Comparing the Different Manifestations of Postpartum Mental Disorders by Origin, among Immigrants and Native-Born in Israel According to Different Mental Scales
Abstract
1. Introduction
2. Methods
2.1. Tools for Mental States Assessments
2.2. Covariates
2.3. Data Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Husain, N.; Cruickshank, K.; Husain, M.; Khan, S.; Tomenson, B.; Rahman, A. Social stress and depression during pregnancy and in the postnatal period in British Pakistani mothers: A cohort study. J. Affect. Disord. 2012, 140, 268–276. [Google Scholar] [CrossRef]
- Woody, C.A.; Ferrari, A.J.; Siskind, D.J.; Whiteford, H.A.; Harris, M.G. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J. Affect. Disord. 2017, 219, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Payne, J.L.; Maguire, J. Pathophysiological mechanisms implicated in postpartum depression. Front. Neuroendocrinol. 2019, 52, 165–180. [Google Scholar] [CrossRef] [PubMed]
- Ceballos, M.; Wallace, G.; Goodwin, G. Postpartum depression among African-American and Latina Mothers living in small cities, towns, and rural communities. J. Racial Ethn. Health Disparities 2017, 4, 916–927. [Google Scholar] [CrossRef] [PubMed]
- National Collaborating Centre for Mental Health. Antenatal and Postnatal Mental Health. NICE. In Antenatal and Postnatal Mental Health: The NICE Guideline on Clinical Management and Service Guidance; British Psychological Society: Leicester, UK, 2007. [Google Scholar]
- Siu, A.L.; Bibbins-Domingo, K.; Grossman, D.C.; Baumann, L.C.; Davidson, K.W.; Ebell, M. Screening for depression in adults. JAMA 2016, 315, 380. [Google Scholar] [CrossRef]
- Austin, M.P.V.; Hadzi-Pavlovic, D.; Priest, S.R.; Reilly, N.; Wilhelm, K.; Saint, K.; Parker, G. Depressive and anxiety disorders in the postpartum period: How prevalent are they and can we improve their detection? Arch. Womens Ment. Health 2010, 13, 395–401. [Google Scholar] [CrossRef]
- Goodman, J.H.; Chenausky, K.L.; Freeman, M.P. Anxiety disorders during pregnancy. J. Clin. Psychiatry 2014, 75, e1153–e1184. [Google Scholar] [CrossRef]
- Dennis, C.L.; Falah-Hassani, K.; Shiri, R. Prevalence of antenatal and postnatal anxiety: Systematic review and meta-analysis. Br. J. Psychiatry 2017, 210, 315–323. [Google Scholar] [CrossRef]
- Mckee, M.D.; Cunningham, M.; Jankowski, K.R.; Zayas, L. Health-related functional status in pregnancy: Relationship to depression and social support in a multi-ethnic population. Obstetrics Gynecol. 2001, 97, 988–993. [Google Scholar] [CrossRef]
- Miller, R.L.; Pallant, J.F.; Negri, L.M. Anxiety and stress in the postpartum: Is there more to postnatal distress than depression? BMC Psychiatry 2006, 6, 1–11. [Google Scholar] [CrossRef]
- Urindwanayo, D. Immigrant women’s mental health in Canada in the antenatal and postpartum period. Can. J. Nurs. Res. 2018, 50, 155–162. [Google Scholar] [CrossRef]
- Clark, C.L.; Glavin, K.; Missal, B.E.; Sæteren, B. Is there a common experience? Somali new mothers’ childbirth experiences in Norway and the United States. Public Health Nurs. 2018, 35, 184–191. [Google Scholar] [CrossRef] [PubMed]
- Alhasanat, D.; Fry-McComish, J. Postpartum depression among immigrant and arabic women: Literature review. J. Immigr. Minor. Health 2015, 17, 1882–1894. [Google Scholar] [CrossRef]
- Falah-Hassani, K.; Shiri, R.; Vigod, S.; Dennis, C.L. Prevalence of postpartum depression among immigrant women: A systematic review and meta-analysis. J. Psychiatr. Res. 2015, 70, 67–82. [Google Scholar] [CrossRef] [PubMed]
- Straiton, M.L.; Aambø, A.K.; Johansen, R. Perceived discrimination, health and mental health among immigrants in Norway: The role of moderating factors. BMC Public Health 2019, 19, 325. [Google Scholar] [CrossRef]
- Bas-Sarmiento, P.; Saucedo-Moreno, M.J.; Fernández-Gutiérrez, M.; Poza-Méndez, M. Mental health in immigrants versus native population: A systematic review of the literature. Arch. Psychiatr. Nursing 2017, 31, 111–121. [Google Scholar] [CrossRef]
- Cohen, J.B. Ethiopian-Israeli community. BMJ Case Rep. 2016, bcr2016216074. [Google Scholar] [CrossRef]
- Fisher, J.; Mello, M.C.D.; Patel, V.; Rahman, A.; Tran, T.; Holton, S.; Holmes, W. Systematic reviews Prevalence and determinants of common perinatal mental disorders in women in low-and lower-middle-income countries: A systematic review. Bull World Health Organ. 2012, 90, 139–149. [Google Scholar] [CrossRef]
- Sawyer, A.; Ayers, S.; Smith, H. Pre- and postnatal psychological wellbeing in Africa: A systematic review. J. Affect. Disord. 2010, 123, 17–29. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, J.N.; Parcesepe, A.; Mekuria, Y.G.; Abitew, D.B.; Gebeyehu, W.; Okello, F.; Shattuck, D. Maternal mental health in Amhara region, Ethiopia: A cross-sectional survey. Glob. Health Sci. Pract. 2014, 2, 482–486. [Google Scholar] [CrossRef] [PubMed]
- Kakyo, T.A.; Muliira, J.K.; Mbalinda, S.N.; Kizza, I.B.; Muliira, R.S. Factors associated with depressive symptoms among postpartum mothers in a rural district in Uganda. Midwifery 2012, 28, 374–379. [Google Scholar] [CrossRef]
- Bashiri, N. Spielvogel, A.M. Postpartum depression: A cross-cultural perspective. Prim. Care Update OB/GYNS 1999, 6, 82–87. [Google Scholar] [CrossRef]
- Ahmed, S.; Shommu, N.S.; Rumana, N.; Barron, G.R.; Wicklum, S.; Turin, T.C. Barriers to access of primary healthcare by immigrant populations in Canada: A literature review. J. Immigr. Minority Health 2016, 18, 1522–1540. [Google Scholar] [CrossRef] [PubMed]
- Simon, G.E.; VonKorff, M.; Piccinelli, M.; Fullerton, C.; Ormel, J. An international study of the relation between somatic symptoms and depression. New Engl. J. Med. 1999, 341, 1329–1335. [Google Scholar] [CrossRef]
- Youngmann, R.; Zilber, N.; Workneh, F.; Giel, R. Adapting the SRQ for Ethiopian populations: A culturally-sensitive psychiatric screening instrument. Transcult. Psychiatry 2008, 45, 566–589. [Google Scholar] [CrossRef]
- Young, A. Internalizing and externalizing medical belief systems: An Ethiopian example. Soc. Sci. Med. 1976, 10, 147–156. [Google Scholar] [CrossRef]
- Illanes, E.; Bustos, L.; Lagos, X.; Navarro, N.; Munoz, S. Associated factors to depressive symptoms and somatic symptoms in climacteric women in the city of Temuco. Rev. Med. Chil. 2002, 130, 885–891. [Google Scholar]
- McMillan, A.S.; Wong, M.C.M.; Zheng, J.; Luo, Y.; Lam, C.L.K. Widespread pain symptoms and psychological distress in southern Chinese with orofacial pain. J. Oral Rehabil. 2010, 37, 2–10. [Google Scholar]
- Ritsner, M.; Ponizovsky, A.; Kurs, R.; Modai, I. Somatization in an immigrant population in israel: A community survey of prevalence, risk factors, and help-seeking behavior. Am. J. Psychiatry 2000, 157, 385–392. [Google Scholar]
- Lanzara, R.; Scipioni, M.; Conti, C. A clinical-psychological perspective on somatization among immigrants: A systematic review. Front. Psychol. 2019, 9, 2792. [Google Scholar] [CrossRef] [PubMed]
- Plummer, F.; Manea, L.; Trepel, D.; McMillan, D. Screening for anxiety disorders with the GAD-7 and GAD-2: A systematic review and diagnostic metaanalysis. Gen. Hosp. Psychiatry 2016, 39, 26–31. [Google Scholar] [CrossRef]
- Zubaran, C.; Schumacher, M.; Roxo, M.R.; Foresti, K. Screening tools for postpartum depression: Validity and cultural dimensions. Afr. J. Psychiatry (S. Africa) 2010, 13, 357–365. [Google Scholar] [CrossRef]
- Shrestha, S.D.; Pradhan, R.; Tran, T.D.; Gualano, R.C.; Fisher, J.R. Reliability and validity of the Edinburgh Postnatal Depression Scale (EPDS) for detecting perinatal common mental disorders (PCMDs) among women in low-and lower-middle-income countries: A systematic review. BMC Pregnancy Childbirth 2016, 16, 1–19. [Google Scholar] [CrossRef]
- Parkerson, H.A.; Thibodeau, M.A.; Brandt, C.P.; Zvolensky, M.J.; Asmundson, G.J.G. Cultural-based biases of the GAD-7. J. Anxiety Disord. 2015, 31, 38–42. [Google Scholar] [CrossRef]
- Hanlon, C.; Medhin, G.; Alem, A.; Araya, M.; Abdulahi, A.; Hughes, M.; Prince, M. Detecting perinatal common mental disorders in Ethiopia: Validation of the self-reporting questionnaire and Edinburgh Postnatal Depression Scale. J. Affect. Disord. 2008, 108, 251–262. [Google Scholar] [CrossRef] [PubMed]
- Lau, Y.; Wang, Y.; Yin, L.; Chan, K.S.; Guo, X. Validation of the mainland Chinese version of the Edinburgh Postnatal Depression Scale in chengdu mothers. Int. J. Nurs. Stud. 2010, 47, 1139–1151. [Google Scholar] [CrossRef]
- Rubertsson, C.; Börjesson, K.; Berglund, A.; Josefsson, A.; Sydsjö, G. The Swedish validation of Edinburgh Postnatal Depression Scale (EPDS) during pregnancy. Nord. J. Psychiatry 2011, 65, 414–418. [Google Scholar] [CrossRef]
- Small, R.; Lumley, J.; Yelland, J.; Brown, S. The performance of the Edinburgh Postnatal Depression Scale in English speaking and non-English speaking populations in Australia. Soc. Psychiatry Psychiatr. Epidemiol. 2007, 42, 70–78. [Google Scholar] [CrossRef]
- Chaudron, L.H.; Szilagyi, P.G.; Tang, W.; Anson, E.; Talbot, N.L.; Wadkins, H.I.; Wisner, K.L. Accuracy of depression screening tools for identifying postpartum depression among urban mothers. Pediatrics 2010, 125, e609–e617. [Google Scholar] [CrossRef]
- Matijasevich, A.; Munhoz, T.N.; Tavares, B.F.; Barbosa, A.P.P.N.; da Silva, D.M.; Abitante, M.S.; Santos, I.S. Validation of the Edinburgh Postnatal Depression Scale (EPDS) for screening of major depressive episode among adults from the general population. BMC Psychiatry 2014, 14, 284. [Google Scholar] [CrossRef]
- Benvenuti, P. The Edinburgh Postnatal Depression Scale: Validation for an Italian sample. J. Affect. Disord. 1999, 53, 137–141. [Google Scholar] [CrossRef]
- Smith-Nielsen, J.; Matthey, S.; Lange, T.; Væver, M.S. Validation of the Edinburgh Postnatal Depression Scale against both DSM-5 and ICD-10 diagnostic criteria for depression. BMC Psychiatry 2018, 18, 393. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Delgadillo, J.; Payne, S.; Gilbody, S.; Godfrey, C.; Gore, S.; Jessop, D.; Dale, V. Brief case finding tools for anxiety disorders: Validation of GAD-7 and GAD-2 in addictions treatment. Drug Alcohol. Depend. 2012, 125, 37–42. [Google Scholar] [CrossRef]
- Christensen, H.; Batterham, P.J.; Grant, J.; Griffiths, K.M.; MacKinnon, A.J. A population study comparing screening performance of prototypes for depression and anxiety with standard scales. BMC Med. Res. Methodol. 2011, 11, 154. [Google Scholar] [CrossRef]
- Beard, C.; Björgvinsson, T. Beyond generalized anxiety disorder: Psychometric properties of the GAD-7 in a heterogeneous psychiatric sample. J. Anxiety Disord. 2014, 28, 547–552. [Google Scholar] [CrossRef]
- Hinz, A.; Klein, A.M.; Brähler, E.; Glaesmer, H.; Luck, T.; Riedel-Heller, S.G.; Hilbert, A. Psychometric evaluation of the generalized anxiety disorder screener GAD-7, based on a large German general population sample. J. Affect. Disord. 2017, 210, 338–344. [Google Scholar] [CrossRef]
- Hergenrather, J.Y.; Aviram, J.; Vysotski, Y.; Campisi-Pinto, S.; Lewitus, G.M.; Meiri, D. Cannabinoid and terpenoid doses are associated with adult ADHD status of medical cannabis patients. Rambam Maimonides Med. J. 2020, 11, e0001. [Google Scholar] [CrossRef]
- Evagorou, O.; Arvaniti, A.; Samakouri, M. Cross-cultural approach of postpartum depression: Manifestation, practices applied, risk factors and therapeutic interventions. Psychiatr. Q. 2016, 87, 129–154. [Google Scholar] [CrossRef]
- Miszkurka, M.; Goulet, L.; Zunzunegui, M.V. Antenatal depressive symptoms among Canadian-born and immigrant women in Quebec: Differential exposure and vulnerability to contextual risk factors. Soc. Psychiatry Psychiatr. Epidemiol. 2012, 47, 1639–1648. [Google Scholar] [CrossRef]
- Harding, T.W.; Busnello, E.A.; Climent, C.E.; Diop, M.; El-Hakim, A.; Giel, R.; Ibrahim, H.H.; Ladrido-Ignacio, L.; Wig, N.N. The WHO collaborative study on strategies for extending mental health care, III: Evaluation design and illustrative results. Am. J. Psychiatry 1983, 140, 1481–1485. [Google Scholar]
- Jurcik, T.; Chentsova-Dutton, Y.E.; Solopieieva-Jurcikova, I.; Ryder, A.G. Russians in treatment: The evidence base supporting cultural adaptations. J. Clin. Psychol. 2013, 69, 774–791. [Google Scholar] [CrossRef]
- Abu-Kaf, S.; Shahar, G. Depression and somatic symptoms among two ethnic groups in Israel: Testing three theoretical models. Isr. J. Psychiatry Relat. Sci. 2017, 54, 32–39. [Google Scholar]
- The Infant Development and Environment Study (TIDES)|Icahn School of Medicine. Available online: https://icahn.mssm.edu/about/departments/environmental-public-health/research/tides (accessed on 30 October 2021).
- Palyada, K.; Sun, Y.Q.; Flint, A.; Butcher, J.; Naikare, H.; Stintzi, A. Characterization of the oxidative stress stimulon and PerR regulon of Campylobacter jejuni. BMC Genom. 2009, 10, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.T.; Chen, W.T.; Li, G.W.; Shen, J.X.; Ye, Q.Q.; Zhang, M.L.; Liu, J. Analysis of the differentially expressed genes induced by cisplatin resistance in oral squamous cell carcinomas and their interaction. Front. Genet. 2020, 10, 1328. [Google Scholar] [CrossRef] [PubMed]
- Rask, S.; Suvisaari, J.; Koskinen, S.; Koponen, P.; Mölsä, M.; Lehtisalo, R.; Castaneda, A.E. The ethnic gap in mental health: A population-based study of Russian, Somali and Kurdish origin migrants in Finland. Scand. J. Public Health 2016, 44, 281–290. [Google Scholar] [CrossRef]
- Lubotzky-Gete, S.; Ornoy, A.; Grotto, I.; Calderon-Margalit, R. Postpartum depression and infant development up to 24 months: A nationwide population-based study. J. Affect. Disord. 2021, 285, 136–143. [Google Scholar] [CrossRef]
- Blank, R. Maternal depression in Israel. Available online: www.knesset.gov.il/mmm (accessed on 31 October 2021).
- Chaudron, L.H.; Szilagyi, P.G.; Kitzman, H.J.; Wadkins, H.I.M.; Conwell, Y. Detection of postpartum depressive symptoms by screening at well-child visits. Pediatrics 2004, 113, 551–558. [Google Scholar] [CrossRef]
- Kleinman, A.; Good, B. Culture and Depression: Studies in the Anthropology and Cross-Cultural Psychiatry of Affect and Disorder; University of California Press: Berkeley, CA, USA, 1985. [Google Scholar]
- Deveci, A.; Taskin, O.; Dinc, G.; Yilmaz, H.; Demet, M.M.; Erbay-Dundar, P.; Ozmen, E. Prevalence of pseudoneurologic conversion disorder in an urban community in Manisa, Turkey. Soc. Psychiatry Psychiatr. Epidemiol. 2007, 42, 857–864. [Google Scholar] [CrossRef]
- Mumford, D.B.; Minhas, F.A.; Akhtar, I.; Akhter, S.; Mubbashar, M.H. Stress and psychiatric disorder in urban Rawalpindi: Community survey. Br. J. Psychiatry 2000, 177, 557–562. [Google Scholar] [CrossRef] [PubMed]
- Toft, T.; Fink, P.E.R.; Oernboel, E.V.A.; Christensen, K.A.J.; Frostholm, L.; Olesen, F. Mental disorders in primary care: Prevalence and co-morbidity among disorders. Results from the functional illness in primary care (FIP) study. Psychol. Med. 2005, 35, 1175–1184. [Google Scholar] [CrossRef]
- de Waal, M.W.; Arnold, I.A.; Spinhoven, P.; Eekhof, J.A.; Assendelft, W.J.; van Hemert, A.M. The role of comorbidity in the detection of psychiatric disorders with checklists for mental and physical symptoms in primary care. Soc. Psychiatry Psychiatr. Epidemiol. 2009, 44, 78–85. [Google Scholar] [CrossRef]
- Roca, M.; Gili, M.; Garcia-Garcia, M.; Salva, J.; Vives, M.; Campayo, J.G.; Comas, A. Prevalence and comorbidity of common mental disorders in primary care. J. Affect. Disord. 2009, 119, 52–58. [Google Scholar] [CrossRef]
- Löwe, B.; Spitzer, R.L.; Williams, J.B.; Mussell, M.; Schellberg, D.; Kroenke, K. Depression, anxiety and somatization in primary care: Syndrome overlap and functional impairment. Gen. Hosp. Psychiatry 2008, 30, 191–199. [Google Scholar] [CrossRef]
- Tamayo, J.M.; Román, K.; Fumero, J.J.; Rivas, M. The level of recognition of physical symptoms in patients with a major depression episode in the outpatient psychiatric practice in Puerto Rico: An observation study. BMC Psychiatry 2005, 5., 1–13. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Juang, K.; Wang, S.; Fuh, J.; Lu, S.; Su, T. Comorbidity of depressive and anxiety disorders in chronic daily headache and its subtypes. Headache J. Head Face Pain 2000, 40, 818–823. [Google Scholar] [CrossRef]
- Kapfhammer, H.P. Somatic symptoms in depression. Dialogues Clin. Neurosci. 2006, 8, 227–239. [Google Scholar]
- Diagnostic and Statistical Manual of Mental Disorders—DSM-5; American Psychiatric Association: Washington, DC, USA, 2013.
- Judah, M.R.; Shurkova, E.Y.; Hager, N.M.; White, E.J.; Judah, M.R.; Taylor, D.L.; Grant, D.M. The relationship between social anxiety and heartbeat evoked potential amplitude. Biol. Psychol. 2018, 139, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Moritz, S.; Schmidt, S.J.; Lüdtke, T.; Braunschneider, L.E.; Manske, A.; Schneider, B.C.; Veckstenstedt, R. Post-psychotic depression: Paranoia and the damage done. Schizophr. Res. 2019, 211, 79–85. [Google Scholar] [CrossRef]
- Cooper, P.J.; Campbell, E.A.; Day, A.; Kennerley, A.D.; Bond, A. Non-psychotic psychiatric disorder after childbirth. A prospective study of prevalence, incidence, course and nature. Br. J. Psychiatry 1988, 152, 799–806. [Google Scholar] [CrossRef] [PubMed]
- Torres, A.; Gelabert, E.; Roca, A.; Navarro, P.; Plaza, A.; Subirà, S.; Garcia-Esteve, L. Course of a major postpartum depressive episode: A prospective 2 years naturalistic follow-up study. J. Affect. Disord. 2019, 245, 965–970. [Google Scholar] [CrossRef]
- Rubertsson, C.; Wickberg, B.; Gustavsson, P.; Rådestad, I. Depressive symptoms in early pregnancy, two months and one year postpartum-prevalence and psychosocial risk factors in a national Swedish sample. Arch. Womens. Ment. Health 2005, 8, 97–104. [Google Scholar] [CrossRef]
- Nguyen, T.T.; Tran, T.D.; Tran, T.; La, B.; Nguyen, H.; Fisher, J. Postpartum change in common mental disorders among rural Vietnamese women: Incidence, recovery and risk and protective factors. Br. J. Psychiatry 2015, 206, 110–115.–115. [Google Scholar] [CrossRef]
- Segre, L.S.; O’Hara, M.W.; Arndt, S.; Stuart, S. The prevalence of postpartum depression. Soc. Psychiatry Psychiatr. Epidemiol. 2007, 42, 316–321. [Google Scholar] [CrossRef] [PubMed]
- Mayberry, L.J.; Horowitz, J.A.; Declercq, E. Depression symptom prevalence and demographic risk factors among U.S. women during the first 2 years postpartum. J. Obstet. Gynecol. Neonatal Nurs. 2007, 36, 542–549. [Google Scholar] [CrossRef]
- Goyal, D.; Gay, C.; Lee, K.A.; Jose, S. How much does low socioeconomic status increase the risk of prenatal and postpartum depressive symptoms in first time mothers? Womens Health Issues 2010, 20, 96–104. [Google Scholar] [CrossRef]
- Beck, C.T. Predictors of postpartum depression: An update. Nurs. Res. 2001, 50, 275–285. [Google Scholar] [CrossRef] [PubMed]
- Robertson, E.; Grace, S.; Wallington, T.; Stewart, D.E. Antenatal risk factors for postpartum depression: A synthesis of recent literature. Gen. Hosp. Psychiatry 2004, 26, 289–295. [Google Scholar] [CrossRef]
- Torres, R.; Goyal, D.; Burke-Aaronson, A.C.; Gay, C.L.; Lee, K.A. Patterns of symptoms of perinatal depression and stress in late adolescent and young adult mothers. J. Obstet. Gynecol. Neonatal Nurs. 2017, 46, 814–823. [Google Scholar] [CrossRef]
- Adewuya, A.O.; Fatoye, F.O.; Ola, B.A.; Ijaodola, O.R.; Ibigbami, S.M.O. Sociodemographic and obstetric risk factors for postpartum depressive symptoms in Nigerian women. J. Psychiatr. Pract. 2005, 11, 353–358. [Google Scholar] [CrossRef] [PubMed]
- Babu, G.R.; Murthy, G.V.S.; Singh, N.; Nath, A.; Rathnaiah, M.; Saldanha, N.; Kinra, S. Sociodemographic and medical risk factors associated with antepartum depression. Front. Public Health 2018, 6, 127. [Google Scholar] [CrossRef]
- Zelkowitz, P.; Saucier, J.F.; Wang, T.; Katofsky, L.; Valenzuela, M.; Westreich, R. Original contribution stability and change in depressive symptoms from pregnancy to two months postpartum in childbearing immigrant women. Arch Womens Ment Health 2008, 11, 1–11. [Google Scholar] [CrossRef]
- Williams, D.R.; Neighbors, H.W.; Jackson, J.S. Racial/ethnic discrimination and health: Findings from community studies. Am. J. Public Health. 2003, 93, 200–208. [Google Scholar] [CrossRef]
- Schulz, A.J.; Gravlee, C.C.; Williams, D.R.; Israel, B.A.; Mentz, G.; Rowe, Z. Discrimination, symptoms of depression, and self-rated health among african american women in detroit: Results from a longitudinal analysis. Am. J. Public Health 2006, 96, 1265–1270. [Google Scholar] [CrossRef] [PubMed]
- Canady, R.B.; Bullen, B.L.; Holzman, C.; Broman, C.; Tian, Y. Discrimination and symptoms of depression in pregnancy among African American and white women. Women’s Health Issues 2008, 18, 292–300. [Google Scholar] [CrossRef] [PubMed]
- King, L.; Feeley, N.; Gold, I.; Hayton, B.; Zelkowitz, P. The healthy migrant effect and predictors of perinatal depression. Women Birth 2019, 32, e341–e350. [Google Scholar] [CrossRef] [PubMed]
- Asnaani, A.; Richey, J.A.; Dimaite, R.; Hinton, D.E.; Hofmann, S.G. A cross-ethnic comparison of lifetime prevalence rates of anxiety disorders. J. Nerv. Ment. Dis. 2010, 198, 551–555. [Google Scholar] [CrossRef]

| INB * N = 480 % (n) | ETH N = 210 % (n) | FSU N = 262 % (n) | p X2/F | |
|---|---|---|---|---|
| Total | ||||
| Maternal age, years (mean ± SD) | 30.9 ± 4.9 | 30.9 ± 5.2 | 31.2 ± 4.9 | 0.693 |
| Religiosity | ||||
| Secular | 38.8 (186) | 16.4 (33) | 63.3 (162) | <0.001 |
| Traditional | 41.0 (197) | 59.7 (120) | 28.9 (74) | |
| Orthodox | 14.2 (68) | 20.9 (42) | 4.7 (12) | |
| Ultra-Orthodox | 6.0 (29) | 3.0 (6) | 3.1 (8) | |
| Maternal Status | ||||
| Married | 96.5 (463) | 87.6 (184) | 95.8 (251) | <0.001 |
| Unmarried | 3.5 (17) | 12.4 (26) | 4.2 (11) | |
| Maternal Education group | ||||
| 1–12 | 34.5 (164) | 67.0 (130) | 37.2 (96) | <0.001 |
| >12 | 65.5 (311) | 33.0 (64) | 62.8 (162) | |
| Income | ||||
| Above average | 46.5 (221) | 19.5 (36) | 43.0 (108) | <0.001 |
| Same as average | 34.9 (166) | 33.2 (61) | 37.1 (93) | |
| Lower than average | 18.5 (88) | 47.3 (87) | 19.9 (50) | |
| Insurance | ||||
| Yes | 94.0 (426) | 73.7 (129) | 86.8 (197) | <0.001 |
| No | 6.0 (27) | 26.3 (46) | 13.2 (30) | |
| Pregnancy | ||||
| Planned | 73.2 (347) | 74.3 (150) | 78.7 (203) | 0.255 |
| Unplanned | 26.8 (127) | 25.7 (52) | 21.3 (55) | |
| Pregnancy | ||||
| Spontaneous | 88.1 (420) | 94.4 (185) | 88.0 (227) | 0.037 |
| Fertility treatment | 11.9 (57) | 5.6 (11) | 12.0 (31) | |
| Perinatal care during pregnancy | ||||
| Full | 90.1 (429) | 87.3 (178) | 95.0 (249) | 0.011 |
| No/partial | 9.9 (47) | 12.7 (26) | 5.0 (13) | |
| Birth type | ||||
| Spontaneous | 70.6 (333) | 64.6 (135) | 70.0 (180) | 0.202 |
| Instrumental | 5.9 (28) | 6.7 (14) | 3.1 (8) | |
| Cesarean | 23.5 (111) | 28.7 (60) | 26.9 (69) | |
| Parity (mean ± SD) | 2.20 ± 1.2 | 2.24 ± 1.4 | 2.18 ± 1.1 | 0.874 |
| 1 | 34.3 (155) | 35.3 (67) | 31.3 (78) | 0.559 |
| 2–4 | 61.1 (276) | 57.4 (109) | 63.1 (157) | |
| >4 | 4.6 (21) | 7.4 (14) | 5.6 (14) | |
| Gestational age (mean ± SD) | 39.0 ± 1.8 | 39.2 ± 1.8 | 38.9 ± 1.6 | 0.061 |
| Gestational age group | ||||
| <36 | 5.9 (22) | 6.3 (10) | 5.5 (12) | 0.007 |
| 37–40 | 80.9 (300) | 67.8 (107) | 79.5 (175) | |
| >40 | 13.2 (49) | 25.9 (41) | 15.0 (33) | |
| Birth weight (mean ± SD) | 3168 ± 509 | 3122 ± 509 | 3272 ± 543 | 0.004 |
| Birth weight group (gr.) | ||||
| <2500 | 8.3 (40) | 11.0 (23) | 8.8 (23) | 0.525 |
| >2500 | 91.7 (440) | 88.0 (186) | 91.2 (238) | |
| Apgar 1 (mean ± SD) | 8.90 ± 0.6 | 8.87 ± 0.5 | 8.96 ± 0.2 | 0.148 |
| Apgar 5 (mean ± SD) | 10.05 ± 2.8 | 9.93 ± 0.2 | 9.94 ± 0.3 | 0.679 |
| Gender | ||||
| Male | 52.0 (246) | 50.7 (107) | 46.9 (123) | 0.418 |
| Female | 48.0 (227) | 49.3 (104) | 53.1 (139) | |
| Multigestation | ||||
| Yes | 4.2 (20) | 2.8 (6) | 2.3 (6) | 0.345 |
| No | 95.8 (458) | 97.2 (206) | 97.7 (257) | |
| Smoking during pregnancy | ||||
| Yes | 9.3 (42) | 14.0 (27) | 9.2 (23) | 0.155 |
| No | 90.7 (412) | 86.0 (166) | 90.8 (227) | |
| Alcohol during pregnancy | ||||
| Yes | 7.9 (36) | 5.9 (11) | 17.7 (44) | <0.001 |
| No | 92.1 (418) | 94.1 (175) | 82.3 (205) | |
| Breastfeeding at 6–8 weeks | ||||
| Exclusive | 39.1 (109) | 57.4 (66) | 46.1 (70) | 0.001 |
| Partial | 13.6 (38) | 18.3 (21) | 15.7 (24) | |
| None | 47.3 (132) | 24.3 (28) | 38.2 (58) | |
| Spouse support (among married) | ||||
| High | 96.4 (426) | 90.5 (153) | 95.5 (231) | 0.015 |
| Low | 3.6 (14) | 9.5 (16) | 4.5 (11) | |
| Stressful events | ||||
| Yes | 32.4 (155) | 35.4 (68) | 39.4 (98) | 0.177 |
| No | 67.6 (303) | 64.6 (124) | 60.6 (151) | |
| Racism (mean ± SD) | 11.04 ± 2.4 | 14.05 ± 7.5 | 11.81 ± 4.1 | <0.001 |
| # | INB % | ETH % | FSU % |
|---|---|---|---|
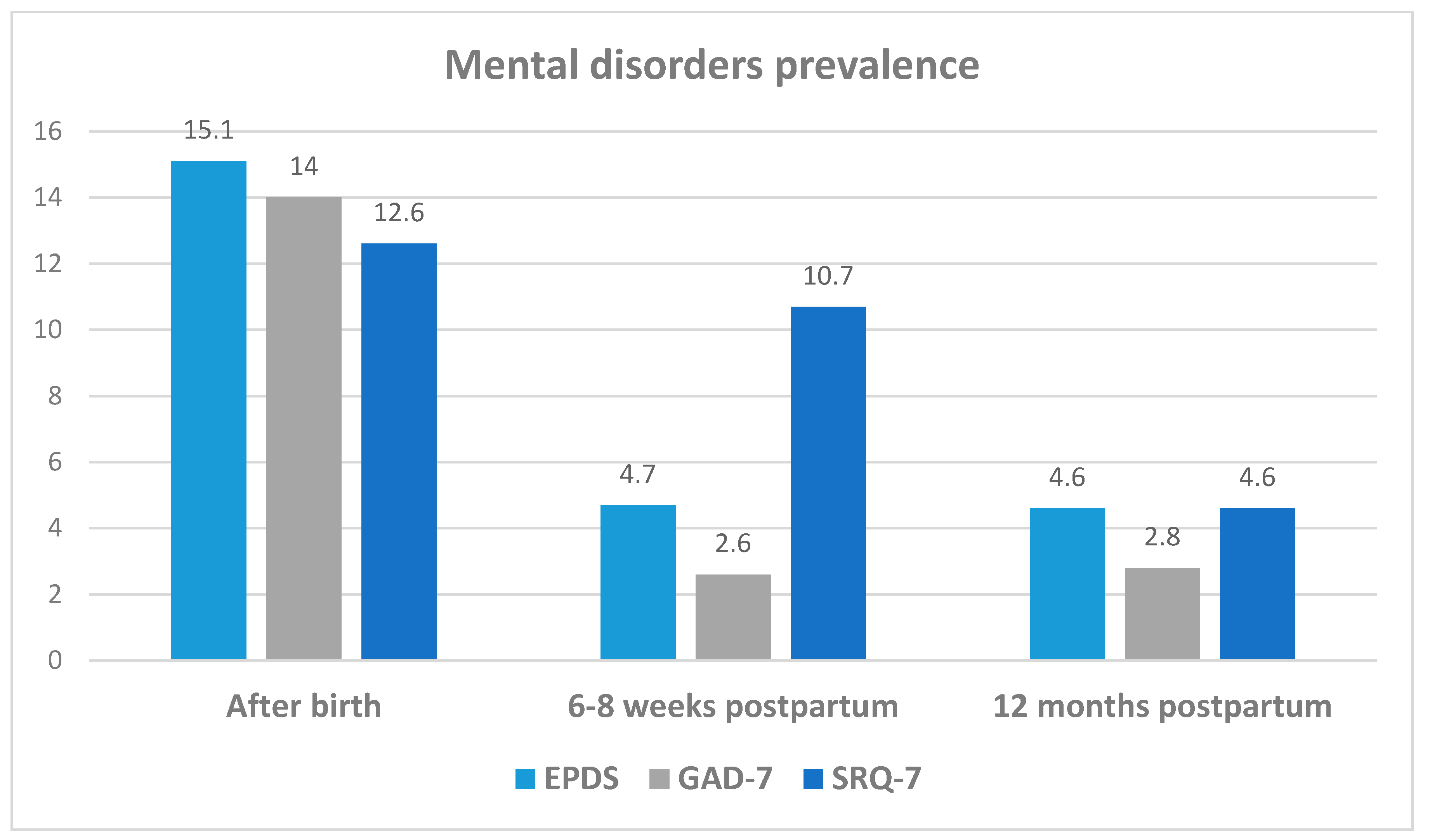
| After birth | |||
| EPDS ≥ 10 | 17.5 | 14.0 | 11.8 ** |
| GAD-7 ≥ 8 | 15.9 | 11.5 ** | 12.6 ** |
| SRQ-7 any symptom | 9.6 | 17.7 ** | 14.0 * |
| 6–8 weeks postpartum | |||
| EPDS ≥ 10 | 3.9 | 5.1 | 5.9 |
| GAD-7 ≥ 8 | 2.5 | 2.6 * | 2.6 |
| SRQ-7 any symptom | 8.0 | 13.9 | 13.2 |
| 12 months postpartum | |||
| EPDS ≥ 10 | 3.2 | 7.9 | 4.7 |
| GAD-7 ≥ 8 | 3.2 | 2.3 ** | 2.3 * |
| SRQ-7 any symptom | 3.2 | 7.9 | 4.7 |
| EPDS β | GAD-7 β | SRQ-7 (SUM) β | |
|---|---|---|---|
| After birth | |||
| INB | Ref. | Ref. | Ref. |
| ETH | −607 | −1.281 ** | 0.221 ** |
| FSU | −0.709 ** | −0.494 ** | 0.121 * |
| Age 18–24 (ref. > 35) | 1.039 * | 0.780 | 0.244 ** |
| Age 25–34 (ref. > 35) | −0.922 ** | −0.461 | −0.148 ** |
| Married (ref. single) | 1.510 ** | −0.996 | −0.164 |
| Education < 12 (ref. > 13) | 1.076 | 0.302 | 0.437 ** |
| Education = 12 (ref. > 13) | −0.261 | −0.462 | 0.028 |
| Trauma events | 0.897 *** | 0.730 *** | 0.190 *** |
| 6–8 weeks postpartum | |||
| INB # | Ref. | Ref. | Ref. |
| ETH # | 0.131 | −0.678 ** | 0.038 |
| FSU # | 0.129 | −0.099 | 0.106 |
| Age 18–24 (ref. > 35) | 0.509 | −0.223 | 0.255 |
| Age 25–34 (ref. > 35) | 0.192 | 0.256 | 0.149 |
| Married (ref. single) | −0.044 | 0.796 | 0.060 |
| Education < 12 (ref. > 13) | 0.306 | 0.336 | 0.450 ** |
| Education = 12 (ref. > 13) | −0.258 | 0.027 | 0.030 |
| Trauma events | 0.805 *** | 0.357 ** | 0.192 *** |
| 12 mo. Postpartum | |||
| INB # | Ref. | Ref. | Ref. |
| ETH ## | −0.112 | −1.072 ** | 0.064 |
| FSU # | 0.029 | −0.630 * | 0.101 |
| Age 18–24 (ref. > 35) | −0.397 | −0.284 | 0.263 |
| Age 25–34 (ref. > 35) | −0.532 | −0.330 | 0.069 |
| Married (ref. single) | −0.044 | 0.495 | 0.044 |
| Education < 12 (ref. > 13) | 0.124 | 0.592 | 0.522 ** |
| Education = 12 (ref. > 13) | 0.872 ** | 0.330 | 0.274 ** |
| Traumatic life events | 0.674 *** | 0.645 *** | 0.186 *** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lubotzky-Gete, S.; Gete, M.; Levy, R.; Kurzweil, Y.; Calderon-Margalit, R. Comparing the Different Manifestations of Postpartum Mental Disorders by Origin, among Immigrants and Native-Born in Israel According to Different Mental Scales. Int. J. Environ. Res. Public Health 2021, 18, 11513. https://doi.org/10.3390/ijerph182111513
Lubotzky-Gete S, Gete M, Levy R, Kurzweil Y, Calderon-Margalit R. Comparing the Different Manifestations of Postpartum Mental Disorders by Origin, among Immigrants and Native-Born in Israel According to Different Mental Scales. International Journal of Environmental Research and Public Health. 2021; 18(21):11513. https://doi.org/10.3390/ijerph182111513
Chicago/Turabian StyleLubotzky-Gete, Shakked, Maru Gete, Roni Levy, Yaffa Kurzweil, and Ronit Calderon-Margalit. 2021. "Comparing the Different Manifestations of Postpartum Mental Disorders by Origin, among Immigrants and Native-Born in Israel According to Different Mental Scales" International Journal of Environmental Research and Public Health 18, no. 21: 11513. https://doi.org/10.3390/ijerph182111513
APA StyleLubotzky-Gete, S., Gete, M., Levy, R., Kurzweil, Y., & Calderon-Margalit, R. (2021). Comparing the Different Manifestations of Postpartum Mental Disorders by Origin, among Immigrants and Native-Born in Israel According to Different Mental Scales. International Journal of Environmental Research and Public Health, 18(21), 11513. https://doi.org/10.3390/ijerph182111513






