2016. Centraal Bureau voor de Statistiek. 2018. Available online: https://www.cbs.nl/nl-nl/onze-diensten/maatwerk-en-microdata/microdata-zelf-onderzoek-doen/microdatabestanden/gemon-2016-gezondheidsmonitor-volwassenen-en-ouderen (accessed on 17 June 2021).
- Kessler, R.C.; Andrews, G.; Colpe, L.J.; Hiripi, E.; Mroczek, D.K.; Normand, S.-L.; Walters, E.E.; Zaslavsky, A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002, 32, 959–976. [Google Scholar] [CrossRef]
- Spee, H.; Smits, N.; de Koning, H. Bruikbaarheid van Kessler Psychological Distress Scale (K10) voor prevalentieschatting van depressie en angststoornissen. Tijdschr. voor Gezondh. 2012, 90, 144–148. [Google Scholar] [CrossRef]
- Bonsaksen, T.; Schoultz, M.; Thygesen, H.; Ruffolo, M.; Price, D.; Leung, J.; Geirdal, A.Ø. Loneliness and Its Associated Factors Nine Months after the COVID-19 Outbreak: A Cross-National Study. Int. J. Environ. Res. Public Health 2021, 18, 2841. [Google Scholar] [CrossRef]
- Chen, J.; Gong, L. Loneliness in urbanising China. Health Soc. Care Community 2021. [Google Scholar] [CrossRef]
- Tan, S.S.; Fierloos, I.N.; Zhang, X.; Koppelaar, E.; Alhambra-Borras, T.; Rentoumis, T.; Williams, G.; Rukavina, T.; van Staveren, R.; Garces-Ferrer, J.; et al. The Association between Loneliness and Health Related Quality of Life (HR-QoL) among Community-Dwelling Older Citizens. Int. J. Environ. Res. Public Health 2020, 17, 600. [Google Scholar] [CrossRef] [Green Version]
- Limarutti, A.; Maier, M.J.; Mir, E. Exploring loneliness and students’ sense of coherence (S-SoC) in the university setting. Curr. Psychol. 2021. [Google Scholar] [CrossRef]
- Sipowicz, K.; Podlecka, M.; Mokros, Ł.; Pietras, T. Lonely in the City–Sociodemographic Status and Somatic Morbidities as Predictors of Loneliness and Depression among Seniors–Preliminary Results. Int. J. Environ. Res. Public Health 2021, 18, 7213. [Google Scholar] [CrossRef]
- Lantz, P.M.; House, J.S.; Lepkowski, J.M.; Williams, D.R.; Mero, R.P.; Chen, J. Socioeconomic factors, health behaviors, and mortality: Results from a nationally representative prospective study of US adults. JAMA 1998, 279, 1703–1708. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Derks, I.P.; Koster, A.; Schram, M.T.; Stehouwer, C.D.; Dagnelie, P.C.; Groffen, D.A.; Bosma, H. The association of early life socioeconomic conditions with prediabetes and type 2 diabetes: Results from the Maastricht study. Int. J. Equity Health 2017, 16, 61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, W.; Qian, L.; Shi, J.; Franklin, M. Comparing performance between log-binomial and robust Poisson regression models for estimating risk ratios under model misspecification. BMC Med. Res. Methodol. 2018, 18, 63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simons, A.M.W.; Groffen, D.A.I.; Bosma, H. Income-related health inequalities: Does perceived discrimination matter? Int. J. Public Health 2013, 58, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Colombet, Z.; Perignon, M.; Salanave, B.; Landais, E.; Martin-Prevel, Y.; Allès, B.; Drogue, S.; Amiot, M.J.; Méjean, C. Socioeconomic inequalities in metabolic syndrome in the French West Indies. BMC Public Health 2019, 19, 1620. [Google Scholar] [CrossRef]
- Ahmad, S.; Demler, O.V.; Sun, Q.; Moorthy, M.V.; Li, C.; Lee, I.-M.; Ridker, P.M.; Manson, J.E.; Hu, F.B.; Fall, T.; et al. Association of the Mediterranean Diet With Onset of Diabetes in the Women’s Health Study. JAMA Netw. Open 2020, 3, e2025466. [Google Scholar] [CrossRef]
- Van Buuren, S. Flexible Imputation of Missing Data; CRC Press: Boca Raton, FL, USA, 2018. [Google Scholar]
- StataCorp. Stata Statistical Software: Release 16; StataCorp LLC: College Station, TX, USA, 2019. [Google Scholar]
- Sosa-Iudicissa, M.; Tejedor-Real, P. Public Health. European Parliament. 2018. Available online: http://www.europarl.europa.eu/thinktank/en/document.html?reference=04A_FT(2013)050503 (accessed on 17 June 2021).
- Mackenbach, J.P.; McKee, M. A comparative analysis of health policy performance in 43 European countries. Eur. J. Public Health 2013, 23, 195–201. [Google Scholar] [CrossRef] [Green Version]
- Broeders, D.; Das, D.; Jennissen, R.; Tiemeijer, W.; de Visser, M. Van Verschil Naar Potentieel. Een Realistisch Perspectief op de Sociaaleconomische Gezondheidsverschillen. wrr-Policy Brief 7. Den Haag: WRR The Netherlands Scientific Council for Government Policy. 2018. Available online: https://www.wrr.nl/publicaties/policy-briefs/2018/08/27/van-verschil-naar-potentieel.-een-realistisch-perspectief-op-de-sociaaleconomische-gezondheidsverschillen (accessed on 9 April 2019).
- National Prevention Agreement. Ministry of Health, Welfare and Sport. 2018. Available online: https://www.rijksoverheid.nl/onderwerpen/gezondheid-en-preventie/nationaal-preventieakkoord (accessed on 9 April 2019).
- Williams, C.Y.K.; Townson, A.T.; Kapur, M.; Ferreira, A.F.; Nunn, R.; Galante, J.; Philips, V.; Gentry, S.; Usher-Smith, J.A. Interventions to reduce social isolation and loneliness during COVID-19 physical distancing measures: A rapid systematic review. PLoS ONE 2021, 16, e0247139. [Google Scholar] [CrossRef]
- One against loneliness. The Hague: Ministry of Health, Welfare and Sport. 2018. Available online: https://www.rijksoverheid.nl/onderwerpen/eenzaamheid/aanpak-eenzaamheid (accessed on 7 March 2019).
- PM Launches Government’s First Loneliness Strategy. Department for Digital, Culture, Media & Sport. 2018. Available online: https://www.gov.uk/government/news/pm-launches-governments-first-loneliness-strategy#:~:text=Loneliness%20is%20one%20of%20the,and%20voluntary%20services%20by%202023 (accessed on 7 March 2019).
- Putrik, P.; de Vries, N.K.; Mujakovic, S.; van Amelsvoort, L.; Kant, I.; Kunst, A.E.; van Oers, H.; Jansen, M. Living environment matters: Relationships between neighborhood characteristics and health of the residents in a Dutch municipality. J. Community Health 2015, 40, 47–56. [Google Scholar] [CrossRef]
- Strak, M.; Janssen, N.; Beelen, R.; Schmitz, O.; Karssenberg, D.; Houthuijs, D.; van den Brink, C.; Dijst, M.; Brunekreef, B.; Hoek, G. Associations between lifestyle and air pollution exposure: Potential for confounding in large administrative data cohorts. Environ. Res. 2017, 156, 364–373. [Google Scholar] [CrossRef] [PubMed]
- Statline. The Netherlands in Figures. Statistics Netherlands. 2020. Available online: https://opendata.cbs.nl/statline/#/CBS/nl/dataset/37296ned/table?ts=1597391508685 (accessed on 14 August 2020).
| Sample Characteristics | N (%) | |
|---|---|---|
| Age | 19–40 | 68,434 (15.4%) |
| 41–64 | 142,790 (32.0%) | |
| 65–80 | 192,640 (43.2%) | |
| 81+ | 41,884 (9.4%) | |
| Gender | Male | 204,095 (45.8%) |
| Female | 241,653 (54.2%) | |
| Migration background | Dutch-born | 389,298 (87.3%) |
| Western background | 38,445 (8.6%) | |
| Non-Western background | 18,005 (4.1%) | |
| Marital status | Married/co-habitant | 313,285 (70.9%) |
| Single | 45,853 (10.4%) | |
| Widowed | 30,593 (6.9%) | |
| Divorced | 51,877 (11.7%) | |
| Education | Primary school | 30,981 (7.5%) |
| Lower vocational | 138,947 (33.5%) | |
| Middle vocational/secondary | 125,981 (30.4%) | |
| Higher vocational/university | 118,985 (28.7%) | |
| Household income quartile | 0–25% | 64,825 (14.6%) |
| 26%–50% | 122,251 (27.5%) | |
| 51%–75% | 125,196 (28.1%) | |
| 76%–100% | 132,739 (29.8%) | |
| Self-reported income adequacy | Inadequate, major concerns | 12,367 (3.0%) |
| Inadequate, some concerns | 43,640 (10.5%) | |
| Adequate, minor concerns | 146,380 (35.1%) | |
| Adequate, no concerns | 215,147 (51.5%) | |
| SES Construct | Q1, lowest SES | 103,316 (25.1%) |
| Q2 | 102,502 (24.9%) | |
| Q3 | 103,322 (25.1%) | |
| Q4, highest SES | 102,697(24.9%) | |
| Physical activity | Sufficient | 288,523 (70.1%) |
| Insufficient | 122,855 (29.9%) | |
| Body Mass Index (BMI) | Underweight (<18.5) | 5410 (1.3%) |
| Normal (18.5–25) | 190,365 (44.8%) | |
| Overweight (25–30) | 164,653 (38.8%) | |
| Obese (30>) | 64,431 (15.2%) | |
| Alcohol consumption | Never | 47,286 (11.4%) |
| Regular consumption | 335,675 (80.9%) | |
| Excessive | 32,256 (7.8%) | |
| Smoking | Never smoked | 170,859 (40.6%) |
| Former smoker | 181,412 (43.2%) | |
| Current smoker | 68,163 (16.2%) | |
| Chronic disease | None | 261,977 (59.9%) |
| At least one | 175,086 (40.1%) | |
| Self-rated health | Fair, bad | 125,043 (28.4%) |
| (Very) good, excellent | 315,079 (71.6%) | |
| Psychological distress | No or low risk | 411,536 (95.1%) |
| High risk | 21,362 (4.9%) | |
| Mode of survey completion | Paper | 221,433 (49.7%) |
| Internet | 223,657 (50.2%) | |
| Face-to-face | 428 (0.1%) | |
| Telephone | 230 (0.01%) | |
| Mean (sd) | ||
| Loneliness | 3.1(2.9) | |
| Model 1 | Model 2 | Model 3 | Model 4 | ||||
|---|---|---|---|---|---|---|---|
| (SES) | (SES + Lifestyle-Related Factors) | (SES + Loneliness) | (SES + Lifestyle-Related + Loneliness) | ||||
| RR/OR (95% CI) | % Reduction | % Reduction | % Reduction | ||||
| Chronic disease (RR) | |||||||
| Q1 lowest SES | 1.75 (1.72–1.79) | 1.58 (1.55–1.61) | 23% | 1.59 (1.55–1.62) | 21% | 1.45 (1.42–1.48) | 40% |
| Q2 | 1.30 (1.27–1.32) | 1.22 (1.20–1.25) | 27% | 1.24 (1.21–1.26) | 20% | 1.17 (1.15–1.20) | 43% |
| Q3 | 1.14 (1.11–1.16) | 1.10 (1.07–1,13) | 29% | 1.11 (1.09–1.14) | 21% | 1.08 (1.05–1.11) | 43% |
| Q4 highest SES | Ref | Ref | Ref | Ref | |||
| Self-rated health (RR) | |||||||
| Q1 lowest SES | 3.26 (3.17–3.35) | 2.73 (2.65–2.81) | 23% | 2.64 (2.57–2.72) | 27% | 2.28 (2.21–2.34) | 43% |
| Q2 | 2.01 (1.94–2.07) | 1.83 (1.78–1.89) | 18% | 1.81 (1.76–1.87) | 20% | 1.68 (1.63–1.73) | 33% |
| Q3 | 1.46 (1.41–1.51) | 1.39 (1.34–1.43) | 15% | 1.39 (1.35–1.44) | 15% | 1.33 (1.29–1.38) | 28% |
| Q4 highest SES | Ref | Ref | Ref | Ref | |||
| Psychological distress (OR) | |||||||
| Q1 lowest SES | 8.93 (8.16–9.77) | 7.29 (6.64–7.99) | 21% | 4.87 (4.43–5.34) | 51% | 4.09 (3.72–4.51) | 61% |
| Q2 | 3.24 (2.94–3.57) | 2.94 (2.67–3.25) | 13% | 2.29 (2.07–2.53) | 42% | 2.12 (1.91–2.34) | 50% |
| Q3 | 1.85 (1.67–2.05) | 1.75 (1.58–1.94) | 12% | 1.58 (1.42–1.76) | 32% | 1.51 (1.36–1.68) | 40% |
| Q4 highest SES | Ref | Ref | Ref | Ref | |||
| RR/OR (95% CI) (% reduction) | Complete sample (n = 445,748) | Age group 19–40 (n = 68,434) | Age group 41–64 (n = 142,790) | Age group 65–80 (n = 192,640) | Age group 81+ (n = 41,884) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Chronic disease (RR) | ||||||||||
| Q1 lowest SES Q2 Q3 Q4 highest SES | 1.59 (1.55–1.62) | 21% | 1.83 (1.72–1.95) | 27% | 1.73 (1.68–1.79) | 22% | 1.27 (1.25–1.30) | 21% | 1.10 (1.06–1.15) | 29% |
| 1.24 (1.21–1.26) | 20% | 1.29 (1.20–1.37) | 26% | 1.29 (1.25–1.33) | 17% | 1.08 (1.06–1,10) | 27% | 1.00 (0.96–1.04) | ||
| 1.11 (1.09–1.14) | 21% | 1.12 (1.05–1.20) | 25% | 1.15 (1.11–1.19) | 12% | 1.01 (0.99–1.04) | 0.99 (0.95–1.03) | |||
| Ref | Ref | Ref | Ref | Ref | ||||||
| Self-rated health (RR) | ||||||||||
| Q1 lowest SES Q2 Q3 Q4 highest SES | 2.64 (2.57–2.72) | 27% | 2.95 (2.70–3.23) | 37% | 2.96 (2.83–3.09) | 28% | 2.11 (2,05–2.18) | 20% | 1.53 (1.46–1.61) | 16% |
| 1.81 (1.76–1.87) | 20% | 1.88 (1.71–2.06) | 27% | 1.90 (1.81–1.99) | 18% | 1.56 (1.51–1.61) | 14% | 1.29 (1.22–1.35) | 9% | |
| 1.39 (1.35–1.44) | 15% | 1.43 (1.29–1.58) | 19% | 1.43 (1.36–1.50) | 12% | 1.25 (1.21–1.29) | 14% | 1.17 (1.10–1.23) | 6% | |
| Ref | Ref | Ref | Ref | Ref | ||||||
| Psychological distress (OR) | ||||||||||
| Q1 lowest SES | 4.87 (4.43–5.34) | 51% | 3.92 (3.32–4.61) | 55% | 5.83 (5.09–6.67) | 51% | 5.18 (4.48–5.98) | 40% | 4.95 (3.86–6.33) | 27% |
| Q2 Q3 Q4 highest SES | 2.29 (2.07–2.53) | 42% | 2.06 (1.73–2.47) | 64% | 2.52 (2.18–2.91) | 40% | 2.32 (2.00–2.70) | 32% | 2.72 (2.11–3.51) | 18% |
| 1.58 (1.42–1.76) | 32% | 1.49 (1.24–1.79) | 36% | 1.64 (1.41–1.90) | 29% | 1.66 (1.40–1.96) | 27% | 1.65 (1.22–2.23) | 21% | |
| Ref | Ref | Ref | Ref | Ref | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meisters, R.; Putrik, P.; Westra, D.; Bosma, H.; Ruwaard, D.; Jansen, M. Is Loneliness an Undervalued Pathway between Socio-Economic Disadvantage and Health? Int. J. Environ. Res. Public Health 2021, 18, 10177. https://doi.org/10.3390/ijerph181910177
Meisters R, Putrik P, Westra D, Bosma H, Ruwaard D, Jansen M. Is Loneliness an Undervalued Pathway between Socio-Economic Disadvantage and Health? International Journal of Environmental Research and Public Health. 2021; 18(19):10177. https://doi.org/10.3390/ijerph181910177
Chicago/Turabian StyleMeisters, Rachelle, Polina Putrik, Daan Westra, Hans Bosma, Dirk Ruwaard, and Maria Jansen. 2021. "Is Loneliness an Undervalued Pathway between Socio-Economic Disadvantage and Health?" International Journal of Environmental Research and Public Health 18, no. 19: 10177. https://doi.org/10.3390/ijerph181910177






