Healthcare Professionals’ Perspective on Implementing a Detector of Behavioural Disturbances in Long-Term Care Homes
Abstract
1. Introduction
1.1. Background
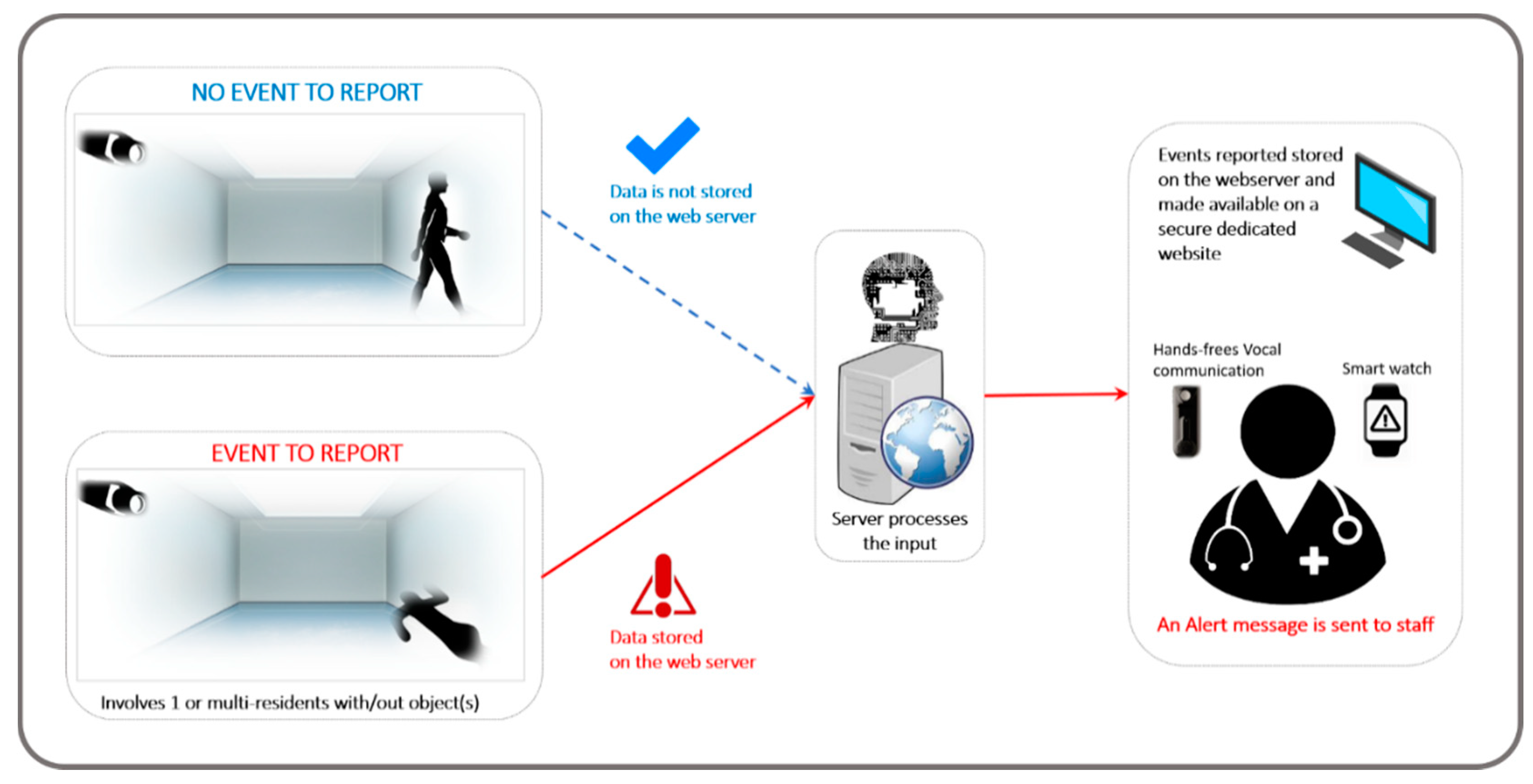
1.2. Description of the Detector of Behavioural Disturbances
2. Materials and Methods
2.1. Study Design
2.2. Focus Group Participants
2.3. Data Collection
2.4. Analytical Plan and Reporting of Results
3. Results
3.1. Ability of the DBD to Detect Relevant Dementia-Related Behavioural Disturbances
“I hate to put this in words, but think of an elderly PwD…any kind as being a child again. Would you leave your child with, without being watched at any given time? Or any place?...Of course not, but that’s what happens. And when in a nursing facility, there isn’t the staffing to have the one-on-one, which would be appropriate, as you would with a child.”
- Behaviours between persons (n = 6): “fighting another person”, “slapping another person”, “pushing another person”, “kicking another person”, “stabbing another person”, and “punching another person”.
- Individual behaviours (n = 8): “walking without a walker”, “falling”, “throwing items”,“ grabbing items off walls”, “walking into another person’s room”, “biting themselves”, “putting things in their mouths, and “scratching themselves”.
3.2. Characteristics of the DBD and Clinical Needs and Preferences
“Yeah, I think best case scenario, obviously, we all want more bodies on the floor to help with, you know, the work load. It’s a lot for the staff, so we want some more staff on the floor uhm…but because that’s not really a feasible option these days, it seems like any kind of technology that could help.”
3.2.1. Benefits of the DBD
- Safety and quicker response time
“It would give maybe nursing and healthcare aides a little bit of peace of mind too that they can do their job better because they’re not constantly having to leave while they’re handing out meds…I think it would be a little more efficient.”
- The DBD as a recording device
“If it’s always going to be real-time or something that’s recorded, then that might be more helpful for OT to kind of go back and look back at what was the factors…So it would help to piece together…potentially how that fall happened, which would…might be helpful for occupational therapists or physiotherapists.”
“I’ve had incidents too, where someone’s been injured by another client, and they’re not found because that person left the room. Or someone’s fallen, and so it’s not someone that you know is high risk and they’ve fallen in the bathroom. This would make me be able to go to them right away than them lying there. Especially if it’s evenings or nights and you’re all busy, and you’re making 1-h checks, someone could be lying on the floor.”
“I think it would help build the trust level between staff and families because we could be more transparent with what actually occurred. I think that would increase our trusting.”
- Support for family members
“Well, the families would be more relieved knowing…more at peace when they go home. Knowing that there are cameras… Like if something happens in the room, it’s going to help, I guess, the family to know that somebody is coming if an incident happens.”
3.2.2. Limitations of the DBD
- Cost
“Cost is always a challenge these days, but purchasing the equipment, paying for things like training. Yeah, I mean the reality of the climate these days is cost is always a barrier and an issue.”
- Integration into the workflow
“You don’t want, really, people sitting there watching the screen when ideally we should be engaging with the residents, right.”
“I think communication of expectations of how it should be used as a resource or how much time should be spent watching it versus being out there, that kind of balance. So communicating how to use the tool effectively, I guess.”
- Potential for behaviour change
“A person can only run as far as they can, you can have all the technology in the world, but it’s that person getting to that incident in an amount of time down the hall and that’s staffing, so…as you said…Uhm you know you can see it on camera, but how fast can you get them to…can you get them from A to B?”
3.3. Integration of the DBD into Daily Routines
“You want to make, like, it easier for staff, not add another thing… Like something that’s already linking to what we have versus kind of adding on.”
3.3.1. Location
“...definitely, because it does escalate in the room with my partner, and I…I had to back off or he was ready to hit me, but, like you say, he…that, that wasn’t his personality before, so you really have to be patient with them and realize where they’re coming from and what’s happened to them, but not all family members know that... They can’t understand and it’s very difficult so to have a camera in the room or something by us would just [be] great.”
3.3.2. Modes of Communication
3.3.3. Professions
“You’d need the whole floor like the nurses and healthcare aides who are there all the time. I think all of them would have to be able to have like that quick time access cause a nurse might be on rounds and it’s the aides on the floor or a nurse is in one room and like I think it has to be everybody, you can’t just assign one just by the nature of what happens day-to-day… It’s your aides and nurses that really need that information the most cause they are like very front-line and would respond first.”
4. Discussion
- Allows nurses and healthcare aides to be more efficient in performing their daily tasks;
- Increases response time to hazardous events;
- Enables prevention of a hazardous event (being able to intervene before a more hazardous event takes place);
- Increases safety for staff (being able to go back and see what exactly happened in the event that staff is accused of malpractice);
- Using this device as a recording would help allied healthcare professionals go back in time and piece together how a fall or another hazardous event occurred;
- Increases the trust level between staff and family members;
- Allows families to feel more at peace when they leave.
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Manuel, D.G.; Garner, R.; Finès, P.; Bancej, C.; Flanagan, W.; Tu, K.; Reimer, K.; Chambers, L.W.; Bernier, J. Alzheimer’s and other dementias in Canada, 2011 to 2031: A microsimulation Population Health Modeling (POHEM) study of projected prevalence, health burden, health services, and caregiving use. Popul. Health Metr. 2016, 14, 37. [Google Scholar] [CrossRef]
- Alzheimer Society of Canada. Report Summary Prevalence and Monetary Costs of Dementia in Canada (2016): A Report by the Alzheimer Society of Canada; Public Health Agency of Canada: Ottawa, ON, Canada, 2016; pp. 231–232. Available online: https://www.canada.ca/en/public-health/services/reports-publications/health-promotion-chronic-disease-prevention-canada-research-policy-practice/vol-36-no-10-2016/report-summary-prevalence-monetary-costs-dementia-canada-2016-report-alzheimer-society-canada.html (accessed on 10 December 2020).
- Salloway, S.; Mintzer, J.; Weiner, M.F.; Cummings, J.L. Disease-modifying therapies in Alzheimer’s disease. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2008, 4, 65–79. [Google Scholar] [CrossRef]
- Wennberg, A.M.V.; Wu, M.N.; Rosenberg, P.B.; Spira, A.P. Sleep Disturbance, Cognitive Decline, and Dementia: A Review. Semin. Neurol. 2017, 37, 395–406. [Google Scholar]
- Volicer, L. Behavioral Problems and Dementia. Clin. Geriatr. Med. 2018, 34, 637–651. [Google Scholar] [CrossRef] [PubMed]
- Apostolova, L.G.; Cummings, J.L. Neuropsychiatric manifestations in mild cognitive impairment: A systematic review of the literature. Dement. Geriatr. Cogn. Disord. 2008, 25, 115–126. [Google Scholar] [CrossRef]
- Spalletta, G.; Musicco, M.; Padovani, A.; Perri, R.; Fadda, L.; Canonico, V.; Trequattrini, A.; Pettenati, C.; Caltagirone, C.; Palmer, K.; et al. Neuropsychiatric symptoms and syndromes in a large cohort of newly diagnosed, untreated patients with Alzheimer disease. Am. J. Geriatr. Psychiatry Off. J. Am. Assoc. Geriatr. Psychiatry 2010, 18, 1026–1035. [Google Scholar] [CrossRef]
- Seignourel, P.J.; Kunik, M.E.; Snow, L.; Wilson, N.; Stanley, M. Anxiety in dementia: A critical review. Clin. Psychol. Rev. 2008, 28, 1071–1082. [Google Scholar] [CrossRef] [PubMed]
- Ferretti, L.; McCurry, S.M.; Logsdon, R.; Gibbons, L.; Teri, L. Anxiety and Alzheimer’s disease. J. Geriatr. Psychiatry Neurol. 2001, 14, 52–58. [Google Scholar] [CrossRef]
- Ohman, A.; Mineka, S. Fears, phobias, and preparedness: Toward an evolved module of fear and fear learning. Psychol. Rev. 2001, 108, 483–522. [Google Scholar] [CrossRef] [PubMed]
- Levenson, R.W. Blood, sweat, and fears: The autonomic architecture of emotion. Ann. N. Y. Acad. Sci. 2003, 1000, 348–366. [Google Scholar] [CrossRef]
- Hope, R.A.; Fairburn, C.G. The nature of wandering in dementia: A community-based study. Int. J. Geriatr. Psychiatry 1990, 5, 239–245. [Google Scholar] [CrossRef]
- Rowe, M.A.; Bennett, V. A look at deaths occurring in persons with dementia lost in the community. Am. J. Alzheimer’s Dis. Other Dement. 2003, 18, 343–348. [Google Scholar] [CrossRef]
- Sverdrup, K.; Bergh, S.; Selbaek, G.; Roen, I.; Kirkevold, O.; Tangen, G.G. Mobility and cognition at admission to the nursing home—A cross-sectional study. BMC Geriatr. 2018, 18, 30. [Google Scholar] [CrossRef] [PubMed]
- Poranen-Clark, T.; von Bonsdorff, M.B.; Rantakokko, M.; Portegijs, E.; Eronen, J.; Kauppinen, M.; Eriksson, J.G.; Rantanen, T.; Viljanen, A. Executive function and life-space mobility in old age. Aging Clin. Exp. Res. 2018, 30, 145–151. [Google Scholar] [CrossRef]
- Brown, C.J.; Roth, D.L.; Allman, R.M.; Sawyer, P.; Ritchie, C.S.; Roseman, J.M. Trajectories of life-space mobility after hospitalization. Ann. Intern. Med. 2009, 150, 372–378. [Google Scholar] [CrossRef]
- Crowe, M.; Andel, R.; Wadley, V.G.; Okonkwo, O.C.; Sawyer, P.; Allman, R.M. Life-space and cognitive decline in a community-based sample of African American and Caucasian older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2008, 63, 1241–1245. [Google Scholar] [CrossRef]
- O’Connor, M.L.; Edwards, J.D.; Wadley, V.G.; Crowe, M. Changes in mobility among older adults with psychometrically defined mild cognitive impairment. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2010, 65, 306–316. [Google Scholar] [CrossRef]
- Lo, A.X.; Rundle, A.G.; Buys, D.; Kennedy, R.E.; Sawyer, P.; Allman, R.M.; Brown, C.J. Neighborhood Disadvantage and Life-Space Mobility Are Associated with Incident Falls in Community-Dwelling Older Adults. J. Am. Geriatr. Soc. 2016, 64, 2218–2225. [Google Scholar] [CrossRef]
- Ikezoe, T.; Mori, N.; Nakamura, M.; Ichihashi, N. Age-related muscle atrophy in the lower extremities and daily physical activity in elderly women. Arch. Gerontol. Geriatr. 2011, 53, e153–e157. [Google Scholar] [CrossRef] [PubMed]
- Goode, P.S.; Burgio, K.L.; Halli, A.D.; Jones, R.W.; Richter, H.E.; Redden, D.T.; Baker, P.S.; Allman, R.M. Prevalence and correlates of fecal incontinence in community-dwelling older adults. J. Am. Geriatr. Soc. 2005, 53, 629–635. [Google Scholar] [CrossRef]
- Makhija, S.K.; Gilbert, G.H.; Clay, O.J.; Matthews, J.C.; Sawyer, P.; Allman, R.M. Oral health-related quality of life and life-space mobility in community-dwelling older adults. J. Am. Geriatr. Soc. 2011, 59, 512–518. [Google Scholar] [CrossRef][Green Version]
- Rantakokko, M.; Portegijs, E.; Viljanen, A.; Iwarsson, S.; Kauppinen, M.; Rantanen, T. Changes in life-space mobility and quality of life among community-dwelling older people: A 2-year follow-up study. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 2016, 25, 1189–1197. [Google Scholar] [CrossRef]
- Tsutsumimoto, K.; Doi, T.; Shimada, H.; Makizako, H.; Uemura, K.; Ando, H.; Suzuki, T. Self-reported Exhaustion is Associated with Small Life Space in Older Adults with Mild Cognitive Impairment. J. Phys. Ther. Sci. 2014, 26, 1979–1983. [Google Scholar] [CrossRef][Green Version]
- Xue, Q.L.; Fried, L.P.; Glass, T.A.; Laffan, A.; Chaves, P.H. Life-space constriction, development of frailty, and the competing risk of mortality: The Women’s Health And Aging Study I. Am. J. Epidemiol. 2008, 167, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Al Snih, S.; Peek, K.M.; Sawyer, P.; Markides, K.S.; Allman, R.M.; Ottenbacher, K.J. Life-space mobility in Mexican Americans aged 75 and older. J. Am. Geriatr. Soc. 2012, 60, 532–537. [Google Scholar] [CrossRef] [PubMed]
- Peel, C.; Sawyer Baker, P.; Roth, D.L.; Brown, C.J.; Brodner, E.V.; Allman, R.M. Assessing mobility in older adults: The UAB Study of Aging Life-Space Assessment. Phys. Ther. 2005, 85, 1008–1119. [Google Scholar] [CrossRef] [PubMed]
- Shimada, H.; Ishizaki, T.; Kato, M.; Morimoto, A.; Tamate, A.; Uchiyama, Y.; Yasumura, S. How often and how far do frail elderly people need to go outdoors to maintain functional capacity? Arch. Gerontol. Geriatr. 2010, 50, 140–146. [Google Scholar] [CrossRef]
- May, D.; Nayak, U.S.; Isaacs, B. The life-space diary: A measure of mobility in old people at home. Int. Rehabil. Med. 1985, 7, 182–186. [Google Scholar] [CrossRef]
- Barnes, L.L.; Wilson, R.S.; Bienias, J.L.; Mendes de Leon, C.F.; Kim HJ, N.; Buchman, A.S.; Bennett, D.A. Correlates of life space in a volunteer cohort of older adults. Exp. Aging Res. 2007, 33, 77–93. [Google Scholar] [CrossRef] [PubMed]
- James, B.D.; Boyle, P.A.; Buchman, A.S.; Barnes, L.L.; Bennett, D.A. Life space and risk of Alzheimer disease, mild cognitive impairment, and cognitive decline in old age. Am. J. Geriatr. Psychiatry Off. J. Am. Assoc. Geriatr. Psychiatry 2011, 19, 961–969. [Google Scholar] [CrossRef]
- Baker, P.S.; Bodner, E.V.; Allman, R.M. Measuring life-space mobility in community-dwelling older adults. J. Am. Geriatr. Soc. 2003, 51, 1610–1614. [Google Scholar] [CrossRef] [PubMed]
- Uemura, K.; Shimada, H.; Makizako, H.; Yoshida, D.; Doi, T.; Yamada, M.; Suzuki, T. Factors associated with life-space in older adults with amnestic mild cognitive impairment. Geriatr. Gerontol. Int. 2013, 13, 161–166. [Google Scholar] [CrossRef]
- Sartori, A.C.; Wadley, V.G.; Clay, O.J.; Parisi, J.M.; Rebok, G.W.; Crowe, M. The relationship between cognitive function and life space: The potential role of personal control beliefs. Psychol. Aging 2012, 27, 364–374. [Google Scholar] [CrossRef]
- Webber, S.C.; Porter, M.M.; Menec, V.H. Mobility in older adults: A comprehensive framework. Gerontologist 2010, 50, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Stalvey, B.T.; Owsley, C.; Sloane, M.E.; Ball, K. The Life Space Questionnaire: A Measure of the Extent of Mobility of Older Adults. J. Appl. Gerontol. 1999, 18, 460–478. [Google Scholar] [CrossRef]
- Øderud, T.; Landmark, B.; Eriksen, S.; Fossberg, A.B.; Aketun, S.; Omland, M.; Hem, K.G.; Østensen, E.; Ausen, D. Persons with Dementia and Their Caregivers Using GPS. Stud. Health Technol. Inform. 2015, 217, 212–221. [Google Scholar] [PubMed]
- Pot, A.M.; Willemse, B.M.; Horjus, S. A pilot study on the use of tracking technology: Feasibility, acceptability, and benefits for people in early stages of dementia and their informal caregivers. Aging Ment. Health 2012, 16, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Haque, A.; Milstein, A.; Fei-Fei, L. Illuminating the dark spaces of healthcare with ambient intelligence. Nature 2020, 585, 193–202. [Google Scholar] [CrossRef]
- Olsson, A.; Engstrom, M.; Asenlof, P.; Skovdahl, K.; Lampic, C. Effects of tracking technology on daily life of persons with dementia: Three experimental single-case studies. Am. J. Alzheimer’s Dis. Other Dement. 2015, 30, 29–40. [Google Scholar] [CrossRef]
- Youngblood, G.M.; Cook, D.J. Data Mining for Hierarchical Model Creation. IEEE Trans. Syst. Man Cybern. Part C (Appl. Rev.) 2007, 37, 561–572. [Google Scholar] [CrossRef]
- Helal, S.; Mann, W.; El-Zabadani, H.; King, J.; Kaddoura, Y.; Jansen, E. The Gator Tech Smart House: A programmable pervasive space. Computer 2005, 38, 50–60. [Google Scholar] [CrossRef]
- Doctor, F.; Hagras, H.; Callaghan, V. A fuzzy embedded agent-based approach for realizing ambient intelligence in intelligent inhabited environments. IEEE Trans. Syst. Man Cybern. Part A Syst. Hum. 2005, 35, 55–65. [Google Scholar] [CrossRef]
- Abowd, G.D.; Mynatt, E.D. Designing for the Human Experience in Smart Environments. In Smart Environments; Cook, D.J., Das, S.K., Eds.; Wiley Interscience: Hoboken, NJ, USA, 2004; pp. 151–174. [Google Scholar]
- Dodge, H.H.; Mattek, N.C.; Austin, D.; Hayes, T.L.; Kaye, J.A. In-home walking speeds and variability trajectories associated with mild cognitive impairment. Neurology 2012, 78, 1946–1952. [Google Scholar] [CrossRef]
- Lam, K.-Y.; Tsang, N.W.-H.; Han, S.; Zhang, W.; Ng, J.K.-Y.; Nath, A. Activity tracking and monitoring of patients with alzheimer’s disease. Multimed. Tools Appl. 2017, 76, 489–521. [Google Scholar] [CrossRef]
- Sánchez, D.; Tentori, M.; Favela, J. Activity Recognition for the Smart Hospital. IEEE Intell. Syst. 2008, 23, 50–57. [Google Scholar] [CrossRef]
- Eisa, S.; Moreira, A. A Behaviour Monitoring System (BMS) for Ambient Assisted Living. Sensors (Basel) 2017, 17, 1946. [Google Scholar] [CrossRef]
- Chiauzzi, E.; Rodarte, C.; DasMahapatra, P. Patient-centered activity monitoring in the self-management of chronic health conditions. BMC Med. 2015, 13, 77. [Google Scholar] [CrossRef] [PubMed]
- Brulin, D.; Benezeth, Y.; Courtial, E. Posture recognition based on fuzzy logic for home monitoring of the elderly. IEEE Trans. Inf. Technol. Biomed. 2012, 16, 974–982. [Google Scholar] [CrossRef] [PubMed]
- Van, N.; Javaid, A.Q.; Weitnauer, M.A. Detection of motion and posture change using an IR-UWB radar. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016; Volume 2016, pp. 3650–3653. [Google Scholar]
- Takano, M.; Ueno, A. Noncontact In-Bed Measurements of Physiological and Behavioral Signals Using an Integrated Fabric-Sheet Sensing Scheme. IEEE J. Biomed. Health Inform. 2019, 23, 618–630. [Google Scholar] [CrossRef] [PubMed]
- Cvetkoska, B.; Marina, N.; Bogatinoska, D.C.; Mitreski, Z. Smart Mirror E-health Assistant—Posture Analyze Algorithm. In Proceedings of the IEEE EUROCON 2017-17th International Conference on Smart Technologies, Ohrid, North Macedonia, 6–8 July 2017. [Google Scholar]
- Nasution, A.H.; Emmanuel, S. Intelligent video surveillance for monitoring elderly in home environments. In Proceedings of the 2007 IEEE 9th Workshop on Multimedia Signal Processing, Chania, Greece, 1–3 October 2007. [Google Scholar]
- Mongkolnam, P.; Booranrom, Y.; Watanapa, B.; Visutarrom, T.; Chan, J.H.; Nukoolkit, C. Smart bedroom for the elderly with gesture and posture analyses using Kinect. Maejo Int. J. Sci. Technol. 2017, 11, 1. [Google Scholar]
- Yu, J.; An, N.; Hassan, T.; Kong, Q. A Pilot Study on a Smart Home for Elders Based on Continuous In-Home Unobtrusive Monitoring Technology. HERD Health Environ. Res. Des. J. 2019, 12, 206–219. [Google Scholar] [CrossRef]
- Chen, D.; Bharucha, A.J.; Wactlar, H.D. Intelligent video monitoring to improve safety of older persons. In Proceedings of the 2007 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Lyon, France, 22–26 August 2007; Volume 2007, pp. 3814–3817. [Google Scholar]
- Zhou, Q.; Yu, S.; Wu, X.; Gao, Q.; Li, C.; Xu, Y. HMMs-Based Human Action Recognition for an Intelligent Household Surveillance Robot. In Proceedings of the 2009 IEEE International Conference on Robotics and Biomimetics (ROBIO), Guilin, China, 19–23 December 2009. [Google Scholar] [CrossRef]
- Hevesi, P.; Wille, S.; Pirkl, G.; When, N.; Lukowicz, P. Monitoring Household Activities and User Location with a Cheap, Unobtrusive Thermal Sensor Array. In Proceedings of the UbiComp ’14: Proceedings of the 2014 ACM International Joint Conference on Pervasive and Ubiquitous Computing, Seattle, WA, USA, September 2014; pp. 141–145. [Google Scholar] [CrossRef]
- Hossain, M.A.; Ahmed, D.T. Virtual caregiver: An ambient-aware elderly monitoring system. IEEE Trans Inf Technol Biomed. 2012, 16, 1024–1031. [Google Scholar] [CrossRef]
- Ariani, A.; Redmond, S.J.; Zhang, Z.; Narayanan, M.R.; Lovell, N.H. Design of an unobtrusive system for fall detection in multiple occupancy residences. In Proceedings of the 2013 35th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), 3–7 July, Osaka, Japan; Volume 2013, pp. 4690–4693. [CrossRef]
- Chaaraoui, A.A.; Padilla-Lopez, J.R.; Ferrández-Pastor, F.J.; Nieto-Hidalgo, M.; Flórez-Revuelta, F. A vision-based system for intelligent monitoring: Human behaviour analysis and privacy by context. Sensors 2014, 14, 8895–8925. [Google Scholar] [CrossRef] [PubMed]
- Chernbumroong, S.; Lotfi, A.; Langensiepen, C. Prediction of Mobility Entropy in an Ambient Intelligent Environment. In Proceedings of the 2014 IEEE Symposium on Intelligent Agents (IA), Orlando, FL, USA, 9–12 December 2014. [Google Scholar] [CrossRef]
- Pino, E.J.; Moran, A.A.; Dorner De la Paz, A.; Aqueveque, P. Validation of non-invasive monitoring device to evaluate sleep quality. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; Volume 2015, pp. 7974–7977. [Google Scholar] [CrossRef]
- Sadek, I.; Mohktari, M. Nonintrusive Remote Monitoring of Sleep in Home-Based Situation. J. Med. Syst. 2018, 42, 64. [Google Scholar] [CrossRef]
- Tataraidze, A.; Korostovtseva, L.; Anishchenko, L.; Bochkarev, M.; Sviryaev, Y.; Ivashov, S. Bioradiolocation-based sleep stage classification. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016; Volume 2016, pp. 2839–2842. [Google Scholar] [CrossRef]
- Aloulou, H.; Mokhtari, M.; Tiberghien, T.; Biswas, J.; Phua, C.; Lin, J.H.K.; Yap, P. Deployment of assistive living technology in a nursing home environment: Methods and lessons learned. BMC Med Inform. Decis. Mak. 2013, 13, 42. [Google Scholar] [CrossRef] [PubMed]
- Coughlin, J.; D’Ambrosio, L.A.; Reimer, B.; Pratt, M.R. Older adult perceptions of smart home technologies: Implications for research, policy & market innovations in healthcare. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society IEEE Engineering in Medicine and Biology Society Annual Conference, Lyon, France, 22–26 August 2007; Volume 2007, pp. 1810–1815. [Google Scholar]
- Blasco, R.; Marco, A.; Casas, R.; Cirujano, D.; Picking, R. A smart kitchen for ambient assisted living. Sensors (Basel) 2014, 14, 1629–1653. [Google Scholar] [CrossRef]
- Hein, A.; Winkelbach, S.; Martens, B.; Wilken, O.; Eichelberg, M.; Spehr, J.; Gietzelt, M.; Wolf, K.H.; Büsching, F.; Hülsken-Giesler, M.; et al. Monitoring systems for the support of home care. Inform. Health Soc. Care 2010, 35, 157–176. [Google Scholar] [CrossRef]
- Mulvenna, M.; Hutton, A.; Coates, V.; Martin, S.; Todd, S.; Bond, R.; Moorhead, A. Views of Caregivers on the Ethics of Assistive Technology Used for Home Surveillance of People Living with Dementia. Neuroethics 2017, 10, 255–266. [Google Scholar] [CrossRef] [PubMed]
- Alwan, M.; Dalal, S.; Mack, D.; Kell, S.; Turner, B.; Leachtenauer, J.; Felder, R. Impact of monitoring technology in assisted living: Outcome pilot. IEEE Trans. Inf. Technol. Biomed. 2006, 10, 192–198. [Google Scholar] [CrossRef]
- Bayen, E.; Jacquemot, J.; Netscher, G.; Agrawal, P.; Tabb Noyce, L.; Bayen, A. Reduction in Fall Rate in Dementia Managed Care Through Video Incident Review: Pilot Study. J. Med Internet Res. 2017, 19, e339. [Google Scholar] [CrossRef]
- East, R.; Mbabaali, S.; Sivelle, C.; Laguelle, N.; Choukou, M.-A. Unobtrusive camera-based monitoring of behavioural disturbances in patients with dementia living in long term care facilities. In Proceedings of the 11th Augmented Human International Conference, Winnipeg, MB, Canada, May 2020; Association for Computing Machinery, 2020; p. 27. [Google Scholar]
- Davis, F.D. A technology Acceptance Model for Empirically Testing New End-User Information Systems: Theory and Results; Massachussetts Institute of Technology: Cambridge, MA, USA, 1986. [Google Scholar]
- Venkatesh, V.; Davis, F.D. A Theoretical Extension of the Technology Acceptance Model: Four Longitudinal Field Studies. Manag. Sci. 2000, 46, 186–2014. [Google Scholar] [CrossRef]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User Acceptance of Information Technology: Toward a Unified View. MIS Q. 2003, 27, 425–478. [Google Scholar] [CrossRef]
- Breen, R.L. A Practical Guide to Focus-Group Research. J. Geogr. High. Educ. 2006, 30, 463–475. [Google Scholar] [CrossRef]
- Hugentobler, M. Book Reviews: Focus Groups as Qualitative Research; Morgan, D.L., Ed.; Sage Publications: Newbury Park, CA, USA, 1988; 88p. [Google Scholar]
- Krueger, R.A. (Ed.) Focus Groups: A Practical Guide for Applied Research; Sage Publications: Newbury Park, CA, USA, 1988. [Google Scholar]
- Morgan, D.L. Successful Focus Groups: Advancing the State of the Art; SAGE publications: Thousand Oaks, CA, USA, 1993; Available online: https://methods.sagepub.com/book/successful-focus-groups (accessed on 11 December 2020).
- Stewart, D.W.; Shamdasani, P. Online Focus Groups. J. Advert. 2017, 46, 48–60. [Google Scholar] [CrossRef]
- Davis, F.D. User acceptance of information technology: System characteristics, user perceptions and behavioral impacts. Int. J. Man-Mach. Stud. 1993, 38, 475–487. [Google Scholar] [CrossRef]
- Davis, F.D. Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef]
- Davis, F.D.; Bagozzi, R.P.; Warshaw, P.R. User Acceptance of Computer Technology: A Comparison of Two Theoretical Models. Manag. Sci. 1989, 35, 982–1003. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Wilkinson, A.; Kanik, M.; O’Neill, J.; Charoenkitkarn, V.; Chignell, M. Ambient Activity Technologies for Managing Responsive Behaviours in Dementia. Proc. Int. Symp. Hum. Factors Ergon. Health Care 2017, 6, 28–35. [Google Scholar] [CrossRef]
- Riva, G. Ambient Intelligence in Health Care. CyberPsychology Behav. 2003, 6, 295–300. [Google Scholar] [CrossRef]
- Martinez-Martin, N.; Luo, Z.; Kaushal, A.; Adeli, E.; Haque, A.; Kelly, S.S.; Wieten, S.; Cho, M.K.; Magnus, D.; Fei-Fei, L.; et al. Ethical issues in using ambient intelligence in health-care settings. Lancet Digit. Health 2021, 3, e115–e123. [Google Scholar] [CrossRef]

| Pseudonym | Role | Experience in the Dementia Unit |
|---|---|---|
| Olivia | Partner of a Resident | The resident has been admitted to the unit for 8 weeks |
| Emma | Social Worker | 20 years in the dementia unit and 2 years on the special needs and special needs behaviour unit |
| Ava | Nurse | Over 2 years and been to the special needs unit for over a year |
| Isabella | Health Care Aide | 22 years |
| Charlotte | Rehabilitation Assistant | 14 years working with geriatrics |
| Mia | Registered Nurse | 16.5 years on the dementia unit |
| Evelyn | Occupational Therapist | 2 years in the dementia unit and 1 year in a personal care home |
| Jessica | Recreation | 2 years in the dementia unit and 15 years in a personal care home |
| Brenda | Geriatric Care | 20 years in geriatric care and 5 years in the dementia unit |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choukou, M.-A.; Mbabaali, S.; East, R. Healthcare Professionals’ Perspective on Implementing a Detector of Behavioural Disturbances in Long-Term Care Homes. Int. J. Environ. Res. Public Health 2021, 18, 2720. https://doi.org/10.3390/ijerph18052720
Choukou M-A, Mbabaali S, East R. Healthcare Professionals’ Perspective on Implementing a Detector of Behavioural Disturbances in Long-Term Care Homes. International Journal of Environmental Research and Public Health. 2021; 18(5):2720. https://doi.org/10.3390/ijerph18052720
Chicago/Turabian StyleChoukou, Mohamed-Amine, Sophia Mbabaali, and Ryan East. 2021. "Healthcare Professionals’ Perspective on Implementing a Detector of Behavioural Disturbances in Long-Term Care Homes" International Journal of Environmental Research and Public Health 18, no. 5: 2720. https://doi.org/10.3390/ijerph18052720
APA StyleChoukou, M.-A., Mbabaali, S., & East, R. (2021). Healthcare Professionals’ Perspective on Implementing a Detector of Behavioural Disturbances in Long-Term Care Homes. International Journal of Environmental Research and Public Health, 18(5), 2720. https://doi.org/10.3390/ijerph18052720







