Impact of Lifestyle Intervention Programs for Children and Adolescents with Overweight or Obesity on Body Weight and Selected Cardiometabolic Factors—A Systematic Review
Abstract
:1. Introduction
| Country, Year [Reference] | Age (Years) | n | Criteria for Measuring Body Weight | Frequency of Dyslipidemia (%) | Study Design | Odds Ratio for Dyslipidemia | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Dyslipidemia | High TG | High TC | High LDL-C | Low HDL-C | |||||||
| Argentina, 2014 [18] | 8–14 | 139 | overweight and obesity | BMI z-score for overweight: 1–2; BMI z-score for obesity > 2 | 50.4 | 31.9 | 11.9 | 10.7 | 29.7 | nd | nd |
| Brazil, 2012 [19] | 6–10 | 147 | overweight and obesity | BMI ≥ 85th pc | 28.0 | 10.2 | 11.6 | 8.8 | 8.8 | cross-sectional study | nd |
| Brazil, 2012 [20] | 7–14 | 698 | normal | BMI ≥ 3rd and < 85th pc | 24.0 | nd | nd | nd | nd | cross-sectional study | 1.0 (ref.) |
| 116 | overweight and obesity | BMI ≥ 85th pc | 26.4 | nd | nd | nd | nd | 3.4 (p < 0.001) | |||
| Brazil, 2009 [21] | 2–19 | 383 | no excess weight | BMI < 85th pc | nd | 4.7 | 47.8 | 36.8 | 6.0 | cross-sectional study | nd |
| 48 | overweight | BMI ≥ 85th and < 95th pc | nd | 14.6 | 45.8 | 50.0 | 4.2 | ||||
| 63 | obesity | BMI ≥ 95th pc | nd | 27.0 | 74.6 | 55.6 | 7.9 | ||||
| China, 2016 [22] | 6–18 | 1649 | normal | BMI criteria according to WGOC | nd | 11.4 | 10.9 | 4.8 | 3.1 | cross-sectional study | nd |
| overweight | nd | 18.5 | 10.0 | 6.2 | 12.3 | ||||||
| obesity | nd | 37.2 | 12.1 | 9.9 | 13.9 | ||||||
| Denmark, 2017 [12] | 6–19 | 1639 | normal | BMI: 10th—90th pc | 5.2 | 0.8 | 2.8 | 2.0 | 1.3 | population-based cohort study | nd |
| 1421 | overweight and obesity | BMI > 90th pc | 28.0 | 14.8 | 7.1 | 6.8 | 12.7 | ||||
| India, 2017 [23] | 5–18 | 65 | obesity | BMI ≥ 95th pc | 63.0 | 46.2 | 40.0 | 60.0 | 40.0 | cross-sectional study | nd |
| Iran, 2015 [14] | 7–12 | 100 | control | BMI < 85th pc and WC < 90th pc | nd | 13.0 | 13.0 | 5.0 | 11.0 | case control study | nd |
| 100 | overweight | BMI: 85th -95th pc and WC < 90th pc | nd | 20.0 | 8.0 | 8.0 | 13.0 | ||||
| 100 | general obesity with central obesity | BMI ≥ 95th pc and WC ≥ 90th pc | nd | 49.0 | 28.0 | 24.0 | 38.0 | ||||
| Iran, 2015 [24] | 11–18 | 2231 | normal | nd | nd | 14.7 | 6.2 | 3.6 | 25.5 | cross-sectional study | nd |
| 412 | overweight and obesity | nd | 10.5 | 5.3 | 2.9 | 20.1 | |||||
| Iran, 2011 [25] | 6–18 | 2064 | overweight and obesity | BMI ≥ 85th pc | 69.9 | 49.9 | 32.4 | 23.0 | 24.4 | retrospective study | nd |
| Iran, 2009 [26] | 4–18 | 50 | normal | BMI: 50th–85th pc | nd | nd | nd | nd | nd | case control study | nd |
| 72 | overweight | BMI z-score: 1–2 | 26.2 | nd | nd | nd | nd | ||||
| 41 | moderately obesity | BMI z-score: 2–2.5 | 16.9 | nd | nd | nd | nd | ||||
| 117 | severely obesity | BMI z-score > 2.5 | 56.8 | nd | nd | nd | nd | ||||
| Mexico, 2016 [10] | 11–16 | 193 | normal | BMI criteria according to IOTF | 42.0 | nd | nd | nd | nd | population-based cross-sectional nutritional survey | 1.0 (ref.) |
| 58 | overweight | 60.0 | nd | nd | nd | nd | 2.07 (p < 0.05) | ||||
| 42 | obesity | 62.0 | nd | nd | nd | nd | 2.21 (p < 0.05) | ||||
| Mexico, 2015 [11] | 2–10 | 241 | normal | BMI criteria according to IOTF | 49.4 | 32.8 | 14.9 | 12.0 | 19.5 | population-based cross-sectional nutritional survey | 1.0 (ref.) |
| 47 | overweight | 63.8 | 48.9 | 19.1 | 8.5 | 36.2 | 1.76 | ||||
| 49 | obesity | 73.5 | 59.2 | 18.4 | 16.3 | 55.1 | 2.79 | ||||
| Pakistan, 2019 [27] | 10–16 | 58 | overweight | BMI ≥ 85th and < 95th pc | 29.3 | 20.7 | 0.0 | 0.0 | 15.5 | cross-sectional study | nd |
| 41 | obesity | BMI ≥ 95th pc | 61.0 | 46.3 | 4.9 | 2.4 | 43.9 | ||||
| Poland, 2011 [13] | 16–18 | 69 | overweight | BMI criteria according to IOTF | nd | 36.2 | nd | nd | 21.7 | nd | nd |
| 19 | obesity | nd | 63.2 | nd | nd | 26.3 | |||||
| Poland, 2010 [28] | <10 | 91 | obesity | BMI > 97th pc | 25.0 | 14.1 | 17.2 | 48.8 | 22.0 | nd | nd |
| Turkey, 2015 [29] | 2–19 | 823 | obesity | BMI ≥ 95th pc | 42.9 | 21.7 | 18.6 | 13.4 | 19.7 | retrospective study | nd |
| United Arab Emirates, 2018 [30] | 4–19 | 216 | overweight and obesity | BMI ≥ 85th pc | 55.3 | 28.6 | 11.7 | 32.7 | 18.0 | cross-sectional study | nd |
| United States, 2015 [31] | 6–19 | 19,151 | normal | BMI ≥ 5th and < 85th pc | 13.8 | nd | 6.3 | nd | 6.8 | cross-sectional study | nd |
| overweight | BMI ≥ 85th and < 95th pc | 22.3 | nd | 6.9 | nd | 14.8 | |||||
| obesity | BMI ≥ 95th pc | 43.3 | nd | 11.6 | nd | 33.2 | |||||
| United States, 2010 [32] | 12–19 | 2008 | normal | BMI > 5th and < 85th pc | 14.2 | 5.9 | nd | 5.8 | 4.3 | cross-sectional study | 1.0 (ref.) |
| 514 | overweight | BMI ≥ 85th and < 95th pc | 22.3 | 13.8 | nd | 8.4 | 8.3 | 1.6 | |||
| 603 | obesity | BMI ≥ 95th pc | 42.9 | 24.1 | nd | 14.2 | 20.5 | 3.0 | |||
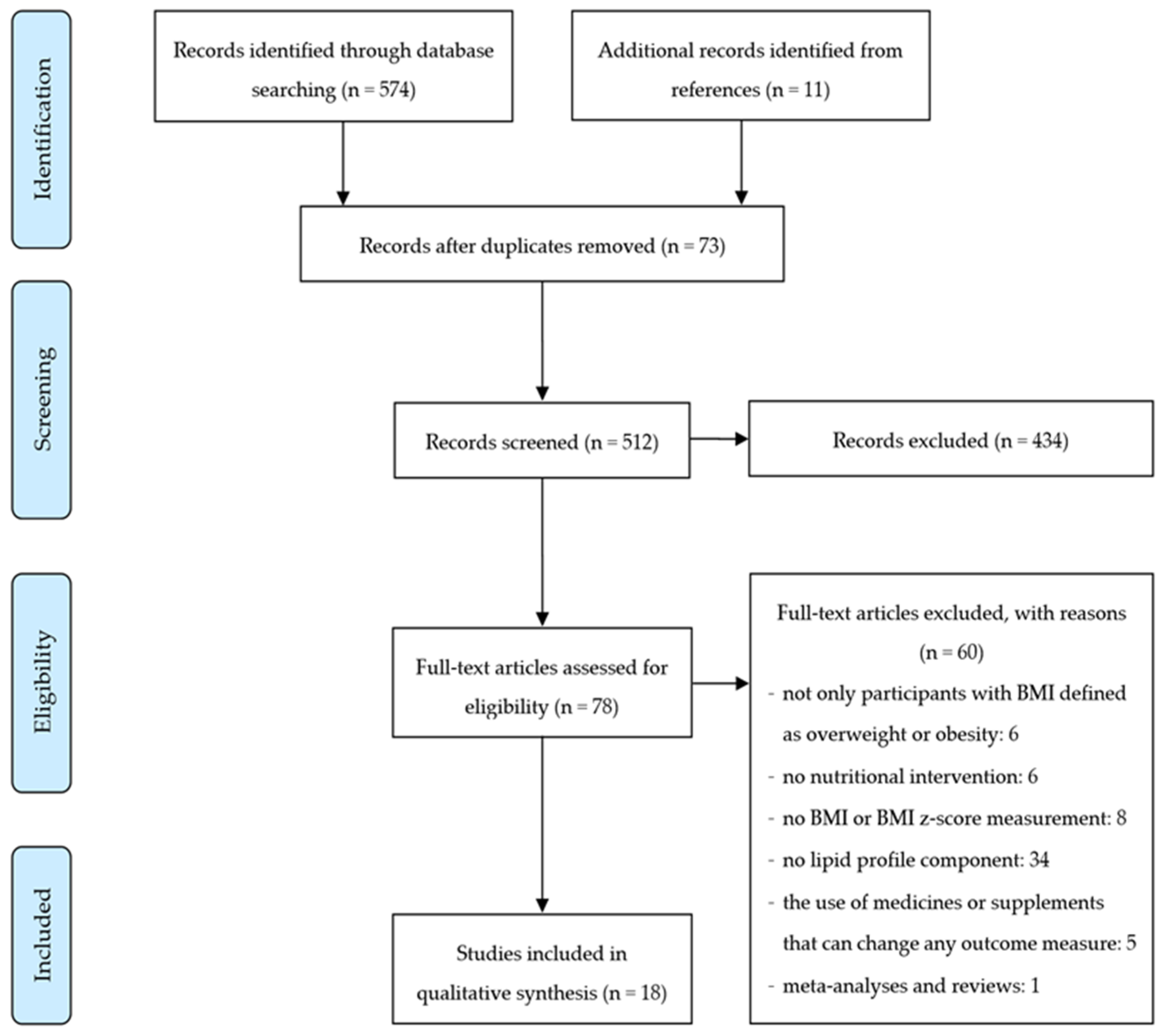
1.1. Search Strategy
1.2. Eligibility Criteria
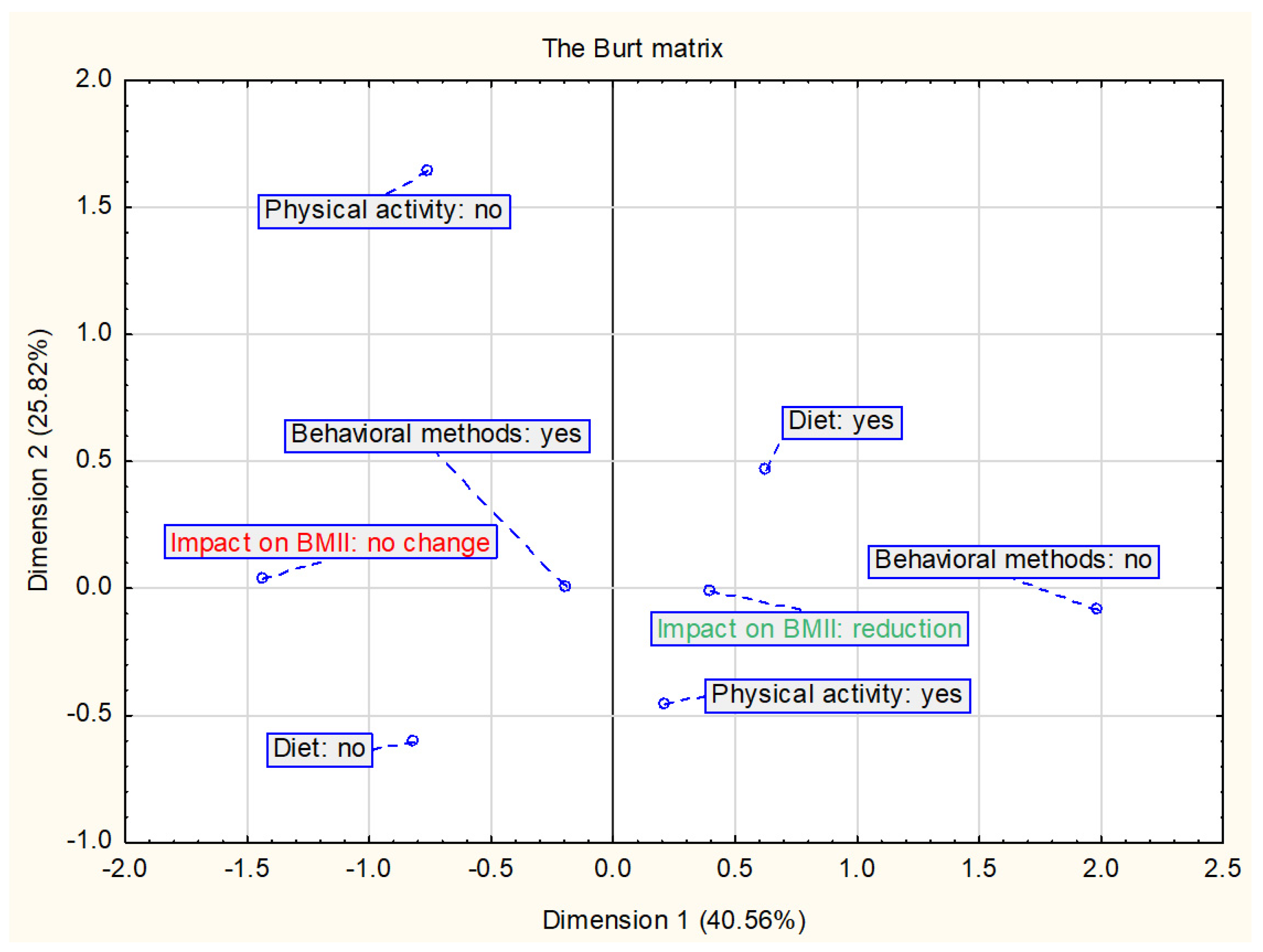
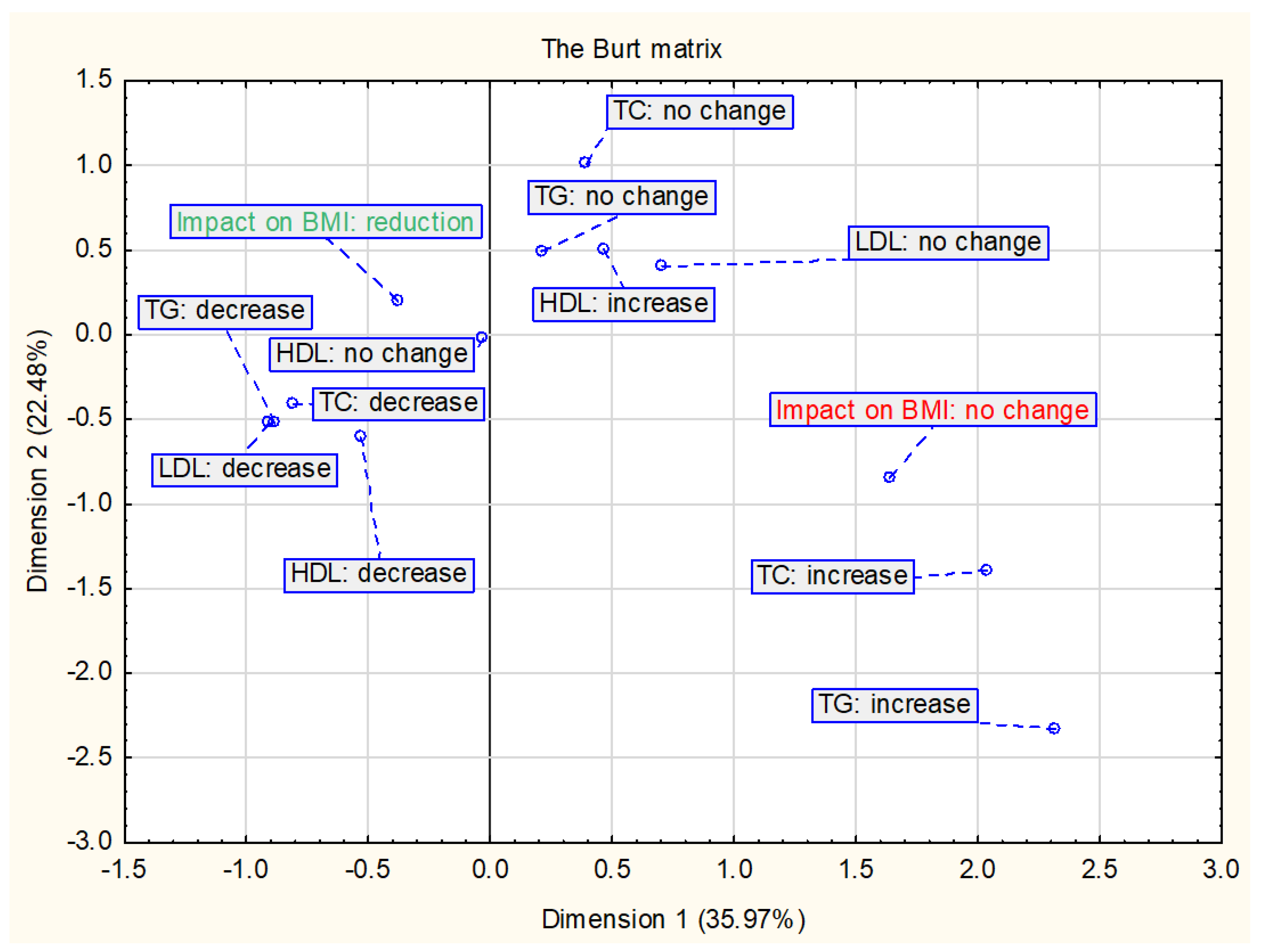
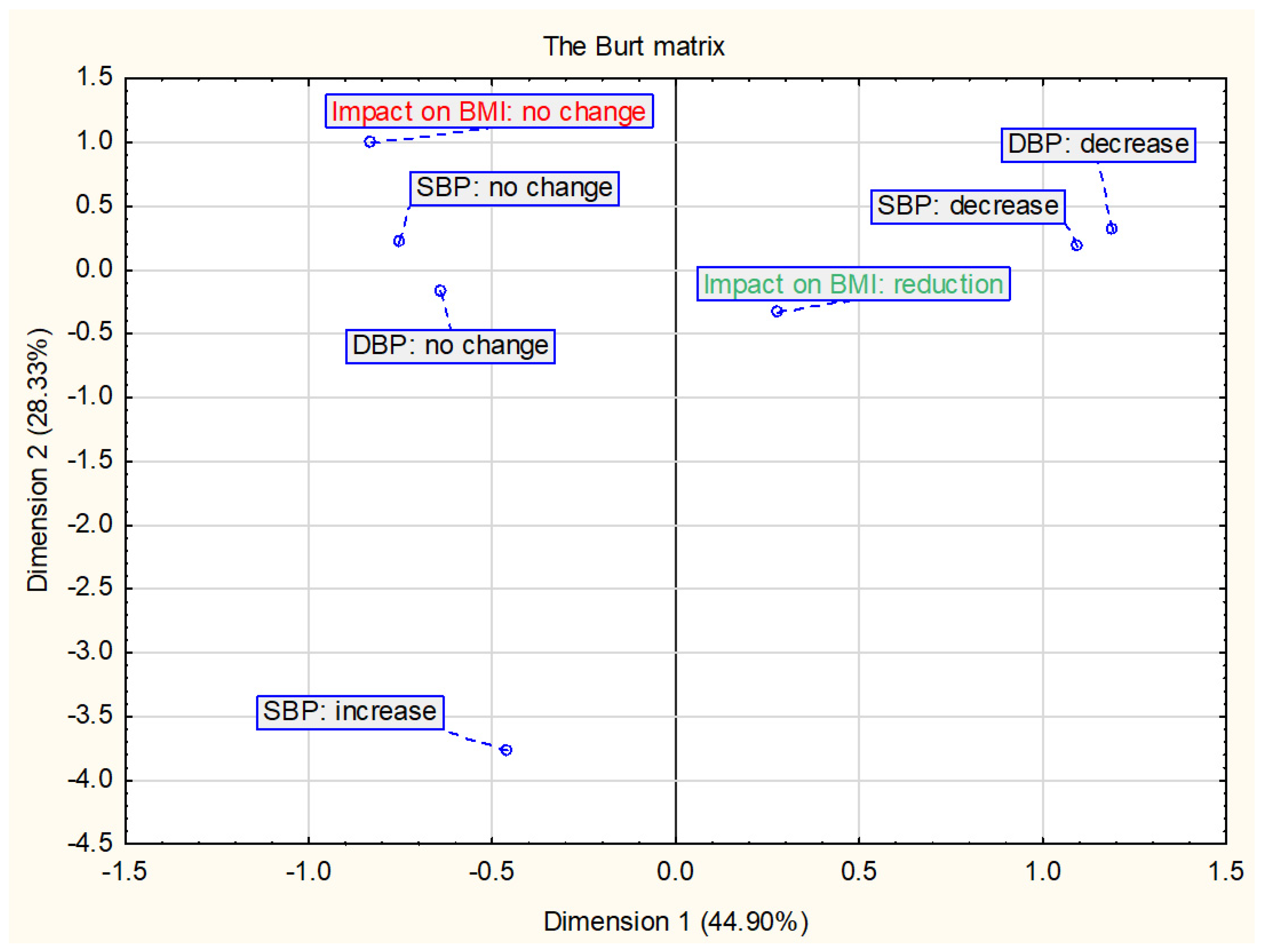
1.3. Statistical Analysis
2. Results
2.1. Studies Characteristic
2.2. Nutritional and Physical Activity Interventions
2.2.1. Nutritional Interventions
2.2.2. Physical Activity Interventions
2.2.3. The Impact of Nutritional and Physical Activity Interventions on the BMI and/or BMI z-Score
2.2.4. The Impact of Nutritional and Physical Activity Interventions on Selected Cardiometabolic Parameters
2.2.5. The Impact of Changes in BMI and/or BMI z-score on Selected Cardiometabolic Parameters
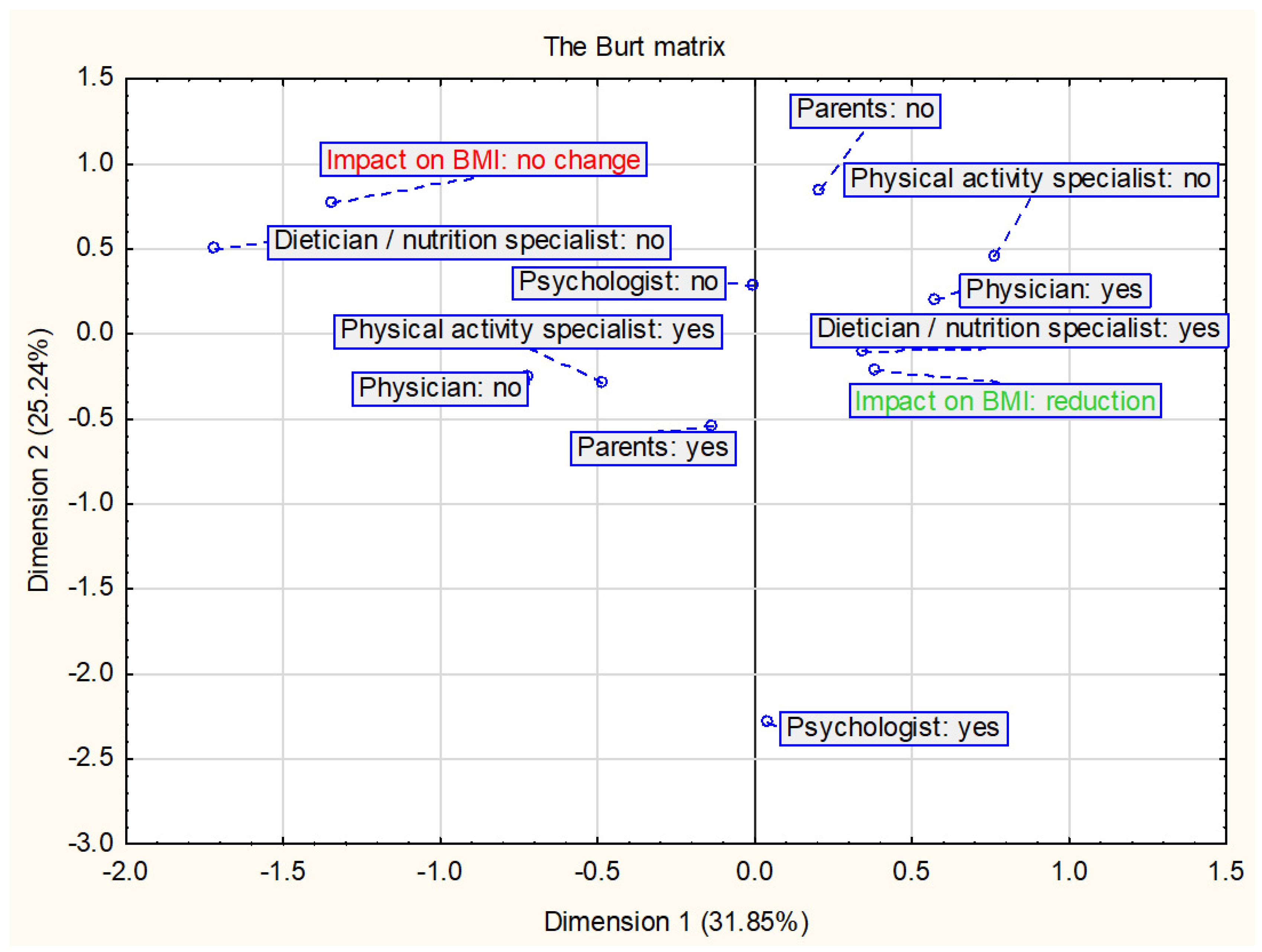
2.3. Parental and Therapeutic tEam Involvement
2.3.1. Parental Involvement
2.3.2. Therapeutic Team Involvement
2.3.3. The Impact of Parental and Therapeutic Team Involvement on the BMI and/or BMI z-Score
2.3.4. The Impact of Parental and Therapeutic Team Involvement on Selected Cardiometabolic Parameters
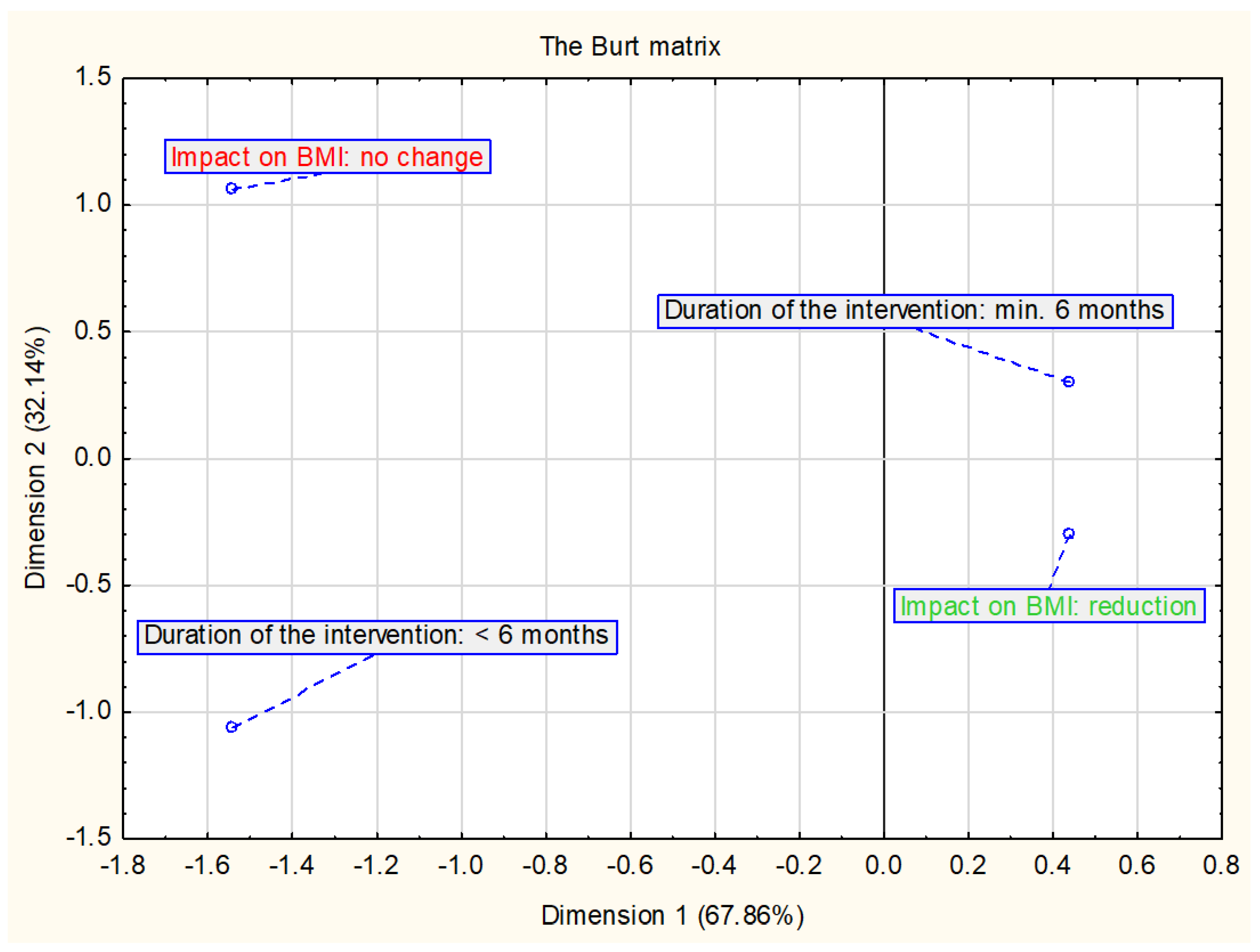
2.4. Duration of the Intervention
The Impact of Duration of the Intervention on the BMI and/or BMI z-Score and Selected Cardiometabolic Parameters
3. Discussion
Strengths and Limitations
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organisation (WHO). Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consultation; World Health Organisation Technical Report Series 894; World Health Organisation: Geneva, Switzerland, 2000; pp. 1–253. [Google Scholar]
- World Health Organisation (WHO). Obesity and Overweight—Key Facts. Available online: https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 1 March 2020).
- OECD. Health at a Glance 2017. Available online: http://dx.doi.org/10.1787/health_glance-2017-en (accessed on 1 March 2020).
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128,9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [Green Version]
- Klatsky, A.L.; Zhang, J.; Udaltsova, N.; Li, Y.; Tran, H.N. Body mass index and mortality in a very large cohort: Is it really healthier to be overweight? Perm J. 2017, 21, 16–142. [Google Scholar] [CrossRef] [Green Version]
- Sahoo, K.; Sahoo, B.; Choudhury, A.K.; Sofi, N.Y.; Kumar, R.; Bhadoria, A.S. Childhood obesity: Causes and consequences. J. Fam. Med. Prim. Care 2015, 4, 187–192. [Google Scholar]
- Inchley, J.; Currie, D.; Jewell, J.; Breda, J.; Barnekow, V. Adolescent Obesity and Related Behaviours: Trends and Inequalities in the WHO European Region, 2002–2014: Observations from the Health Behaviour in School-Aged Children (HBSC) WHO Collaborative Cross-National Study; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2017. [Google Scholar]
- Zarzycka, D.; Szara, M.; Sroka, A. School age obesity—Epidemiology, health effects, methods of prevention. Pediatr. Endocrinol. 2015, 14.2.51, 79–88. [Google Scholar] [CrossRef]
- Peterson, A.L.; McBride, P.E. A review of guidelines for dyslipidemia in children and adolescents. WMJ 2012, 11, 274–282. [Google Scholar]
- Bibiloni, M.D.M.; Salas, R.; De la Garza, Y.E.; Villarreal, J.Z.; Sureda, A.; Tur, J.A. Serum lipid profile, prevalence of dyslipidaemia, and associated risk factors among northern Mexican adolescents. JPGN 2016, 63, 544–549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bibiloni, M.D.M.; Salas, R.; Novelo, H.I.; Villarreal, J.Z.; Sureda, A.; Tur, J.A. Serum lipid levels and dyslipidaemia prevalence among 2–10 year-old Northern Mexican children. PLoS ONE 2015, 10, e0119877. [Google Scholar] [CrossRef] [Green Version]
- Nielsen, T.R.H.; Lausten-Thomsen, U.; Fonvig, C.E.; Bøjsøe, C.; Pedersen, L.; Bratholm, P.S.; Hansen, T.; Pedersen, O.; Holm, J.C. Dyslipidemia and reference values for fasting plasma lipid concentrations in Danish/North-European white children and adolescents. BMC Pediatrics 2017, 17, 116. [Google Scholar] [CrossRef] [PubMed]
- Mikołajczak, J.; Piotrowska, E.; Biernat, J.; Wyka, J.; Żechałko-Czajkowska, A. Assessment of risk factors of metabolic syndrome in girls and boys from south-west area of Poland. Ann. Natl. Inst. Hyg. 2011, 62, 83–92. [Google Scholar]
- Bijari, B.; Taheri, F.; Chahkandi, T.; Kazemi, T.; Namakin, K.; Zardast, M. The relationship between serum lipids and obesity among elementary school in Birjand: A case control study. JRHS 2015, 15, 83–87. [Google Scholar] [PubMed]
- Freedman, D.S.; Dietz, W.H.; Srinivasan, S.R.; Berenson, G.S. The relation of overweight to cardiovascular risk factors among children and adolescents: The Bogalusa Heart Study. Pediatrics 1999, 103, 1175–1182. [Google Scholar] [CrossRef]
- Alleyne, G.; Chan Hon Yee, C.; Clark, H.; Gluckman, P.; Gore, A.; King, B.; Oye Lithur, N.; Nabarro, D.; Nishtar, S.; Radcliffe, P.; et al. Report of the Commission on Ending Childhood Obesity; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Bohn, B.; Wiegand, S.; Kiess, W.; Reinehr, T.; Stachow, R.; Oepen, J.; Langhof, H.; Hermann, T.; Widhalm, K.; Wabitsch, M.; et al. Changing characteristics of obese children and adolescents entering pediatric lifestyle intervention programs in Germany over the last 11 years: An adiposity patients registry multicenter analysis of 65,453 children and adolescents. Obes. Facts 2017, 10, 517–530. [Google Scholar] [CrossRef] [Green Version]
- Casavalle, P.L.; Lifshitz, F.; Romano, L.S.; Pandolfo, M.; Caamaño, A.; Boyer, P.M.; Rodríguez, P.N.; Friedman, S.M. Prevalence of dyslipidemia and metabolic syndrome risk factor in overweight and obese children. Pediatr. Endocrinol. Rev. 2014, 12, 213–223. [Google Scholar]
- Rinaldi, A.E.; de Oliveira, E.P.; Moreto, F.; Gabriel, G.F.; Corrente, J.E.; Burini, R.C. Dietary intake and blood lipid profile in overweight and obese schoolchildren. BMC Res. Notes 2012, 5, 598. [Google Scholar] [CrossRef] [Green Version]
- De Alcântara Neto, O.D.; Silva Rde, C.; Assis, A.M.; Pinto Ede, J. Factors associated with dyslipidemia in children and adolescents enrolled in public schools of Salvador, Bahia. Rev. Bras. Epidemiol. 2012, 15, 335–345. [Google Scholar]
- Pereira, A.; Guedes, A.D.; Verreschi, I.T.N.; Santos, R.D.; Martinez, T.L.R. Obesity and its association with other cardiovascular risk factors in school children in Itapetininga, Brazil. Arq. Bras. Cardiol. 2009, 93, 253–260. [Google Scholar] [PubMed] [Green Version]
- Ding, W.; Cheng, H.; Yan, Y.; Zhao, X.; Chen, F.; Huang, G.; Hou, D.; Mi, J. 10-year trends in serum lipid levels and dyslipidemia among children and adolescents from several schools in Beijing, China. J. Epidemiol. 2016, 26, 637–645. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jacob, A.S.; Reetha, G. Prevalence of metabolic comorbidities in obese children. Int. J. Contemp. Pediatr. 2017, 4, 1450–1455. [Google Scholar] [CrossRef]
- Taheri, F.; Chahkandi, T.; Kazemi, T.; Bijari, B.; Zardast, M.; Namakin, K. Lipid profiles and prevalence of dyslipidemia in eastern iranian adolescents, Birjand, 2012. Iran J. Med. Sci. 2015, 40, 341–348. [Google Scholar]
- Hashemipour, M.; Soghrati, M.; Ahmadi, M.M.; Soghrati, M. Anthropometric indices associated with dyslipidemia in obese children and adolescents: A retrospective study in Isfahan. Arya Atheroscler. 2011, 7, 31–39. [Google Scholar]
- Ghergerehchi, R. Dyslipidemia in Iranian overweight and obese children. Ther. Clin. Risk Manag. 2009, 5, 739–743. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nazli, R.; Fatima, S.; Farooq, N.; Ullah, I.; Haider, J.; Zubair, A. Frequency of dyslipidemia in young overweight and obese students (age 10–16 years) in private schools of Swat. Prof. Med. J. 2019, 26, 939–943. [Google Scholar] [CrossRef]
- Petriczko, E.; Marcisz-Grzanka, K.; Cebula, J.; Bartnik, M.; Krzywińska-Zdeb, E.; Horodnicka-Józwa, A.; Dawid, G.; Walczak, M. Metabolic complications of simple obesity in children below 10 years old. Endokrynol. Ped. 2010, 2, 27–34. [Google Scholar]
- Elmaoğulları, S.; Tepe, D.; Uçaktürk, S.A.; Karaca Kara, F.; Demirel, F. Prevalence of dyslipidemia and associated factors in obese children and adolescents. J. Clin. Res. Pediatr. Endocrinol. 2015, 7, 228–234. [Google Scholar] [CrossRef]
- Deeb, A.; Attia, S.; Mahmoud, S.; Elhaj, G.; Elfatih, A. Dyslipidemia and fatty liver disease in overweight and obese children. J. Obes. 2018, 2018, 8626818. [Google Scholar] [CrossRef] [Green Version]
- Nguyen, D.; Kit, B.; Carroll, M. Abnormal cholesterol among children and adolescents in the United States, 2011–2014. NCHS Data Brief. 2015, 228, 1–8. [Google Scholar]
- May, A.L.; Kuklina, E.V.; Yoon, P.W. Prevalence of abnormal lipid levels among youths—United States, 1999–2006. MMWR Morb. Mortal. Wkly. Rep. 2010, 59, 29–33. [Google Scholar]
- Greenacre, M. Correspondence analysis in medical research. Stat. Methods Med. Res. 1992, 1, 97–117. [Google Scholar] [CrossRef] [PubMed]
- Weller, S.C. Correspondence Analysis. In Encyclopedia of Biostatistics, 2nd ed.; Armitage, P., Colton, T., Eds.; John Wiley & Sons: London, UK, 2005. [Google Scholar]
- Bruyndonckx, L.; Hoymans, V.Y.; De Guchtenaere, A.; Van Helvoirt, M.; Van Craenenbroeck, E.M.; Frederix, G.; Lemmens, K.; Vissers, D.K.; Vrints, C.J.; Ramet, J.; et al. Diet, exercise, and endothelial function in obese adolescents. Pediatrics 2015, 135, e653–e661. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, J.; Lau, W.P.; Wang, H.; Ma, J. Evaluation of a comprehensive intervention with a behavioural modification strategy for childhood obesity prevention: A nonrandomized cluster controlled trial. BMC Public Health 2015, 15, 1206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, Q.; Ruan, H.; Tao, Y.; Zheng, X.; Shen, X.; Cai, W. Effects of a summer program for weight management in obese children and adolescents in Shanghai. Asia Pac. J. Clin. Nutr. 2014, 23, 459–464. [Google Scholar] [PubMed]
- Larsen, K.T.; Huang, T.; Ried-Larsen, M.; Andersen, L.B.; Heidemann, M.; Møller, N.C. A Multi-Component Day-Camp Weight-Loss Program Is Effective in Reducing BMI in Children after One Year: A Randomized Controlled Trial. PLoS ONE 2016, 11, e0157182. [Google Scholar] [CrossRef] [Green Version]
- Grønbæk, H.; Lange, A.; Birkebæk, N.H.; Holland-Fischer, P.; Solvig, J.; Hørlyck, A.; Kristensen, K.; Rittig, S.; Vilstrup, H. Effect of a 10-week weight loss camp on fatty liver disease and insulin sensitivity in obese Danish children. J. Pediatr. Gastroenterol. Nutr. 2012, 54, 223–228. [Google Scholar] [CrossRef]
- Obert, P.; Gueugnon, C.; Nottin, S.; Vinet, A.; Gayrard, S.; Rupp, T.; Dumoulin, G.; Tordi, N.; Mougin, F. Impact of diet and exercise training-induced weight loss on myocardial mechanics in severely obese adolescents. Obesity 2013, 21, 2091–2098. [Google Scholar] [CrossRef]
- Partsalaki, I.; Karvela, A.; Spiliotis, B.E. Metabolic impact of a ketogenic diet compared to a hypocaloric diet in obese children and adolescents. J. Pediatr. Endocrinol. Metab. 2012, 25, 697–704. [Google Scholar] [CrossRef] [PubMed]
- Verduci, E.; Lassandro, C.; Giacchero, R.; Miniello, V.L.; Banderali, G.; Radaelli, G. Change in Metabolic Profile after 1-Year Nutritional-Behavioral Intervention in Obese Children. Nutrients 2015, 7, 10089–10099. [Google Scholar] [CrossRef] [Green Version]
- Parillo, M.; Licenziati, M.R.; Vacca, M.; De Marco, D.; Iannuzzi, A. Metabolic changes after a hypocaloric, low-glycemic-index diet in obese children. J. Endocrinol. Investig. 2012, 35, 629–633. [Google Scholar] [PubMed]
- Seo, Y.G.; Lim, H.; Kim, Y.; Ju, Y.S.; Lee, H.J.; Jang, H.B.; Park, S.I.; Park, K.H. The Effect of a Multidisciplinary Lifestyle Intervention on Obesity Status, Body Composition, Physical Fitness, and Cardiometabolic Risk Markers in Children and Adolescents with Obesity. Nutrients 2019, 11, 137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kolsgaard, M.L.; Joner, G.; Brunborg, C.; Anderssen, S.A.; Tonstad, S.; Andersen, L.F. Reduction in BMI z-score and improvement in cardiometabolic risk factors in obese children and adolescents. The Oslo Adiposity Intervention Study—A hospital/public health nurse combined treatment. BMC Pediatr. 2011, 11, 47. [Google Scholar] [CrossRef] [Green Version]
- Murer, S.B.; Knöpfli, B.H.; Aeberli, I.; Jung, A.; Wildhaber, J.; Wildhaber-Brooks, J.; Zimmermann, M.B. Baseline leptin and leptin reduction predict improvements in metabolic variables and long-term fat loss in obese children and adolescents: A prospective study of an inpatient weight-loss program. Am. J. Clin. Nutr. 2011, 93, 695–702. [Google Scholar] [CrossRef] [PubMed]
- Visuthranukul, C.; Sirimongkol, P.; Prachansuwan, A.; Pruksananonda, C.; Chomtho, S. Low-glycemic index diet may improve insulin sensitivity in obese children. Pediatr. Res. 2015, 78, 567–573. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doughty, K.N.; Njike, V.Y.; Katz, D.L. Effects of a cognitive-behavioral therapy-based immersion obesity treatment program for adolescents on weight, fitness, and cardiovascular risk factors: A pilot study. Child Obes. 2015, 11, 215–218. [Google Scholar] [CrossRef] [Green Version]
- Macknin, M.; Kong, T.; Weier, A.; Worley, S.; Tang, A.S.; Alkhouri, N.; Golubic, M. Plant-based, no-added-fat or American Heart Association diets: Impact on cardiovascular risk in obese children with hypercholesterolemia and their parents. J. Pediatr. 2015, 166, 953–959. [Google Scholar] [CrossRef] [Green Version]
- Nourse, S.E.; Olson, I.; Popat, R.A.; Stauffer, K.J.; Vu, C.N.; Berry, S.; Kazmucha, J.; Ogareva, O.; Couch, S.C.; Urbina, E.M.; et al. Live Video Diet and Exercise Intervention in Overweight and Obese Youth: Adherence and Cardiovascular Health. J. Pediatr. 2015, 167, 533–539. [Google Scholar] [CrossRef] [PubMed]
- Bean, M.K.; Mazzeo, S.E.; Stern, M.; Evans, R.K.; Bryan, D.; Ning, Y.; Wickham, E.P., 3rd; Laver, J. Six-month dietary changes in ethnically diverse, obese adolescents participating in a multidisciplinary weight management program. Clin. Pediatr. (Phila) 2011, 50, 408–416. [Google Scholar] [CrossRef] [Green Version]
- Savoye, M.; Nowicka, P.; Shaw, M.; Yu, S.; Dziura, J.; Chavent, G.; O’Malley, G.; Serrecchia, J.B.; Tamborlane, W.V.; Caprio, S. Long-term results of an obesity program in an ethnically diverse pediatric population. Pediatrics 2011, 127, 402–410. [Google Scholar] [CrossRef] [Green Version]
- Jacob, J.J.; Isaac, R. Behavioral therapy for management of obesity. Indian J. Endocrinol. Metab. 2012, 16, 28–32. [Google Scholar] [CrossRef] [PubMed]
- Ho, M.; Garnett, S.P.; Baur, L.; Burrows, T.; Stewart, L.; Neve, M.; Collins, C. Effectiveness of lifestyle interventions in child obesity: Systematic review with meta-analysis. Pediatrics 2012, 130, e1647–e1671. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sbruzzi, G.; Eibel, B.; Barbiero, S.M.; Petkowicz, R.O.; Ribeiro, R.O.; Cesa, C.C.; Martins, C.C.; Marobin, R.; Schaan, C.W.; Souza, W.B.; et al. Educational interventions in childhood obesity: A systematic review with meta-analysis of randomized clinical trials. Prev. Med. 2013, 56, 254–264. [Google Scholar] [CrossRef]
- Janicke, D.M.; Steele, R.G.; Gayes, L.A.; Lim, C.S.; Clifford, L.M.; Schneider, E.M.; Carmody, J.K.; Westen, S. Systematic review and meta-analysis of comprehensive behavioral family lifestyle interventions addressing pediatric obesity. J. Pediatric Psychol. 2014, 39, 809–825. [Google Scholar] [CrossRef] [Green Version]
- O’Connor, E.A.; Evans, C.V.; Burda, B.U.; Walsh, E.S.; Eder, M.; Lozano, P. screening for obesity and intervention for weight management in children and adolescents. Evidence report and systematic review for the US Preventive Services Task Force. JAMA 2017, 317, 2427–2444. [Google Scholar] [CrossRef]
- Mead, E.; Brown, T.; Rees, K.; Azevedo, L.B.; Whittaker, V.; Jones, D.; Olajide, J.; Mainardi, G.M.; Corpeleijn, E.; O’Malley, C.; et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11 years. Coch. Dat. Sys. Rev. 2017, 6, CD012651. [Google Scholar] [CrossRef] [Green Version]
- Rajjo, T.; Mohammed, K.; Alsawas, M.; Ahmed, A.T.; Farah, W.; Asi, N.; Almasri, J.; Prokop, L.J.; Murad, M.H. Treatment of pediatric obesity: An umbrella systematic review. J. Clin. Endocrinol. Metab. 2017, 102, 763–775. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El-Medany, A.Y.M.; Birch, L.; Hunt, L.P.; Matson, R.I.B.; Chong, A.H.W.; Beynon, R.; Hamilton-Shield, J.; Perry, R. What change in body mass index is required to improve cardiovascular outcomes in childhood and adolescent obesity through lifestyle interventions: A meta-regression. Child Obes. 2020, 16, 449–478. [Google Scholar] [CrossRef]
- Ford, A.L.; Hunt, L.P.; Cooper, A.; Shield, J.P.H. What reduction in BMI SDS is required in obese adolescents to improve body composition and cardiometabolic health? Arch Dis. Child. 2010, 95, 256–261. [Google Scholar] [CrossRef]
- Ewald, H.; Kirby, J.; Rees, K.; Robertson, W. Parent-only interventions in the treatment of childhood obesity: A systematic review of randomized controlled trials. J. Public Health 2014, 36, 476–489. [Google Scholar] [CrossRef] [Green Version]
- Jull, A.; Chen, R. Parent-only vs. parent-child (family-focused) approaches for weight loss in obese and overweight children: A systematic review and meta-analysis. Obes. Rev. 2013, 14, 761–768. [Google Scholar] [CrossRef]
- Kelishadi, R.; Azizi-Soleiman, F. Controlling childhood obesity: A systematic review on strategies and challenges. J. Res. Med. Sci. 2014, 19, 993–1008. [Google Scholar]
- Skouteris, H.; McCabe, M.; Swinburn, B.; Newgreen, V.; Sacher, P.; Chadwick, P. Parental influence and obesity prevention in pre-schoolers: A systematic review of interventions. Obes. Rev. 2011, 12, 315–328. [Google Scholar] [CrossRef]
- Loveman, E.; Al-Khudairy, L.; Johnson, R.E.; Robertson, W.; Colquitt, J.L.; Mead, E.L.; Ells, L.J.; Metzendorf, M.; Rees, K. Parent-only interventions for childhood overweight or obesity in children aged 5 to 11 years. Cochrane Database Syst. Rev. 2015, 12, CD012008. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Country, Year [Reference] | Participants, Criteria for Overweight and Obesity | Duration of the Intervention, Study Design | Therapeutic Team | Characteristics of the Intervention | Control Group | Effect of the Intervention |
|---|---|---|---|---|---|---|
| Belgium, 2015 [35] | n = 33, 27.3% boys, 12–18 years (mean 15.4 ± 1.5 years), BMI ≥ 97th pc (< 16 years old), BMI ≥ 35 (> 16 years old) | 10 months, quasi-randomized trial | pediatrician, physiotherapists |
| n = 28, 21.4% boys, years (mean 15.1 ± 1.2 years):
| Compared to control group: ↓ % BF, BMI, BMI z-score, BW, LDL-C ↑ HDL-C, SBP ↔ DBP, TC |
| China, 2015 [36] | n = 90, 38.9% boys, 7–12 years (mean 9.41 ± 1.03 years), BMI criteria according to WGOC | 1 year, nonrandomized controlled trial with cluster sampling | medical research postgraduate students, physical trainer | Comprehensive intervention group:
| n = 136, 32.4% boys, 7–12 years, mean age 9.16 ± 1.12 years:
| Compared to diet only intervention group: ↓ % BF, BMI, HDL-C, SBP ↔ DBP, LDL-C, WC ↑ TC, TG Compared to control group: ↓ % BF, DBP, SBP ↔ BMI, HDL-C, LDL-C, WC ↑ TC, TG |
| n = 96, 42.7% boys, 7–12 years (mean 9.27 ± 1.34 years), BMI criteria according to WGOC | Diet only intervention group:
| Compared to control group: ↔ BMI, DBP, LDL-C, SBP, TG, WC ↑ % BF, HDL-C, TC | ||||
| China, 2014 [37] | n = 20, 55% boys, 7–17 years, BMI ≥ 95th pc | 4 weeks, intervention study | no data |
| no control group | Compared to baseline: ↓ BFM, BMI, BW, DBP, LDL-C, SBP, TC, TG, WC, WHR ↔HDL-C |
| Denmark, 2016 [38] | n = 55, 47.3% boys, 11–13 years (mean 12.0 ± 0.4 years), BMI criteria according to IOTF | 1 year, randomized controlled trial | dietician, trained instructors, school nurses | Day-camp intervention (6 weeks) and family-based intervention (after day-camp):
| Standard intervention arm (SIA—6 weeks) (n = 52, 41.2% boys, 11–13 years (mean 12.0 ± 0.4 years):
| After 6 weeks, compared to SIA group: ↓ % BF, BMI, BMI z-score, TC/HDL-C ratio, SBP, WC, % of abdominal fat, clustered cardiovascular risk z-score ↔ FFM, TG After 52 weeks, compared to SIA group: ↓ BMI, BMI z-score, TC/HDL-C ratio, clustered cardiovascular risk z-score ↔ % BF, FFM, SBP, TG, WC, % of abdominal fat |
| Denmark, 2012 [39] | n = 117, 43.6% boys, mean age 12.1 ± 1.3 years, no criteria for assessing obesity | 10 weeks, intervention study | no data |
| no control group | Compared to baseline: ↓ % BF, BFM, BMI z-score, BW, DBP, LDL-C, SBP, TC, TG, WC, WHR ↔ HDL-C 12-month follow-up compared to the end of the weight loss camp: ↑ BFM, BMI z-score, BW, DBP, LDL-C, SBP, TG, TC, WC, WHR ↔ % BF, HDL-C 12-month follow-up compared to baseline: ↓ % BF, BFM, BMI z-score ↑ BW, DBP, SBP ↔ HDL-C, LDL-C, TC, TG, WC, WHR |
| France, 2013 [40] | n = 28, 32% boys, mean age 14.2 ± 1.5 years, BMI > 97th pc and BMI z-score > 3 | 9 months, intervention study | dieticians, fitness teacher |
| n = 20, 40% boys, mean age 14.9 ± 1.6 years:
| Compared to baseline: ↓ BFM, BMI, BMI z-score, BW, DBP, SBP, WC ↑ HDL-C ↔ LDL-C, TC, TG Compared to control group: ↑ BMI, BMI z-score, BW ↔ DBP, SBP |
| Greece, 2012 [41] | n = 21, 47.6% boys, 8–18 years (mean 12.8 ± 2.1 years), BMI > 95th pc | 6 months, intervention study | dietician, pediatric endocrinologist | Ketogenic diet group:
| no control group | Compared to baseline: ↓ BFM, BMI, BW, WC ↔ DBP, HDL-C, LDL-C, SBP, TC, TG Compared to hypocaloric diet group: ↔ BFM, BMI, BW, DBP, HDL-C, LDL-C, SBP, TC, TG, WC |
| n = 17, 41.2% boys, 8–18 years (mean 12.7 ± 2.8 years), BMI > 95th pc | Hypocaloric diet group:
| Compared to baseline: ↓ BFM, BMI, BW, WC ↔ DBP, HDL-C, LDL-C, SBP, TC, TG | ||||
| Italy, 2015 [42] | n = 90, 49% boys, ≥ 6 years (mean 9.7 ± 2.6 years), no criteria for assessing obesity | 1 year, intervention study | dietician, pediatrician |
| no control group | Compared to baseline: ↓ BMI z-score, TG, TG/HDL-C ratio ↑ HDL-C ↔ DBP, LDL-C, LDL-C/HDL-C ratio, SBP, TC, TC/HDL-C ratio, WC |
| Italy, 2012 [43] | n = 11, mean age 118.0 ± 19.6 months, BMI z-score ≥ 2 | 6 months, randomized controlled trial | dietician | Low Glycemic Index diet:
| no control group | Compared to baseline: ↓ BMI, BMI z-score, DBP, SBP, WC ↔ HDL-C, TC, TG Compared to HGI group: ↓ BMI, BMI z-score, TG ↔ HDL-C, TC |
| n = 11, mean age 113.9 ± 19.4 months, BMI z-score ≥ 2 | High Glycemic Index diet group (HGI):
| Compared to baseline: ↓ BMI, BMI z-score, DBP, SBP ↔ HDL-C, TC, TG, WC | ||||
| Korea, 2019 [44] | n = 44, 63.6% boys, 6–16 years (mean 12.1 ± 2.2 years), BMI > 85th pc | 16 weeks, intervention study | doctor, clinical dietician, social workers, nurses | Usual care group:
| no control group | Compared to baseline: ↑ BFM, LM ↔ % BF, BMI z-score, DBP, HDL-C, LDL-C, SBP, TG, WC |
| n = 26, 65.4% boys 6–16 years (mean 12.8 ± 1.7 years), BMI > 85th pc | doctor, clinical dietician, exercise specialists, social workers, nurses | Exercise group:
| Compared to baseline: ↑ LM ↓ % BF, BMI z-score, DBP, LDL-C ↔ BFM, HDL-C, SBP, TG, WC Compared to usual care group: ↓ BMI z-score | |||
| Norway, 2011 [45] | n = 230, 47.4% boys, 7–17 years, body weight > 97.5 pc for height | 1 year, intervention study | clinical nutritionist, pediatrician, physical activity specialist, public health nurses |
| no control group | Compared to baseline: ↓ BMI z-score, LDL-C, TC ↔ HDL-C, TG |
| Switzerland, 2011 [46] | n = 203, 56.2% boys, mean age 14.1 ± 2.0 years, BMI > 98th pc | 2 months, prospective study | dietician, exercise therapist pediatrician, psychologist, nurses |
| no control group | Compared to baseline: ↓ % BF, BFM, BMI z-score, BW, HDL-C, LDL-C, SBP, TC, TG ↔ DBP 6- and 12-months follow-up compared to baseline: ↓ % BF, BFM, BMI z-score, BW ↑ LM |
| Thailand, 2015 [47] | n = 25, 64% boys, 9–16 years (mean 11.9 ± 1.9 years), BMI criteria according to IOTF | 6 months, prospective randomized controlled trial | dietician, pediatrician |
| n = 27, 70.3% boys, 9–16 years, mean age 12.0 ± 2.1 years:
| Compared to baseline: ↓ BMI z-score ↔ % BF, DBP, HDL-C, LDL-C, SBP, TC, TG, WC Compared to control group: ↔ % BF, BMI, BMI z-score, HDL-C, LDL-C, TC, TG, WC |
| United States, 2015 [48] | n = 12, 8.3% boys, 13–17 years (mean 15.2 ± 1.3 years), BMI > 95th pc | 14–18 weeks, intervention study | no data |
| no control group | Compared to baseline: ↓ BMI, BMI z-score, BW, LDL-C, TC, WC ↔ DBP, SBP, TG ↑ HDL-C |
| United States, 2015 [49] | n =14, 36% boys, 9–18 years, BMI ≥ 95th pc | 4 weeks, prospective randomized trial | no data | Plant-based no added fat diet group:
| no control group | Compared to baseline: ↓ BMI z-score, LDL-C, SBP, TC ↔ BW, DBP, HDL-C, TG, WC Compared to AHA group: ↓ BMI z-score ↔ BW, DBP, HDL-C, LDL-C, SBP, TC, TG, WC |
| n = 14, 36% boys, 9–18 years, BMI ≥ 95th pc | The American Heart Association diet group (AHA):
| Compared to baseline: ↓ HDL-C, WC ↔ BMI z-score, BW, DBP, LDL-C, SBP, TC, TG | ||||
| United States, 2015 [50] | n = 20, 55% boys, 10–19 years (mean 14.3 ± 2.1 years), BMI > 85th pc | 12 weeks, intervention study | nutritionist, trainer |
| no control group | Compared to baseline: ↓ LDL-C, TC, WHR ↔ BMI, BMI z-score, BW, DBP, HDL-C, SBP, TG |
| United States, 2011 [51] | n = 186, 33.9% boys, 11–18 years (mean 13.7 ± 1.8 years), BMI ≥ 95th pc | 6 months, intervention study | dietician, behavioral support specialist, exercise physiologist |
| no control group | Compared to baseline: ↓ % BF, BMI, BMI z-score, HDL-C, LDL-C, TC, TG |
| United States, 2011 [52] | n = 105, 44.8% boys, 8–16 years (mean 12.0 ± 2.5 years), BMI ≥ 95th pc | 2 years, randomized controlled trial | dieticians, physicians, exercise physiologists, social worker |
| n = 69, 31.9% boys, 8–16 years (mean 12.5 ± 2.3 years):
| Compared to control group—end of intervention: ↓ % BF, BFM, BMI, BMI z-score, BW, TC ↔ DBP, HDL-C, LDL-C, SBP, TG Compared to control group after 12-month follow-up: ↓ % BF, BFM, BMI, BMI z-score, BW, LDL-C, TC ↔ DBP, HDL-C, SBP, TG |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bondyra-Wiśniewska, B.; Myszkowska-Ryciak, J.; Harton, A. Impact of Lifestyle Intervention Programs for Children and Adolescents with Overweight or Obesity on Body Weight and Selected Cardiometabolic Factors—A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 2061. https://doi.org/10.3390/ijerph18042061
Bondyra-Wiśniewska B, Myszkowska-Ryciak J, Harton A. Impact of Lifestyle Intervention Programs for Children and Adolescents with Overweight or Obesity on Body Weight and Selected Cardiometabolic Factors—A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(4):2061. https://doi.org/10.3390/ijerph18042061
Chicago/Turabian StyleBondyra-Wiśniewska, Beata, Joanna Myszkowska-Ryciak, and Anna Harton. 2021. "Impact of Lifestyle Intervention Programs for Children and Adolescents with Overweight or Obesity on Body Weight and Selected Cardiometabolic Factors—A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 4: 2061. https://doi.org/10.3390/ijerph18042061







