The Psychological Consequences of COVID-19 Fear and the Moderator Effects of Individuals’ Underlying Illness and Witnessing Infected Friends and Family
Abstract
1. Introduction
1.1. COVID-19 Fear of Individuals
1.2. The Effect of COVID-19 Fear on Depression, Anxiety, and Stress
1.3. Moderation Roles of Underling Illness and Having Infected or Dead Relatives and/or Friends
2. Method
2.1. Study Design, Participants, and Procedure
2.2. Data Analysis
2.3. Measures
3. Results
3.1. Descriptive Analysis
3.2. Correlations between Variables
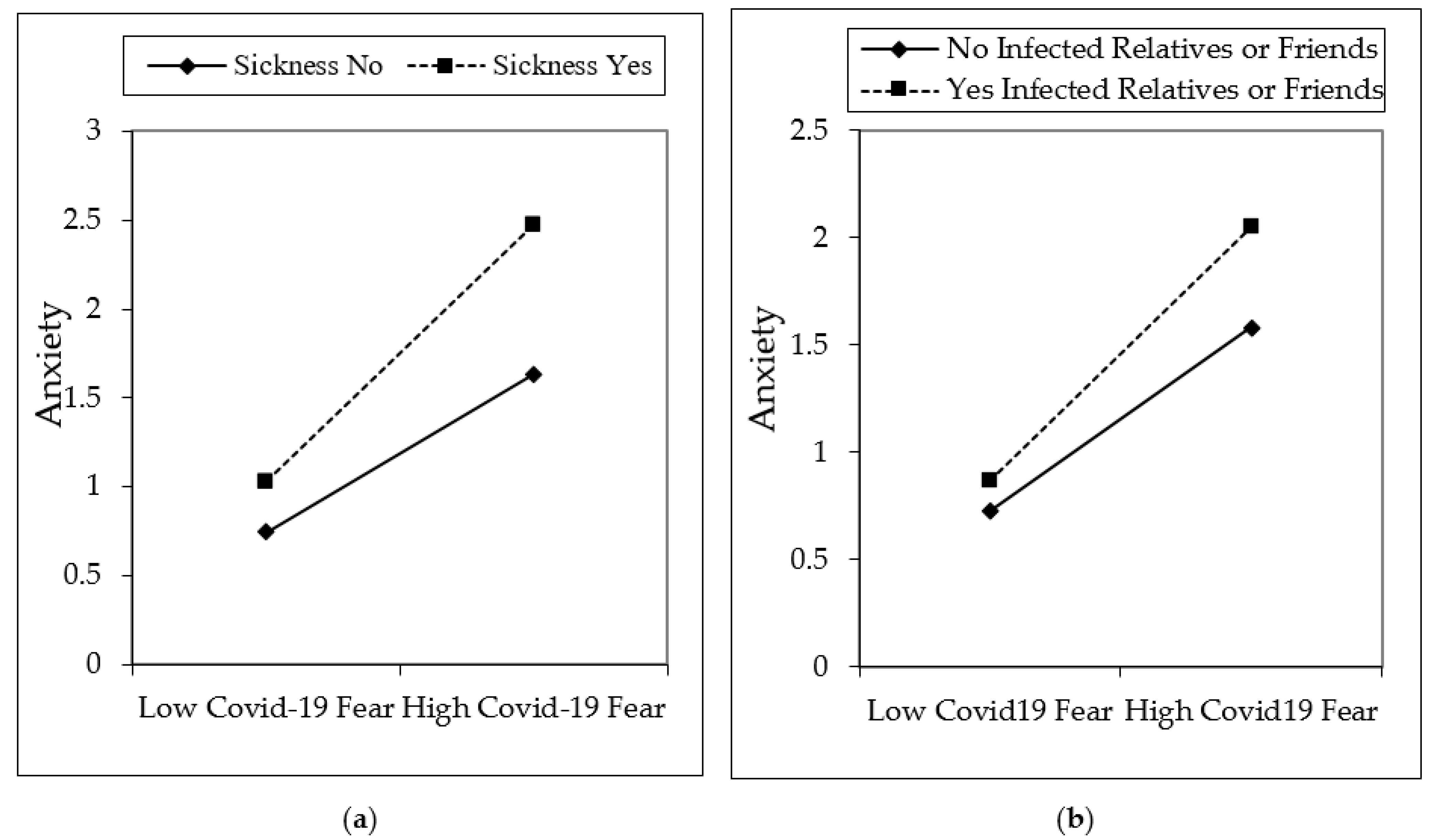
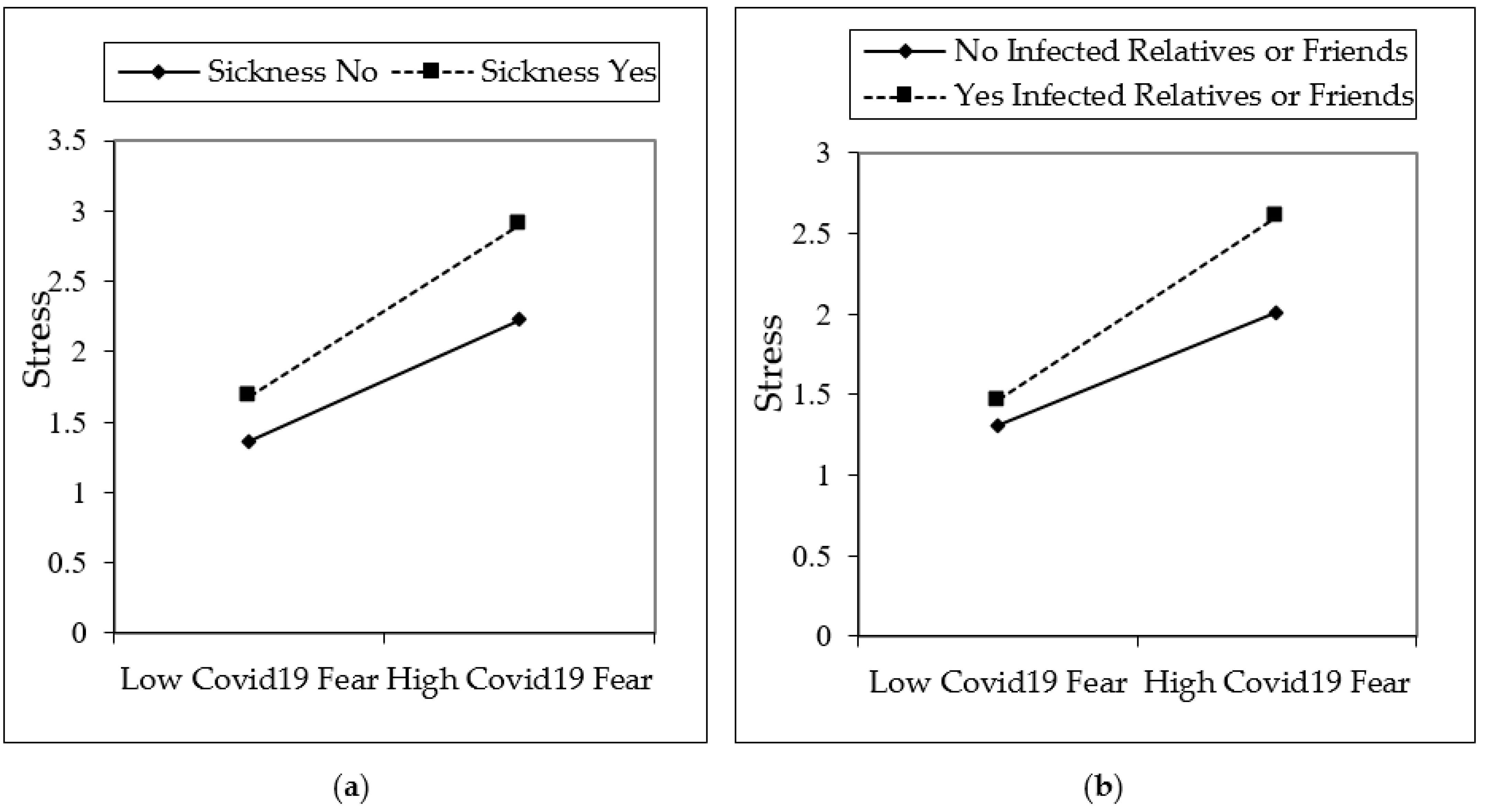
3.3. Hypothesis Testing
4. Discussion
5. Limitations and Suggestions for Future Studies
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bäuerle, A.; Teufel, M.; Musche, V.; Weismüller, B.; Kohler, H.; Hetkamp, M.; Dörrie, N.; Schweda, A.; Skoda, E.-M. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: A cross-sectional study in Germany. J. Public Health 2020, 42, 672–678. [Google Scholar] [CrossRef]
- John Hopkins. John Hopkins University of Medicine, Coronavirus Resource Center. 2020. Available online: https://coronavirus.jhu.edu/map.html (accessed on 20 December 2020).
- Lam, M.H.-B.; Wing, Y.-K.; Yu, M.W.-M.; Leung, C.-M.; Ma, R.C.W.; Kong, A.P.S.; So, W.Y.; Fong, S.Y.-Y.; Lam, S.-P. Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: Long-term follow-up. Arch. Intern. Med. 2009, 169, 2142–2147. [Google Scholar] [CrossRef]
- Petzold, M.B.; Bendau, A.; Plag, J.; Pyrkosch, L.; Maricic, L.; Betzler, F.; Rogoll, J.; Große, J.; Ströhle, A. Risk, resilience, psychological distress, and anxiety at the beginning of the COVID-19 pandemic in Germany. Brain Behav. 2020, e01745. [Google Scholar] [CrossRef]
- Sheridan, A.; Andersen, A.L.; Hansen, E.T.; Johannesen, N. Social distancing laws cause only small losses of economic activity during the COVID-19 pandemic in Scandinavia. Proc. Natl. Acad. Sci. USA 2020, 117, 20468–20473. [Google Scholar] [CrossRef]
- Phelps, C.; Sperry, L.L. Children and the COVID-19 pandemic. Psychol. Trauma Theory Res. Pr. Policy 2020, 12, S73–S75. [Google Scholar] [CrossRef] [PubMed]
- Işıklı, S. COVID-19 Salgını’nın Psikolojik Sonuçları ve Etkili Başa Çıkma Yöntemleri, Hacettepe Üniversitesi Psikoloji Bölümü. Published by Hacettepe University in 1 July 2020, Ankara. pp. 1–36. Available online: https://corona.hacettepe.edu.tr/wp-content/uploads/2020/06/Covid-19_psikolojik_sonuclari_basa_cikma_yontemleri.pdf (accessed on 19 December 2020).
- Roychowdhury, D. 2019 Novel Coronavirus Disease, Crisis, and Isolation. Front. Psychol. 2020, 11, 1958. [Google Scholar] [CrossRef]
- Czeisler, M.É.; Tynan, M.A.; Howard, M.E.; Honeycutt, S.; Fulmer, E.B.; Kidder, D.P.; Robbins, R.; Barger, L.K.; Facer-Childs, E.R.; Baldwin, G.; et al. Public Attitudes, Behaviors, and Beliefs Related to COVID-19, Stay-at-Home Orders, Nonessential Business Closures, and Public Health Guidance—United States, New York City, and Los Angeles, 5–12 May 2020. MMWR. Morb. Mortal. Wkly. Rep. 2020, 69, 751–758. [Google Scholar] [CrossRef] [PubMed]
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Bio Med. Atenei Parm. 2020, 91, 157–160. [Google Scholar] [CrossRef]
- Jebril, N. World Health Organization Declared a Pandemic Public Health Menace: A Systematic Review of the Coronavirus Disease 2019 “COVID-19”. Available online: https://www.psychosocial.com/article/PR290311/25748/ (accessed on 1 April 2020). [CrossRef]
- WHO. Available online: https://www.who.int/news-room/statements (accessed on 20 December 2020).
- T.R. Ministry of Health, Turkish Republic Ministry of Health. Available online: https://covid19.saglik.gov.tr/TR-66935/genel-koronavirus-tablosu.html (accessed on 20 December 2020).
- Flanagan, E.W.; Beyl, R.A.; Fearnbach, S.N.; Altazan, A.D.; Martin, C.K.; Redman, L.M. The impact of COVID-19 stay-at-home orders on health behaviors in adults. Obesity 2021, 29, 438–445. [Google Scholar] [CrossRef]
- Chee, M.J.; Koziel Ly, N.K.; Anisman, H.; Matheson, K. Piece of Cake: Coping with COVID 19. Nutrients 2020, 12, 3803. [Google Scholar] [CrossRef] [PubMed]
- Bozkurt, Y.; Zeybek, Z.; Aşkın, R. COVİD-19 Pandemisi: Psikolojik Etkileri ve Terapötik Müdahaleler, İstanbul Ticaret Üniversitesi Sosyal Bilimler Dergisi, 2020, Bahar (Covid19-Özel Ek), 304–318. Available online: https://dergipark.org.tr/en/pub/iticusbe/issue/55168/753233 (accessed on 20 December 2020).
- Reger, M.A.; Stanley, I.H.; Joiner, T.E. Suicide Mortality and Coronavirus Disease 2019—A Perfect Storm? JAMA Psychiatry 2020, 77, 1093–1094. [Google Scholar] [CrossRef]
- Okuhara, T.; Okada, H.; Kiuchi, T. Predictors of Staying at Home during the COVID-19 Pandemic and Social Lockdown based on Protection Motivation Theory: A Cross-Sectional Study in Japan. Healthcare 2020, 8, 475. [Google Scholar] [CrossRef] [PubMed]
- Dong, L.; Hu, S.; Gao, J. Discovering drugs to treat coronavirus disease 2019 (COVID-19). Drug Discov. Ther. 2020, 14, 58–60. [Google Scholar] [CrossRef]
- Van Bavel, J.J.; Baicker, K.; Boggio, P.S.; Capraro, V.; Cichocka, A.; Cikara, M.; Crockett, M.J.; Crum, A.J.; Douglas, K.M.; Druckman, J.N.; et al. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020, 4, 460–471. [Google Scholar] [CrossRef]
- Hatun, O.; Dicle, A.N.; Demirci, İ. Koronavirüs salgınının psikolojik yansımaları ve salgınla başa çıkma. J. Turk. Stud. 2020, 15, 531–554. [Google Scholar] [CrossRef]
- Hoşgör, H.; Ülker, Z.; Sağcan, H. Acil Sağlik Hizmetleri Çalişanlarinda Covid-19 Anksiyetesi Ve Mesleki Performans Ilişkisinin Tanimlayici Değişkenler Açisindan Incelenmesi. Mehmet Akif Ersoy Üniversitesi İktisadi İdari Bilimler Fakültesi Derg. 2020, 7, 865–886. [Google Scholar] [CrossRef]
- Guan, W.; Ni, Z.; Hu, Y.; Liang, W.; Ou, C.; He, J.; Liu, L.; Shan, H.; Lei, C.; Hui, D.S.C.; et al. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Melki, J.; Tamim, H.; Hadid, D.; Farhat, S.; Makki, M.; Ghandour, L.; Hitti, E. Media Exposure and Health Behavior during Pandemics: The Mediating Effect of Perceived Knowledge and Fear on Compliance with COVID-19 Prevention Measures. Health Commun. 2020. [Google Scholar] [CrossRef]
- Karakaş, M. Covid-19 salgınının çok boyutlu sosyolojisi ve yeni normal meselesi. Sosyol. Derg. 2020, 40, 541–573. [Google Scholar] [CrossRef]
- Madhava Chandran, K.; Valsan, T.; Naveena, K.; Krishnakumar, K. Analysis of the uncertainty among people due to the COVID-19 Pandemic. Int. J. Indian Psychol. 2020, 8, 1894–1901. [Google Scholar] [CrossRef]
- Bakioğlu, F.; Korkmaz, O.; Ercan, H. Fear of COVID-19 and Positivity: Mediating Role of Intolerance of Uncertainty, Depression, Anxiety, and Stress. Int. J. Ment. Health Addict. 2020, 28, 1–14. [Google Scholar]
- Daniel, R.; Kathleen Hall, J. Conspiracy theories as barriers to controlling the spread of COVID-19 in the U.S. Soc. Sci. Med. 2020, 263, 113356. [Google Scholar] [CrossRef]
- Muhammad, S.R. Dialogic Content Analysis of Misinformation about COVID-19 on Social Media in Pakistan. Linguist. Lit. Rev. 2020, 6, 131–143. [Google Scholar] [CrossRef]
- Nussbaumer-Streit, B.; Mayr, V.; Dobrescu, A.I.; Chapman, A.; Persad, E.; Klerings, I.; Wagner, G.; Siebert, U.; Ledinger, D.; Zachariah, C.; et al. Quarantine alone or in combination with other public health measures to control COVID-19: A rapid review. Cochrane Database Syst. Rev. 2020. [Google Scholar] [CrossRef]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 2020, 16, 57. [Google Scholar] [CrossRef]
- Burrell, A.; Selman, L.E. How do funeral practices impact bereaved relatives’ mental health, grief and bereavement? A mixed methods review with implications for COVID-19. Omega-J. Death Dying 2020. [Google Scholar] [CrossRef] [PubMed]
- Almandoz, J.P.; Xie, L.; Schellinger, J.N.; Mathew, M.S.; Gazda, C.; Ofori, A.; Kukreja, S.; Messiah, S.E. Impact of COVID-19 stay-at-home orders on weight-related behaviours among patients with obesity. Clin. Obes. 2020, 10, e12386. [Google Scholar] [CrossRef] [PubMed]
- Narzisi, A. Handle the Autism Spectrum Condition during Coronavirus (COVID-19) Stay at Home Period: Ten Tips for Helping Parents and Caregivers of Young Children. Brain Sci. 2020, 10, 207. [Google Scholar] [CrossRef]
- Griffith, A.K. Parental Burnout and Child Maltreatment During the COVID-19 Pandemic. J. Fam. Violence 2020. [Google Scholar] [CrossRef] [PubMed]
- Pietromonaco, P.R.; Overall, N.C. Applying relationship science to evaluate how the COVID-19 pandemic may impact couples’ relationships. Am. Psychol. 2020. [Google Scholar] [CrossRef]
- Campbell, A.M. An increasing risk of family violence during the Covid-19 pandemic: Strengthening community collaborations to save lives. Forensic Sci. Int. Rep. 2020, 2, 100089. [Google Scholar] [CrossRef]
- Zhang, H. The Influence of the Ongoing COVID-19 Pandemic on Family Violence in China. J. Fam. Violence 2020. [Google Scholar] [CrossRef] [PubMed]
- Usher, K.; Bhullar, N.; Durkin, J.; Gyamfi, N.; Jackson, D. Family violence and COVID-19: Increased vulnerability and reduced options for support. Int. J. Ment. Health Nurs. 2020, 29, 549–552. [Google Scholar] [CrossRef] [PubMed]
- Kofman, Y.B.; Garfin, D.R. Home is not always a haven: The domestic violence crisis amid the COVID-19 pandemic. Psychol. Trauma Theory Res. Pr. Policy 2020, 12, S199–S201. [Google Scholar] [CrossRef]
- Ciftci, A. Koronafobi Virüsten Daha Hızlı Yayılıyor. Available online: https://yesilay.org.tr/tr/makaleler/koronafobi-virusten-daha-hizli-yayiliyor (accessed on 21 December 2020).
- WHO. World Health Organization, COVID-19 Strategy Update. Available online: https://www.who.int/docs/default-source/coronaviruse/covid-strategy-update-14april2020.pdf?sfvrsn=29da3ba0_6 (accessed on 14 April 2020).
- Odriozola-González, P.; Planchuelo-Gómez, Á.; Irurtia-Muñiz, M.J.; de Luis-García, R. Psychological symptoms of the outbreak of the COVID-19 crisis and confinement in the population of Spain. J. Health Psychol. 2020. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef]
- Justo-Alonso, A.; García-Dantas, A.; González-Vázquez, A.I.; Sánchez-Martín, M.; Del Río-Casanova, L. How did Different Generations Cope with the COVID-19 Pandemic? Early Stages of the Pandemic in Spain. Psicothema 2020, 32, 490–500. [Google Scholar] [CrossRef]
- Wathelet, M.; Duhem, S.; Vaiva, G.; Baubet, T.; Habran, E.; Veerapa, E.; Debien, C.; Molenda, S.; Horn, M.; Grandgenèvre, P.; et al. Factors Associated With Mental Health Disorders Among University Students in France Confined During the COVID-19 Pandemic. JAMA Netw. Open 2020, 3, e2025591. [Google Scholar] [CrossRef]
- Guessoum, S.B.; Lachal, J.; Radjack, R.; Carretier, E.; Minassian, S.; Benoit, L.; Moro, M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020, 291, 113264. [Google Scholar] [CrossRef]
- Kimter, N. Covid-19 Günlerinde Bireylerin Psikolojik Sağlamlık Düzeylerinin Bazı Değişkenler Açısından İncelenmesi. IBAD Sos. Bilim. Derg. 2020, 574–605. [Google Scholar] [CrossRef]
- Liu, T.; Liang, W.; Zhong, H.; He, J.; Chen, Z.; He, G.; Song, T.; Chen, S.; Wang, P.; Li, J.; et al. Risk factors associated with COVID-19 infection: A retrospective cohort study based on contacts tracing. Emerg. Microbes Infect. 2020, 9, 1546–1553. [Google Scholar] [CrossRef]
- Van Der Velden, P.G.; Contino, C.; Das, M.; Van Loon, P.; Bosmans, M.W. Anxiety and depression symptoms, and lack of emotional support among the general population before and during the COVID-19 pandemic. A prospective national study on prevalence and risk factors. J. Affect. Disord. 2020, 277, 540–548. [Google Scholar] [CrossRef] [PubMed]
- Azzam, N.A.; Aljebreen, A.; Almuhareb, A.; Almadi, M.A. Disability and quality of life before and during the COVID-19 outbreak: A cross-sectional study in inflammatory bowel disease patients. Saudi J. Gastroenterol. 2020, 26, 256–262. [Google Scholar] [CrossRef]
- Kang, C.; Yang, S.; Yuan, J.; Xu, L.; Zhao, X.; Yang, J. Patients with chronic illness urgently need integrated physical and psychological care during the COVID-19 outbreak. Asian J. Psychiatry 2020, 51, 102081. [Google Scholar] [CrossRef]
- Lunn, P.D.; Timmons, S.; Belton, C.A.; Barjaková, M.; Julienne, H.; Lavin, C. Motivating social distancing during the COVID-19 pandemic: An online experiment. Soc. Sci. Med. 2020, 265, 113478. [Google Scholar] [CrossRef]
- Chhabra, S. Psychological Implications of COVID-19 Pandemic—A Wide Spectrum of Manifestations. J. Evol. Med. Dent. Sci. 2020, 9, 2386. [Google Scholar] [CrossRef]
- Mattioli, A.V.; Sciomer, S.; Cocchi, C.; Maffei, S.; Gallina, S. Quarantine during COVID-19 outbreak: Changes in diet and physical activity increase the risk of cardiovascular disease. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 1409–1417. [Google Scholar] [CrossRef] [PubMed]
- Elran-Barak, R.; Mozeikov, M. One Month into the Reinforcement of Social Distancing due to the COVID-19 Outbreak: Subjective Health, Health Behaviors, and Loneliness among People with Chronic Medical Conditions. Int. J. Environ. Res. Public Health 2020, 17, 5403. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.X.; Wang, Y.; Rauch, A.; Wei, F. Unprecedented disruption of lives and work: Health, distress and life satisfaction of working adults in China one month into the COVID-19 outbreak. Psychiatry Res. 2020, 288, 112958. [Google Scholar] [CrossRef] [PubMed]
- Dong, Z.; Ma, J.; Hao, Y.; Shen, X.; Liu, F.; Gao, Y.; Zhang, L. The social psychological impact of the COVID-19 pandemic on medical staff in China: A cross-sectional study. Eur. Psychiatry 2020, 63, E65. [Google Scholar] [CrossRef] [PubMed]
- Ma, T.; Heywood, A.; MacIntyre, C. Travel health seeking behaviours, masks, vaccines and outbreak awareness of Australian Chinese travellers visiting friends and relatives—Implications for control of COVID-19. Infect. Dis. Health 2021, 26, 38–47. [Google Scholar] [CrossRef]
- Zhang, H.; Chen, R.; Chen, J.; Chen, B. COVID-19 Transmission Within a Family Cluster in Yancheng, China. Front. Med. 2020, 7, 387. [Google Scholar] [CrossRef] [PubMed]
- Rajmil, L. Role of children in the transmission of the COVID-19 pandemic: A rapid scoping review. BMJ Paediatr. Open 2020, 4, e000722. [Google Scholar] [CrossRef]
- Abdelrahman, M. Personality Traits, Risk Perception, and Protective Behaviors of Arab Residents of Qatar During the COVID-19 Pandemic. Int. J. Ment. Health Addict. 2020. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F.; Rockwood, N.J. Conditional Process Analysis: Concepts, Computation, and Advances in the Modeling of the Contingencies of Mechanisms. Am. Behav. Sci. 2020, 64, 19–54. [Google Scholar] [CrossRef]
- Dawson, J.F. Moderation in management research: What, why, when and how. J. Bus. Psych. 2020, 29, 1–19. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.-Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID19 Scale: Development and initial validation. Int. J. Ment. Health Addict. 2020. [Google Scholar] [CrossRef]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Henry, J.D.; Crawford, J.R. The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2005, 44, 227–239. [Google Scholar] [CrossRef] [PubMed]
- Yılmaz, Ö.; Boz, H.; Arslan, A. Depresyon Anksiyete Stres Ölçeğinin (DASS 21) Türkçe Kısa Formunun Geçerlilik-Güvenilirlik Çalışması. Finans Ekon. Sos. Araştırmalar Derg. (FESA) 2017, 2, 92–104. [Google Scholar]
- Roy, D.; Tripathy, S.; Kar, S.K.; Sharma, N.; Verma, S.K.; Kaushal, V. Study of knowledge, attitude, anxiety and perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J. Psychiatry 2020, 51, 102083. [Google Scholar] [CrossRef]
- Shigemura, J.; Ursano, R.J.; Morganstein, J.C.; Kurosawa, M.; Benedek, D.M. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin. Neurosci. 2020, 74, 281–282. [Google Scholar] [CrossRef] [PubMed]
- Tee, M.L.; Tee, C.A.; Anlacan, J.P.; Aligam, K.J.G.; Reyes, P.W.C.; Kuruchittham, V.; Ho, R.C. Psychological impact of COVID-19 pandemic in the Philippines. J. Affect. Disord. 2020, 277, 379–391. [Google Scholar] [CrossRef] [PubMed]
- Khan, K.S.; Mamun, M.A.; Griffiths, M.D.; Ullah, I. The Mental Health Impact of the COVID-19 Pandemic Across Different Cohorts. Int. J. Ment. Health Addict. 2020. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, K. Patterns of Social Reactions to COVID-19 Pandemic; Reasons & Proposed Ways to Overcome. Adv. J. Soc. Sci. 2020, 7, 54–59. [Google Scholar] [CrossRef]


| f | % | M | SD | ||
|---|---|---|---|---|---|
| Gender | 1.57 | 0.50 | |||
| Female | 1863 | 56.7 | |||
| Male | 1424 | 43.3 | |||
| Age | 31.78 | 13.77 | |||
| 16–25 | 1667 | 50.7 | |||
| 25–40 | 737 | 22.4 | |||
| 40–65 | 837 | 25.5 | |||
| 65–96 | 46 | 1.4 | |||
| Marital Status | 1.39 | 0.49 | |||
| Single | 1993 | 60.6 | |||
| Married | 1294 | 39.4 | |||
| Education Level | 4.95 | 0.78 | |||
| No Graduation | 7 | 0.2 | |||
| Elementary | 74 | 2.3 | |||
| Middle School | 70 | 2.1 | |||
| High School | 374 | 11.4 | |||
| University | 2178 | 66.3 | |||
| Masters or PhD | 584 | 17.8 | |||
| Underlying Illness | 0.30 | 0.46 | |||
| I Have an Underlying Illness | 2288 | 69.6 | |||
| I Have no Underlying Illness | 999 | 30.4 | |||
| Infected Relatives or Friends | 0.62 | 0.48 | |||
| No | 1240 | 37.7 | |||
| Yes | 2047 | 62.3 | |||
| Total | 3287 | 100% | |||
| No | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Gender (1 = m. 2 = f.) | ||||||||||
| 2 | Age | −0.442 ** | |||||||||
| 3 | Marital St. 1–2 = No–Yes | −0.408 ** | 0.752 ** | ||||||||
| 4 | Education | −0.095 ** | −0.015 | −0.029 | |||||||
| 5 | COVID-19 Fear | 0.236 ** | −0.183 ** | −0.158 ** | −0.053 ** | (0.87) | |||||
| 6 | Underlying Illness, 0–1 = No–Yes | −0.02 | 0.233 ** | 0.134 ** | −0.087 ** | 0.068 ** | |||||
| 7 | Infected Relatives or Friends, 0–1 = No–Yes | −0.023 | −0.001 | 0.053 ** | 0.024 | 0.021 | 0.080 ** | ||||
| 8 | Stress | 0.242 ** | −0.309 ** | −0.286 ** | −0.054 ** | 0.365 ** | 0.116 ** | 0.049 ** | (0.89) | ||
| 9 | Anxiety | 0.187 ** | −0.203 ** | −0.190 ** | −0.067 ** | 0.514 ** | 0.161 ** | 0.079 ** | 0.564 ** | (.85) | |
| 10 | Depression | 0.177 ** | −0.31 ** | −0.296 ** | −0.027 | 0.35 ** | 0.08 ** | 0.03 | 0.73** | 0.56 ** | (0.91) |
| Mean | 1.57 | 31.78 | 1.39 | 4.95 | 2.48 | 0.30 | 0.62 | 0.72 | 0.32 | 0.55 | |
| Sd. | 0.49 | 13.77 | 0.49 | 0.78 | 0.83 | 0.46 | 0.48 | 0.70 | 0.47 | 0.69 |
| Variable | Model 1 | Model 2 | Model 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE | p | B | SE | p | B | SE | p | |
| Constant | 1.20 | 0.10 | <0.001 | −0.57 | 0.10 | <0.001 | 0.92 | 0.13 | <0.001 |
| Gender | 0.05 | 0.03 | 0.07 | −0.05 | 0.03 | 0.07 | −0.04 | 0.03 | 0.08 |
| Age | −0.01 | 0.00 | <0.001 | −0.01 | 0.00 | <0.001 | −0.01 | 0.00 | <0.001 |
| Marital Status, 1 = single 2 = married | −0.20 | 0.04 | <0.001 | −0.18 | 0.03 | <0.001 | −0.19 | 0.03 | <0.001 |
| Education | −0.03 | 0.02 | 0.06 | −0.01 | 0.01 | 0.47 | −0.01 | 0.01 | 0.51 |
| COVID-19 Fear | 0.25 | 0.01 | <0.001 | 0.10 | 0.04 | 0.01 | |||
| Underlying Illness (0 = No 1 = Yes) | 0.19 | 0.03 | <0.001 | 0.18 | 0.02 | <0.001 | |||
| Infected Relatives or | 0.03 | 0.02 | 0.21 | 0.03 | 0.02 | 0.26 | |||
| Friends (0 = No 1 = Yes) | |||||||||
| COVID-19 Fear × Infected Rel. or Fr. | 0.05 | 0.02 | 0.00 | ||||||
| COVID-19 Fear × Underlying Illness | 0.09 | 0.02 | <0.001 | ||||||
| F | 98.14 | 124.34 | 100.96 | ||||||
| p | <0.001 | <0.001 | <0.001 | ||||||
| R2 | 0.11 | 0.21 | 0.22 | ||||||
| R2 Change | |||||||||
| Variables | Model 1 | Model 2 | Model 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE | p | B | SE | p | B | SE | p | |
| Constant | 0.55 | 0.07 | <0.001 | −0.14 | 0.07 | 0.03 | 0.20 | 0.08 | 0.02 |
| Gender | 0.10 | 0.02 | <0.001 | 0.01 | 0.02 | 0.72 | 0.01 | 0.02 | 0.63 |
| Age | 0.00 | 0.00 | <0.001 | 0.00 | 0.00 | <0.001 | 0.00 | 0.00 | <0.001 |
| Marital Status, 1 = single 2 = married | −0.07 | 0.03 | 0.01 | −0.05 | 0.02 | 0.01 | −0.06 | 0.02 | 0.01 |
| Education | −0.04 | 0.01 | <0.001 | −0.02 | 0.01 | 0.03 | −0.02 | 0.01 | 0.03 |
| COVID-19 Fear | 0.27 | 0.01 | <0.001 | 0.13 | 0.02 | <0.001 | |||
| Underlying Illness (0 = No 1 = Yes) | 0.16 | 0.02 | <0.001 | 0.15 | 0.02 | <0.001 | |||
| Have Infected Relatives or Friends (0 = No 1 = Yes) | 0.06 | 0.01 | <0.001 | 0.06 | 0.01 | <0.001 | |||
| COVID-19 Fear × Infected Rel. or Fr. | 0.05 | 0.01 | <0.001 | ||||||
| COVID-19 Fear × Underlying Illness | 0.10 | 0.02 | <0.001 | ||||||
| F | 50.87 | 207.56 | 174.94 | ||||||
| p | <0.001 | <0.001 | <0.001 | ||||||
| R2 | 0.06 | 0.31 | 0.33 | ||||||
| R2 Change | 0.25 | 0.02 | |||||||
| Variable | Model 1 | Model 2 | Model 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE | p | B | SE | p | B | SE | p | |
| Constant | 1.19 | 0.11 | <0.001 | 0.54 | 0.10 | <0.001 | 0.89 | 0.13 | <0.001 |
| Gender | 0.16 | 0.03 | <0.001 | 0.07 | 0.03 | 0.01 | 0.07 | 0.03 | <0.001 |
| Age | −0.01 | 0.00 | <0.001 | −0.01 | 0.00 | <0.001 | −0.01 | 0.00 | <0.001 |
| Marital Status, 1 = single 2 = married | −0.15 | 0.04 | <0.001 | −0.13 | 0.03 | <0.001 | −0.13 | 0.03 | <0.001 |
| Education | −0.04 | 0.02 | 0.00 | −0.03 | 0.01 | 0.08 | −0.02 | 0.01 | 0.09 |
| COVID-19 Fear | 0.24 | 0.01 | <0.001 | 0.10 | 0.04 | 0.01 | |||
| Underlying Illness (0 = No 1 = Yes) | 0.23 | 0.02 | <0.001 | 0.22 | 0.02 | <0.001 | |||
| Have Infected Relatives or Friends (0 = No 1 = Yes) | 0.05 | 0.02 | 0.02 | 0.05 | 0.02 | 0.02 | |||
| COVID-19 Fear × Infected Rel. or Fr. | 0.06 | 0.02 | <0.001 | ||||||
| COVID-19 Fear × Underlying Illness | 0.06 | 0.02 | 0.01 | ||||||
| F | 107.71 | 137.41 | 110.26 | ||||||
| p | <0.001 | <0.001 | <0.001 | ||||||
| R2 | 0.12 | 0.23 | 0.23 | ||||||
| R2 Change | 0.11 | 0.01 | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koçak, O.; Koçak, Ö.E.; Younis, M.Z. The Psychological Consequences of COVID-19 Fear and the Moderator Effects of Individuals’ Underlying Illness and Witnessing Infected Friends and Family. Int. J. Environ. Res. Public Health 2021, 18, 1836. https://doi.org/10.3390/ijerph18041836
Koçak O, Koçak ÖE, Younis MZ. The Psychological Consequences of COVID-19 Fear and the Moderator Effects of Individuals’ Underlying Illness and Witnessing Infected Friends and Family. International Journal of Environmental Research and Public Health. 2021; 18(4):1836. https://doi.org/10.3390/ijerph18041836
Chicago/Turabian StyleKoçak, Orhan, Ömer Erdem Koçak, and Mustafa Z. Younis. 2021. "The Psychological Consequences of COVID-19 Fear and the Moderator Effects of Individuals’ Underlying Illness and Witnessing Infected Friends and Family" International Journal of Environmental Research and Public Health 18, no. 4: 1836. https://doi.org/10.3390/ijerph18041836
APA StyleKoçak, O., Koçak, Ö. E., & Younis, M. Z. (2021). The Psychological Consequences of COVID-19 Fear and the Moderator Effects of Individuals’ Underlying Illness and Witnessing Infected Friends and Family. International Journal of Environmental Research and Public Health, 18(4), 1836. https://doi.org/10.3390/ijerph18041836








