How Does Urban Sprawl Affect Public Health? Evidence from Panel Survey Data in Urbanizing China
Abstract
1. Introduction
2. Research Methods and Data Sources
2.1. Model
2.2. Data Sources
2.3. Variable Definition
3. Empirical Analysis
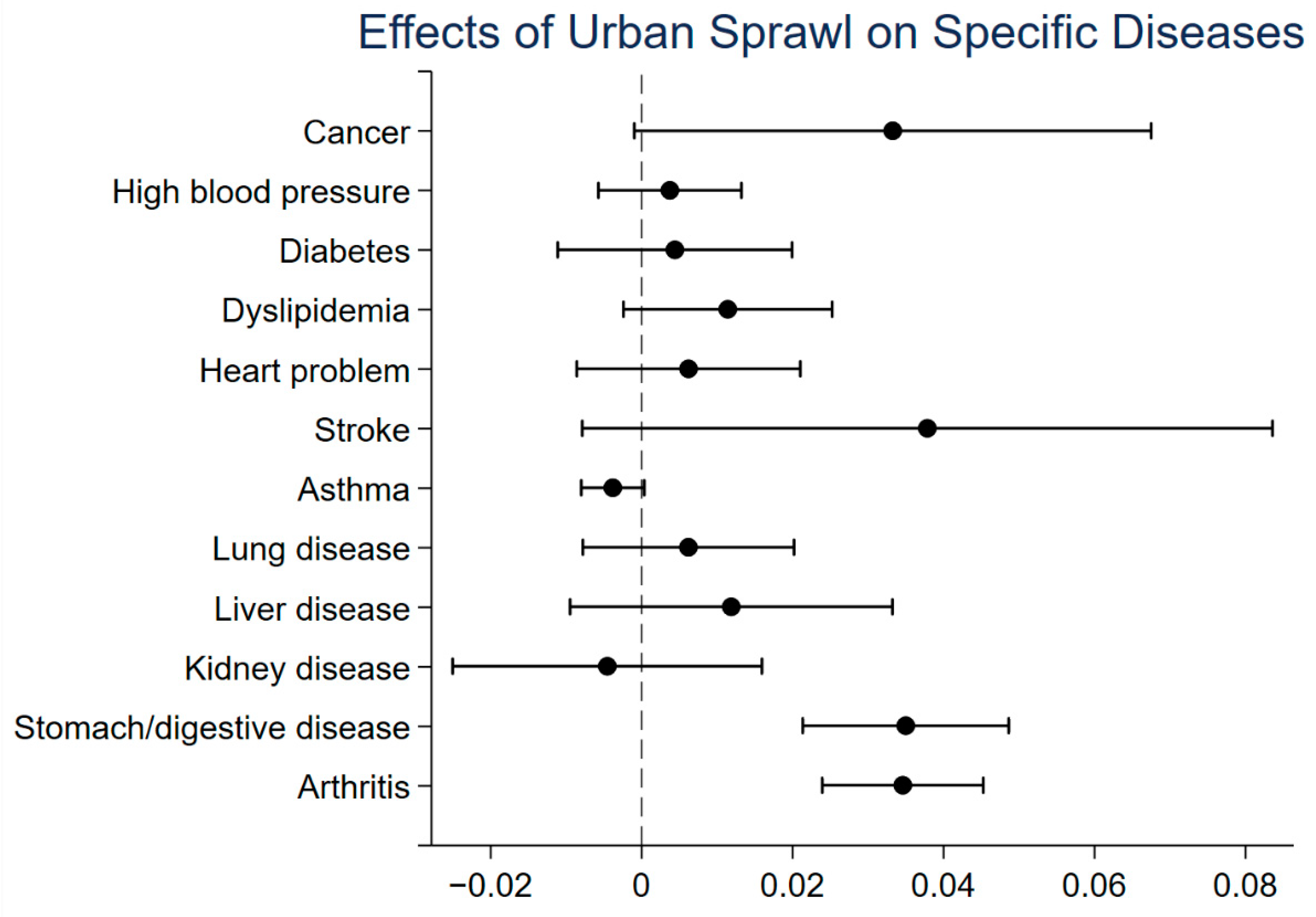
3.1. Benchmark Regression Results
3.2. Robustness Test
3.3. Heterogeneity Analysis
3.3.1. Gender Heterogeneity
3.3.2. Age Heterogeneity
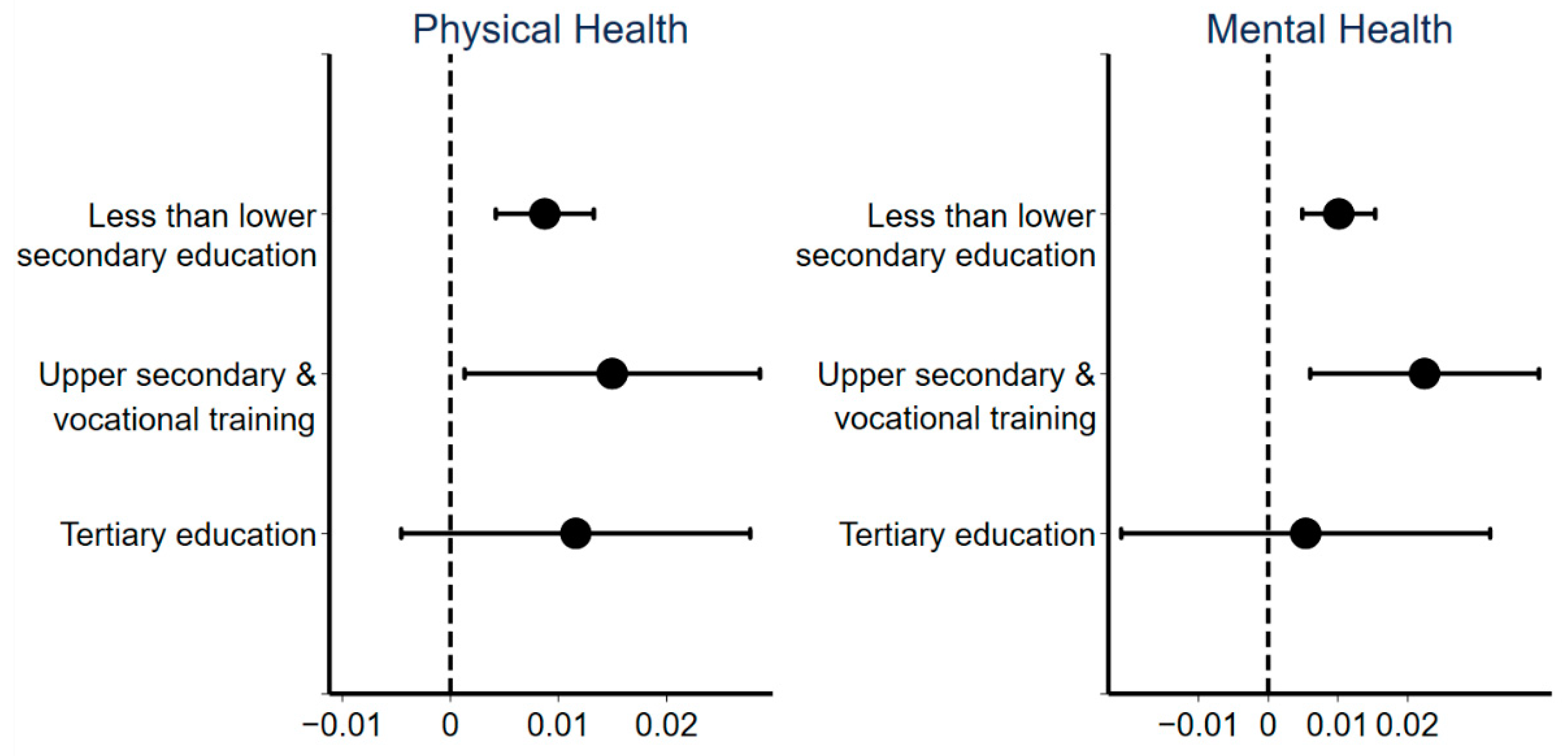
3.3.3. Education Heterogeneity
3.3.4. Income Heterogeneity
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Frenkel, A.; Ashkenazi, M. Measuring urban sprawl: How can we deal with it? Environ. Plan. B Plan. Des. 2008, 35, 56–79. [Google Scholar] [CrossRef]
- Inostroza, L.; Baur, R.; Csaplovics, E. Urban sprawl and fragmentation in Latin America: A dynamic quantification and characterization of spatial patterns. J. Environ. Manag. 2013, 115, 87–97. [Google Scholar] [CrossRef]
- Ewing, R.; Hamidi, S.; Grace, J.B.; Wei, Y.D. Does urban sprawl hold down upward mobility? Landsc. Urban Plan. 2016, 148, 80–88. [Google Scholar] [CrossRef]
- Wang, X.; Shi, R.; Zhou, Y. Dynamics of urban sprawl and sustainable development in China. Socio-Econ. Plan. Sci. 2020, 70, 100736. [Google Scholar] [CrossRef]
- Glaeser, E.L.; Kahn, M.E. Sprawl and Urban Growth. In Handbook of Regional and Urban Economics; JV Henderson and J.-F. Thisse: Amsterdam, The Netherlands, 2004; Volume 4. [Google Scholar] [CrossRef]
- Aguilera, A.; Mignot, D. Urban sprawl, polycentrism and commuting. A comparison of seven French urban areas. Urban Public Econ. Rev. 2004, 1, 93–113. [Google Scholar]
- Oueslati, W.; Alvanides, S.; Garrod, G. Determinants of urban sprawl in European cities. Urban Stud. 2015, 52, 1594–1614. [Google Scholar] [CrossRef]
- Lv, Y.; Zhou, L.; Yao, G.; Zheng, X. Detecting the true urban polycentric pattern of Chinese cities in morphological dimensions: A multiscale analysis based on geospatial big data. Cities 2021, 116, 103298. [Google Scholar] [CrossRef]
- OECD. Rethinking Urban Sprawl Moving towards Sustainable Cities; OECD Publishing: Paris, France, 2018; Available online: https://oe.cd/urban-sprawl (accessed on 20 April 2021).
- Fallah, B.N.; Partridge, M.D.; Olfert, M.R. Urban sprawl and productivity: Evidence from US metropolitan areas. Pap. Reg. Sci. 2011, 90, 451–472. [Google Scholar] [CrossRef]
- Hamidi, S.; Zandiatashbar, A. Does urban form matter for innovation productivity? A national multi-level study of the association between neighbourhood innovation capacity and urban sprawl. Urban Stud. 2019, 56, 1576–1594. [Google Scholar] [CrossRef]
- Ye, H.; He, X.; Song, Y.; Li, X.; Zhang, G.; Lin, T.; Xiao, L. A sustainable urban form: The challenges of compactness from the viewpoint of energy consumption and carbon emission. Energy Build. 2015, 93, 90–98. [Google Scholar] [CrossRef]
- Navamuel, E.L.; Morollón, F.R.; Cuartas, B.M. Energy consumption and urban sprawl: Evidence for the Spanish case. J. Clean. Prod. 2018, 172, 3479–3486. [Google Scholar] [CrossRef]
- Stone, B., Jr. Urban sprawl and air quality in large US cities. J. Environ. Manag. 2008, 86, 688–698. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Liu, Y. Effects of China’s urban form on urban air quality. Urban Stud. 2016, 53, 2607–2623. [Google Scholar] [CrossRef]
- Mou, Y.; Song, Y.; Xu, Q.; He, Q.; Hu, A. Influence of urban-growth pattern on air quality in China: A study of 338 cities. Int. J. Environ. Res. Public Health 2018, 15, 1805. [Google Scholar] [CrossRef]
- Sultana, S.; Weber, J. Journey-to-work patterns in the age of sprawl: Evidence from two midsize southern metropolitan areas. Prof. Geogr. 2007, 59, 193–208. [Google Scholar] [CrossRef]
- Miller, M.D. The impacts of Atlanta’s urban sprawl on forest cover and fragmentation. Appl. Geogr. 2012, 34, 171–179. [Google Scholar] [CrossRef]
- Canedoli, C.; Crocco, F.; Comolli, R.; Padoa-Schioppa, E. Landscape fragmentation and urban sprawl in the urban region of Milan. Landsc. Res. 2018, 43, 632–651. [Google Scholar] [CrossRef]
- Brueckner, J.K. Urban sprawl: Diagnosis and remedies. Int. Reg. Sci. Rev. 2000, 23, 160–171. [Google Scholar] [CrossRef]
- Frumkin, H. Urban Sprawl and Public Health. Public Health Rep. 2002, 117, 201–217. [Google Scholar] [CrossRef]
- Ewing, R.; Schieber, R.A.; Zegeer, C.V. Urban sprawl as a risk factor in motor vehicle occupant and pedestrian fatalities. Am. J. Public Health 2003, 93, 1541–1545. [Google Scholar] [CrossRef]
- Frumkin, H.; Frank, L.; Frank, L.D.; Jackson, R.J. Urban Sprawl and Public Health: Designing, Planning, and Building for Healthy Communities; Island Press: Washington, DC, USA, 2004. [Google Scholar]
- Iram, A.; Rasool, L.; Shahzad, F.; Saeed, Y. Impact of Urban sprawl on public health: An Analysis of Lahore-Pakistan. World Appl. Sci. J. 2012, 20, 80–86. [Google Scholar] [CrossRef]
- Ewing, R.; Meakins, G.; Hamidi, S.; Nelson, A.C. Relationship between urban sprawl and physical activity, obesity, and morbidity–Update and refinement. Health Place 2014, 26, 118–126. [Google Scholar] [CrossRef]
- Garrido-Cumbrera, M.; Ruiz, D.G.; Braçe, O.; Lara, E.L. Exploring the association between urban sprawl and mental health. J. Transp. Health 2018, 10, 381–390. [Google Scholar] [CrossRef]
- Hamidi, S.; Ewing, R.; Tatalovich, Z.; Grace, J.B.; Berrigan, D. Associations between urban sprawl and life expectancy in the United States. Int. J. Environ. Res. Public Health 2018, 15, 861. [Google Scholar] [CrossRef]
- Lopez, R. Urban sprawl and risk for being overweight or obese. Am. J. Public Health 2004, 94, 1574–1579. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Kaestner, R. Effects of urban sprawl on obesity. J. Health Econ. 2010, 29, 779–787. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Yang, S.; Liu, M.; Qiu, G.; Li, H.; Luo, M.; Jia, P. Urban sprawl and childhood obesity. Obes. Rev. 2021, 22, e13091. [Google Scholar] [CrossRef]
- Lathey, V.; Guhathakurta, S.; Aggarwal, R.M. The impact of subregional variations in urban sprawl on the prevalence of obesity and related morbidity. J. Plan. Educ. Res. 2009, 29, 127–141. [Google Scholar] [CrossRef]
- Fan, Y.; Song, Y. Is sprawl associated with a widening urban–suburban mortality gap? J. Urban Health 2009, 86, 708–728. [Google Scholar] [CrossRef][Green Version]
- Berrigan, D.; Tatalovich, Z.; Pickle, L.W.; Ewing, R.; Ballard-Barbash, R. Urban sprawl, obesity, and cancer mortality in the United States: Cross-sectional analysis and methodological challenges. Int. J. Health Geogr. 2014, 13, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Griffin, B.A.; Eibner, C.; Bird, C.E.; Jewell, A.; Margolis, K.; Shih, R.; Slaughter, M.E.; Whitsel, E.A.; Allison, M.; Escarce, J.J. The relationship between urban sprawl and coronary heart disease in women. Health Place 2013, 20, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.S.; Lung, S.C.C. Multiple impacts and pathways of urban form and environmental factors on cardiovascular mortality. Sci. Total Environ. 2020, 738, 139512. [Google Scholar] [CrossRef]
- Trubka, R.; Newman, P.; Bilsborough, D. The costs of urban sprawl–Physical activity links to healthcare costs and productivity. Environ. Des. Guide 2010, 1–13. Available online: https://www.jstor.org/stable/26150804 (accessed on 25 September 2021).
- Çetin, M.; Bakırtaş, İ. Does Urbanization Induce the Health Expenditures? A Dynamic Macro-Panel Analysis for Developing Countries. Dumlupınar Üniversitesi Sos. Bilimler Derg. 2019, 61, 208–222. [Google Scholar]
- World Health Organization. China-WHO Country Cooperation Strategy 2016–2020. 2016. Available online: https://iris.wpro.who.int/bitstream/handle/10665.1/13088/WPRO_2016_DPM_003_eng.pdf (accessed on 12 May 2021).
- Garden, F.L.; Jalaludin, B.B. Impact of urban sprawl on overweight, obesity, and physical activity in Sydney, Australia. J. Urban Health 2009, 86, 19–30. [Google Scholar] [CrossRef] [PubMed]
- Tsai, Y.H. Quantifying urban form: Compactness versus’ sprawl’. Urban Stud. 2005, 42, 141–161. [Google Scholar] [CrossRef]
- Koprowska, K.; Łaszkiewicz, E.; Kronenberg, J. Is urban sprawl linked to green space availability? Ecol. Indic. 2020, 108, 105723. [Google Scholar] [CrossRef]
- Guerra, E.; Dong, X.; Kondo, M. Do denser neighborhoods have safer streets? population density and traffic safety in the Philadelphia Region. J. Plan. Educ. Res. 2019. [Google Scholar] [CrossRef]
- Travisi, C.M.; Camagni, R.; Nijkamp, P. Impacts of urban sprawl and commuting: A modelling study for Italy. J. Transp. Geogr. 2010, 18, 382–392. [Google Scholar] [CrossRef]
- Wanner, M.; Götschi, T.; Martin-Diener, E.; Kahlmeier, S.; Martin, B.W. Active transport, physical activity, and body weight in adults: A systematic review. Am. J. Prev. Med. 2012, 42, 493–502. [Google Scholar] [CrossRef] [PubMed]
- Fishman, E.; Böcker, L.; Helbich, M. Adult active transport in the Netherlands: An analysis of its contribution to physical activity requirements. PLoS ONE 2015, 10, e0121871. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Wei, J.; Duan, D.H.; Guo, Y.M.; Yang, D.X.; Jia, C.; Mi, X.T. Impact of Land-Use and Land-Cover Change on urban air quality in representative cities of China. J. Atmos. Sol. -Terr. Phys. 2016, 142, 43–54. [Google Scholar] [CrossRef]
- Zheng, Z.; Zhang, X.; Wang, J.; Dandekar, A.; Kim, H.; Qiu, Y.; Xu, X.; Cui, Y.; Wang, A.; Chen, L.C.; et al. Exposure to fine airborne particulate matters induces hepatic fibrosis in murine models. J. Hepatol. 2015, 63, 1397–1404. [Google Scholar] [CrossRef]
- Liu, C.; Chen, R.; Zhao, Y.; Ma, Z.; Bi, J.; Liu, Y.; Meng, X.; Wang, Y.; Chen, X.; Li, W.; et al. Associations between ambient fine particulate air pollution and hypertension: A nationwide cross-sectional study in China. Sci. Total Environ. 2017, 584, 869–874. [Google Scholar] [CrossRef]
- Calderón-Garcidueñas, L.; Azzarelli, B.; Acuna, H.; Garcia, R.; Gambling, T.M.; Osnaya, N.; Monroy, S.; Tizapantzi, M.D.R.; Carson, J.L.; Villarreal-Calderon, A.; et al. Air pollution and brain damage. Toxicol. Pathol. 2002, 30, 373–389. [Google Scholar] [CrossRef] [PubMed]
- Moulton, P.V.; Yang, W. Air pollution, oxidative stress, and Alzheimer’s disease. J. Environ. Public Health 2012, 472751. [Google Scholar] [CrossRef] [PubMed]
- Melis, G.; Gelormino, E.; Marra, G.; Ferracin, E.; Costa, G. The effects of the urban built environment on mental health: A cohort study in a large northern Italian city. Int. J. Environ. Res. Public Health 2015, 12, 14898–14915. [Google Scholar] [CrossRef] [PubMed]
- Adaku, E. Urban sprawl: A view from developing and developed countries. Afr. J. Geogr. Reg. Plan. 2014, 1, 193–207. [Google Scholar]
- Zhou, Y.; Ma, J.C.L. Economic restructuring and suburbanization in China. Urban Geogr. 2000, 21, 205–236. [Google Scholar] [CrossRef]
- Feng, J.; Zhou, Y.; Wu, F. New Trends of Suburbanization in Beijing since 1990: From Government-led to Market-oriented. Reg. Stud. 2008, 42, 83–99. [Google Scholar] [CrossRef]
- Lim, Y.H.; Kim, H.; Kim, J.H.; Bae, S.; Park, H.Y.; Hong, Y.C. Air pollution and symptoms of depression in elderly adults. Environ. Health Perspect. 2012, 120, 1023–1028. [Google Scholar] [CrossRef]
- Wang, Y.; Eliot, M.N.; Koutrakis, P.; Gryparis, A.; Schwartz, J.D.; Coull, B.A.; Mittleman, M.; Milberg, W.P.; Lipsitz, L.A.; Wellenius, G. Ambient air pollution and depressive symptoms in older adults: Results from the MOBILIZE Boston study. Environ. Health Perspect. 2014, 122, 553–558. [Google Scholar] [CrossRef]
- Lei, X.; Smith, J.P.; Sun, X.; Zhao, Y. Gender differences in cognition in China and reasons for change over time: Evidence from CHARLS. J. Econ. Ageing 2014, 4, 46–55. [Google Scholar] [CrossRef]
- Zhao, Y.; Hu, Y.; Smith, J.P.; Strauss, J.; Yang, G. Cohort profile: The China health and retirement longitudinal study (CHARLS). Int. J. Epidemiol. 2014, 43, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Huang, J.; Wen, D.; Li, J. An updated MODIS global urban extent product (MGUP) from 2001 to 2018 based on an automated mapping approach. Int. J. Appl. Earth Obs. Geoinf. 2021, 95, 102255. [Google Scholar] [CrossRef]
- Mertes, C.M.; Schneider, A.; Sulla-Menashe, D.; Tatem, A.J.; Tan, B. Detecting change in urban areas at continental scales with MODIS data. Remote Sens. Environ. 2015, 158, 331–347. [Google Scholar] [CrossRef]
- Sulla-Menashe, D.; Gray, J.M.; Abercrombie, S.P.; Friedl, M.A. Hierarchical mapping of annual global land cover 2001 to present: The MODIS Collection 6 Land Cover product. Remote Sens. Environ. 2019, 222, 183–194. [Google Scholar] [CrossRef]
- Bai, Z.; Wang, J.; Wang, M.; Gao, M.; Sun, J. Accuracy assessment of multi-source gridded population distribution datasets in China. Sustainability 2018, 10, 1363. [Google Scholar] [CrossRef]
- Cohen-Mansfield, J.; Pawlson, G.; Lipson, S.; Volpato, S. The measurement of health: A comparison of indices of disease severity. J. Clin. Epidemiol. 2001, 54, 1094–1102. [Google Scholar] [CrossRef]
- Wang, Y.; Luo, N. Air Pollution, Health Depreciation and Medical Costs: Research Based on the Three Perspectives of Physical Health, Mental Health and Social Adaptability. Econ. Res. J. 2020, 55, 80–97. (In Chinese) [Google Scholar]
- Cheng, S.T.; Chan, A.C. The center for epidemiologic studies depression scale in older Chinese: Thresholds for long and short forms. Int. J. Geriatr. Psychiatry A J. Psychiatry Late Life Allied Sci. 2005, 20, 465–470. [Google Scholar] [CrossRef]
- Qin, X.; Wang, S.; Hsieh, C.R. The prevalence of depression and depressive symptoms among adults in China: Estimation based on a National Household Survey. China Econ. Rev. 2018, 51, 271–282. [Google Scholar] [CrossRef]
- Fulton, W.B.; Pendall, R.; Nguyẽn, M.; Harrison, A. Who Sprawls Most? How Growth Patterns Differ across the US; Brookings Institution, Center on Urban and Metropolitan Policy: Washington, DC, USA, 2001. [Google Scholar]
- Koball, H.L.; Moiduddin, E.; Henderson, J.; Goesling, B.; Besculides, M. What do we know about the link between marriage and health? J. Fam. Issues 2010, 31, 1019–1040. [Google Scholar] [CrossRef]
- Cutler, D.M.; Lleras-Muney, A.; Vogl, T. Socioeconomic status and health: Dimensions and mechanisms. NBER Working Paper 2008, 14333. [Google Scholar] [CrossRef]
- Cutler, D.M.; Glaeser, E. What explains differences in smoking, drinking, and other health-related behaviors? Am. Econ. Rev. 2005, 95, 238–242. [Google Scholar] [CrossRef] [PubMed]
- Bagnardi, V.; Rota, M.; Botteri, E.; Tramacere, I.; Islami, F.; Fedirko, V.; Scotti, L.; Jenab, M.; Turati, F.; Pasquali, E.; et al. Alcohol consumption and site-specific cancer risk: A comprehensive dose–response meta-analysis. Br. J. Cancer 2015, 112, 580–593. [Google Scholar] [CrossRef] [PubMed]
- Garaycoechea, J.I.; Crossan, G.; Langevin, F.; Mulderrig, L.; Louzada, S.; Yang, F.; Guilbaud, G.; Park, N.; Roerink, S.; Nik-Zainal, S.; et al. Alcohol and endogenous aldehydes damage chromosomes and mutate stem cells. Nature 2018, 553, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Kahn, J.R.; Pearlin, L.I. Financial strain over the life course and health among older adults. J. Health Soc. Behav. 2006, 47, 17–31. [Google Scholar] [CrossRef] [PubMed]
- Van Doorslaer, E.; Masseria, C.; Koolman, X. Inequalities in access to medical care by income in developed countries. CMAJ 2006, 174, 177–183. [Google Scholar] [CrossRef]
- Li, G.; Li, F. Urban sprawl in China: Differences and socioeconomic drivers. Sci. Total Environ. 2019, 673, 367–377. [Google Scholar] [CrossRef]
- Tao, L.I. Spatial distribution of the aged population in shanghai and influencing factors. City Plan. Rev. 2020, 6, 39–46. (In Chinese) [Google Scholar] [CrossRef]
- Li, Z.; Yuan, L. Professional intergenerational mobility in entering state owned departments: Family background and education. S. China J. Econ. 2019, 9, 69–83. (In Chinese) [Google Scholar] [CrossRef]




| Variable Name | Definition | Obs | Mean | SD | Min | Max |
|---|---|---|---|---|---|---|
| Health | ||||||
| Physical health | Total number of diseases the respondent had | 9232 | 1.718 | 1.586 | 0 | 10 |
| Mental health | Score of the short form of the Center for Epidemiological Studies Depression scale | 9435 | 7.160 | 5.757 | 0 | 30 |
| Urban sprawl | ||||||
| Urban sprawl | Urban sprawl index | 9803 | 2.581 | 3.092 | −11.813 | 19.625 |
| Individual demographic characteristics | ||||||
| Age | 9803 | 60.502 | 9.439 | 45 | 94 | |
| Gender | 0 for female; 1 for male | 9803 | 0.471 | 0.499 | 0 | 1 |
| Marriage | 0 for separated, divorced, widowed, and never married; 1 for married | 9803 | 0.135 | 0.342 | 0 | 1 |
| Education | 0 for less than lower secondary education, 1 for upper secondary and vocational training | 9803 | 0.156 | 0.363 | 0 | 1 |
| Education_2 | 0 for less than lower secondary education, 1 for tertiary education | 9803 | 0.035 | 0.183 | 0 | 1 |
| Employment | 0 for unemployed, retired, or never worked; 1 for currently working | 9803 | 0.536 | 0.499 | 0 | 1 |
| Health behavior variables | ||||||
| Smoke | 0 for never having smoked; 1 for ever smoking | 9803 | 0.404 | 0.491 | 0 | 1 |
| Drink | 0 for never having an alcoholic drink in the past; 1 for having had an alcoholic drink in the past | 9803 | 0.428 | 0.495 | 0 | 1 |
| Family structure variables | ||||||
| Ln(Hhincome) | The sum of all income at the household level | 9803 | 9.713 | 2.379 | 0 | 14.863 |
| Hhcoresd | 0 for no child co-resides with respondent; 1 for any child co-resides with respondent | 9803 | 0.549 | 0.498 | 0 | 1 |
| Hhnum | The number of people living in household | 9803 | 3.305 | 1.576 | 1 | 12 |
| Physical Health | Mental Health | |
|---|---|---|
| (1) | (2) | |
| Urban sprawl | 0.011 *** | 0.012 *** |
| (4.04) | (3.94) | |
| Age | 0.033 *** | −0.000 |
| (25.13) | (−0.34) | |
| Gender | −0.208 *** | −0.244 *** |
| (−6.40) | (−8.26) | |
| Marriage | −0.084 ** | 0.112 *** |
| (−2.53) | (3.74) | |
| Education | 0.049 | −0.240 *** |
| (1.27) | (−7.64) | |
| Education_2 | 0.048 | −0.345 *** |
| (0.79) | (−5.56) | |
| Employment | −0.024 | −0.045 ** |
| (−1.49) | (−2.40) | |
| Drink | 0.058 *** | −0.005 |
| (3.75) | (−0.24) | |
| Smoke | 0.133 *** | 0.061 ** |
| (5.66) | (2.26) | |
| Ln(Hhincome) | −0.008*** | −0.022 *** |
| (−3.68) | (−7.18) | |
| Hhcoresd | 0.012 | −0.006 |
| (0.83) | (−0.28) | |
| Hhnum | −0.032 *** | 0.006 |
| (−5.42) | (0.93) | |
| Constant | −1.342 *** | 2.296 *** |
| (−14.22) | (26.62) | |
| N | 9232 | 9435 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yan, Y.; Liu, H.; He, C. How Does Urban Sprawl Affect Public Health? Evidence from Panel Survey Data in Urbanizing China. Int. J. Environ. Res. Public Health 2021, 18, 10181. https://doi.org/10.3390/ijerph181910181
Yan Y, Liu H, He C. How Does Urban Sprawl Affect Public Health? Evidence from Panel Survey Data in Urbanizing China. International Journal of Environmental Research and Public Health. 2021; 18(19):10181. https://doi.org/10.3390/ijerph181910181
Chicago/Turabian StyleYan, Yan, Hui Liu, and Canfei He. 2021. "How Does Urban Sprawl Affect Public Health? Evidence from Panel Survey Data in Urbanizing China" International Journal of Environmental Research and Public Health 18, no. 19: 10181. https://doi.org/10.3390/ijerph181910181
APA StyleYan, Y., Liu, H., & He, C. (2021). How Does Urban Sprawl Affect Public Health? Evidence from Panel Survey Data in Urbanizing China. International Journal of Environmental Research and Public Health, 18(19), 10181. https://doi.org/10.3390/ijerph181910181







