Mental Illness Inequalities by Multimorbidity, Use of Health Resources and Socio-Economic Status in an Aging Society
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data
2.1.1. Health Indicators
2.1.2. Socioeconomic Status (SES)
2.1.3. Health Care
2.2. Methods
2.3. Ethics Statement
3. Results
3.1. Descriptive Statistics
3.2. Inequality in Mental Health
3.3. Inequity in Health Care Use among Individuals with Mental Health Disorders
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vigo, D.; Thornicroft, G.; Atun, R. Estimating the true global burden of mental illness. Lancet Psychiatry 2016, 3, 171–178. [Google Scholar] [CrossRef] [Green Version]
- Institute for Health Metrics and Evaluation (IHME). Rethinking Development and Health: Findings from the Global Burden of Disease Study; Seattle, W., Ed.; IHME: Seattle, WA, USA, 2016. [Google Scholar]
- Rhem, J.; Shield, K.D. Global Burden of Disease and the Impact of Mental and Addictive Disorders. Curr. Psychiatry Rep. 2019, 21, 10. [Google Scholar] [CrossRef] [PubMed]
- Whiteford, H.A.; Degenhardt, L.; Rehm, J.; Baxter, A.J.; Ferrari, A.J.; Erskine, H.E.; Charlson, F.J.; Norman, R.E.; Flaxman, A.D.; Johns, N.; et al. Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. Lancet 2013, 382, 1575–1586. [Google Scholar] [CrossRef]
- WHO. The Global Burden of Disease: 2004 Update; WHO: Geneva, Switzerland, 2008. [Google Scholar]
- OECD/European Union. Health at a Glance: Europe 2018: State of Health in the EU Cycle; OECD Publishing: Paris, France; European Union: Brussels, Belgium, 2018; Available online: https://doi.org/10.1787/health_glance_eur-2018-en (accessed on 11 September 2020).
- Funk, M.; Ivbijaro, G. Integrating Mental Health into Primary Care. A Global Perspective; World Health Organization and World Organization of Family Doctors (Wonca): Geneva, Switzerland, 2008; ISBN 978-92-4-156368-0. Available online: https://www.who.int/mental_health/resources/mentalhealth_PHC_2008.pdf (accessed on 11 September 2020).
- Layard, R. The Economics of Mental Health; IZA World of Labor: Bonn, Germany, 2016; p. 321. [Google Scholar]
- Dening, T.; Barapatre, C. Mental Health and the Ageing Population. J. Br. Menopause Soc. 2004, 10, 49–53. [Google Scholar] [CrossRef]
- Barnett, K.; Mercer, S.W.; Norbury, M.; Watt, G.; Wyke, S.; Guthrie, B. Epidemiology of multimorbidity and implications for healthcare, research, and medical education: A cross-sectional study. Lancet 2012, 380, 37–43. [Google Scholar] [CrossRef]
- Mathers, C.D.; Loncar, D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006, 3, e442. [Google Scholar] [CrossRef] [Green Version]
- Samb, B.; Desai, N.; Nishtar, S.; Mendis, S.; Wright, A.; Hsu, J.; Martiniuk, A.; Celletti, F.; Patel, K.; Adshead, F.; et al. Prevention and management of chronic disease: A litmus test for health-systems strengthening in low-income and middle-income countries. Lancet 2010, 376, 1785–1797. [Google Scholar] [CrossRef]
- Jadad, A.R.; Cabrera, A.; Martos, F.; Smith, R.; Lyons, R.F. When People Live with Multiple Chronic Diseases: A Collaborative Approach to an Emerging Global Challenge; Andalusian School of Public Health: Granada, Spain, 2010. [Google Scholar]
- García-Goñi, M.; Hernández-Quevedo, C.; Nuño-Solinís, R.; Paolucci, F. Pathways towards chronic care-focused healthcare systems: Evidence from Spain. Health Policy 2012, 108, 236–245. [Google Scholar] [CrossRef] [Green Version]
- OECD. Health Reform: Meeting the Challenge of Ageing and Multiple Morbidities. Paris, France. 2011. Available online: http://www.oecd-ilibrary.org/content/book/9789264122314-en (accessed on 29 October 2020).
- Tinetti, M.E.; Fried, T.R.; Boyd, C.M. Designing health care for the most common chronic condition—Multimorbidity. JAMA 2012, 307, 2493–2494. [Google Scholar] [CrossRef]
- Vogeli, C.; Shields, A.E.; Lee, T.A.; Gibson, T.B.; Marder, W.D.; Weiss, K.B.; Blumenthal, D. Multiple chronic conditions: Prevalence, health consequences, and implications for quality, care management, and costs. J. Gen. Intern. Med. 2007, 22 (Suppl. S3), 391–395. [Google Scholar] [CrossRef] [Green Version]
- Rocca, W.A.; Boyd, C.M.; Grossardt, B.R.; Bobo, W.V.; Finney Rutten, L.J.; Roger, V.L.; Ebbert, J.O.; Therneau, T.M.; Yawn, B.P.; St Sauver, J.L.; et al. Prevalence of Multimorbidity in a Geographically Defined American Population: Patterns by Age, Sex, and Race/Ethnicity. Mayo Clin. Proc. 2014, 89, 1336–1349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Orueta, J.F.; García-Álvarez, A.; García-Goñi, M.; Paolucci, F.; Nuño-Solinís, R. Prevalence and costs of multimorbidity by deprivation levels in the Basque Country. A population based study using health administrative databases. PLoS ONE 2014, 9, e89787. [Google Scholar] [CrossRef] [PubMed]
- Sakib, M.N.; Shooshtari, S.; St. John, F.; Menec, V. The prevalence of multimorbidity and associations with lifestyle factors among middle-aged Canadians: An analysis of Canadian Longitudinal Study on Aging data. BMC Public Health 2019, 19, 243. [Google Scholar] [CrossRef] [PubMed]
- Bengoa, R. Curar y cuidar. In Curar y Cuidar. Innovación en la Gestión de Enfermedades Crónicas: Una Guía Práctica Para Avanzar; Bengoa, R., Nuño Solinís, N., Eds.; Elsevier Masson: Barcelona, Spain, 2008; Chapter 2. [Google Scholar]
- Kiely, K.M.; Brady, B.; Byle, J. Gender, mental health and ageing. Maturitas 2019, 129, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Prince, M.J.; Wu, F.; Guo, Y.; Gutierrez Robledo, L.M.; O’Donnell, M.; Sullivan, R.; Yusuf, S. The burden of disease in older people and implications for health policy and practice. Lancet 2015, 385, 549–562. [Google Scholar] [CrossRef]
- Oliver, A.; Mossialos, E. Equity of access to health care: Outlining the foundations for action. J. Epidemiol. Community Health 2004, 58, 655–658. [Google Scholar] [CrossRef] [Green Version]
- Adler, N.E.; Newman, K. Socioeconomic disparities in health: Pathways and policies. Health Aff. 2002, 21, 60–76. [Google Scholar] [CrossRef]
- Luo, J.; Zhang, X.; Jin, C.; Wang, D. Inequality of access to health care among the urban elderly in Northwestern China. Health Policy 2009, 93, 111–117. [Google Scholar] [CrossRef]
- Sommers, B.D.; Baicker, K.; Epstein, A.M. Mortality and access to care among adults after state Medicaid expansions. N. Engl. J. Med. 2012, 367, 1025–1034. [Google Scholar] [CrossRef]
- Djernes, J.K. Prevalence and predictors of depression in populations of elderly: A review. Acta Psychiatr. Scand. 2006, 113, 372–387. [Google Scholar] [CrossRef]
- Frølich, A.; Ghith, N.; Schiøtz, M.; Jacobsen, R.; Stockmarr, A. Multimorbidity, healthcare utilization and socioeconomic status: A register-based study in Denmark. PLoS ONE 2019, 14, e0214183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schiøtz, M.L.; Stockmarr, A.; Høst, D.; Glümer, C.; Frølich, A. Social disparities in the prevalence of multimorbidity: A register-based population study. BMC Public Health 2017, 17, 422. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kivimäki, M.; Batty, G.D.; Pentti, J.; Shipley, M.J.; Sipilä, P.N.; Nyberg, S.T.; Suominen, S.B.; Oksanen, T.; Stenholm, S.; Vitranen, M.; et al. Association between socioeconomic status and the development of mental and physical health conditions in adulthood: A multi-cohort study. Lancet Public Health 2020, 5, e140–e149. [Google Scholar] [CrossRef]
- Domènech-Abella, J.; Mundó, J.; Leonardi, M.; Chatterji, S.; Tobiasz-Adamczyk, B.; Koskinen, S.; Ayuso-Mateos, J.L.; Haro, J.M. The association between socioeconomic status and depression among older adults in Finland, Poland and Spain: A comparative cross-sectional study of distinct measures and pathways. J. Affect. Disord. 2018, 241, 311–318. [Google Scholar] [CrossRef] [Green Version]
- Pickett, K.E.; Wilkinson, R.G. Inequality: An underacknowledged source of mental illness and distress. Br. J. Psychiatry 2010, 197, 426–428. [Google Scholar] [CrossRef] [Green Version]
- Murali, V.; Oyebode, F. Poverty, social inequality and mental health. Adv. Psychiatr. Treat. 2004, 10, 216–224. [Google Scholar] [CrossRef]
- Fryers, T.; Melzer, D.; Jenkins, R. Social inequalities and the common mental disorders: A systematic review of the evidence. Soc. Psychiatr. Epidemiol. 2003, 38, 229–237. [Google Scholar] [CrossRef]
- Lorant, V.; Deliege, D.; Eaton, W.; Robert, A.; Philippot, P.; Ansseau, M. Socioeconomic inequalities in depression: A meta-analysis. Am. J. Epidemiol. 2003, 157, 98–112. [Google Scholar] [CrossRef] [Green Version]
- Eckersley, R. Beyond inequality: Acknowledging the complexity of social determinants of health. Soc. Sci. Med. 2015, 147, 121–125. [Google Scholar] [CrossRef]
- Dohrenwend, B.P.; Dohrenwend, B.S. Social Status and Psychological Disorder; a Causal Inquiry; Wiley-Interscience: New York, NY, USA, 1969. [Google Scholar]
- Eaton, W.W. A formal theory of selection for schizophrenia. Am. J. Sociol. 1980, 86, 149–158. [Google Scholar] [CrossRef]
- García-Armesto, S.; Abadía-Taira, M.B.; Durán, A.; Hernández-Quevedo, C.; Bernal-Delgado, E. Spain: Health System Review; Health Systems in Transition; WHO Regional Office for Europe: Copenhagen, Denmark, 2010; Volume 12, pp. 1–295. [Google Scholar]
- Gabilondo, A.; Alonso-Moran, E.; Nuño-Solinis, R.; Orueta, J.F.; Iruin, A. Comorbidities with chronic physical conditions and gender profiles of illness in schizophrenia. Results from PREST, a new health dataset. J. Psychosom. Res. 2017, 93, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Spanish Institute of Health Information. Spanish Version (eCIE9MC) of the Electronic International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), 8th ed.; Ministerio de Sanidad, Servicios Sociales e Igualdad: Madrid, Spain, 2012. Available online: https://www.mscbs.gob.es/en/estadEstudios/estadisticas/docs/CIE9MC_8ed.pdf (accessed on 1 November 2020).
- WHO Collaborating Centre for Drug Statistics Methodology. International Language for Drug Utilization Research ATC/DDD; ATC/DDD Index: Oslo, Norway, 2012; Available online: https://www.whocc.no/filearchive/publications/1_2013guidelines.pdf (accessed on 1 November 2020).
- Johns Hopkins Bloomberg School of Public Health. The Johns Hopkins ACG Case-Mix System Technical Reference Guide Manual Version 9.0; Johns Hopkins Bloomberg School of Public Health: Baltimore, MD, USA, 2009. [Google Scholar]
- Forjaz, M.J.; Rodriguez-Blazquez, C.; Ayala, A.; Rodriguez-Rodriguez, V.; De Pedro-Cuesta, J. Garcia-Gutierrez, S.; Prados-Torres, A. Chronic conditions, disability, and quality of life in older adults with multimorbidity in Spain. Eur. J. Intern. Med. 2015, 26, 176–181. [Google Scholar] [CrossRef] [PubMed]
- Villagrasa, B.; Olaya, B.; Lopez-Anton, R.; De la Cámara, C.; Lobo, A.; Santabárbara, J. Prevalence of anxiety disorder among older adults in Spain: A meta-analysis. J. Affect. Dis. 2019, 246, 408–417. [Google Scholar] [CrossRef] [PubMed]
- Coventry, P.; Lovell, K.; Dickens, C.; Bower, P.; Chew-Graham, C.; McElvenny, D.; Hann, M.; Cherrington, A.; Garrett, C.; Gibbonsm, C.J.; et al. Integrated primary care for patients with mental and physical multimorbidity: Clúster randomised controlled trial of collaborative care for patients with depression comorbib with diabetis or cardiovascular disease. BMJ 2015, 350, h638. [Google Scholar] [CrossRef] [Green Version]
- Fortin, M.; Lapointe, L.; Hudon, C.; Vanasse, A.; Ntetu, A.; Maltais, D. Multimorbidity and quality of life in primary care: A systematic review. Health Qual. Life Outcomes 2004, 2, 51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walker, A. Multiple chronic diseases and quality of life: Patterns emerging from a large national sample, Australia. Chronic Illn. 2007, 3, 202–218. [Google Scholar] [CrossRef]
- Gijsen, R.; Hoeymans, N.; Schellevis, F.; Ruwaard, D.; Satariano, W.; Bos, G. Causes and consequences of comorbidity: A review. J. Clin. Epidemiol. 2001, 54, 661–674. [Google Scholar] [CrossRef]
- Wolff, J.; Starfield, B.; Anderson, G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch. Intern. Med. 2002, 162, 2269–2276. [Google Scholar] [CrossRef] [PubMed]
- Salisbury, C.; Johnson, C.; Purdy, S.; Valderas, J.M.; Montgomery, A. Epidemiology and impact of multimorbidity in primary care: A retrospective cohort study. Br. J. Gen. Pract. 2011, 582, e12–e21. [Google Scholar] [CrossRef]
- Domínguez-Berjón, M.F.; Borrell, C.; Cano-Serral, G.; Esnaola, S.; Nolasco, A.; Pasarín, M.I.; Ramis, R.; Saurina, G.; Escolar-Pujolar, A. Constructing a deprivation index based on census data in large Spanish cities (the MEDEA Project). Gac. Sanit. 2008, 22, 179–187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ingram, E.; Ledden, S.; Beardon, S.; Gomez, M.; Hogarth, S.; McDonald, H.; Osborn, D.P.; Sheringhan, J. Household and area-level social determinants of multimorbidity: A systematic review. J. Epidemiol. Community Health 2020. [Google Scholar] [CrossRef]
- Ellis, E.P. Risk adjustment in competitive health plan markets. In Handbook of Health Economics; Culyer, A.J., Newhouse, J.P., Eds.; Elsevier: Amsterdam, The Netherlands, 2000; Chapter 14; p. 755. [Google Scholar]
- Wagstaff, A.; Paci, P.; Van Doorslaer, E. On the measurement of inequalities in health. Soc. Sci. Med. 1991, 33, 545–557. [Google Scholar] [CrossRef] [Green Version]
- Wagstaff, A. Inequality aversion, health inequality and health achievement. J. Health Econ. 2002, 21, 627–641. [Google Scholar] [CrossRef] [Green Version]
- Van Doorslaer, E.; Wagstaff, A.; Bleichrodt, H.; Calonge, S.; Gerdtham, U.; Gerfin, M.; Geurts, J.; Gross, L.; Häkkinen, U.; Leu, R.L.; et al. Income-related inequalities in health: Some international comparisons. J. Health Econ. 1997, 16, 93–112. [Google Scholar] [CrossRef] [Green Version]
- Orueta, J.F.; García-Álvarez, A.; Alonso-Morán, E.; Vallejo-Torres, L.; Nuño-Solinís, R. Socioeconomic variation in the burden of chronic conditions and health care provision–analyzing administrative individuls level data from the Basque Country, Spain. BMC Public Health 2013, 13, 870. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wagstaff, A. The bounds of the concentration index when the variable of interest is binary, with an application to immunization inequality. Health Econ. 2005, 14, 429–432. [Google Scholar] [CrossRef] [PubMed]
- Van Doorslaer, E.; Koolman, X.; Jones, A.M. Explaining income-related inequalities in doctor utilisation in Europe. Health Econ. 2004, 13, 629–647. [Google Scholar] [CrossRef] [PubMed]
- Gravelle, H. Measuring income related inequality in health: Standardisation of the partial concentration index. Health Econ. 2003, 12, 803–819. [Google Scholar] [CrossRef] [PubMed]
- Biswas, T.; Islam, M.S.; Linton, N.; Rawal, L.B. Socio-Economic Inequality of Chronic Non-Communicable Diseases in Bangladesh. PLoS ONE 2016, 11, e0167140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lai, S.; Shen, C.; Yang, X.; Zhang, X.; Xu, Y.; Li, Q.; Gao, J.; Zhou, Z. Socioeconomic inequalities in the prevalence of chronic diseases and preventive care among adults aged 45 and older in Shaanxi Province, China. BMC Public Health 2019, 19, 1460. [Google Scholar] [CrossRef] [Green Version]
- Bono, F.; Matranga, D. Socioeconomic inequality in non-communicable diseases in Europe between 2004 and 2015: Evidence from the SHARE survey. Eur. J. Public Health 2019, 29, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Cassell, A.; Edwards, D.; Harshfield, A.; Rhodes, K.; Brimicombe, J.; Payne, R.; Griffit, S. The epidemiology of multimorbidity in primary care: A retrospective cohort study. Br. J. Gen. Pract. 2018, 68, e245–e251. [Google Scholar] [CrossRef] [Green Version]
- Garrido-Cumbrera, M.; Borrell, C.; Palència, L.; Espelt, A.; Rodríguez-Sanz, M.; Pasarín, M.I.; Kunst, A. Social class inequalities in the utilization of health care and preventive services in Spain, a country with a national health system. Int. J. Health Serv. 2010, 40, 525–542. [Google Scholar] [CrossRef] [PubMed]
- Regidor, E.; Martínez, D.; Calle, M.E.; Astasio, P.; Ortega, P.; Domínguez, V. Socioeconomic patterns in the use of public and private health services and equity in health care. BMC Health Serv. Res. 2008, 8, 183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diderichsen, F.; Andersen, I.; Manuel, C.; The Working Group of the Danish Review on Social Determinants of Health; Nybo Andersen, A.-M.; Bach, E.; Baadsgard, M.; Brønnum-Hansen, H.; Hansen, F.K.; Jeune, B.; et al. Health Inequality—Determinants and Policies. Scand. J. Public Health 2012, 40, 12–105. [Google Scholar] [CrossRef] [Green Version]
- Iruin-Sanz, A.; Pereira-Rodríguez, C.; Nuño-Solinís, R. The role of geographic context on mental health: Lessons from the implementation of mental health atlases in the Basque Country (Spain). Epidemiol. Psychiatr. Sci. 2015, 24, 42–44. [Google Scholar] [CrossRef]
- Nuño-Solinis, R.; Vázquez-Pérez, P.; Toro-Polanco, N.; Hernández-Quevedo, C. Integrated care: The Basque perspective. Int. J. Healthc. Manag. 2013, 6, 211–216. [Google Scholar] [CrossRef]
- Guthrie, B.; Saultz, J.W.; Freeman, G.K.; Haggerty, J.L. Continuity of care matters. BMJ 2008, 337, a867. [Google Scholar] [CrossRef] [Green Version]
- Santini, Z.I.; Jose, P.E.; Cornwell, E.Y.; Koyanagi, A.; Nielsen, L.; Hinrichsen, C.; Meilstrup, C.; Madsen, K.R.; Koushede, V. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. Lancet Public Health 2020, 5, e62–e70. [Google Scholar] [CrossRef] [Green Version]
- Urtaran-Laresgoiti, M.; Álvarez-Rosete, A.; Nuño-Solinís, R. A system-wide transformation towards integrated care in the Basque Country: A realist evaluation. Int. J. Care Coord. 2018, 21, 98–108. [Google Scholar] [CrossRef]
| Target Population | Anxiety and Other Neurotic, Stress-Related and Somatoform Disorders | Prevalence Ratio per 1000 Population | Depression | Prevalence Ratio per 1000 Population | Dementia | Prevalence Ratio per 1000 Population | Schizophrenia, Affective Psychosis or Bipolar Disorder | Prevalence Ratio per 1000 Population | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | |||||
| All | 2,262,698 | 100 | 242,736 | 100 | 107.277 | 79,838 | 100 | 35.284 | 37,449 | 100 | 16.551 | 15,141 | 100 | 6.692 |
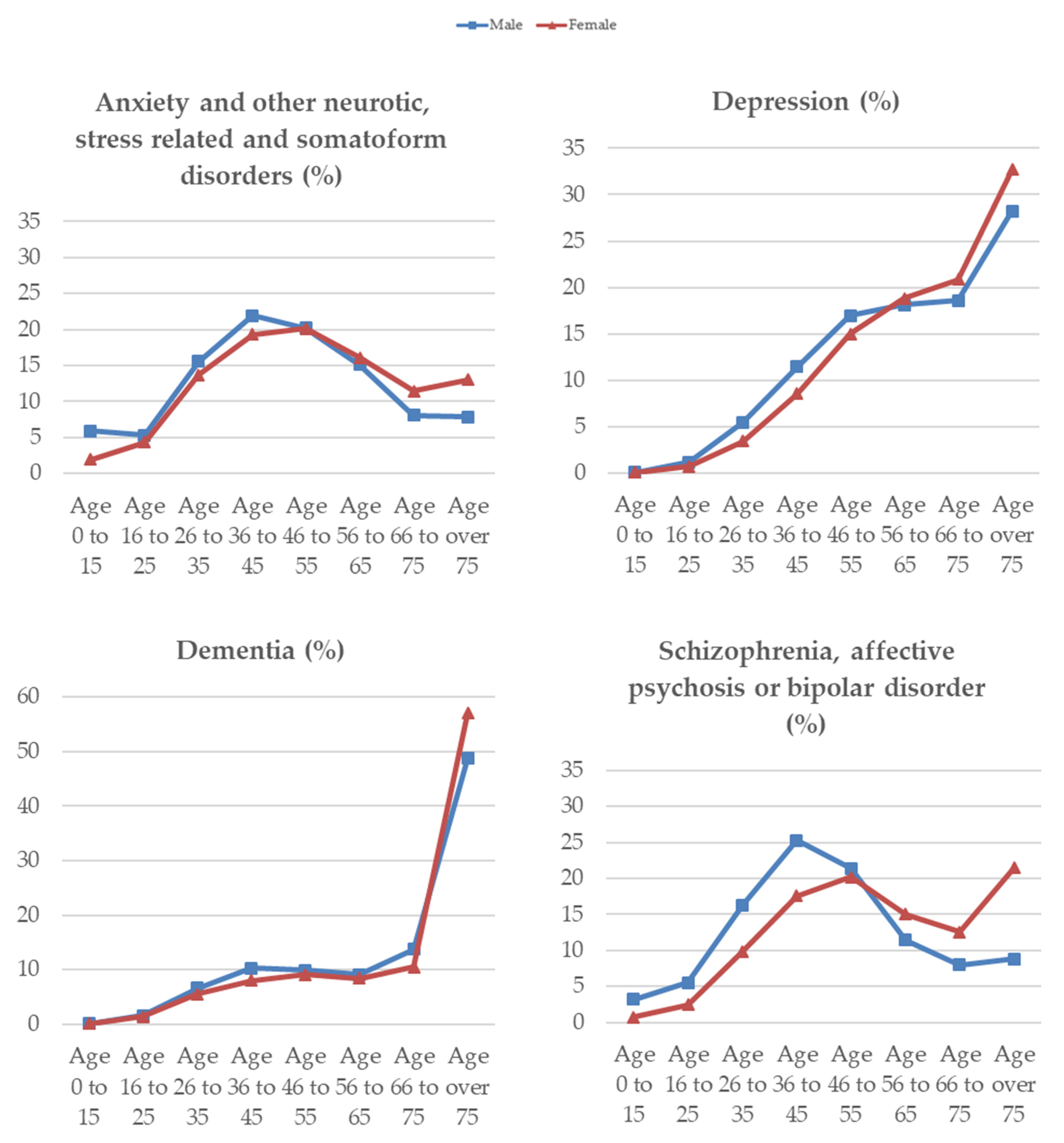
| Sex | ||||||||||||||
| Males | 1,111,050 | 49.10 | 80,755 | 33.27 | 72.683 | 19,944 | 24.98 | 17.951 | 12,308 | 32.87 | 11.078 | 8068 | 53.29 | 7.262 |
| Females | 1,151,648 | 50.90 | 161,981 | 66.73 | 140.651 | 59,894 | 75.02 | 52.007 | 25,141 | 67.13 | 21.830 | 7073 | 46.71 | 6.142 |
| Age groups | ||||||||||||||
| Age 0 to 15 | 305,753 | 7999 | 25 | 38 | 311 | |||||||||
| Males | 157,884 | 51.64 | 4798 | 59.98 | 30.389 | 11 | 44.00 | 0.070 | 16 | 42.11 | 0.101 | 257 | 82.64 | 1.628 |
| Females | 147,689 | 48.30 | 3201 | 40.02 | 21.674 | 14 | 56.00 | 0.095 | 22 | 57.89 | 0.149 | 54 | 17.36 | 0.366 |
| Age 16 to 25 | 192,636 | 11,361 | 625 | 543 | 619 | |||||||||
| Males | 98,802 | 51.29 | 4304 | 37.88 | 43.562 | 231 | 36.96 | 2.338 | 191 | 35.17 | 1.933 | 447 | 72.21 | 4.524 |
| Females | 93,834 | 48.71 | 7057 | 62.12 | 75.207 | 394 | 63.04 | 4.199 | 352 | 64.83 | 3.751 | 172 | 27.79 | 1.833 |
| Age 26 to 35 | 331,211 | 34,734 | 3136 | 2200 | 2016 | |||||||||
| Males | 169,592 | 51.20 | 12,543 | 36.11 | 73.960 | 1092 | 34.82 | 6.439 | 816 | 37.09 | 4.812 | 1316 | 65.28 | 7.760 |
| Females | 161,619 | 48.80 | 22,191 | 63.89 | 137.304 | 2044 | 65.18 | 12.647 | 1384 | 62.91 | 8.563 | 700 | 34.72 | 4.331 |
| Age 36 to 45 | 384,784 | 48,927 | 7377 | 3288 | 3287 | |||||||||
| Males | 197,378 | 51.30 | 17,690 | 36.16 | 89.625 | 2277 | 30.87 | 11.536 | 1270 | 38.63 | 6.434 | 2041 | 62.09 | 10.341 |
| Females | 187,406 | 48.70 | 31,237 | 63.84 | 166.681 | 5100 | 69.13 | 27.214 | 2018 | 61.37 | 10.768 | 1246 | 37.91 | 6.649 |
| Age 46 to 55 | 345,705 | 48,982 | 12,354 | 3495 | 3155 | |||||||||
| Males | 171,859 | 49.71 | 16,328 | 33.33 | 95.008 | 3384 | 27.39 | 19.691 | 1213 | 34.71 | 7.058 | 1727 | 54.74 | 10.049 |
| Females | 173,855 | 50.29 | 32,654 | 66.67 | 187.823 | 8970 | 72.61 | 51.595 | 2282 | 65.29 | 13.126 | 1428 | 45.26 | 8.214 |
| Age 56 to 65 | 275,701 | 38,196 | 14,892 | 3230 | 1986 | |||||||||
| Males | 135,372 | 49.10 | 12,183 | 31.90 | 89.996 | 3613 | 24.26 | 26.689 | 1120 | 34.67 | 8.273 | 922 | 46.42 | 6.811 |
| Females | 140,329 | 50.90 | 26,013 | 68.10 | 185.372 | 11,279 | 75.74 | 80.375 | 2110 | 65.33 | 15.036 | 1064 | 53.58 | 7.582 |
| Age 66 to 75 | 204,458 | 25,129 | 16,148 | 4332 | 1537 | |||||||||
| Males | 95,303 | 46.61 | 6548 | 26.06 | 68.707 | 3709 | 22.97 | 38.918 | 1688 | 38.97 | 17.712 | 646 | 42.03 | 6.778 |
| Females | 109,155 | 53.39 | 18,581 | 73.94 | 170.226 | 12,439 | 77.03 | 113.957 | 2644 | 61.03 | 24.222 | 891 | 57.97 | 8.163 |
| Age over 75 | 222,630 | 27,408 | 25,227 | 20,323 | 2230 | |||||||||
| Males | 84,869 | 41.51 | 6361 | 25.31 | 74.951 | 5627 | 22.31 | 66.302 | 5994 | 29.49 | 70.626 | 712 | 31.93 | 8.389 |
| Females | 137,761 | 67.38 | 21,047 | 83.76 | 152.779 | 19,600 | 77.69 | 142.275 | 14,329 | 70.51 | 104.013 | 1518 | 68.07 | 11.019 |
| Socioeconomic Status (quintiles) | ||||||||||||||
| SES1 (highest) | 479,316 | 43,774 | 15,482 | 7491 | 2851 | |||||||||
| Males | 228,747 | 47.72 | 14,066 | 32.13 | 61.492 | 3976 | 25.68 | 17.382 | 2379 | 31.76 | 10.400 | 1449 | 50.82 | 6.335 |
| Females | 250,569 | 52.28 | 29,708 | 67.87 | 118.562 | 11,506 | 74.32 | 45.919 | 5112 | 68.24 | 20.402 | 1402 | 49.18 | 5.595 |
| SES2 | 487,140 | 50,072 | 16,422 | 7534 | 3034 | |||||||||
| Males | 238,951 | 49.05 | 16,602 | 33.16 | 69.479 | 4168 | 25.38 | 17.443 | 2413 | 32.03 | 10.098 | 1646 | 54.25 | 6.888 |
| Females | 248,189 | 50.95 | 33,470 | 66.84 | 134.857 | 12,254 | 74.62 | 49.374 | 5121 | 67.97 | 20.633 | 1388 | 45.75 | 5.593 |
| SES3 | 457,665 | 50,145 | 16,245 | 7269 | 3088 | |||||||||
| Males | 226,345 | 49.46 | 16,774 | 33.45 | 74.108 | 4054 | 24.96 | 17.911 | 2454 | 33.76 | 10.842 | 1656 | 53.63 | 7.316 |
| Females | 231,320 | 50.54 | 33,371 | 66.55 | 144.263 | 12,191 | 75.04 | 52.702 | 4815 | 66.24 | 20.815 | 1432 | 46.37 | 6.191 |
| SES4 | 422,729 | 47,917 | 15,694 | 7484 | 3030 | |||||||||
| Males | 209,966 | 49.67 | 16,187 | 33.78 | 77.093 | 3952 | 25.18 | 18.822 | 2553 | 34.11 | 12.159 | 1620 | 53.47 | 7.716 |
| Females | 212,763 | 50.33 | 31,730 | 66.22 | 149.133 | 11,742 | 74.82 | 55.188 | 4931 | 65.89 | 23.176 | 1410 | 46.53 | 6.627 |
| SES5 (lowest) | 415,848 | 50,828 | 15,995 | 7671 | 3138 | |||||||||
| Males | 207,041 | 49.79 | 17,126 | 33.69 | 82.718 | 3794 | 23.72 | 18.325 | 2509 | 32.71 | 12.118 | 1697 | 54.08 | 8.196 |
| Females | 208,807 | 50.21 | 33,702 | 66.31 | 161.403 | 12,201 | 76.28 | 58.432 | 5162 | 67.29 | 24.721 | 1441 | 45.92 | 6.901 |
| Health Care Services | All | Anxiety and Other Neurotic, Stress-Related and Somatoform Disorders | Depression | Dementia | Schizophrenia, Affective Psychosis or Bipolar Disorder | No Mental Health Disorders * | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
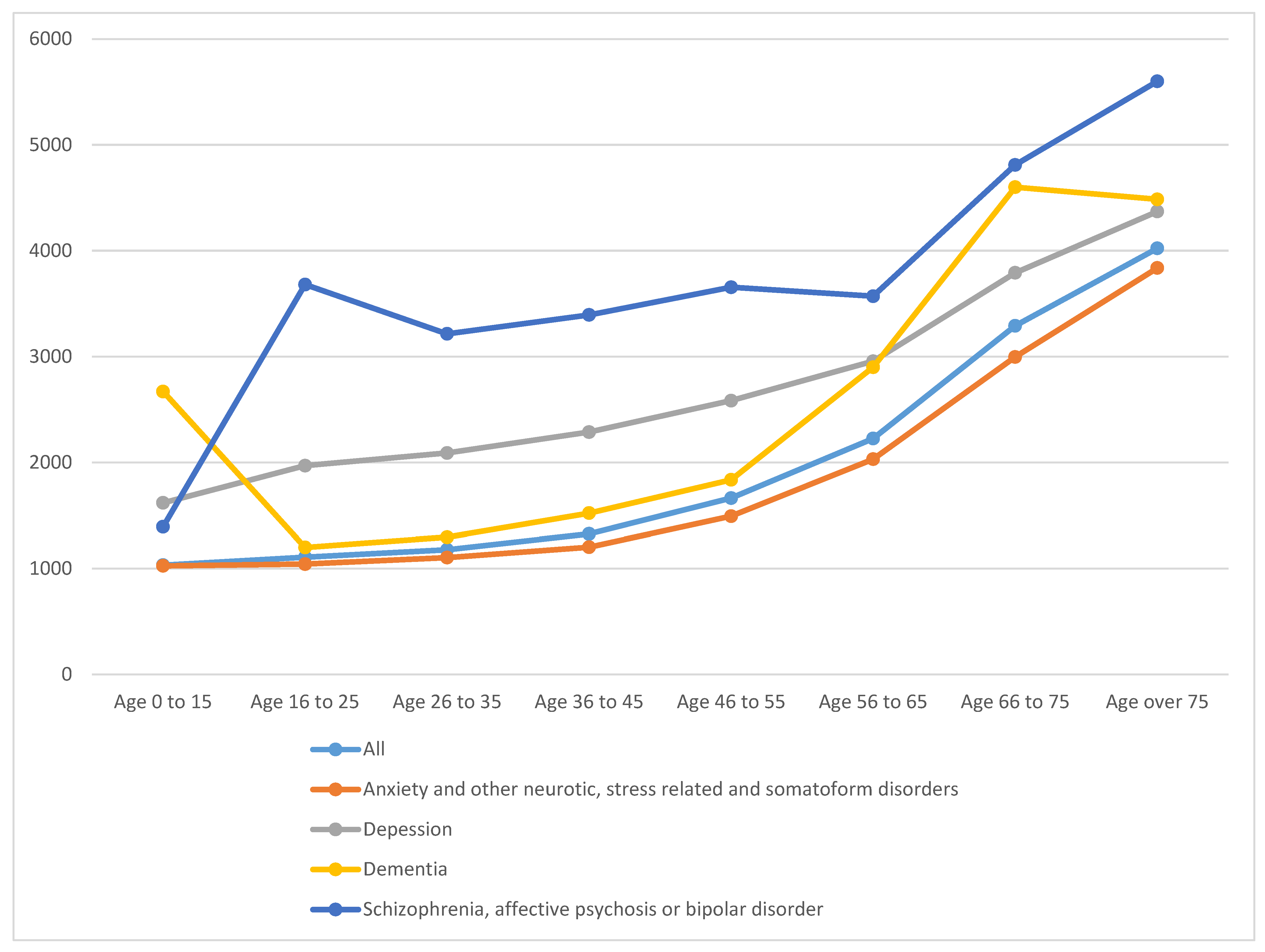
| Mean (€) (Std.Dev.) | % | Mean (€) (Std.Dev.) | % | Mean (€) (Std.Dev.) | % | Mean (€) (Std.Dev.) | % | Mean (€) (Std.Dev.) | % | Mean (€) (Std.Dev.) | % | |
| Primary care | 261.14 (327.62) | 23.05 | 424.19 (385.95) | 22.97 | 636.67 (465.55) | 18.67 | 566.88 (548.94) | 15.67 | 460.06 (473.32) | 11.84 | 229.14 (298.31) | 24.25 |
| Specialist care | 257.08 (999.97) | 22.69 | 454.41 (1168.73) | 24.60 | 639.36 (1488.21) | 18.74 | 491.49 (1410.76) | 13.59 | 932.16 (1676.79) | 23.98 | 219.04 (946.01) | 23.19 |
| Emergency care | 54.20 (142.78) | 4.78 | 85.48 (208.99) | 4.63 | 94.87 (217.99) | 2.78 | 114.78 (244.75) | 3.17 | 135.52 (319.32) | 3.49 | 48.90 (129.38) | 5.17 |
| Inpatient stays in general hospitals | 376.29 (2294.01) | 33.21 | 588.01 (2804.42) | 31.84 | 1092.68 (3874.26) | 32.03 | 1646.42 (4898.19) | 45.52 | 1664.43 (4685.37) | 42.82 | 314.36 (2090.98) | 33.27 |
| Prescription drugs and pharmaceutical products | 175.21 (513.43) | 15.47 | 294.74 (644.16) | 15.96 | 947.40 (1046.47) | 27.78 | 797.90 (1055.04) | 22.06 | 694.65 (1225.34) | 17.87 | 133.50 (433.35) | 14.17 |
| Total Health Care costs | 1132.90 (3152.11) | 100 | 1846.84 (3814.89) | 100.00 | 3410.98 (5140.61) | 100.00 | 3617.47 (6022.26) | 100.00 | 3886.82 (5867.48) | 100.00 | 944.94 (2846.28) | 100.00 |
| Anxiety and Other Neurotic, Stress-Related and Somatoform Disorders | Depression | Dementia | Schizophrenia, Affective Psychosis or Bipolar Disorder | |||||
|---|---|---|---|---|---|---|---|---|
| CI | Std.Dev. | CI | Std.Dev. | CI | Std.Dev. | CI | Std.Dev. | |
| Total (a) | −0.067 * | −54.654 | −0.041 * | −20.074 | −0.030 * | −10.068 | −0.051 * | −10.891 |
| Gender (b) | ||||||||
| Female | −0.071 * | −46.072 | −0.050 * | −21.119 | −0.029 * | 8.275 | −0.049 * | −7.153 |
| Male | −0.064 * | −30.412 | −0.015 * | −3.745 | −0.031 * | −6.000 | −0.053 * | −8.130 |
| Age groups | ||||||||
| 0 to 15 | −0.165 * | −24.293 | −0.241 ** | −1.928 | −0.298 * | −2.830 | −0.111 * | −3.327 |
| 16 to 25 | −0.130 * | −22.851 | −0.096 * | −4.110 | −0.157 * | −6.115 | −0.033 | −1.419 |
| 26 to 35 | −0.104 * | −31.483 | −0.051 * | −4.876 | −0.114 * | −9.043 | −0.051 * | −3.961 |
| 36 to 45 | −0.076 * | −27.213 | −0.071 * | −10.365 | −0.110 * | −10.685 | −0.060 * | −5.950 |
| 46 to 55 | −0.048 * | −17.169 | −0.058 * | −10.918 | −0.080 * | −8.112 | −0.078 * | −7.442 |
| 56 to 65 | −0.044 * | −13.985 | −0.068 * | −13.905 | −0.071 * | −6.914 | −0.078 * | −5.939 |
| 66 to 75 | −0.050 * | −12.982 | −0.037 * | −7.941 | −0.044 * | −5.068 | −0.003 | −0.208 |
| Over 75 | −0.049 * | −13.163 | −0.013 * | −3.322 | 0.011 * | 2.551 | −0.011 | −0.905 |
| All | Anxiety and Other Neurotic, Stress-Related and Somatoform Disorders | Depression | Dementia | Schizophrenia, Affective Psychosis or BipoLar Disorder | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| CI | Std. Err. | CI | Std. Err. | CI | Std. Err. | CI | Std. Err. | CI | Std. Err. | |
| 0 conditions | 0.067 * | 101.342 | ||||||||
| 1 conditions | −0.030 * | −31.373 | 0.045 * | 21.617 | 0.091 * | 11.837 | 0.047 * | 5.964 | 0.044 * | 6.026 |
| 2 conditions | −0.040 * | −31.901 | 0.001 | 0.498 | 0.055 * | 11.160 | 0.035 * | 4.719 | 0.006 | 0.542 |
| 3 conditions | −0.048 * | −30.600 | −0.012 * | −3.511 | 0.015 * | 3.085 | 0.018 * | 2.291 | −0.008 | −0.636 |
| 4 conditions | −0.062 * | −30.119 | −0.032 * | −8.053 | −0.011 ** | −2.097 | 0.003 | 0.352 | −0.015 | −1.081 |
| 5 conditions | −0.069 * | −25.944 | −0.045 * | −9.203 | −0.036 * | −6.117 | −0.027 * | −2.975 | −0.036 ** | −1.961 |
| 6 conditions | −0.075 * | −20.522 | −0.047 * | −7.264 | −0.047 * | −6.583 | −0.041 * | −3.828 | −0.046 ** | −2.023 |
| 7 conditions | −0.085 * | −17.113 | −0.058 * | −6.894 | −0.035 * | −3.859 | −0.041 * | −3.170 | −0.056 ** | −2.029 |
| 8 conditions | −0.084 * | −12.494 | −0.049 * | −4.395 | −0.056 * | −4.883 | −0.029 ** | 1.824 | 0.001 | 0.020 |
| 9 conditions | −0.116 * | −12.468 | −0.114 * | −7.551 | −0.100 * | −6.596 | −0.076 * | −3.898 | −0.084 * | −2.165 |
| 10 or more conditions | −0.121 * | −14.129 | −0.112 * | −7.939 | −0.122 * | −8.504 | −0.112 * | −6.301 | −0.177 * | −5.175 |
| All | Anxiety and Other Neurotic, Stress-Related and Somatoform Disorders | Depression | Dementia | Schizophrenia, Affective Psychosis or Bipolar Disorder | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Observed CI (a) | HI (b) | Observed CI | HI | Observed CI | HI | Observed CI | HI | Observed CI | HI | |
| Primary care | −0.064 * | −0.035 * | −0.035 * | −0.017 * | −0.036 * | −0.021 * | −0.022 * | −0.011 * | −0.035 * | −0.016 * |
| Specialist care | −0.093 * | −0.047 * | −0.052 * | −0.032 * | −0.068 * | −0.046 * | −0.056 * | −0.032 * | −0.048 * | −0.034 * |
| Inpatient stays in general hospitals | −0.097 * | −0.020 | −0.056 * | −0.006 * | −0.057 * | −0.013 * | −0.034 * | −0.009 | −0.046 * | −0.010 * |
| Emergency care | −0.057 * | −0.055 * | −0.066 * | −0.045 * | −0.085 * | −0.057 * | −0.062 * | −0.042 * | −0.061 * | −0.035 |
| Pharmaceuticals | −0.093 * | −0.011 * | −0.046 * | −0.007 * | −0.022 * | −0.003 | 0.001 | 0.004 * | −0.028 * | −0.002 |
| Total HC Costs | −0.086 * | −0.030 * | −0.049 * | −0.017 * | −0.046 * | −0.019 * | −0.028 * | −0.011 * | −0.043 * | −0.016 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Goñi, M.; Stoyanova, A.P.; Nuño-Solinís, R. Mental Illness Inequalities by Multimorbidity, Use of Health Resources and Socio-Economic Status in an Aging Society. Int. J. Environ. Res. Public Health 2021, 18, 458. https://doi.org/10.3390/ijerph18020458
García-Goñi M, Stoyanova AP, Nuño-Solinís R. Mental Illness Inequalities by Multimorbidity, Use of Health Resources and Socio-Economic Status in an Aging Society. International Journal of Environmental Research and Public Health. 2021; 18(2):458. https://doi.org/10.3390/ijerph18020458
Chicago/Turabian StyleGarcía-Goñi, Manuel, Alexandrina P. Stoyanova, and Roberto Nuño-Solinís. 2021. "Mental Illness Inequalities by Multimorbidity, Use of Health Resources and Socio-Economic Status in an Aging Society" International Journal of Environmental Research and Public Health 18, no. 2: 458. https://doi.org/10.3390/ijerph18020458
APA StyleGarcía-Goñi, M., Stoyanova, A. P., & Nuño-Solinís, R. (2021). Mental Illness Inequalities by Multimorbidity, Use of Health Resources and Socio-Economic Status in an Aging Society. International Journal of Environmental Research and Public Health, 18(2), 458. https://doi.org/10.3390/ijerph18020458





