Habitual Physical Activity and Diabetes Control in Young and Older Adults with Type II Diabetes: A Longitudinal Correlational Study
Abstract
:1. Introduction
2. Methods
2.1. Research Design
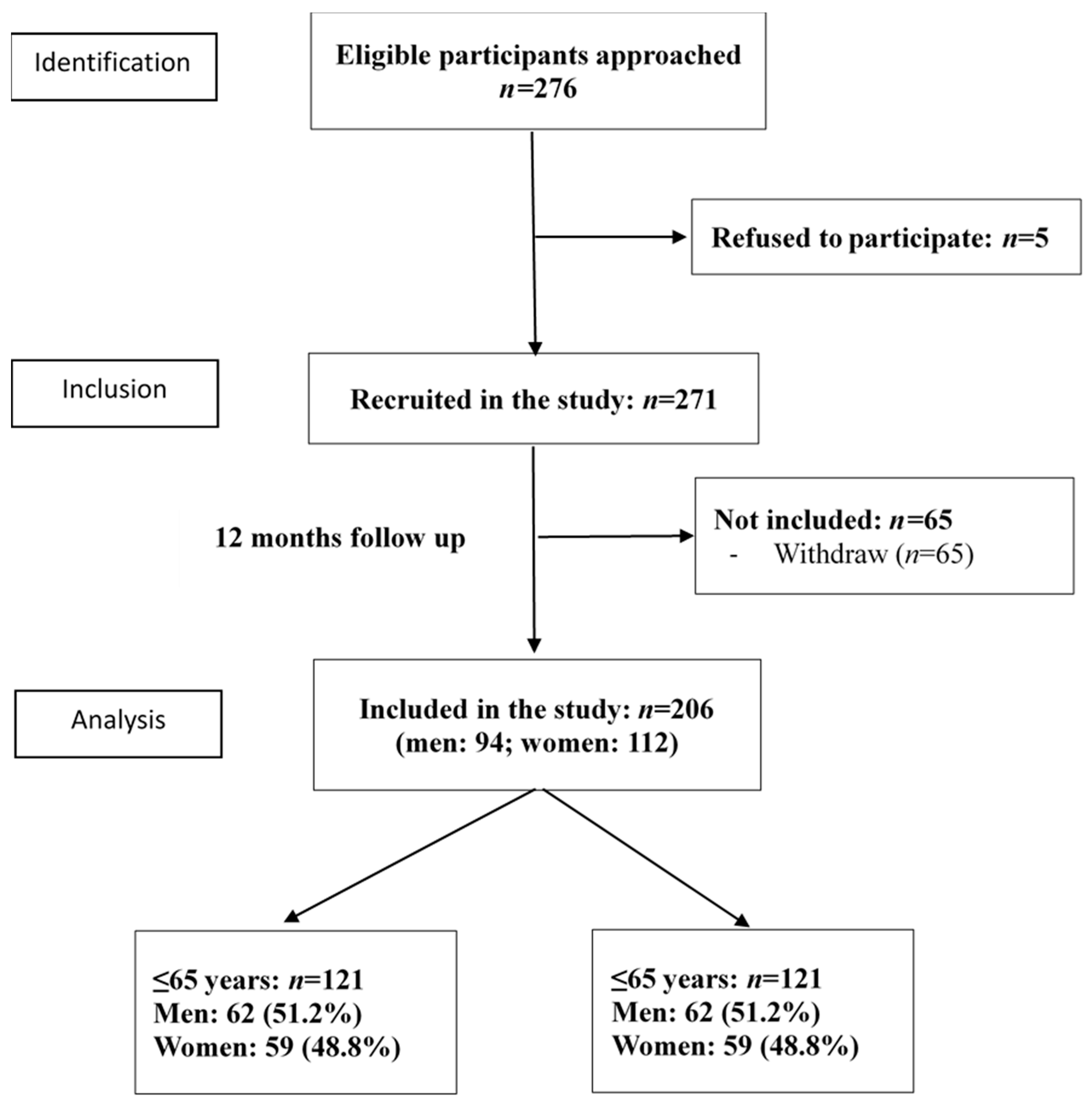
2.2. Participants
2.3. Measurements
2.4. Data Analysis
3. Results
3.1. Demographic Characteristics
3.2. Diabetes Control in Young and Older Patients with T2DM
3.3. Daily Habitual Physical Activity in Young and Older Patients with T2DM
3.4. Association of Habitual Physical Activity with Diabetes Control in Patients with T2DM
4. Discussion
4.1. Diabetes Control in Young and Older T2DM Patients
4.2. Habitual Physical Activity in Young and Older T2DM Patients
4.3. Limitations and Implications
5. Conclusions and Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| T2DM | type II Diabetes mellitus |
| ADA | American Diabetes Association |
| HbA1c | Hemoglobin A1c |
| IPAQ | International Physical Activity Questionnaire. |
| LDL-C | low-density lipoprotein cholesterol |
| VO2 max | maximal oxygen uptake. |
| VO2 peak | peak oxygen uptake. |
| MMSE | Mini-Mental State Examination |
| HADS | Hospital Anxiety and Depression Scale |
| MET | metabolic equivalent |
References
- Jiang, Y.D.; Chang, C.H.; Tai, T.Y.; Chen, J.F.; Chuang, L.M. Incidence and prevalence rates of diabetes mellitus in Taiwan: Analysis of the 2000-2009 Nationwide Health Insurance database. J. Formos Med. Assoc. 2012, 111, 599–604. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nanayakkara, N.; Curtis, A.J.; Heritier, S.; Gadowski, A.M.; Pavkov, M.E.; Kenealy, T.; Owens, D.R.; Thomas, R.L.; Song, S.; Wong, J.; et al. Impact of age at type 2 diabetes mellitus diagnosis on mortality and vascular complications: Systematic review and meta-analyses. Diabetologia 2021, 64, 275–287. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes, A. 14. Diabetes Care in the Hospital: Standards of Medical Care in Diabetes-2018. Diabetes Care 2018, 41, S144–S151. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asano, R.Y.; Sales, M.M.; Browne, R.A.; Moraes, J.F.; Coelho Junior, H.J.; Moraes, M.R.; Simoes, H.G. Acute effects of physical exercise in type 2 diabetes: A review. World J. Diabetes 2014, 5, 659–665. [Google Scholar] [CrossRef] [PubMed]
- Jan, C.F.; Chang, H.C.; Tantoh, D.M.; Chen, P.H.; Liu, W.H.; Huang, J.Y.; Wu, M.C.; Liaw, Y.P. Duration-response association between exercise and HDL in both male and female Taiwanese adults aged 40 years and above. Oncotarget 2018, 9, 2120–2127. [Google Scholar] [CrossRef] [PubMed]
- Irvine, C.; Taylor, N.F. Progressive resistance exercise improves glycaemic control in people with type 2 diabetes mellitus: A systematic review. Aust. J. Physiother. 2009, 55, 237–246. [Google Scholar] [CrossRef] [Green Version]
- Umpierre, D.; Ribeiro, P.A.; Kramer, C.K.; Leitao, C.B.; Zucatti, A.T.; Azevedo, M.J.; Gross, J.L.; Ribeiro, J.P.; Schaan, B.D. Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes: A systematic review and meta-analysis. JAMA 2011, 305, 1790–1799. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hansen, D.; Dendale, P.; Jonkers, R.A.; Beelen, M.; Manders, R.J.; Corluy, L.; Mullens, A.; Berger, J.; Meeusen, R.; van Loon, L.J. Continuous low- to moderate-intensity exercise training is as effective as moderate- to high-intensity exercise training at lowering blood HbA(1c) in obese type 2 diabetes patients. Diabetologia 2009, 52, 1789–1797. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Dijk, J.W.; Tummers, K.; Stehouwer, C.D.; Hartgens, F.; van Loon, L.J. Exercise therapy in type 2 diabetes: Is daily exercise required to optimize glycemic control? Diabetes Care 2012, 35, 948–954. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsu, C.H.H.; Tsao, T.H.; Chang, H.W. A preliminary study of recommendations for physical activity for patients with type 2 diabetes. Taiwan J. Public Health 2011, 30, 72–81. [Google Scholar] [CrossRef]
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985, 100, 126–131. [Google Scholar] [PubMed]
- Subramaniam, M.; Zhang, Y.; Lau, J.H.; Vaingankar, J.A.; Abdin, E.; Chong, S.A.; Lee, E.S. Patterns of physical activity and health-related quality of life amongst patients with multimorbidity in a multi-ethnic Asian population. BMC Public Health 2019, 19, 1612. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mynarski, W.; Psurek, A.; Borek, Z.; Rozpara, M.; Grabara, M.; Strojek, K. Declared and real physical activity in patients with type 2 diabetes mellitus as assessed by the International Physical Activity Questionnaire and Caltrac accelerometer monitor: A potential tool for physical activity assessment in patients with type 2 diabetes mellitus. Diabetes Res. Clin. Pract. 2012, 98, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Liou, Y.M.; Jwo, C.J.; Yao, K.G.; Chiang, L.C.; Huang, L.H. Selection of appropriate Chinese terms to represent intensity and types of physical activity terms for use in the Taiwan version of IPAQ. J. Nurs. Res. 2008, 16, 252–263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diabetes Association Of The Republic Of China, T. Executive summary of the DAROC clinical practice guidelines for diabetes care-2018. J. Formos Med. Assoc. 2020, 119, 577–586. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.Y.; Yu, N.C.; Sheu, W.H.; Tsai, S.T.; Tai, T.Y. Team care of type 2 diabetes mellitus in Taiwan. Diabetes Res. Clin. Pract. 2014, 106 (Suppl. 2), S309–S313. [Google Scholar] [CrossRef]
- Nam, G.E.; Han, B.; Joo, C.L.; Kang, S.Y.; Lim, J.; Kim, Y.H.; Park, H.S. Poor Control of Blood Glucose, Lifestyle, and Cardiometabolic Parameters in Younger Adult Patients with Type 2 Diabetes Mellitus. J. Clin. Med. 2019, 8, 1405. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wen, C.P.; Wai, J.P.; Tsai, M.K.; Yang, Y.C.; Cheng, T.Y.; Lee, M.C.; Chan, H.T.; Tsao, C.K.; Tsai, S.P.; Wu, X. Minimum amount of physical activity for reduced mortality and extended life expectancy: A prospective cohort study. Lancet 2011, 378, 1244–1253. [Google Scholar] [CrossRef]
- Golightly, Y.M.; Allen, K.D.; Ambrose, K.R.; Stiller, J.L.; Evenson, K.R.; Voisin, C.; Hootman, J.M.; Callahan, L.F. Physical Activity as a Vital Sign: A Systematic Review. Prev. Chronic Dis. 2017, 14, E123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Variable | All Patients | ≤65 Years | >65 Years | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | X2 | p | |
| Gender | 206 | 100 | 121 | 58.7 | 85 | 41.3 | 3.718 | 0.054 |
| Men | 94 | 45.6 | 62 | 51.2 | 32 | 37.6 | ||
| Women | 112 | 54.4 | 59 | 48.8 | 53 | 62.4 | ||
| Occupation | 34.191 | 0.000 | ||||||
| Unemployed/retired | 138 | 67 | 63 | 52.1 | 75 | 88.3 | ||
| Working | 68 | 33 | 58 | 47.9 | 10 | 11.8 | ||
| Education level | 20.265 | 0.000 | ||||||
| Illiterate | 25 | 12.1 | 5 | 4.1 | 20 | 23.5 | ||
| <12years | 147 | 71.4 | 90 | 74.4 | 57 | 67.1 | ||
| >12years | 34 | 16.5 | 26 | 21.5 | 8 | 9.4 | ||
| Marital status | 2.910 | 0.088 | ||||||
| Married | 160 | 77.7 | 99 | 81.8 | 61 | 71.8 | ||
| Single/Divorced/separated/Widowed | 46 | 22.3 | 22 | 18.2 | 24 | 28.2 | ||
| Number of years diagnosed | 26.732 | 0.000 | ||||||
| 1 to 5 years | 27 | 13.1 | 23 | 19 | 4 | 4.7 | ||
| 6 to 10 years | 58 | 28.2 | 40 | 33.1 | 18 | 21.2 | ||
| 11 to 15 years | 55 | 26.7 | 32 | 26.4 | 23 | 27.1 | ||
| 16 to 20 years | 35 | 17 | 19 | 15.7 | 16 | 18.8 | ||
| >20 years | 28 | 13.6 | 6 | 5 | 22 | 25.9 | ||
| Primary caregiver | 7.896 | 0.005 | ||||||
| Husband or wife | 126 | 61.2 | 84 | 69.4 | 42 | 49.4 | ||
| Others | 79 | 38.5 | 37 | 30.6 | 42 | 50.0 | ||
| Living condition | ||||||||
| Living with spouse or children | 187 | 91 | 110 | 90.9 | 77 | 90.6 | 2.954 | 0.228 |
| Solitary | 13 | 6.3 | 6 | 5 | 7 | 8.2 | ||
| Others | 3 | 1.5 | 3 | 2.5 | 0 | 0 | ||
| BMI, kg/m2 | 14.26 | 0.003 | ||||||
| Underweight (<18.5) | 4 | 1.9 | 3 | 2.5 | 1 | 1.2 | ||
| Normal(18.5~24) | 69 | 33.5 | 31 | 25.6 | 38 | 44.7 | ||
| Overweight(24–27) | 61 | 29.6 | 33 | 27.3 | 28 | 32.9 | ||
| Obese(>27) | 72 | 35 | 54 | 44.6 | 18 | 21.2 | ||
| Medications | ||||||||
| Metformin or other oral drugs | 163 | 79.1% | 98 | 81.0% | 65 | 76.5% | 1.046 | 0.790 |
| Insulin injection | 30 | 14.6% | 17 | 14.0% | 13 | 15.3% | ||
| Combine insulin and other oral drugs | 11 | 5.3% | 5 | 4.1% | 6 | 7.1% | ||
| Glycemic control | 0.556 | 0.456 | ||||||
| HbA1c ≤ 7% | 62 | 30.1 | 34 | 28.1 | 28 | 32.9 | ||
| HbA1c > 7% | 144 | 69.9 | 87 | 71.9 | 57 | 67.1 | ||
| Blood pressure control 1 | 13.75 | 0.000 | ||||||
| Normal | 76 | 36.9 | 32 | 26.4 | 44 | 51.8 | ||
| Abnormal | 130 | 63.1 | 89 | 73.6 | 41 | 48.2 | ||
| LDL-C control | 6.541 | 0.011 | ||||||
| ≤100 mg/dl | 87 | 42.2 | 42 | 34.7 | 45 | 52.9 | ||
| >100 mg/dl | 110 | 53.4 | 73 | 60.3 | 37 | 43.5 | ||
| Diabetes control 2 | 3.823 | 0.051 | ||||||
| Normal | 8 | 3.9 | 2 | 1.7 | 6 | 7.1 | ||
| Abnormal | 189 | 91.7 | 113 | 93.4 | 76 | 89.4 | ||
| Complications 3 | ||||||||
| Neuropathy | 34 | 16.5 | 21 | 17.4 | 13 | 15.3 | 0.154 | 0.695 |
| Cardiovascular | 36 | 17.5 | 14 | 11.6 | 22 | 25.9 | 7.091 | 0.008 |
| Nephropathy | 13 | 6.3 | 11 | 9.1 | 2 | 2.4 | 3.834 | 0.050 |
| Eye problems | 59 | 28.6 | 14 | 11.6 | 45 | 52.9 | 41.811 | 0.000 |
| All Patients | ≤65 Years | >65 Years | ||||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | t | p | |
| Frequency of performing physical activity (day/week) | ||||||||
| High intensity physical activities | 0.36 | 1.316 | 0.5 | 1.6 | 0.1 | 0.7 | 2.248 | 0.026 |
| Moderate intensity physical activities | 1.22 | 2.463 | 0.9 | 2.0 | 1.7 | 2.9 | −2.32 | 0.022 |
| Low intensity physical activities | 4.02 | 2.927 | 3.8 | 2.8 | 4.3 | 3.1 | −1.325 | 0.187 |
| Amount of time spent on physical activities (minute/day) | ||||||||
| High intensity physical activities | 11.54 | 46.953 | 13.2 | 47.4 | 9.2 | 46.5 | 0.605 | 0.546 |
| Moderate intensity physical activities | 15.78 | 38.615 | 13.8 | 41.0 | 18.6 | 34.9 | −0.894 | 0.373 |
| Low intensity physical activities | 43.77 | 66.508 | 47.1 | 75.4 | 39.1 | 51.6 | 0.855 | 0.393 |
| Sedentary activities 1 | 300.23 | 131.759 | 290.7 | 133.7 | 314.3 | 128.5 | −1.158 | 0.249 |
| Amount of time spent on physical activities (minute/week) 2 | ||||||||
| High intensity physical activities | 40.6 | 202.1 | 51.8 | 226.8 | 24.7 | 160.6 | 0.946 | 0.345 |
| Moderate intensity physical activities | 85.0 | 232.8 | 62.4 | 234.9 | 117.0 | 227.2 | −1.673 | 0.096 |
| Low intensity physical activities | 254.0 | 448.3 | 260.6 | 504.0 | 244.7 | 357.0 | 0.25 | 0.803 |
| Total physical activities (METs) | 1388.0 | 1954.5 | 1373.4 | 2183.0 | 1408.9 | 1585.5 | 0.946 | 0.345 |
| n | % | n | % | n | % | X2 | p | |
| Intensity of physical activities | 0.729 | 0.695 | ||||||
| Performing high intensity of physical activities 3 | 24 | 11.7 | 13 | 10.7 | 11 | 12.9 | ||
| Performing moderate intensity of physical activities 4 | 105 | 51.0 | 60 | 49.6 | 45 | 52.9 | ||
| Performing low intensity of physical activities 5 | 77 | 37.4 | 48 | 39.7 | 29 | 34.1 | ||
| Glycemic Control | Blood Pressure Control 3 | LDL-C Control | Diabetes Control 4 | |||||
|---|---|---|---|---|---|---|---|---|
| r | p | r | p | r | p | r | p | |
| All patients | ||||||||
| Frequency of performing physical activity (day/week) | ||||||||
| High intensity physical activities | −0.040 | 0.564 | 0.155 | 0.027 | 0.102 | 0.155 | 0.036 | 0.612 |
| Moderate intensity physical activities | −0.157 | 0.024 | −0.092 | 0.190 | −0.063 | 0.378 | −0.022 | 0.761 |
| Low intensity physical activities | 0.004 | 0.950 | −0.126 | 0.071 | −0.026 | 0.717 | −0.088 | 0.217 |
| Amount of time spent on physical activities (minute/day) | ||||||||
| High intensity physical activities | 0.013 | 0.849 | 0.076 | 0.280 | −0.018 | 0.801 | −0.048 | 0.502 |
| Moderate intensity physical activities | −0.113 | 0.105 | −0.002 | 0.982 | 0.019 | 0.788 | 0.010 | 0.894 |
| Low intensity physical activities | −0.049 | 0.485 | −0.003 | 0.971 | 0.015 | 0.832 | 0.038 | 0.602 |
| Sedentary activities 1 | 0.042 | 0.584 | −0.12 | 0.115 | −0.044 | 0.578 | −0.094 | 0.232 |
| Amount of time spent on physical activities (minute/week) 2 | ||||||||
| High intensity physical activities | 0.054 | 0.439 | 0.123 | 0.077 | 0.027 | 0.704 | 0.018 | 0.805 |
| Moderate intensity physical activities | −0.163 | 0.019 | −0.056 | 0.422 | 0.033 | 0.642 | −0.003 | 0.962 |
| Low intensity physical activities | −0.066 | 0.348 | −0.015 | 0.826 | −0.008 | 0.906 | 0.025 | 0.724 |
| Total physical activities (METs) | −0.099 | 0.158 | 0.036 | 0.610 | 0.029 | 0.687 | 0.027 | 0.711 |
| Intensity of physical activities 5 | −0.113 | 0.106 | −0.009 | 0.903 | 0.020 | 0.783 | −0.036 | 0.613 |
| ≤65 years | ||||||||
| Frequency of performing physical activity (day/week) | ||||||||
| High intensity physical activities | −0.088 | 0.338 | 0.135 | 0.141 | 0.116 | 0.218 | 0.050 | 0.597 |
| Moderate intensity physical activities | −0.206 | 0.024 | 0.054 | 0.558 | −0.076 | 0.419 | −0.067 | 0.476 |
| Low intensity physical activities | 0.006 | 0.944 | −0.131 | 0.151 | 0.003 | 0.972 | 0.003 | 0.974 |
| Amount of time spent on physical activities (minute/day) | ||||||||
| High intensity physical activities | 0.048 | 0.604 | 0.043 | 0.641 | 0.069 | 0.465 | 0.014 | 0.881 |
| Moderate intensity physical activities | −0.107 | 0.244 | 0.106 | 0.249 | 0.008 | 0.934 | 0.025 | 0.790 |
| Low intensity physical activities | −0.007 | 0.937 | −0.136 | 0.140 | 0.008 | 0.934 | 0.071 | 0.454 |
| Sedentary activities 1 | 0.046 | 0.646 | −0.040 | 0.688 | −0.031 | 0.765 | −0.095 | 0.354 |
| Amount of time spent on physical activities (minute/week) 2 | ||||||||
| High intensity physical activities | 0.049 | 0.591 | 0.104 | 0.257 | 0.077 | 0.413 | 0.041 | 0.66 |
| Moderate intensity physical activities | −0.162 | 0.076 | 0.066 | 0.470 | 0.048 | 0.609 | 0.020 | 0.830 |
| Low intensity physical activities | −0.021 | 0.815 | −0.132 | 0.149 | −0.007 | 0.939 | 0.070 | 0.458 |
| Total physical activities (METs) | −0.063 | 0.495 | 0.005 | 0.953 | 0.066 | 0.483 | 0.084 | 0.372 |
| Intensity of physical activities 5 | −0.080 | 0.381 | −0.036 | 0.693 | 0.048 | 0.614 | 0.023 | 0.803 |
| >65 years | ||||||||
| Frequency of performing physical activity (day/week) | ||||||||
| High intensity physical activities | 0.067 | 0.546 | 0.139 | 0.207 | −0.011 | 0.919 | −0.007 | 0.949 |
| Moderate intensity physical activities | −0.103 | 0.35 | −0.141 | 0.197 | 0.002 | 0.983 | −0.030 | 0.791 |
| Low intensity physical activities | 0.013 | 0.908 | −0.077 | 0.484 | −0.021 | 0.851 | −0.126 | 0.258 |
| Amount of time spent on physical activities (minute/day) | ||||||||
| High intensity physical activities | −0.04 | 0.719 | 0.099 | 0.369 | −0.152 | 0.173 | −0.122 | 0.274 |
| Moderate intensity physical activities | −0.117 | 0.285 | −0.118 | 0.281 | 0.064 | 0.565 | −0.005 | 0.967 |
| Low intensity physical activities | −0.145 | 0.187 | 0.190 | 0.082 | 0.000 | 0.997 | 0.037 | 0.738 |
| Sedentary activities 1 | 0.047 | 0.700 | −0.188 | 0.119 | −0.038 | 0.762 | −0.148 | 0.233 |
| Amount of time spent on physical activities (minute/week) 2 | ||||||||
| High intensity physical activities | 0.057 | 0.606 | 0.129 | 0.238 | −0.098 | 0.383 | −0.008 | 0.946 |
| Moderate intensity physical activities | −0.153 | 0.163 | −0.150 | 0.171 | 0.062 | 0.581 | −0.006 | 0.959 |
| Low intensity physical activities | −0.157 | 0.151 | 0.176 | 0.107 | −0.022 | 0.842 | 0.016 | 0.890 |
| Total physical activities (METs) | −0.170 | 0.119 | 0.101 | 0.358 | −0.035 | 0.753 | 0.002 | 0.985 |
| Intensity of physical activities 5 | −0.151 | 0.168 | 0.061 | 0.581 | 0.008 | 0.941 | −0.084 | 0.453 |
| Univariate | Multiple | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Wald | p | OR | 95% CI | Wald | p | OR | 95% CI | |||
| On Glycemic Control (HbA1c) | ||||||||||
| Frequency of performing moderate physical activity (day/week) | 4.909 | 0.027 | 0.879 | 0.784 | 0.985 | 3.571 | 0.059 | 0.889 | 0.787 | 1.004 |
| Age (≤65 vs. >65) 1 | 0.555 | 0.456 | 0.796 | 0.436 | 1.452 | 1.557 | 0.212 | 0.648 | 0.328 | 1.281 |
| Sex (female vs. male) 2 | 0.047 | 0.829 | 0.936 | 0.515 | 1.701 | 0.212 | 0.645 | 0.863 | 0.462 | 1.614 |
| Number of years diagnosed | 4.925 | 0.026 | 1.054 | 1.006 | 1.104 | 6.467 | 0.011 | 1.067 | 1.015 | 1.121 |
| Performing moderate intensity physical activities (minutes/week) | 4.199 | 0.040 | 0.998 | 0.997 | 1.000 | 3.864 | 0.049 | 0.999 | 0.997 | 1.000 |
| Age (≤65 vs. >65) 1 | 0.555 | 0.456 | 0.796 | 0.436 | 1.452 | 1.813 | 0.178 | 0.626 | 0.316 | 1.238 |
| Sex (female vs. male) 2 | 0.047 | 0.829 | 0.936 | 0.515 | 1.701 | 0.289 | 0.591 | 0.842 | 0.449 | 1.578 |
| Number of years diagnosed | 4.925 | 0.026 | 1.054 | 1.006 | 1.104 | 6.943 | 0.008 | 1.070 | 1.017 | 1.124 |
| On Blood Pressure | ||||||||||
| Frequency of performing high physical activity (day/week) | 3.465 | 0.063 | 1.513 | 0.978 | 2.341 | 3.130 | 0.077 | 1.495 | 0.958 | 2.335 |
| Age (≤65 vs. >65) 1 | 13.345 | 0.000 | 0.335 | 0.186 | 0.602 | 9.556 | 0.002 | 0.364 | 0.192 | 0.691 |
| Sex (female vs. male) 2 | 0.009 | 0.926 | 0.973 | 0.552 | 1.718 | 0.912 | 0.339 | 0.741 | 0.401 | 1.371 |
| Number of years diagnosed | 4.447 | 0.035 | 0.961 | 0.925 | 0.997 | 0.391 | 0.532 | 0.987 | 0.948 | 1.028 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, C.-H.; Kuo, C.-P.; Huang, C.-N.; Hwang, S.-L.; Liao, W.-C.; Lee, M.-C. Habitual Physical Activity and Diabetes Control in Young and Older Adults with Type II Diabetes: A Longitudinal Correlational Study. Int. J. Environ. Res. Public Health 2021, 18, 1330. https://doi.org/10.3390/ijerph18031330
Chang C-H, Kuo C-P, Huang C-N, Hwang S-L, Liao W-C, Lee M-C. Habitual Physical Activity and Diabetes Control in Young and Older Adults with Type II Diabetes: A Longitudinal Correlational Study. International Journal of Environmental Research and Public Health. 2021; 18(3):1330. https://doi.org/10.3390/ijerph18031330
Chicago/Turabian StyleChang, Chia-Hsun, Ching-Pyng Kuo, Chien-Ning Huang, Shiow-Li Hwang, Wen-Chun Liao, and Meng-Chih Lee. 2021. "Habitual Physical Activity and Diabetes Control in Young and Older Adults with Type II Diabetes: A Longitudinal Correlational Study" International Journal of Environmental Research and Public Health 18, no. 3: 1330. https://doi.org/10.3390/ijerph18031330








