Perinatal Mortality Analysis in Espírito Santo, Brazil, 2008 to 2017
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Location
2.3. Study Population
2.4. Data Collection
2.5. Study Variables
2.6. Statistical Analysis
2.7. Ethical and Legal Aspects of This Research
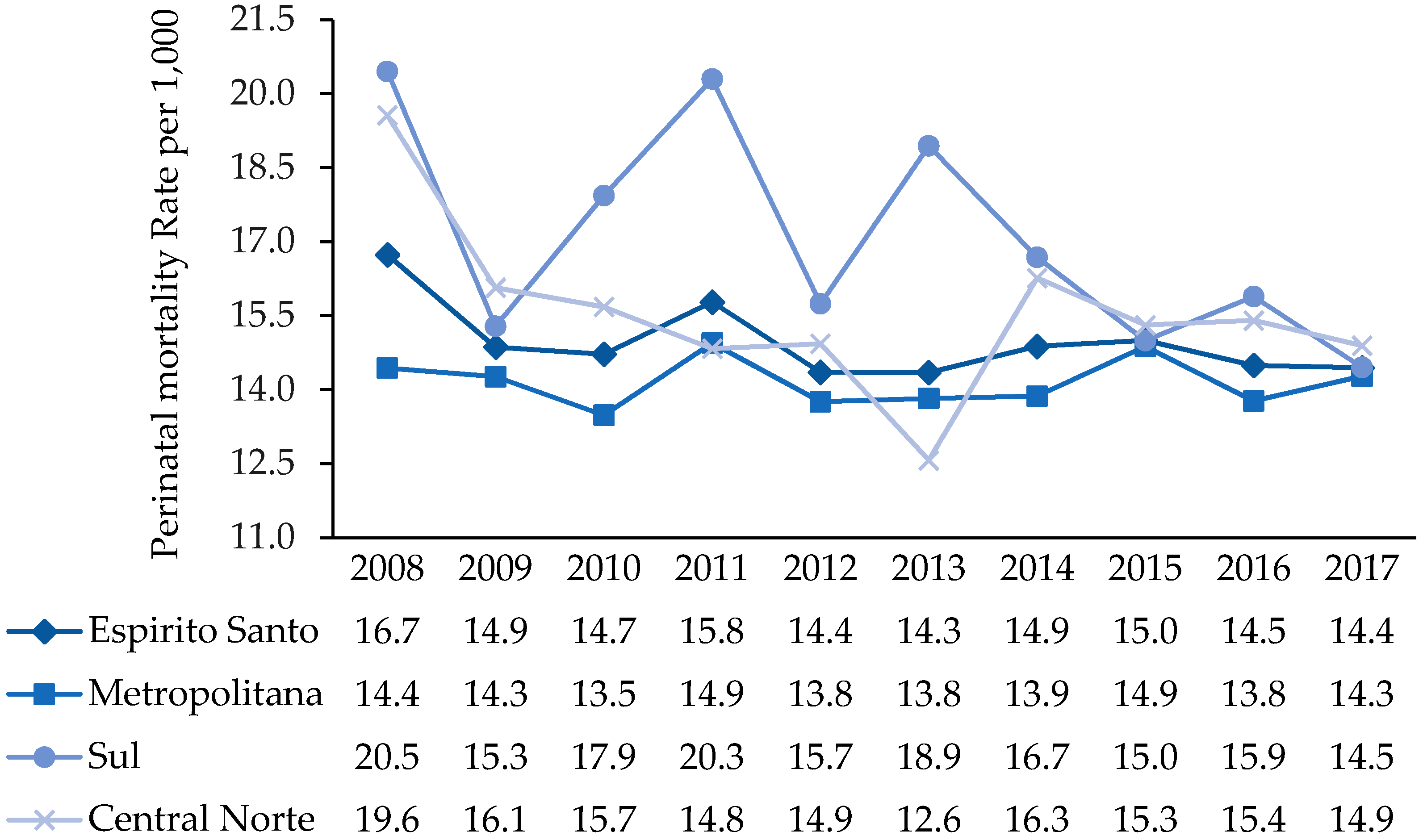
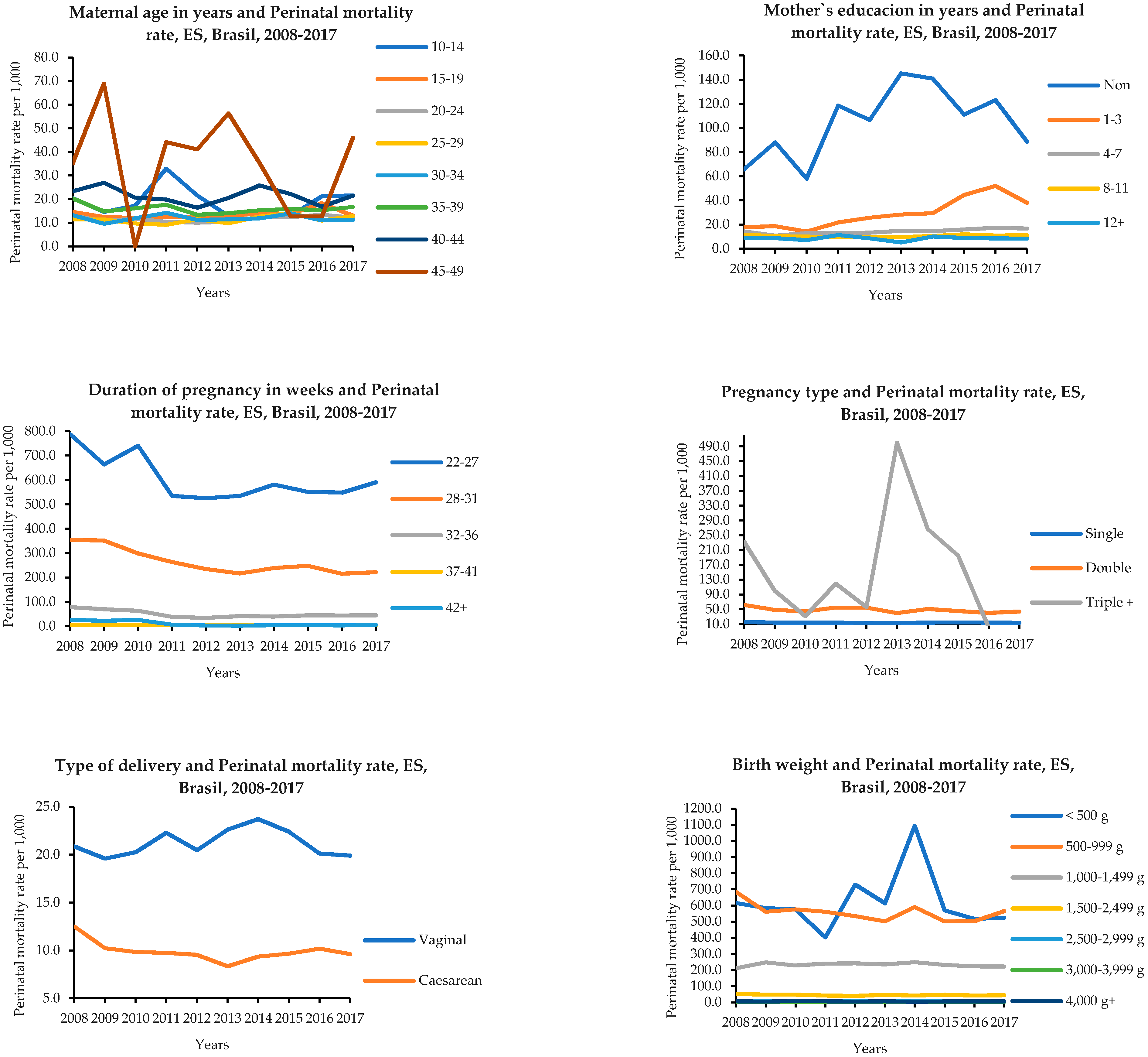
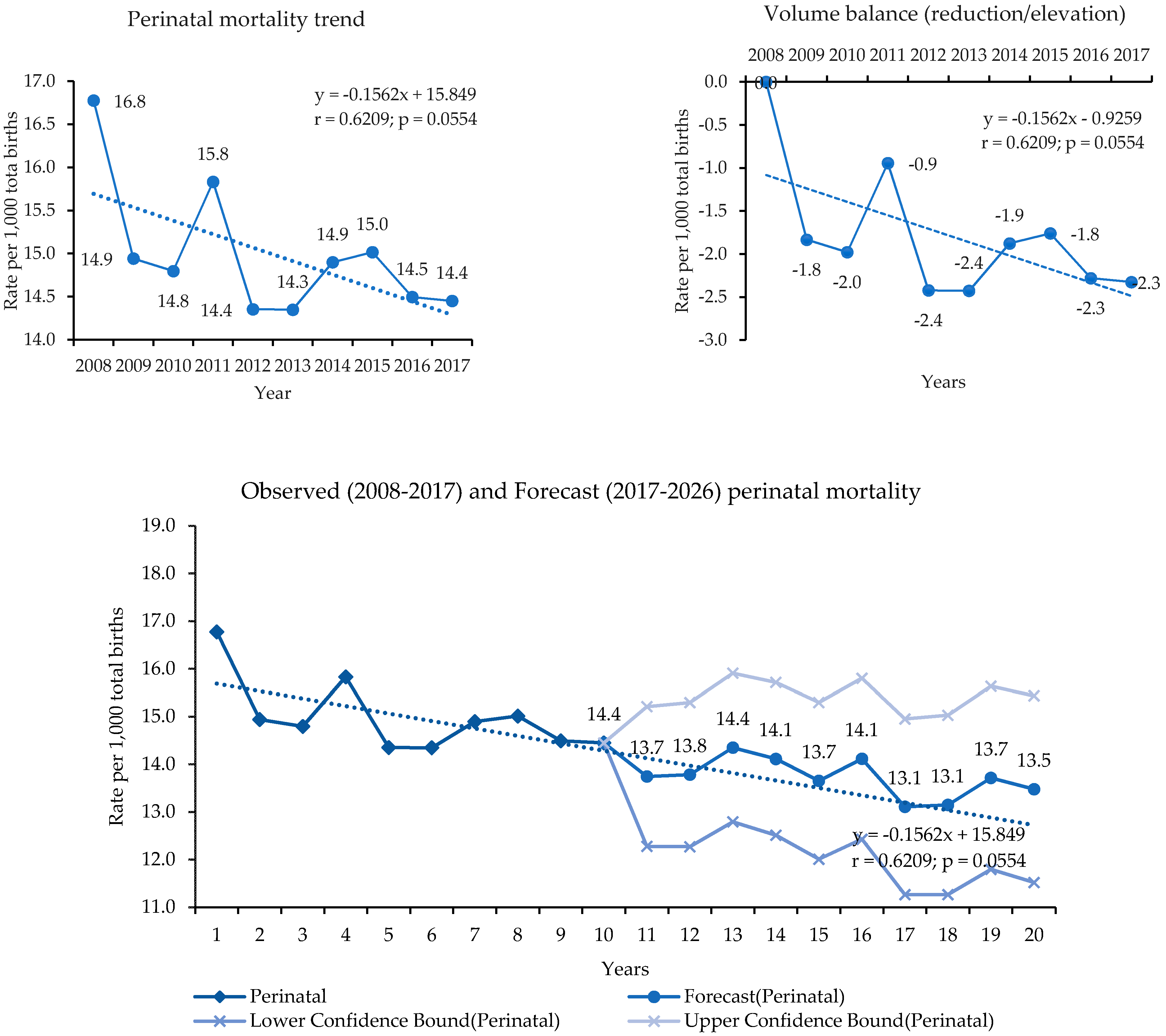
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Masson, V.L.; Farquhar, C.M.; Sadler, L.C. Validation of local review for the identification of contributory factors and potentially avoidable perinatal deaths. Aust. N. Z. J. Obstet. Gynaecol. 2016, 56, 282–288. [Google Scholar] [CrossRef] [PubMed]
- Merali, H.S.; Lipsitz, S.; Hevelone, N.; Gawande, A.A.; Lashoher, A.; Agrawal, P.; Spector, J. Audit-identified avoidable factors in maternal and perinatal deaths in low resource settings: A systematic review. BMC Pregnancy Childbirth 2014, 14, 280. [Google Scholar] [CrossRef]
- Oza, S.; Lawn, J.E.; Hogan, D.R.; Mathers, C.; Cousens, S.N. Neonatal cause-of-death estimates for the early and late neonatal periods for 194 countries: 2000–2013. Bull. World Health Organ. 2015, 93, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Blencowe, H.; Calvert, C.; Lawn, J.E.; Cousens, S.; Campbell, O.M. Measuring maternal, foetal and neonatal mortality: Challenges and solutions. Best Pract. Res. Clin. Obstet. Gynaecol. 2016, 36, 14–29. [Google Scholar] [CrossRef]
- Bhutta, Z.A.; Black, R.E. Global Maternal, Newborn, and Child Health—So Near and Yet So Far. N. Engl. J. Med. 2013, 369, 2226–2235. [Google Scholar] [CrossRef] [PubMed]
- Lawn, J.E.; Blencowe, H.; Oza, S.; You, D.; Lee, A.C.; Waiswa, P.; Lancet Every Newborn Study Group. Every Newborn: Progress, priorities, and potential beyond survival. Lancet 2014, 384, 189–205. [Google Scholar] [CrossRef]
- Prado, D.S.; Mendes, R.B.; Gurgel, R.Q.; Barreto, I.D.D.C.; Cipolotti, R.; Gurgel, R.Q. The influence of mode of delivery on neonatal and maternal short and longterm outcomes. Rev. Saude Publica 2018, 52, 95. [Google Scholar] [CrossRef] [PubMed]
- Moschen, S.A.; Macke, J.; Bebber, S.; da Silva, M.B.C. Sustainable development of communities: ISO 37120 and UN goals. Int. J. Sustain. High. Educ. 2019, 5, 887–900. [Google Scholar] [CrossRef]
- Lee, E.J.; Gambatese, M.; Begier, E.; Soto, A.; Das, T.; Madsen, A. Understanding perinatal death: A systematic analysis of New York City fetal and neonatal death vital record Data and Implications for Improvement, 2007–2011. Matern. Child Health J. 2014, 18, 1945–1954. [Google Scholar] [CrossRef] [PubMed]
- Grove, J.; Claeson, M.; Bryce, J.; Amouzou, A.; Boerma, T.; Waiswa, P.; Victora, C. Maternal, newborn, and child health and the Sustainable Development Goals—A call for sustained and improved measurement. Lancet 2015, 386, 1511–1514. [Google Scholar] [CrossRef]
- Morais Neto, O.L.D.; Barros, M.B.D.A.; Martelli, C.M.T.; Silva, S.A.; Cavenaghi, S.M.; Siqueira Jr, J.B. Diferenças no padrão de ocorrência da mortalidade neonatal e pós-neonatal no Município de Goiânia, Brasil, 1992–1996. Cad. Saúde Pública 2001, 17, 1241–1250. [Google Scholar] [CrossRef]
- Elmusharaf, K. Exclusão social em ambientes de atenção primária: Chegou a hora da medição. J. Hum. Growth Dev. 2019, 29, 10–13. [Google Scholar]
- Martins, E.F.; Rezende, E.M.; Almeida, M.C.D.M.; Lana, F.C.F. Mortalidade perinatal e desigualdades socioespaciais. Rev. Lat. Am. Enfermagem. 2013, 21, 1–9. [Google Scholar] [CrossRef]
- Usynina, A.A.; Grjibovski, A.M.; Krettek, A.; Odland, J.Ø.; Kudryavtsev, A.V.; Anda, E.E. Risk factors for perinatal mortality in Murmansk County, Russia: A registry-based study. Glob. Health Action 2017, 10, 1270536. [Google Scholar] [CrossRef] [PubMed]
- Chinkhumba, J.; De Allegri, M.; Muula, A.S.; Robberstad, B. Maternal and perinatal mortality by place of delivery in sub-Saharan Africa: A meta-analysis of population-based cohort studies. BMC Public Health 2014, 14, 1–9. [Google Scholar] [CrossRef]
- Knight, H.E.; Cromwell, D.A.; Gurol-Urganci, I.; Harron, K.; van der Meulen, J.H.; Smith, G.C. Perinatal mortality associated with induction of labour versus expectant management in nulliparous women aged 35 years or over: An English national cohort study. PLoS Med. 2017, 14, 1–14. [Google Scholar] [CrossRef]
- Hoffmann, C.B.P.C.; Schultz, L.F.; Vaichulonis, C.G.; do Nascimento, I.B.; João, C.G.; Borges, D.C.; Silva, J.C. Perinatal mortality: Epidemiological profile, causes and avoidable factors at a reference public maternity hospital in the State of Santa Catarina, Brazil, 2011–2015. J. Perinat. Med. 2020, 48, 162–167. [Google Scholar] [CrossRef]
- Vogel, J.P.; Souza, J.P.; Mori, R.; Morisaki, N.; Lumbiganon, P.; Laopaiboon, M.; WHO Multicountry Survey on Maternal and Newborn Health Research Network. Maternal complications and perinatal mortality: Findings of the World Health Organization Multicountry Survey on Maternal and Newborn Health. BJOG 2014, 121, 76–88. [Google Scholar] [CrossRef] [PubMed]
- Gardosi, J.; Madurasinghe, V.; Williams, M.; Malik, A.; Francis, A. Maternal and fetal risk factors for stillbirth: Population based study. BMJ 2013, 346, 1–14. [Google Scholar] [CrossRef]
- Rodrigues, E.C.; Alves, B.D.C.A.; Veiga, G.L.D.; Adami, F.; Carlesso, J.S.; Figueiredo, F.W.D.S.; Fonseca, A.L.A. Neonatal mortality in Luanda, angola: What can be done to reduce it? J. Hum. Growth Dev. 2019, 29, 161–168. [Google Scholar] [CrossRef]
- Ministério da Saúde. Secretaria de Vigilância em Saúde. Secretaria de Atenção à Saúde. Manual de Vigilância do Óbito Infantil e Fetal e do Comitê de Prevenção do Óbito Infantil e Fetal, 2nd ed. Brasília. 2009. Available online: http://bvsms.saude.gov.br/bvs/publicacoes/manual_obito_infantil_fetal_2ed.pdf (accessed on 22 June 2020).
- Rasella, D.; Aquino, R.; Santos, C.A.; Paes-Sousa, R.; Barreto, M.L. Effect of a conditional cash transfer programme on childhood mortality: A nationwide analysis of Brazilian municipalities. Lancet 2013, 382, 57–64. [Google Scholar] [CrossRef]
- Tomasi, E.; Fernandes, P.A.A.; Fischer, T.; Siqueira, F.C.V.; Silveira, D.S.D.; Thumé, E.; Facchini, L.A. Qualidade da atenção pré-natal na rede básica de saúde do Brasil: Indicadores e desigualdades sociais. Cad. Saude Publica 2017, 33, 1–11. [Google Scholar] [CrossRef]
- Morris, N.M.; Udry, J.R.; Chase, C.L. Shifting age parity distribution of births and the decrease in infant mortality. Am. J. Public Health 1975, 65, 359–362. [Google Scholar] [CrossRef]
- Tomasi, E.; Barros, F.C.; Victora, C.G. As mães e suas gestações: Comparação de duas coortes de base populacional no Sul do Brasil. Cad. Saude Publica 1996, 12, S21–S25. [Google Scholar] [CrossRef][Green Version]
- Horta, B.L.; Barros, F.C.; Halpern, R.; Victora, C.G. Baixo peso ao nascer em duas coortes de base populacional no Sul do Brasil. Cad. Saude Publica 1996, 12, S27–S31. [Google Scholar] [CrossRef]
- Bickler, G.; Morton, S.; Menne, B. Health and sustainable development: An analysis of 20 European voluntary national reviews. Public Health 2020, 180, 180–184. [Google Scholar] [CrossRef] [PubMed]
- Ntambue, A.M.; Malonga, F.K.; Dramaix-Wilmet, M.; Ngatu, R.N.; Donnen, P. Better than nothing? maternal, newborn, and child health services and perinatal mortality, Lubumbashi, democratic republic of the Congo: A cohort study. BMC Pregnancy Childbirth 2016, 16, 89. [Google Scholar] [CrossRef] [PubMed]
- MacDorman, M.F.; Gregory, E.C.W. Fetal and Perinatal Mortality: United States, 2013. Natl. Vital Stat. Rep. 2015, 64, 1–24. [Google Scholar]
- Donoso, S.E. ¿Está aumentando la mortalidad perinatal en Chile? Rev. Chil. Obstet. Ginecol. 2011, 76, 377–379. [Google Scholar] [CrossRef]
- Bernal, C.D.P.; Cardona, R.D. Caracterización de la mortalidad perinatal en Manizales, Colombia 2009–2012. Hacia Promoc. Salud 2014, 19, 2009–2012. [Google Scholar]
- Rafael, R.A.; Ribeiro, V.S.; Cavalcante, M.C.; Santos, A.M.; Simões, V.M. Probabilistic record linkage: Recovery of data on infant deaths and stillbirths in Maranhão State, Brazil. Cad. Saude Publica 2011, 27, 1371–1379. [Google Scholar] [CrossRef] [PubMed]
- de Medeiros, V.A.B.; dos Santos Bezerra, I.N.; Monteiro, F.S.; de Melo Mota, L. Perfil da mortalidfade neonatal em alagoas no período de 2008 a 2017. Rev. Ciênc. Plur. 2019, 5, 16–31. [Google Scholar] [CrossRef]
- Rêgo, M.G.D.S.; Vilela, M.B.R.; Oliveira, C.M.D.; Bonfim, C.V.D. System of Brazil Muertes perinatales evitables por intervención del Sistema de. Rev. Gaúcha Enferm. 2018, 39, 2017-0084. [Google Scholar]
- Vieira, M.S.M.; Vieira, F.M.; Fröde, T.S.; d’Orsi, E. Fetal Deaths in Brazil: Historical Series Descriptive Analysis 1996–2012. Matern. Child Health J. 2016, 20, 1634–1650. [Google Scholar] [CrossRef]
- Barbeiro, F.M.D.S.; Fonseca, S.C.; Tauffer, M.G.; Ferreira, M.D.S.S.; Silva, F.P.D.; Ventura, P.M.; Quadros, J.I. Fetal deaths in Brazil: A systematic review. Rev. Saude Publica 2015. ahead of print. [Google Scholar] [CrossRef]
- Victora, C.G.; Aquino, E.M.; do Carmo Leal, M.; Monteiro, C.A.; Barros, F.C.; Szwarcwald, C.L. Maternal and child health in Brazil: Progress and challenges. Lancet 2011, 377, 1863–1876. [Google Scholar] [CrossRef]
- Cockerill, R.; Whitworth, M.K.; Heazell, A.E.P. Do medical certificates of stillbirth provide accurate and useful information regarding the cause of death? Paediatr. Perinat. Epidemiol. 2012, 26, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Willcox, M.L.; Price, J.; Scott, S.; Nicholson, B.D.; Stuart, B.; Roberts, N.W.; Harnden, A. Death audits and reviews for reducing maternal, perinatal and child mortality. Cochrane Database Syst. Rev. 2020. [Google Scholar] [CrossRef]
- Melo, C.M.D.; Aquino, T.I.S.; Soares, M.Q.; Bevilacqua, P.D. Vigilância do óbito como indicador da qualidade da atenção à saúde da mulher e da criança. Cienc. Saude Coletiva 2017, 22, 3457–3465. [Google Scholar] [CrossRef]
- Silva, V.L.S.D.; Santos, I.S.; Medronha, N.S.; Matijasevich, A. Mortalidade infantil na cidade de Pelotas, estado do Rio Grande do Sul, Brasil, no período 2005-2008: Uso da investigação de óbitos na análise das causas evitáveis. Epidemiol. Serv. Saúde 2012, 21, 265–274. [Google Scholar] [CrossRef]
- Lansky, S. Gestão da qualidade e da integralidade do cuidado em saúde para a mulher e a criança no SUS-BH: A experiência da comissão perinatal. Rev. Tempus Actas Saúde Coletiva 2010, 4, 191–199. [Google Scholar]
- Lassi, Z.S.; Bhutta, Z.A. Community-based intervention packages for reducing maternal and neonatal morbidity and mortality and improving neonatal outcomes. Cochrane Database Syst. Rev. 2015. ahead of print. [Google Scholar] [CrossRef]
- Berhan, Y.; Berhan, A. A meta-analysis of selected maternal and fetal factors for perinatal mortality. Ethiop. J. Health Sci. 2014, 24, 55–68. [Google Scholar] [CrossRef] [PubMed]
- Mboya, I.B.; Mahande, M.J.; Obure, J.; Mwambi, H.G. Predictors of perinatal death in the presence of missing data: A birth registry-based study in northern Tanzania. PLoS ONE 2020, 15, e0231636. [Google Scholar] [CrossRef]
- Tesfalul, M.A.; Natureeba, P.; Day, N.; Thomas, O.; Gaw, S.L. Identifying risk factors for perinatal death at Tororo District Hospital, Uganda: A case-control study. BMC Pregnancy Childbirth 2020, 20, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Venâncio, T.S.; Tuan, T.S.; Vaz, F.P.C.; Nascimento, L.F.C. Análise espacial da mortalidade perinatal no estado de São Paulo, de 2003 a 2012. Rev. Bras. Ginecol. Obs. 2016, 38, 492–498. [Google Scholar] [CrossRef]
- Berhan, Y.; Berhan, A. Causes of maternal mortality in Ethiopia: A significant decline in abortion related death. Ethiop. J. Health Sci. 2014, 24, 15–28. [Google Scholar] [CrossRef]
- Rêgo, M.G.D.S.; Vilela, M.B.R.; Oliveira, C.M.D.; Bonfim, C.V.D. Óbitos perinatais evitáveis por intervenções do Sistema Único de Saúde do Brasil. Rev. Gauch. Enferm. 2018, 39, e20170084. [Google Scholar] [CrossRef]
- Lansky, S.; França, E.; Leal, M.C. Perinatal mortality and evitability: A review. Rev. Saude Publica 2002, 36, 759–772. [Google Scholar] [CrossRef]
- França, E.B.; Lansky, S.; Rego, M.A.S.; Malta, D.C.; França, J.S.; Teixeira, R.; Vasconcelos, A.M.N. Principais causas da mortalidade na infância no Brasil, em 1990 e 2015: Estimativas do estudo de Carga Global de Doença. Rev. Bras. Epidemiol. 2017, 20, 46–60. [Google Scholar] [CrossRef] [PubMed]
- Ventura, R.N.; Oliveira, E.M.D.; Silva, E.M.K.D.; Silva, N.N.D.; Puccini, R.F. Condições de vida e mortalidade infantil no município do Embu, São Paulo. Rev. Paul. Pediatr. 2008, 26, 251–257. [Google Scholar] [CrossRef]
- Duarte, G.; Coltro, P.S.; Bedone, R.V.; Nogueira, A.A.; Gelonezzi, G.M.; Franco, L.J. Trends in the modes of delivery and their impact on perinatal mortality rates. Rev. Saude Publica 2004, 38, 379–384. [Google Scholar] [CrossRef] [PubMed]
- Malta, D.C.; Duarte, E.C. Causas de mortes evitáveis por ações efetivas dos serviços de saúde: Uma revisão da literatura. Cienc. Saude Coletiva 2007, 12, 765–776. [Google Scholar] [CrossRef] [PubMed]
- Ministério da Saúde, MDS. Manual de Vigilância do Óbito Infantil e Fetal e do Comitê de Prevenção do Óbito Infantil e Fetal, 2nd ed.; Ministério da Saúde: Brasília, Brasil, 2009.
- Fonseca, S.C.; Coutinho, E.D.S.F. Características biológicas e evitabilidade de óbitos perinatais em uma localidade na cidade do Rio de Janeiro, 1999 a 2003. Rev. Bras. Saude Matern. Infant. 2008, 8, 171–178. [Google Scholar] [CrossRef]
- Lansky, S.; França, E.; Leal, M.C. Mortalidade perinatal e evitabilidade: Revisão da literatura. Rev. Saude Publica 2002, 36, 759–772. [Google Scholar]
- Malta, D.C.; Duarte, E.C.; Almeida, M.F.D.; Dias, M.A.D.S.; Morais Neto, O.L.D.; Moura, L.D.; Souza, M.D.F.M.D. List of avoidable causes of deaths due to interventions of the Brazilian Health System. Epidemiol. Serv. Saúde 2007, 4, 233–244. [Google Scholar] [CrossRef]
- Schoeps, D.; Almeida, M.F.D.; Alencar, G.P.; França Jr, I.; Novaes, H.M.D.; Siqueira, A.A.F.D.; Rodrigues, L.C. Risk factors for early neonatal mortality. Rev. Saude Publica 2007, 41, 1013–1022. [Google Scholar] [CrossRef]
- Cunha, A.C.; Nascimento, M.I. Natimorto: Uma revisão dos Sistemas de Classificação TT—Stillbirth: A Review of the Classification Systems. Femina. 2015. Available online: http://www.bireme.br (accessed on 19 October 2019).
- Laurenti, R.; Buchalla, C.M.; Costa, M.L., Jr. Estudo da morbidade e da mortalidade perinatal em maternidades. I-Descrição do projeto e resultados gerais. Rev. Saude Publica 1984, 18, 436–447. [Google Scholar] [CrossRef]
- Shukla, V.V.; Carlo, W.A. Review of the evidence for interventions to reduce perinatal mortality in low- and middle-income countries. Int. J. Pediatr. Adolesc. Med. 2020, 7, 2–8. [Google Scholar] [CrossRef]

| Years | Natality | Mortality (per 1000) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Live Births | Fetal | Early Neonatal | Perinatal | |||||||||
| f | % | R | f | %* | R | f | %* | R | f | % | R | |
| 2008 | 51,852 | 9.6 | 14.8 | 487 | 55.5 | 9.3 | 391 | 44.5 | 7.5 | 878 | 10.8 | 16.8 |
| 2009 | 51,457 | 9.6 | 14.6 | 487 | 62.8 | 9.4 | 289 | 37.2 | 5.6 | 776 | 9.5 | 14.9 |
| 2010 | 51,853 | 9.6 | 14.8 | 461 | 59.6 | 8.8 | 313 | 40.4 | 6.0 | 774 | 9.5 | 14.8 |
| 2011 | 53,053 | 9.9 | 15.1 | 520 | 61.3 | 9.7 | 328 | 38.7 | 6.2 | 848 | 10.4 | 15.8 |
| 2012 | 52,835 | 9.8 | 15.0 | 474 | 62.0 | 8.9 | 291 | 38.0 | 5.5 | 765 | 9.4 | 14.4 |
| 2013 | 54,065 | 10.1 | 15.4 | 512 | 65.4 | 9.4 | 271 | 34.6 | 5.0 | 783 | 9.6 | 14.3 |
| 2014 | 56,548 | 10.5 | 16.1 | 505 | 59.4 | 8.9 | 345 | 40.6 | 6.1 | 850 | 10.5 | 14.9 |
| 2015 | 56,941 | 10.6 | 16.2 | 535 | 62.0 | 9.3 | 328 | 38.0 | 5.8 | 863 | 10.6 | 15.0 |
| 2016 | 53,413 | 9.9 | 15.2 | 470 | 60.2 | 8.7 | 311 | 39.8 | 5.8 | 781 | 9.6 | 14.5 |
| 2017 | 55,846 | 10.4 | 15.9 | 488 | 60.0 | 8.7 | 326 | 40.0 | 5.8 | 814 | 10.0 | 14.4 |
| Total | 537,863 | 100.0 | 153.0 | 4.939 | 60.7 | 9.1 | 3.193 | 39.3 | 5.9 | 8132 | 100.0 | 15.0 |
| Characteristics | Mortality Rates per Thousand and Proportional (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Fetal | Early Neonatal | Perinatal | ||||||||
| LBs | f | FMR | % | f | ENMR | % | f | PMR | % | |
| Mother’s age (years) | ||||||||||
| 10 to 19 | 92,862 | 707 | 7.6 | 14.3 | 583 | 6.2 | 18.3 | 1290 | 13.8 | 15.9 |
| 20 to 29 | 273,829 | 1875 | 6.8 | 38.0 | 1296 | 4.7 | 40.6 | 3171 | 11.5 | 39.0 |
| 30 to 39 | 159,129 | 1333 | 8.3 | 27.0 | 787 | 4.9 | 24.6 | 2120 | 13.2 | 26.1 |
| 40 to 49 | 11,988 | 193 | 15.8 | 3.9 | 76 | 6.3 | 2.4 | 269 | 22.1 | 3.3 |
| 50+ | 52 | 0 | 0.0 | 0.0 | 1 | 19.2 | 0.0 | 1 | 19.2 | 0.0 |
| Ignored | 3 | 831 | 996.4 | 16.8 | 450 | 150,000 | 14.1 | 1281 | 153.6 | 15.8 |
| Mother’s education (years) | ||||||||||
| Non | 2026 | 120 | 55.9 | 2.4 | 87 | 42.9 | 2.7 | 207 | 96.5 | 2.5 |
| 1 to 3 | 15,861 | 272 | 16.9 | 5.5 | 130 | 8.2 | 4.1 | 402 | 24.9 | 4.9 |
| 4 to 7 | 122,975 | 1087 | 8.8 | 22.0 | 657 | 5.3 | 20.6 | 1744 | 14.1 | 21.4 |
| 8 to 11 | 290,732 | 1796 | 6.1 | 36.4 | 1269 | 4.4 | 39.7 | 3065 | 10.5 | 37.7 |
| 12+ | 95,399 | 451 | 4.7 | 9.1 | 357 | 3.7 | 11.2 | 808 | 8.4 | 9.9 |
| Ignored | 10,870 | 1212 | 100.3 | 24.5 | 693 | 63.8 | 21.7 | 1905 | 157.7 | 23.4 |
| Duration of pregnancy (weeks) | ||||||||||
| 22 to 27 | 2356 | 1054 | 309.1 | 21.3 | 1009 | 428.3 | 31.6 | 2063 | 605.0 | 25.4 |
| 28 to 31 | 4599 | 941 | 169.9 | 19.1 | 482 | 104.8 | 15.1 | 1423 | 256.9 | 17.5 |
| 32 to 36 | 39,755 | 1348 | 32.8 | 27.3 | 565 | 14.2 | 17.7 | 1913 | 46.5 | 23.5 |
| 37 to 41 | 470,370 | 1168 | 2.5 | 23.6 | 756 | 1.6 | 23.7 | 1924 | 4.1 | 23.7 |
| 42+ | 10,428 | 30 | 2.9 | 0.6 | 26 | 2.5 | 0.8 | 56 | 5.4 | 0.7 |
| Ignored | 10,355 | 398 | 37.0 | 8.1 | 355 | 34.3 | 11.1 | 753 | 70 | 9.3 |
| Pregnancy type | ||||||||||
| Single | 526,338 | 4467 | 8.4 | 90.4 | 2641 | 5.0 | 82.7 | 7108 | 13.4 | 87.4 |
| Double | 10,748 | 243 | 22.1 | 4.9 | 281 | 26.1 | 8.8 | 524 | 47.7 | 6.4 |
| Triple/more | 237 | 17 | 66.9 | 0.3 | 17 | 71.7 | 0.5 | 34 | 133.9 | 0.4 |
| Ignored | 540 | 212 | 281.9 | 4.3 | 254 | 470.4 | 8.0 | 466 | 619.7 | 5.7 |
| Delivery | ||||||||||
| Vaginal | 199,065 | 2917 | 14.4 | 59.1 | 1359 | 6.8 | 42.6 | 4276 | 21.2 | 52.6 |
| Caesarean | 338,081 | 1788 | 5.3 | 36.2 | 1560 | 4.6 | 48.9 | 3348 | 9.9 | 41.2 |
| Ignored | 717 | 234 | 246.1 | 4.7 | 274 | 382.1 | 8.6 | 508 | 534.2 | 6.2 |
| Place of occurrence | ||||||||||
| Hospital | 529,450 | 4537 | 8.5 | 91.9 | 3101 | 5.9 | 97.1 | 7638 | 14.3 | 93.9 |
| Other health centers | 7347 | 177 | 23.5 | 3.6 | 37 | 5.0 | 1.2 | 214 | 28.4 | 2.6 |
| Home | 701 | 139 | 165.5 | 2.8 | 22 | 31.4 | 0.7 | 161 | 191.7 | 2.0 |
| Public highway | 0 | 11 | 1000 | 0.2 | 12 | 0.0 | 0.4 | 23 | 2090.9 | 0.3 |
| Other | 341 | 39 | 102.6 | 0.8 | 16 | 46.9 | 0.5 | 55 | 144.7 | 0.7 |
| Ignored | 24 | 36 | 600.0 | 0.7 | 5 | 208.3 | 0.2 | 41 | 683.3 | 0.5 |
| Total | 537,863 | 4939 | 9.1 | 100.0 | 3193 | 5.9 | 100.0 | 8132 | 15.0 | 100.0 |
| Characteristics | Mortality Rate per Thousand and Proportional (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| (Fetus and Newborn) | Fetal | Early Neonatal | Perinatal | |||||||
| LBs | f | FMR | %* | f | ENMR | %* | f | PMR | % | |
| Sex | ||||||||||
| Male | 276,029 | 2521 | 9.1 | 51.0 | 1783 | 6.5 | 55.8 | 4304 | 15.5 | 52.9 |
| Female | 261,773 | 2169 | 8.2 | 43.9 | 1380 | 5.3 | 43.2 | 3549 | 13.4 | 43.6 |
| Ignored | 61 | 249 | 803.2 | 5.0 | 30 | 491.8 | 0.9 | 279 | 900.0 | 3.4 |
| Color/race | ||||||||||
| White | 162,982 | 39 | 0.2 | 0.8 | 1067 | 6.5 | 33.4 | 1106 | 6.8 | 13.6 |
| Black | 21,801 | 13 | 0.6 | 0.3 | 61 | 2.8 | 1.9 | 74 | 3.4 | 0.9 |
| Yellow | 829 | 0 | 0.0 | 0.0 | 5 | 6.0 | 0.2 | 5 | 6.0 | 0.1 |
| Mixed | 336,260 | 130 | 0.4 | 2.6 | 1481 | 4.4 | 46.4 | 1611 | 4.8 | 19.8 |
| Indigenous | 1169 | 0 | 0.0 | 0.0 | 8 | 6.8 | 0.3 | 8 | 6.2 | 0.1 |
| Ignored | 14,822 | 4757 | 243.0 | 96.3 | 571 | 38.5 | 17.9 | 5328 | 272.1 | 65.5 |
| Birth weight | ||||||||||
| <500 g | 436 | 142 | 245.7 | 2.9 | 201 | 461.0 | 6.3 | 343 | 593.4 | 4.2 |
| 500 to 999 g | 2392 | 998 | 294.4 | 20.2 | 888 | 371.2 | 27.8 | 1886 | 556.3 | 23.2 |
| 1000 to 1499 g | 3865 | 655 | 144.9 | 13.3 | 398 | 103.0 | 12.5 | 1053 | 233.0 | 12.9 |
| 1500 to 2499 g | 35,956 | 1104 | 29.8 | 22.4 | 560 | 15.6 | 17.5 | 1664 | 44.9 | 20.5 |
| 2500 to 2999 g | 114,449 | 485 | 4.2 | 9.8 | 329 | 2.9 | 10.3 | 814 | 7.1 | 10.0 |
| 3000 to 3999 g | 349,382 | 525 | 1.5 | 10.6 | 424 | 1.2 | 13.3 | 949 | 2.7 | 11.7 |
| 4000 g+ | 31,343 | 111 | 3.5 | 2.2 | 57 | 1.8 | 1.8 | 168 | 5.3 | 2.1 |
| Ignored | 40 | 919 | 958.3 | 18.6 | 336 | 8400.0 | 10.5 | 1255 | 1308.7 | 15.4 |
| Total | 537,863 | 4939 | 9.1 | 100.0 | 3193 | 5.9 | 100.0 | 8132 | 15.0 | 100.0 |
| Factors (NB, Pregnancy, Delivery, and Maternal) (NB, Maternal/Pregnancy) | 2008–2017 | ||||
|---|---|---|---|---|---|
| PD | TBs | PMR | RR (95% CI) | p-Value | |
| Sex | |||||
| Male | 4304 | 278,550 | 15.5 | 1.15 (1.10:1.20) | <0.00001 |
| Female | 3549 | 263,942 | 13.4 | 1.00 | (Reference) |
| Race/skin color | |||||
| Black | 74 | 21,814 | 3.4 | 0.50 (0.39:0.63) | <0.00001 |
| Mixed | 1611 | 336,390 | 4.8 | 0.71 (0.65:0.76) | <0.00001 |
| White | 1106 | 163,021 | 6.8 | 1.00 | (Reference) |
| Pregnancy type | |||||
| Double | 524 | 10,991 | 47.7 | 3.56 (3.25:3.90) | <0.00001 |
| Triple/more | 34 | 254 | 133.9 | 10.00 (6.98:14.31) | <0.00001 |
| Single | 7108 | 530,805 | 13.4 | 1.00 | (Reference) |
| Delivery type | |||||
| Cesarean | 3348 | 339,869 | 9.9 | 0.47 (0.44:0.49) | <0.00001 |
| Vaginal | 4276 | 201,882 | 21.2 | 1.00 | (Reference) |
| Birth weight (grams) | |||||
| <1.500 | 3282 | 8488 | 386.66 | 99.38 (93.58:105.54) | <0.00001 |
| 1.500 to 2.499 | 1664 | 37,060 | 44.90 | 11.54 (10.80:12.33) | <0.00001 |
| ≥2.500 | 1931 | 496,295 | 3.89 | 1.00 | (Reference) |
| Gestational age (weeks) | |||||
| <37 | 5399 | 50,053 | 107.9 | 26.44 (25.08:27.87) | <0.00001 |
| 37–41 | 1924 | 471,538 | 4.1 | 1.00 | (Reference) |
| ≥42 | 56 | 10,458 | 5.4 | 1.31 (1.01:1.71) | <0.00001 |
| Mother’s age (years) | |||||
| <19 | 1290 | 93,569 | 13.8 | 1.20 (1.12:1.28) | <0.00001 |
| 20–29 | 3171 | 275,704 | 11.5 | 1.00 | (Reference) |
| ≥29 | 2389 | 172,695 | 13.8 | 1.20 (1.14:1.27) | <0.00001 |
| Maternal education (years) | |||||
| No education | 207 | 2146 | 96.5 | 11.44 (9.76:13.41) | <0.00001 |
| 1–3 | 402 | 16,133 | 24.9 | 2.96 (2.62:3.34) | <0.00001 |
| 4–7 | 1744 | 124,062 | 14.1 | 1.67 (1.53:1.81) | <0.00001 |
| 8–11 | 3065 | 292,528 | 10.5 | 1.24 (1.15:1.34) | <0.00001 |
| ≥12 | 808 | 95,850 | 8.4 | 1.00 | (Reference) |
| Place of occurrence | |||||
| Hospital | 7638 | 533,987 | 14.3 | 1.00 | (Reference) |
| Other health estab. | 214 | 7524 | 28.4 | 1.99 (1.79:2.28) | <0.00001 |
| Home | 161 | 840 | 191.7 | 13.40 (11.30:15.88) | <0.00001 |
| ICD-10th Chapters/Categories of Causes and Codes | Perinatal Mortality | |
|---|---|---|
| f | % | |
| I. Some infectious and parasitic diseases | 50 | 0.61 |
| Congenital syphilis (A50) | 49 | 0.60 |
| Other bacterial diseases (A21–A22, A24–A28, A31–A32, A38, and A42–A49) | 1 | 0.01 |
| XVI. Some conditions originating in the perinatal period | 6997 | 86.04 |
| Fetus and newborn affected by maternal factors and complications of pregnancy, labor, and delivery (P00–P04) | 4042 | 49.70 |
| Fetal growth retardation, fetal malnutrition, and disorders related to short gestation and low birth weight (P05–P07) | 290 | 3.57 |
| Trauma during birth (P10–P15) | 12 | 0.15 |
| Intrauterine hypoxia and birth asphyxia (P20–P21) | 897 | 11.03 |
| Other respiratory disorders originating in the perinatal period (P22–28) | 527 | 6.48 |
| Congenital infectious and parasitic diseases (P35–P37) | 229 | 2.82 |
| Other conditions originating in the perinatal period (P38–39, P55, P08, P29, P50–P54, and P56–P96) | 1000 | 12.30 |
| XVII. Congenital malformations, deformities, and other congenital anomalies | 1059 | 13.02 |
| Spina bifida (Q05) | 6 | 0.07 |
| Congenital malformations of the circulatory system (Q20–Q28) | 234 | 2.88 |
| Absence, atresia, and small bowel stenosis (Q41) | 4 | 0.05 |
| Other congenital malformations and deformities of the musculoskeletal system (Q67–Q79) | 107 | 1.32 |
| Other malformations, deformities, and other anomalies (Q00–Q04, Q06–Q07, Q10–Q18, Q30–Q34, Q35–Q37, Q50–Q52, Q54–Q64, Q80–Q89, and Q90–Q99) | 708 | 8.71 |
| … Other chapters and categories of causes | 26 | 0.32 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bezerra, I.M.P.; Ramos, J.L.S.; Pianissola, M.C.; Adami, F.; Rocha, J.B.F.d.; Ribeiro, M.A.L.; de Castro, M.R.; Bezerra, J.d.F.; Smiderle, F.R.N.; Sousa, L.V.d.A.; et al. Perinatal Mortality Analysis in Espírito Santo, Brazil, 2008 to 2017. Int. J. Environ. Res. Public Health 2021, 18, 11671. https://doi.org/10.3390/ijerph182111671
Bezerra IMP, Ramos JLS, Pianissola MC, Adami F, Rocha JBFd, Ribeiro MAL, de Castro MR, Bezerra JdF, Smiderle FRN, Sousa LVdA, et al. Perinatal Mortality Analysis in Espírito Santo, Brazil, 2008 to 2017. International Journal of Environmental Research and Public Health. 2021; 18(21):11671. https://doi.org/10.3390/ijerph182111671
Chicago/Turabian StyleBezerra, Italla Maria Pinheiro, José Lucas Souza Ramos, Micael Colodetti Pianissola, Fernando Adami, João Batista Francalino da Rocha, Mariane Albuquerque Lima Ribeiro, Magda Ribeiro de Castro, Juliana da Fonsêca Bezerra, Fabiana Rosa Neves Smiderle, Luiz Vinicius de Alcantara Sousa, and et al. 2021. "Perinatal Mortality Analysis in Espírito Santo, Brazil, 2008 to 2017" International Journal of Environmental Research and Public Health 18, no. 21: 11671. https://doi.org/10.3390/ijerph182111671
APA StyleBezerra, I. M. P., Ramos, J. L. S., Pianissola, M. C., Adami, F., Rocha, J. B. F. d., Ribeiro, M. A. L., de Castro, M. R., Bezerra, J. d. F., Smiderle, F. R. N., Sousa, L. V. d. A., Siqueira, C. E., & de Abreu, L. C. (2021). Perinatal Mortality Analysis in Espírito Santo, Brazil, 2008 to 2017. International Journal of Environmental Research and Public Health, 18(21), 11671. https://doi.org/10.3390/ijerph182111671







