HIV Education, Empathy, and Empowerment (HIVE3): A Peer Support Intervention for Reducing Intersectional Stigma as a Barrier to HIV Testing among Men Who Have Sex with Men in Ghana
Abstract
:1. Introduction
2. The Dennis Peer Support Model
3. The Approach Employed in Adapting HIVE3
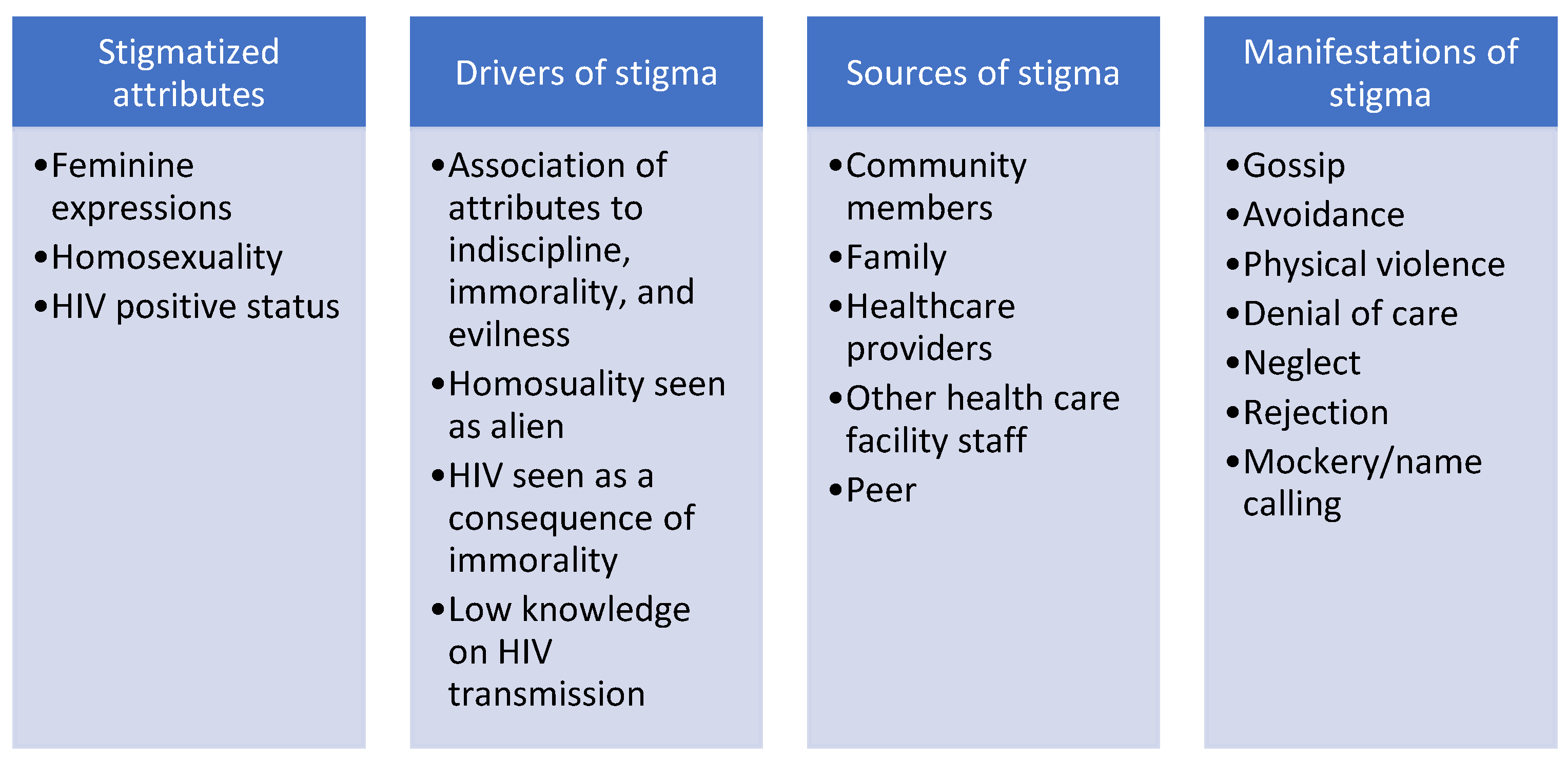
3.1. ADAPT-IT Step One—Assessment
3.2. ADAPT-IT Steps Two—Decision, Three—Adaptation, and Four—Production
3.3. ADAPT-IT Steps Five—Topical Experts and Six—Integration
3.4. ADAPT-IT Steps Seven—Training and Eight—Pilot Testing
“I am afraid that I might get into trouble. Looking at the current situation in the country on LGBTQI+ communities, I don’t feel comfortable even though you have given me all the assurance on security. Thank you for the opportunity, but I can’t continue with the study”— A participant explaining his reasons for dropping out of the study.
4. Discussion of Lessons Learned
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abubakari, G.M.; Turner, D.; Ni, Z.; Conserve, D.F.; Dada, D.; Otchere, A.; Amanfoh, Y.; Boakye, F.; Torpey, K.; Nelson, L.E. Community-Based Interventions as Opportunities to Increase HIV Self-Testing and Linkage to Care Among Men Who Have Sex with Men—Lessons From Ghana, West Africa. Front. Public Health 2021, 9, 581. [Google Scholar] [CrossRef]
- Kushwaha, S.; Lalani, Y.; Maina, G.; Ogunbajo, A.; Wilton, L.; Agyarko-Poku, T.; Nelson, L.E. “But the moment they find out that you are MSM…”: A qualitative investigation of HIV prevention experiences among men who have sex with men (MSM) in Ghana’s health care system. BMC Public Health 2017, 17, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Atuguba, R.A. Homosexuality in Ghana: Morality, Law, Human Rights. J. Politi- Law 2019, 12, p113. [Google Scholar] [CrossRef]
- Gyamerah, A.A.O. Unburying the Ostrich’s Head and Opening Pandora’s Box: A Paradigm Shift to Address HIV Among Men Who Have Sex With Men in Ghana’s National AIDS Response; Columbia University: New York, NU, USA, 2017. [Google Scholar]
- Banks, W.D. Queering Ghana: Sexuality, Community, and the Struggle for Cultural Belonging in an African Nation. Ph.D. Thesis, Wayne State University, Detroit, MI, USA, 2013. [Google Scholar]
- Ghana AIDS Commission. National HIV and AIDS Monitoring and Evaluation Plan 2016–2020. 2017. Available online: http://www.ghanaids.gov.gh/gac1/pubs/M&E%20Plan%202016-2020.pdf (accessed on 10 May 2021).
- Gyamerah, A.O.; Taylor, K.D.; Atuahene, K.; Anarfi, J.K.; Fletcher, M.; Raymond, H.F.; McFarland, W.; Dodoo, F.N.-A. Stigma, discrimination, violence, and HIV testing among men who have sex with men in four major cities in Ghana. AIDS Care 2020, 32, 1036–1044. [Google Scholar] [CrossRef] [PubMed]
- Ali, H.; Amoyaw, F.; Baden, D.; Durand, L.; Bronson, M.; Kim, A.; Grant-Greene, Y.; Imtiaz, R.; Swaminathan, M. Ghana’s HIV epidemic and PEPFAR’s contribution towards epidemic control. Ghana Med. J. 2019, 53, 59–62. [Google Scholar] [CrossRef] [Green Version]
- Abubakari, G.M.R.; Turner, D.; Nelson, L.E.; Odhiambo, A.J.; Boakye, F.; Manu, A.; Wilton, L. An Application of the ADAPT-ITT Model to an Evidence-Based Behavioral HIV Prevention Intervention (Nyansapo) for Men Who Have Sex with Men (MSM) in Ghana. Int. Health Trends Perspect. 2021, 1, 1–16. [Google Scholar] [CrossRef]
- Ogunbajo, A.; Leblanc, N.; Kushwaha, S.; Boakye, F.; Hanson, S.; Smith, M.D.; Nelson, L. Knowledge and Acceptability of HIV pre-exposure prophylaxis (PrEP) among men who have sex with men (MSM) in Ghana. AIDS Care 2019, 32, 330–336. [Google Scholar] [CrossRef] [PubMed]
- Ogunbajo, A.; Kershaw, T.; Kushwaha, S.; Boakye, F.; Wallace-Atiapah, N.-D.; Nelson, L.E. Barriers, Motivators, and Facilitators to Engagement in HIV Care Among HIV-Infected Ghanaian Men Who have Sex with Men (MSM). AIDS Behav. 2017, 22, 829–839. [Google Scholar] [CrossRef] [PubMed]
- Nelson, L.E.; Wilton, L.; Agyarko-Poku, T.; Zhang, N.; Zou, Y.; Aluoch, M.; Apea, V.; Hanson, S.O.; Adu-Sarkodie, Y. Predictors of Condom Use among Peer Social Networks of Men Who Have Sex with Men in Ghana, West Africa. PLoS ONE 2015, 10, e0115504. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abubakari, G.M.; Nelson, L.E.; Ogunbajo, A.; Boakye, F.; Appiah, P.; Odhiambo, A.; Sa, T.; Zhang, N.; Ngozi, I.; Scott, A.; et al. Implementation and evaluation of a culturally grounded group-based HIV prevention programme for men who have sex with men in Ghana. Glob. Public Heath 2020, 16, 1028–1045. [Google Scholar] [CrossRef]
- Veronese, V.; Ryan, K.E.; Hughes, C.; Lim, M.S.; Pedrana, A.; Stoové, M. Using Digital Communication Technology to Increase HIV Testing Among Men Who Have Sex With Men and Transgender Women: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2020, 22, e14230. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, A.; Ferro, E.G.; Weikum, D.; Vagenas, P.; Lama, J.R.; Sánchez, J.; Altice, F.L. Communication technology use and mHealth acceptance among HIV-infected men who have sex with men in Peru: Implications for HIV prevention and treatment. AIDS Care 2014, 27, 273–282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Girault, P.; Green, K.; Clement, N.F.; Rahman, Y.A.A.; Adams, B.; Wambugu, S. Piloting a Social Networks Strategy to Increase HIV Testing and Counseling Among Men Who Have Sex with Men in Greater Accra and Ashanti Region, Ghana. AIDS Behav. 2015, 19, 1990–2000. [Google Scholar] [CrossRef]
- Cohen, S.; Underwood, L.G.; Gottlieb, B.H. Social Support Measurement and Intervention: A Guide for Health and Social Scientists; Oxford University Press: Oxford, UK, 2000. [Google Scholar]
- Wills, T.A.; Shinar, O. Measuring perceived and received social support. In Social Support Measurement and Intervention: A Guide for Health and Social Scientists; Cohen, S., Underwood, L.G., Gottlieb, B.H., Eds.; Oxford University Press: Oxford, UK, 2000; pp. 86–135. [Google Scholar]
- Wills, T.A. Supportive functions of interpersonal relationships. In Social Support and Health; Cohen, S., Syme, S.L., Eds.; Academic Press: Cambridge, MA, USA, 1985; pp. 61–82. [Google Scholar]
- Burleson, B.R.; Albrecht, T.L.; Sarason, I.G. Communication of Social Support: Messages, Interactions, Relationships, and Community; Sage Publications, Inc.: Washington, DC, USA, 1994. [Google Scholar]
- Kahn, R.L.; Antonucci, T.C. Convoys over the life course: Attachment, roles, and social support. Life-Span Dev. Behav. 1980, 253–286. Available online: https://agris.fao.org/agris-search/search.do?recordID=US201302069551 (accessed on 10 May 2021).
- House, J.S. Work Stress and Social Support; Addison-Wesley: Boston, MA, USA, 1981; Available online: https://www.econbiz.de/Record/work-stress-and-social-support-house-james/10004389064 (accessed on 10 May 2021).
- Wingwood, G.M.; Diclemente, R.J.; Stallworth, J.; Purcell, D.W.; Jean, R.; Villamizar, K.; Er, D.J.; Devarona, M.; Taveras, J.; Painter, T.M.; et al. Efficacy of a health educator-delivered HIV prevention intervention for Latina women: A randomized controlled trial. Am. J. Public Health 2011, 101, 2245–2252. [Google Scholar] [CrossRef]
- Wingood, G.M.; DiClemente, R.J. TheADAPT-ITT model: A novel method of adapting evidence-based HIV interventions. J. Acquir. Immune Defic. Syndr. 2008, 47, S40–S46. [Google Scholar] [CrossRef] [PubMed]
- Wingwood, G.M.; Simpson-Robinson, L.; Braxton, N.D.; Rainford, J.L. Design of a faith-based HIV intervention: Successful collaboration between a university and a church. Health Promot. Pract. 2011, 12, 823–831. [Google Scholar] [CrossRef]
- Dennis, C.-L. Peer support within a health care context: A concept analysis. Int. J. Nurs. Stud. 2003, 40, 321–332. [Google Scholar] [CrossRef]
- Degenhardt, L.; Mathers, B.; Vickerman, P.; Rhodes, T.; Latkin, C.; Hickman, M. Prevention of HIV infection for people who inject drugs: Why individual, structural, and combination approaches are needed. Lancet 2010, 376, 285–301. [Google Scholar] [CrossRef]
- Beyrer, C.; Wirtz, A.L.; Baral, S.; Peryskina, A.; Sifakis, F. Epidemiologic Links Between Drug Use and HIV Epidemics: An International Perspective. JAIDS J. Acquir. Immune Defic. Syndr. 2010, 55, S10–S16. [Google Scholar] [CrossRef] [Green Version]
- Berkman, L.F.; Glass, T.; Brissette, I.; Seeman, T.E. From social integration to health: Durkheim in the new millennium. Soc. Sci. Med. 2000, 51, 843–857. [Google Scholar] [CrossRef]
- Baral, S.; Beyrer, C.; Muessig, K.; Poteat, T.; Wirtz, A.L.; Decker, M.; Sherman, S.G.; Kerrigan, D. Burden of HIV among female sex workers in low-income and middle-income countries: A systematic review and meta-analysis. Lancet Infect. Dis. 2012, 12, 538–549. [Google Scholar] [CrossRef]
- Bluthenthal, R.; Lorvick, J.; Kral, A.; Erringer, E.; Kahn, J. Collateral damage in the war on drugs: HIV risk behaviors among injection drug users. Int. J. Drug Policy 1999, 10, 25–38. [Google Scholar] [CrossRef]
- Malinowska-Sempruch, K.; Hoover, J.; Alexandrova, A. Unintended Consequences: Drug Policies Fuel the HIV Epidemic in Russia and Ukraine. War on Drugs, HIV/AIDS, and Human Rights; Malinowska-Sempruch, K., Gallagher, S., Eds.; NYIdea Press: New York, NY, USA, 2004; pp. 194–211. [Google Scholar]
- Shangani, S.; Escudero, D.; Kirwa, K.; Harrison, A.; Marshall, B.; Operario, N. Effectiveness of peer-led interventions to increase HIV testing among men who have sex with men: A systematic review and meta-analysis. AIDS Care 2016, 29, 1003–1013. [Google Scholar] [CrossRef]
- Genberg, B.L.; Shangani, S.; Sabatino, K.; Rachlis, B.; Wachira, J.; Braitstein, P.; Operario, D. Improving Engagement in the HIV Care Cascade: A Systematic Review of Interventions Involving People Living with HIV/AIDS as Peers. AIDS Behav. 2016, 20, 2452–2463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doctor, A. The Effectiveness of a Nurse Designed Intervention Using Peer Teaching on HIV Knowledge, Hiv Testing, and Linkage to Care for African American Gay or Bisexual Men. Ph.D. Thesis, The Catholic University of America, Washington, DC, USA, 2021. [Google Scholar]
- Ko, N.-Y.; Hsieh, C.-H.; Wang, M.-C.; Lee, C.; Chen, C.-L.; Chung, A.-C.; Hsu, S.-T.; Yen, C.-F.; Marc, L.; Zhang, D. Effects of Internet Popular Opinion Leaders (iPOL) Among Internet-Using Men Who Have Sex with Men. J. Med. Internet Res. 2013, 15, e40. [Google Scholar] [CrossRef] [PubMed]
- Wilton, L.; Herbst, J.H.; Coury-Doniger, P.; Painter, T.M.; English, G.; Alvarez, M.E.; Scahill, M.; Roberson, M.A.; Lucas, B.; Johnson, W.D.; et al. Efficacy of an HIV/STI Prevention Intervention for Black Men Who Have Sex with Men: Findings from the Many Men, Many Voices (3MV) Project. AIDS Behav. 2009, 13, 532–544. [Google Scholar] [CrossRef]
- Dennis, C.-L. Postpartum depression peer support: Maternal perceptions from a randomized controlled trial. Int. J. Nurs. Stud. 2010, 47, 560–568. [Google Scholar] [CrossRef] [PubMed]
- Fleming, M. The Importance of Health Promotion Principles and Practices. Health Promotion in the 21st Century: New Approaches to Achieving Health for All; Allen & Unwin: London, UK, 2020; pp. 1–12. [Google Scholar]
- Tang, T.S.; Ayala, G.X.; Cherrington, A.; Rana, G. A Review of Volunteer-Based Peer Support Interventions in Diabetes. Diabetes Spectr. 2011, 24, 85–98. [Google Scholar] [CrossRef] [Green Version]
- Stojanovski, K.; Naja-Riese, G.; King, E.J.; Fuchs, J.D. A Systematic Review of the Social Network Strategy to Optimize HIV Testing in Key Populations to End the Epidemic in the United States. AIDS Behav. 2021, 25, 2680–2698. [Google Scholar] [CrossRef]
- Schumann, C.; Kahn, D.; Broaddus, M.; Dougherty, J.; Elderbrook, M.; Vergeront, J.; Westergaard, R. Implementing a Standardized Social Networks Testing Strategy in a Low HIV Prevalence Jurisdiction. AIDS Behav. 2018, 23, 41–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gaiter, J.L.; Johnson, W.D.; Taylor, E.; Thadiparthi, S.; Duncan-Alexander, T.; Lemon, C.; Turner, A.; Hickman, D.; Brown, N.; Aponte, E.; et al. Sisters Empowered, Sisters Aware: Three Strategies to Recruit African American Women for HIV Testing. AIDS Educ. Prev. 2013, 25, 190–202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGoy, S.L.; Pettit, A.C.; Morrison, M.; Alexander, L.R.; Johnson, P.; Williams, B.; Banister, D.; Young, M.K.; Wester, C.; Rebeiro, P.F. Use of Social Network Strategy Among Young Black Men Who Have Sex with Men for HIV Testing, Linkage to Care, and Reengagement in Care, Tennessee, 2013–2016. Public Health Rep. 2018, 133, 43S–51S. [Google Scholar] [CrossRef] [PubMed]
- Kimbrough, L.W.; Fisher, H.E.; Jones, K.T.; Johnson, W.; Thadiparthi, S.; Dooley, S. Accessing Social Networks with High Rates of Undiagnosed HIV Infection: The Social Networks Demonstration Project. Am. J. Public Health 2009, 99, 1093–1099. [Google Scholar] [CrossRef] [PubMed]
- Holloway, I.W.; Rice, E.; Gibbs, J.; Winetrobe, H.; Dunlap, S.; Rhoades, H. Acceptability of Smartphone Application-Based HIV Prevention Among Young Men Who Have Sex with Men. AIDS Behav. 2013, 18, 285–296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muessig, K.E.; Pike, E.C.; Fowler, B.; Legrand, S.; Parsons, J.; Bull, S.S.; Wilson, P.A.; Wohl, D.A.; Hightow-Weidman, L.B. Putting Prevention in Their Pockets: Developing Mobile Phone-Based HIV Interventions for Black Men Who Have Sex with Men. AIDS Patient Care STDs 2013, 27, 211–222. [Google Scholar] [CrossRef] [PubMed]
- Hay, K.; Kwardem, L.; Welbourn, A.; Namiba, A.; Tariq, S.; Coventry, L.; Dhairyawan, R.; Durrant, A. “Support for the supporters”: A qualitative study of the use of WhatsApp by and for mentor mothers with HIV in the UK. AIDS Care 2020, 32, 127–135. [Google Scholar] [CrossRef]
| Session | Modules/Exercise Description |
|---|---|
| ONE: Build Rapport and Confidentiality between Peer Mentors, Mentees, and other Team Members. Create space for familiarization and setting of a conducive environment for the remainder of the sessions. | A. We created introductory activities, and used energizers, such as songs and body movements, to welcome mentors, and create conversation. B. Setting of ground rules for the training. Mentors brainstormed and created a list of rules and expectations on a flip chart; we discussed the list, and signed them to show adherence. Some key rules include punctuality, no disturbances, unnecessary noise, cell phones, respect for each other, etc. C. Expectations and objectives. Mentors created a list of expectations, and we provided an oversight on the drivers of the intervention. D. Characteristics of a peer mentor. We use the same process as B and C to allow mentors to establish their understanding of a peer mentor, and their best characteristics. We then discussed the characteristics, and how to exhibit such characteristics. E. Confidentiality exercise. We created an activity to show the importance of confidentiality, and discussed the role of confidentiality in peer mentoring. |
| TWO: Understand Intersectional Stigma and How it Impacts HIV Care for MSM. Build participant understanding of the connection between stigma and health seeking behaviors/experiences (e.g., HIV testing, and retention to care), and ways to reduce intersectional stigma. | A. Stigma, Discrimination, and Intersectionality. We led a discussion on understanding stigma by asking mentors to define stigma, and provide examples supporting their explanations with a working definition. We then used examples in the Ghanaian context to depict intersectional stigma. We then implemented a matching terminology activity where pairs try to identify corresponding definitions related to our intervention; examples include stigma, outing, closeted, etc. B. MSM Experiences with Intersectional Stigma. Mentors reflected, shared, and discussed their personal experiences living as MSM in Ghana. C. HIV and Stigma. Mentors discussed in groups the meaning of HIV-related stigma, why HIV stigma exists, and how it affects people living with HIV, and discussed the consequences of stigma within healthcare sectors in their experiences. D. Reducing Stigma: Mentors brainstorm on reducing intersectional stigma in Ghana, and shared their personal recommendations through group discussions. |
| THREE: The Dennis Peer Support Model and the Role of Peer Mentors. Create peer mentors’ understanding on the DPSM, and its components on peer support (emotional, informational, and appraisal), and examine the role of peer mentors in providing support on dealing with intersectional stigma. | A. DPSM and its components. We used a PowerPoint presentation to explain the DPSM model and the various components. We then split mentors into groups to discuss the various components: emotional; information; appraisal/affirmatory support; and the sources of such support for them as mentors. B. Emotional. We used focused group discussions to brainstorm personal difficulties or self-esteem threats facing MSM, gender non-conforming MSM, and HIV+ MSM in Ghana (i.e., doubts about ability, social attractiveness), and established some of the mechanisms of emotional support (i.e., expressions of caring, encouragement, attentive listening, reflection, reassurance, and commonly avoiding criticism or exhortatory advice-giving) that they could offer mentees. C. Informational. Mentors defined information support and situations where they could provide informational support (HIV symptoms, questions about medication usage or side-effects, questions about other support groups for MSM or PLWHA in Ghana). D. Appraisal/Affirmational. Mentors examined affirmational support and the mechanisms of affirmational support (i.e., encouragement to persist in problem resolution, reassurances that efforts will result in positive outcomes, assistance to endure frustration, and communication of optimism). E. Distinguish Peer Support. We read scenarios, and asked mentors to explain the kind of support needed, and we provided additional explanations when needed. Examples of scenarios (e.g., an individual wants to disclose their HIV status to their parents, but is nervous, and he asks if he can walk through the conversation with you; an individual has a partner who is concerned they might have been infected with HIV; they want to know the nearest free testing center). F. Identifying Peer Support Need. Mentors formed groups, and created a play of their choice showing an MSM experiencing at least two intersecting stigmas at a health care facility, and they acted it out to allow the other peers to identify the kind of support the person needed. |
| FOUR: Effective Communication in Delivering Peer Support. Implementing emotional, and appraisal/affirmatory support using strategies for effective communications, empathetic listening and texting, as well as the strategy of LARA. | A. Effective Communication Strategies. Mentors discussed communication and its importance in groups, and facilitators provided a working definition and strategies (such as, focus on the issue and not the person, be genuine and not manipulative, show empathy, be flexible and open-minded, share experiences, ask questions, and express positive feelings, the 5Cs of effective communication—clear, cohesive, complete, concise, and concrete). B. Empathetic Listening and Texting. Mentors discussed empathetic listening and texting (paying attention, showing empathy, emotional identification, compassion, feeling, insight, the basic principle “seek to understand, before being understood”). They practice listening in role plays, and texting via WhatsApp. C. Non-Violent Communication: LARA. We provided an overview of LARA: listen (very carefully); affirm a feeling or value you share with the client; respond directly to the concerns or questions the client has raised; ask questions or add information. Mentors then practiced using their scenarios. |
| FIVE: Self-Efficacy. Develop self-efficacy and effective communication on sexual health, HIV, and risk reduction strategies among MSM. | A. Self-Efficacy. The purpose of this module is to enable mentors understand self-efficacy and ways to develop self-efficacy. We provided an overview of self-efficacy, and reviewed the different ways self-efficacy can be developed with mentors (e.g., performance accomplishment, verbal persuasion, physiological states). We discussed ways of withdrawing from difficult tasks, lack of concentration, energy spent focusing on limitations and failures, etc. C. Negative/Positive Message Exercise. Mentors discussed how self-talk affects self-efficacy. They created statements on why they believe they cannot be successful as MSM/as a PLWHA (“I don’t think I am a model for living with HIV/AIDS”, “I don’t think I am motivated enough to live with my illness.”, or “I am too effeminate to be considered a man”, etc.), and discarded the statements, and rewrote positive versions of the statements to apply in their lives. D. Motivational Interviewing. We discussed how mentors can develop interview skills which will foster social support (asking permission, eliciting/evoking change, provoking extremes, looking forward, importance and confidence ratings, open-ended questions). They practiced interviewing using these tips for feedback. E. Resources for self-care and effective coping. Mentors discussed the difference between effective coping and self-efficacy (i.e., focus on action instead of belief of self-worth or ability to accomplish given task; self-care—activities and practices that we can engage in on a regular basis to reduce stress, and maintain and enhance our short- and longer-term health and wellbeing). |
| SIX: Other Areas of Support, Usage of HIVE3 Platform, Signing up Gain the knowledge and skills to deal with other issues, such as economic stress and other types of stress that MSM go through. Train peer mentors to use the mobile application to link peer groups from the HIVE3 platform to operate as sub-groups. | A. Recap from the previous session. Mentors shared lessons from the previous sessions, and asked questions for clarifications. B. Dealing with economic stress and other stress. We provided an overview of economic related stress, family stress, psychosocial stress, etc., and how to deal or manage these stresses. We examine ways to deal with economic stress, for example, how to be entrepreneurial. C. Training on the Use of Mobile Application. We discussed the use of mobile phones and applications to manage discussion with peer mentors. Phones were given t o mentors on a later date, and they currently use them to provide support to participants. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abubakari, G.M.; Owusu-Dampare, F.; Ogunbajo, A.; Gyasi, J.; Adu, M.; Appiah, P.; Torpey, K.; Nyblade, L.; Nelson, L.E. HIV Education, Empathy, and Empowerment (HIVE3): A Peer Support Intervention for Reducing Intersectional Stigma as a Barrier to HIV Testing among Men Who Have Sex with Men in Ghana. Int. J. Environ. Res. Public Health 2021, 18, 13103. https://doi.org/10.3390/ijerph182413103
Abubakari GM, Owusu-Dampare F, Ogunbajo A, Gyasi J, Adu M, Appiah P, Torpey K, Nyblade L, Nelson LE. HIV Education, Empathy, and Empowerment (HIVE3): A Peer Support Intervention for Reducing Intersectional Stigma as a Barrier to HIV Testing among Men Who Have Sex with Men in Ghana. International Journal of Environmental Research and Public Health. 2021; 18(24):13103. https://doi.org/10.3390/ijerph182413103
Chicago/Turabian StyleAbubakari, Gamji M’Rabiu, Francis Owusu-Dampare, Adedotun Ogunbajo, Joseph Gyasi, Michael Adu, Patrick Appiah, Kwasi Torpey, Laura Nyblade, and LaRon E. Nelson. 2021. "HIV Education, Empathy, and Empowerment (HIVE3): A Peer Support Intervention for Reducing Intersectional Stigma as a Barrier to HIV Testing among Men Who Have Sex with Men in Ghana" International Journal of Environmental Research and Public Health 18, no. 24: 13103. https://doi.org/10.3390/ijerph182413103
APA StyleAbubakari, G. M., Owusu-Dampare, F., Ogunbajo, A., Gyasi, J., Adu, M., Appiah, P., Torpey, K., Nyblade, L., & Nelson, L. E. (2021). HIV Education, Empathy, and Empowerment (HIVE3): A Peer Support Intervention for Reducing Intersectional Stigma as a Barrier to HIV Testing among Men Who Have Sex with Men in Ghana. International Journal of Environmental Research and Public Health, 18(24), 13103. https://doi.org/10.3390/ijerph182413103






