“People Associate Us with Movement so It’s an Awesome Opportunity”: Perspectives from Physiotherapists on Promoting Physical Activity, Exercise and Sport
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Ethical Considerations
2.3. Recruitment
2.4. Data Collection
2.5. Data Analysis
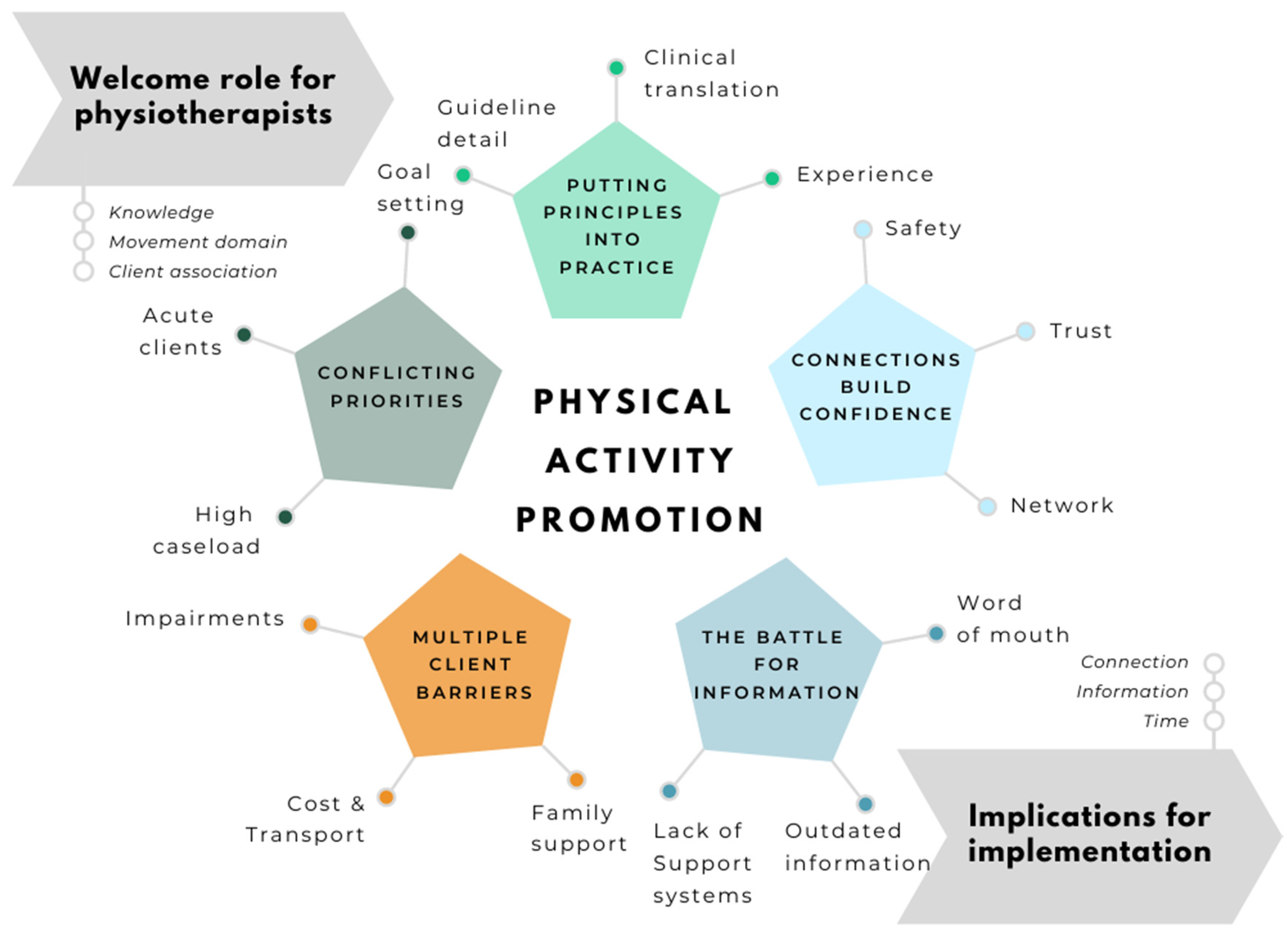
3. Results
3.1. Putting Principles into Practice
“I feel like people associate us with movement and it’s an awesome opportunity to be able to deliver that message”(P31, Paediatric acute)
“It’s just part of being a physiotherapist. We help with function, and we help with mobility, and one way to facilitate that is to tell them to do those activities, not just when they’re seeing us in hospital, but outside so they don’t come back into hospital. … We might be one of the most knowledgeable [professions] about prescribing those type of things to the patients”(P4; Adult acute)
“Oh goodness. I know it’s [recommended PA] a few hours. I think it’s like about two or three hours of physical activity, and then one hour of screen time, or something like that”(P37; Paediatric community)
“The World Health Organization saying, what? 30 min of moderate to vigorous activity to do that at least five times a week, I think”(P13; Adult Rehabilitation)
“I think the skills are developed with experience. I don’t think we teach that at Uni, and I don’t think junior physios have that when they walk straight into the job”(P3; Adult community)
“Unfortunately we don’t really follow up, give them a call further down the track to see if they followed up on that. I guess, in an ideal world, that’s what we’d like to do to ensure that that’s followed through. But, because it’s so busy, and so time constrained, it’s not something that we can do easily”(P4, Adult acute)
“[It’s about] getting people moving any way they can. So, I guess it’s going to be a little more population specific as to what you might consider appropriate... In an elderly population … I would say anything that is moving segments is general activity. Whether it’s something in the garden, or just moving off the couch, that’s something. But if you look at younger populations, usually you’re thinking sport, getting active, surfing, running, tennis, playing a sport, something like that”(P1; Adult musculoskeletal)
3.2. Working with Conflicting Priorities
“Sometimes, not always, it’s not your main focus especially when you’ve got high acuity patients and you’ve got a deteriorating chest. You’re going to prioritize that every day of the week over a sedentary person’s general exercise”(P21; Adult acute)
“as an acute physio, to get someone to adhere to that, it’s a lot of behavioural change and a lot of one-on-one working. In our workload, we see them maybe once for half an hour, maybe twice, three times and they’re discharged”(P21, Adult acute)
“…we have certain exercises that people kind of continue to do, and we have it targeted for them specifically in wanting to see how many repetitions and things they do. So it’s structuring that kind of aspect of what we do here at the hospital. I was thinking about those same kinds of things. You want instructor, whoever they might be now in a structured program to be able to kind of set up particular exercises, monitor them, monitor their progress, see if things are changing and progress”(P12; Adult Rehabilitation)
“I think that’s [promoting PA] one of the main things I try to do. I think that’s my end goal really, for my kids is to not really need the therapy but to be participating in something that it’s more fun and interests them”(P33; Paediatric musculoskeletal)
3.3. Multiple Client Barriers
“…some of our patients, their mobility is quite poor. They, usually, are accompanied by carers or family members, especially, if you have kids that are working 9–5, and they’re like, “I, honestly, don’t have the time to bring my mother in”(P17; Adult rehabilitation)
“Sometimes too it’s education... families can be almost resistant because they don’t think it [sport] will be suitable …some people, if they haven’t been exposed to it, or don’t have the education or anything, they can see it [sport] as not appropriate for a severely disabled child. Or think it’s too much for them, they’ve already got so much on their plate”(P31; Paediatric acute)
“I guess the biggest barrier is that, for clients like mine who have specific needs, there aren’t structured exercise classes…”(P3; Adult community)
3.4. Connections Build Confidence
“You have to really have that disease as a specialty and for us to feel comfortable to refer to them. We have one exercise physiologist here who specialises in cancer, which is great”(P18; Adult acute?)
“… we probably tend to refer within the district. Because we know them, we know the people who run the programs. We know exactly what they’re doing. Whereas anything outside, our kind of health bubble, it’s like we don’t know what they do. We don’t know what the quality is, what the cost is”(P12; Adult rehabilitation?)
“… here at the hospital [we] have a recreation officer. So for kids that need more specific modifications or different activities, we’ve been getting them involved more recently for things like race running and linking in with those specialised disability sporting events”(P35; Paediatric rehabilitation?)
“And I think they probably know as much about us as we know about them, as well. They probably are very unfamiliar with the services that run here at the hospital, and it’s just that how do we bridge that gap?”(P11; Adult Rehabilitation)
3.5. The Battle for Information
“...when it’s more complicated or there are disabilities involved, that’s where I think I don’t have the resources and I’d like to know more, .... I’d literally be asking around me in our department, because I know there’s people that have the answers”(P31; Paediatric acute)
“You can put it all together, but then within a couple months it can be outdated. So you know the effort to put it together and then keep it updated with all of what’s available in the community is a big task”(P8, Adult Aged Care)
“challenge is knowing what’s available to them. And I would push that back to the local therapists a lot because they know their community better”(P23; Paediatric musculoskeletal)
3.6. Implementation Strategies: Connections, Information and Time
3.6.1. An Online Information Portal:
“I think it’d be great to have a database where you could... I don’t know if it’d be a flow chart or where you can click different options and whether they’re ambulant in a wheelchair, whether they’re fragile, whether they’re disproportionate, whether they can’t fall on their head and do scrums. Where you can pick different options in there and click the area, their geographical area and a whole heap of options come up ”(P33, Paediatric musculoskeletal)
3.6.2. Forums for Connecting Physiotherapists, Community Providers and Clients:
“we’ve got groups of kids to come in, and they all try a sport together. And we’ve had some really nice feedback from those groups, where they come in, feel quite empowered, and then go out and get more linked-in with their community groups”(P27; Paediatric rehabilitation)
3.6.3. Dedicated PA Liaison Staff:
I think even the presence of a dedicated service towards that, who could do brief follow ups. And then do the legwork of providing information. Resources in the community, proper referrals to where it may ever be is a lot more efficacious than us doing it. We’re juggling a lot of balls as acute physiotherapists a lot of the time”(P21, Adult acute)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Bauman, A.E.; Grunseit, A.C.; Rangul, V.; Heitmann, B.L. Physical activity, obesity and mortality: Does pattern of physical activity have stronger epidemiological associations? BMC Public Health 2017, 17, 788. [Google Scholar] [CrossRef]
- WHO. Global Strategy and Action Plan on Ageing and Health; World Health Organization (WHO): Geneva, Switzerland, 2017. [Google Scholar]
- Zhao, M.; Veeranki, S.P.; Magnussen, C.G.; Xi, B. Recommended physical activity and all cause and cause specific mortality in US adults: Prospective cohort study. BMJ 2020, 370, m2031. [Google Scholar] [CrossRef] [PubMed]
- Ding, D.; Lawson, K.D.; Kolbe-Alexander, T.L.; Finkelstein, E.A.; Katzmarzyk, P.T.; van Mechelen, W.; Pratt, M. The economic burden of physical inactivity: A global analysis of major non-communicable diseases. Lancet 2016, 388, 1311–1324. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef] [Green Version]
- Hassett, L.; Shields, N.; Cole, J.; Owen, K.; Sherrington, C. Comparisons of leisure-time physical activity participation by adults with and without a disability: Results of an Australian cross-sectional national survey. BMJ Open Sport Exerc. Med. 2021, 7, e000991. [Google Scholar] [CrossRef]
- AIHW. Insufficient Physical Activity. 2020. Available online: https://www.aihw.gov.au/reports/risk-factors/insufficient-physical-activity/contents/insufficient-physical-activity (accessed on 18 January 2021).
- CDC. Adult Physical Inactivity Prevalence Maps by Race/Ethnicity. 2020. Available online: https://www.cdc.gov/physicalactivity/data/inactivity-prevalence-maps/ (accessed on 18 January 2021).
- BHF. Physical Inactivity. 2017. Available online: https://www.bhf.org.uk/informationsupport/risk-factors/physical-inactivity (accessed on 30 January 2021).
- Gray, M. Covid-19 will be followed by a deconditioning pandemic. BMJ Opin. 2020. Available online: https://blogs.bmj.com/bmj/2020/06/15/covid-19-will-be-followed-by-a-deconditioning-pandemic/ (accessed on 30 January 2021).
- WHO. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World; World Health Organization (WHO): Geneva, Switzerland, 2018. [Google Scholar]
- WHO. WHO Guidelines on Physical Activity and Sedentary Behaviour; World Health Organization (WHO): Geneva, Switzerland, 2020. [Google Scholar]
- WHO. Promoting Physical Activity in the Health Sector; World Health Organization (WHO) Europe: Geneva, Switzerland, 2018. [Google Scholar]
- Das, P.; Horton, R. Physical activity-time to take it seriously and regularly. Lancet 2016, 388, 1254–1255. [Google Scholar] [CrossRef]
- Gray, S.M.; McKay, H.A.; Nettlefold, L.; Race, D.; Macdonald, H.M.; Naylor, P.-J.; Sims-Gould, J. Physical activity is good for older adults-but is programme implementation being overlooked? A systematic review of intervention studies that reported frameworks or measures of implementation. Br. J. Sports Med. 2021, 55, 84–91. [Google Scholar] [CrossRef]
- Lowe, A.; Littlewood, C.; McLean, S. Understanding physical activity promotion in physiotherapy practice: A qualitative study. Musculoskelet. Sci. Pract. 2018, 35, 1–7. [Google Scholar] [CrossRef]
- Lowe, A.; Littlewood, C.; McLean, S.; Kilner, K. Physiotherapy and physical activity: A cross-sectional survey exploring physical activity promotion, knowledge of physical activity guidelines and the physical activity habits of UK physiotherapists. BMJ Open Sport Exerc. Med. 2017, 3, e000290. [Google Scholar] [CrossRef] [Green Version]
- Walkeden, S.; Walker, K.M. Perceptions of physiotherapists about their role in health promotion at an acute hospital: A qualitative study. Physiotherapy 2015, 101, 226–231. [Google Scholar] [CrossRef]
- Kunstler, B. Physical activity promotion in Australian physiotherapy practice: How do physiotherapists promote physical activity and what factors influence promotion? (PhD Academy Award). Br. J. Sports Med. 2020, 54, 306–307. [Google Scholar] [CrossRef]
- Ginis, K.A.M.; Ma, J.K.; Latimer-Cheung, A.E.; Rimmer, J.H. A systematic review of review articles addressing factors related to physical activity participation among children and adults with physical disabilities. Health Psychol. Rev. 2016, 10, 478–494. [Google Scholar] [CrossRef] [PubMed]
- Kunstler, B.; Fuller, R.; Pervan, S.; Merolli, M. Australian adults expect physiotherapists to provide physical activity advice: A survey. J. Physiother. 2019, 65, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Shirley, D.; Van Der Ploeg, H.P.; Bauman, A.E. Physical Activity Promotion in the Physical Therapy Setting: Perspectives From Practitioners and Students. Phys. Ther. 2010, 90, 1311–1322. [Google Scholar] [CrossRef] [Green Version]
- AHPRA. Physiotherapy Board of Australia Registrant Data Table - December 2019. Available online: https://www.physiotherapyboard.gov.au/About/Statistics.aspx (accessed on 30 January 2021).
- HWD. Health Workforce Data Physiotherapy 2019. 2019. Available online: https://hwd.health.gov.au/assets/Physiotherapist%202019.pdf (accessed on 30 January 2021).
- Brauer, S.G.; Haines, T.P.; Bew, P.G. Fostering clinician-led research. Aust. J. Physiother. 2007, 53, 143–144. [Google Scholar] [CrossRef] [Green Version]
- Moore, A.; Jull, G. More clinician led research? Man. Ther. 2013, 18, 359. [Google Scholar] [CrossRef] [PubMed]
- Skinner, E.H.; Hough, J.; Wang, Y.T.; Hough, C.R.; Southby, A.; Snowdon, D.A.; Sturgess, T.; Haines, T.P. Physiotherapy departments in Australian tertiary hospitals regularly participate in and disseminate research results despite a lack of allocated staff: A prospective cross-sectional survey. Physiother. Theory Pract. 2015, 31, 200–206. [Google Scholar] [CrossRef]
- Wenke, R.; Mickan, S. The role and impact of research positions within health care settings in allied health: A systematic review. BMC Health Serv. Res. 2016, 16, 355. [Google Scholar] [CrossRef]
- Morgan, D.L.; Krueger, R.A. When to Use Focus Groups and Why. In Successful Focus Groups: Advancing the State of the Art; Morgan, D.L., Ed.; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 1993; pp. 3–19. [Google Scholar]
- Litosseliti, L. Using Focus Groups in Research; Continuum Research Methods Series; Continuum: London, UK, 2003. [Google Scholar]
- Plummer, P. Focus group methodology. Part 1: Design considerations. Int. J. Ther. Rehabil. 2017, 24, 297–301. [Google Scholar] [CrossRef]
- Bradshaw, C.; Atkinson, S.; Doody, O. Employing a Qualitative Description Approach in Health Care Research. Glob. Qual. Nurs. Res. 2017, 4, 2333393617742282. [Google Scholar] [CrossRef] [Green Version]
- Maxwell, J.A. A Realist Approach for Qualitative Research; SAGE: Thousand Oaks, CA, USA, 2012. [Google Scholar]
- Kaushik, V.; Walsh, C.A. Pragmatism as a research paradigm and its implications for social work research. Soc. Sci. 2019, 8, 255. [Google Scholar] [CrossRef]
- Palys, T. Purposive Sampling. In The SAGE Encyclopedia of Qualitative Research Methods; Given, L.M., Ed.; SAGE Publications: Thousand Oaks, CA, USA, 2008; p. 698. [Google Scholar]
- Malterud, K.; Siersma, V.D.; Guassora, A.D. Sample Size in Qualitative Interview Studies: Guided by Information Power. Qual. Health Res. 2015, 26, 1753–1760. [Google Scholar] [CrossRef]
- Varpio, L.; Ajjawi, R.; Monrouxe, L.V.; O’Brien, B.C.; Rees, C.E. Shedding the cobra effect: Problematising thematic emergence, triangulation, saturation and member checking. Med. Educ. 2017, 51, 40–50. [Google Scholar] [CrossRef] [PubMed]
- Guest, G.; Namey, E.; McKenna, K. How Many Focus Groups Are Enough? Building an Evidence Base for Nonprobability Sample Sizes. Field Methods 2016, 29, 3–22. [Google Scholar] [CrossRef]
- QSR International Pty Ltd. NVivo Qualitative Data Analysis Software: Version NVivo12; QSR International Pty Ltd.: Chadstone, Australia, 2018. [Google Scholar]
- Heritage, J. Conversation analysis and institutional talk. In Handbook of Language and Social Interaction; Fitch, K.L., Sanders, R.E., Eds.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 2005; pp. 103–147. [Google Scholar]
- Sandelowski, M. What’s in a name? Qualitative description revisited. Res. Nurs. Health 2010, 33, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Sandelowski, M. Whatever Happened to Qualitative Description? Res. Nurs. Health 2000, 23, 334–340. [Google Scholar] [CrossRef]
- Miles, M.B.; Huberman, A.M. Qualitative Data Analysis: An Expanded Sourcebook, 2nd ed.; SAGE: Thousands Oaks, CA, USA, 1994. [Google Scholar]
- Smith, B.; McGannon, K.R. Developing rigor in qualitative research: Problems and opportunities within sport and exercise psychology. Int. Rev. Sport Exerc. Psychol. 2018, 11, 101–121. [Google Scholar] [CrossRef]
- Doody, O.; Slevin, E.; Taggart, L. Focus group interviews part 3: Analysis. Br. J. Nurs. 2013, 22, 266–269. [Google Scholar] [CrossRef] [Green Version]
- Thorne, S. Interpretive Description; Left Coast Press: Walnut Creek, CA, USA, 2008; Volume 2. [Google Scholar]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Freene, N.; Cools, S.; Bissett, B. Are we missing opportunities? Physiotherapy and physical activity promotion: A cross-sectional survey. BMC Sports Sci. Med. Rehabil. 2017, 9, 19. [Google Scholar] [CrossRef] [PubMed]
- Martin Ginis, K.A.; West, C.R. From guidelines to practice: Development and implementation of disability-specific physical activity guidelines. Disabil. Rehabil. 2020, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Soper, A.K.; Cross, A.; Rosenbaum, P.; Gorter, J.W. Exploring the international uptake of the “F-words in childhood disability”: A citation analysis. Child Care Health Dev. 2019, 45, 473–490. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, P.; Gorter, J.W. The ‘F-words’ in childhood disability: I swear this is how we should think. Child Care Health Dev. 2012, 38, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Devereux-Fitzgerald, A.; Powell, R.; Dewhurst, A.; French, D.P. The acceptability of physical activity interventions to older adults: A systematic review and meta-synthesis. Soc. Sci. Med. 2016, 158, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Zubala, A.; MacGillivray, S.; Frost, H.; Kroll, T.; Skelton, D.A.; Gavine, A.; Gray, N.M.; Toma, M.; Morris, J. Promotion of physical activity interventions for community dwelling older adults: A systematic review of reviews. PLoS ONE 2017, 12, e0180902. [Google Scholar] [CrossRef]
- Goodgold, S. Wellness promotion beliefs and practices of pediatric physical therapists. Pediatr. Phys. Ther. 2005, 17, 148–157. [Google Scholar] [CrossRef]
- Shields, N.; Synnot, A. Perceived barriers and facilitators to participation in physical activity for children with disability: A qualitative study. BMC Pediatr. 2016, 16, 1–10. [Google Scholar] [CrossRef] [Green Version]
| Characteristic | n | % of Participants | |
|---|---|---|---|
| Total Participants | 39 | ||
| Gender | Male | 13 | 33 |
| Female | 26 | 67 | |
| Years of Experience | 0–2 | 4 | 10 |
| 3–5 | 10 | 26 | |
| 6–10 | 8 | 21 | |
| 11–20 | 10 | 26 | |
| >20 years | 7 | 18 | |
| Work Setting/Clinical area * | Aged Care | 3 | 8 |
| Neurology/rehabilitation | 17 | 44 | |
| Tertiary paediatrics | 13 | 33 | |
| Community | 5 | 13 | |
| Outpatients/musculoskeletal | 9 | 23 | |
| Acute inpatients | 8 | 21 | |
| Client Age | Paediatric | 17 | 44 |
| Adult | 22 | 56 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
West, K.; Purcell, K.; Haynes, A.; Taylor, J.; Hassett, L.; Sherrington, C. “People Associate Us with Movement so It’s an Awesome Opportunity”: Perspectives from Physiotherapists on Promoting Physical Activity, Exercise and Sport. Int. J. Environ. Res. Public Health 2021, 18, 2963. https://doi.org/10.3390/ijerph18062963
West K, Purcell K, Haynes A, Taylor J, Hassett L, Sherrington C. “People Associate Us with Movement so It’s an Awesome Opportunity”: Perspectives from Physiotherapists on Promoting Physical Activity, Exercise and Sport. International Journal of Environmental Research and Public Health. 2021; 18(6):2963. https://doi.org/10.3390/ijerph18062963
Chicago/Turabian StyleWest, Kerry, Kate Purcell, Abby Haynes, Jennifer Taylor, Leanne Hassett, and Catherine Sherrington. 2021. "“People Associate Us with Movement so It’s an Awesome Opportunity”: Perspectives from Physiotherapists on Promoting Physical Activity, Exercise and Sport" International Journal of Environmental Research and Public Health 18, no. 6: 2963. https://doi.org/10.3390/ijerph18062963






