Adolescents’ Bipolar Experiences and Suicide Risk: Well-being and Mental Health Difficulties as Mediators
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instruments
2.3. Procedure
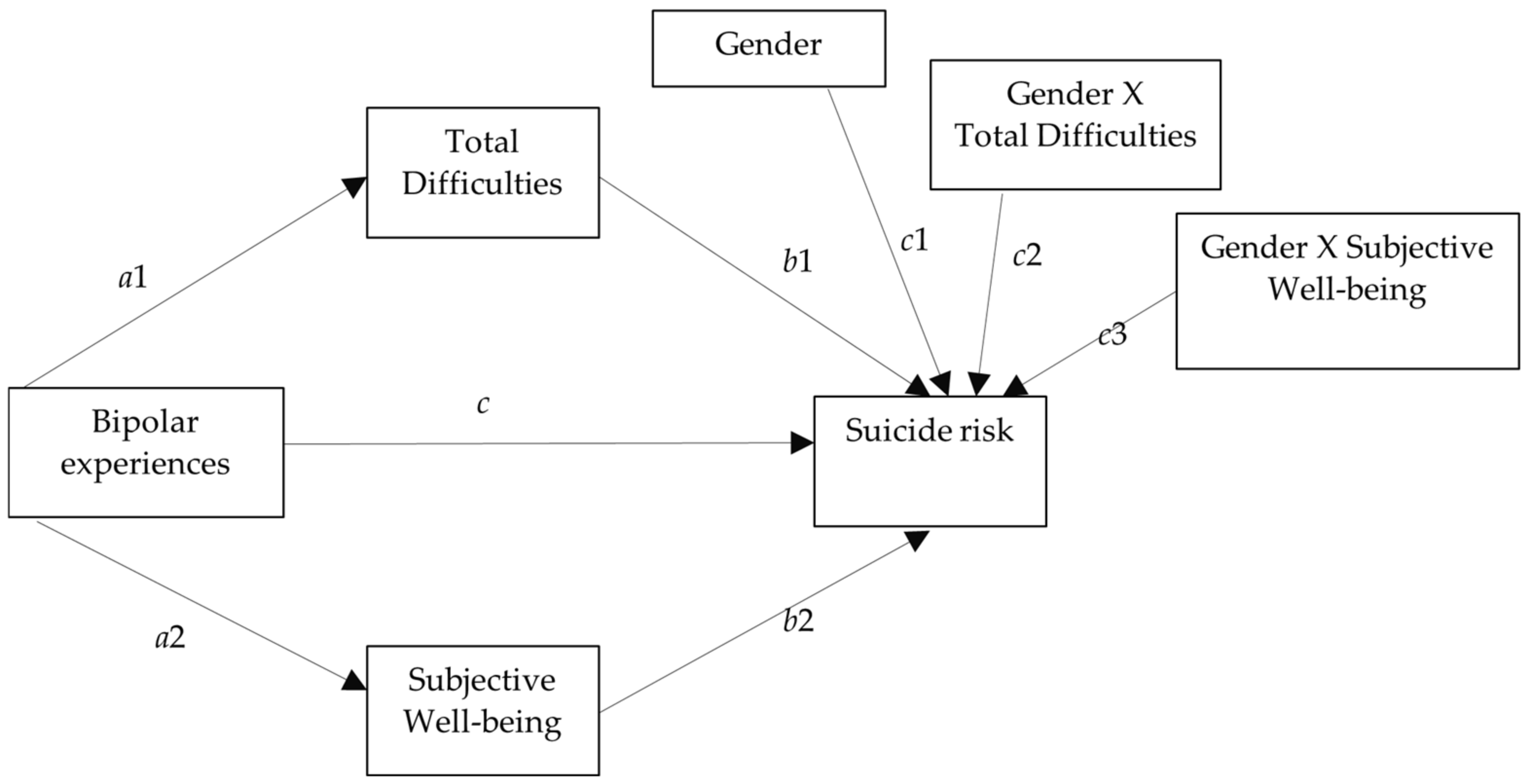
2.4. Data Analysis
3. Results
3.1. Preliminary Analysis
3.2. Mediation Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Faedda, G.L.; Serra, G.; Marangoni, C.; Salvatore, P.; Sani, G.; Vázquez, G.H.; Tondo, L.; Girardi, P.; Baldessarini, R.J.; Koukopoulos, A. Clinical risk factors for bipolar disorders: A systematic review of prospective studies. J. Affect. Disord. 2014, 168, 314–321. [Google Scholar] [CrossRef]
- Pettersson, E.; Lahey, B.B.; Larsson, H.; Lichtenstein, P. Criterion validity and utility of the general factor of psychopathology in childhood: Predictive associations with independently measured severe adverse mental health outcomes in adolescence. J. Am. Acad. Child Psychiatry 2018, 57, 372–383. [Google Scholar] [CrossRef]
- World Health Organization. Public Health Action for the Prevention of Suicide: A Framework; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Cotter, P.; Kaess, M.; Corcoran, P.; Parzer, P.; Brunner, R.; Keeley, H.; Carli, V.; Wasserman, C.; Hoven, C.; Sarchiapone, M.; et al. Help–seeking behaviour following school–based screening for current suicidality among European adolescents. Soc. Psychiatry Psychiatr. Epidemiol. 2015, 50, 973–982. [Google Scholar] [CrossRef] [PubMed]
- Barzilay, S.; Feldman, D.; Snir, A.; Apter, A.; Carli, V.; Hoven, C.W.; Wasserman, C.; Sarchiapone, M.; Wasserman, D. The interpersonal theory of suicide and adolescent suicidal behavior. J. Affect. Disord. 2015, 183, 68–74. [Google Scholar] [CrossRef]
- Nock, M.K.; Green, J.G.; Hwang, I.; McLaughlin, K.A.; Sampson, N.A.; Zaslavsky, A.M.; Kessler, R.C. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry 2013, 70, 300–310. [Google Scholar] [CrossRef] [Green Version]
- Barzilay, S.; Apter, A. Predictors of suicide in adolescents and adults with mood and common comorbid disorders. Neuropsychiatry 2014, 4, 81–93. [Google Scholar] [CrossRef]
- Buchman-Schmitt, J.M.; Brislin, S.J.; Venables, N.C.; Joiner, T.E.; Patrick, C.J. Trait liabilities and specific promotive processes in psychopathology: The example of suicidal behavior. J. Affect. Disord. 2017, 216, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Bachmann, S. Epidemiology of suicide and the psychiatric perspective. Int. J. Environ. Res. Public Health 2018, 15, 1425. [Google Scholar] [CrossRef] [Green Version]
- Miranda-Mendizabal, A.; Castellví, P.; Parés-Badell, O.; Alayo, I.; Almenara, J.; Alonso, I.; Blasco, M.J.; Cebrià, A.; Gabilondo, A.; Gili, M.; et al. Gender differences in suicidal behavior in adolescents and young adults: Systematic review and meta-analysis of longitudinal studies. Int. J. Public Health 2019, 64, 265–283. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rubin, K.H.; Bukowski, W.; Parker, J. Peer interactions, relationships, and groups. In Handbook of Child Psychology: Social, Emotional, and Personality Development; Eisenberg, N., Ed.; Wiley: New York, NY, USA, 2006; Volume 6, pp. 571–645. [Google Scholar]
- Lam, C.B.; McHale, S.M.; Crouter, A.C. Time with peers from middle childhood to late adolescence: Developmental course and adjustment correlates. Child Dev. 2014, 85, 1677–1693. [Google Scholar] [CrossRef] [Green Version]
- Escobar, D.F.S.S.; Jesus, T.F.; Noll, P.R.S.; Noll, M. Family and School Context: Effects on the Mental Health of Brazilian Students. Int. J. Environ. Res. Public Health 2020, 17, 6042. [Google Scholar] [CrossRef]
- Blakemore, S.J.; Mills, K.L. Is adolescence a sensitive period for sociocultural processing? Annu. Rev. Psychol. 2014, 65, 187–207. [Google Scholar] [CrossRef]
- Escobar, D.F.S.S.; Noll, P.R.S.; Jesus, T.F.; Noll, M. Assessing the Mental Health of Brazilian Students Involved in Risky Behaviors. Int. J. Environ. Res. Public Health 2020, 17, 3647. [Google Scholar] [CrossRef]
- Kretschmer, T. What explains correlates of peer victimization? A systematic review of mediating factors. Adolesc. Res. Rev. 2016, 1, 341–356. [Google Scholar] [CrossRef] [Green Version]
- Van Geel, M.; Vedder, P.; Tanilon, J. Relationship between peer victimization, cyberbullying, and suicide in children and adolescents: A meta–analysis. JAMA Pediatr. 2014, 168, 435–442. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Balazs, J.; Miklosi, M.; Halasz, J.; Horváth, L.O.; Szentiványi, D.; Vida, P. Suicidal risk, psychopathology, and quality of life in a clinical population of adolescents. Front. Psychiatry 2018, 9, 17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cui, Y.; Li, F.; Leckman, J.F.; Guo, L.; Ke, X.; Liu, J.; Zheng, Y.; Li, Y. The prevalence of behavioral and emotional problems among Chinese school children and adolescents aged 6–16: A national survey. Eur. Child Adolesc. Psychiatry 2020, 1–9. [Google Scholar] [CrossRef]
- Pathak, R.; Sharma, R.C.; Parvan, U.C.; Gupta, B.P.; Ojha, R.K.; Goel, N.K. Behavioural and emotional problems in school going adolescents. Australas. Med. J. 2011, 4, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Vanaelst, B.; De Vriendt, T.; Ahrens, W.; Bammann, K.; Hadjigeorgiou, C.; Konstabel, K.; Lissner, L.; Michels, N.; Molnar, D.; Moreno, L.A.; et al. Prevalence of psychosomatic and emotional symptoms in European school-aged children and its relationship with childhood adversities: Results from the IDEFICS study. Eur. Child Adolesc. Psychiatry 2012, 21, 253–265. [Google Scholar] [CrossRef] [PubMed]
- Merikangas, K.R.; He, J.P.; Burstein, M.; Swanson, S.A.; Avenevoli, S.; Cui, L.; Benjet, C.; Georgiades, K.; Swendsen, J. Lifetime prevalence of mental disorders in US adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS–A). J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 980–989. [Google Scholar] [CrossRef] [Green Version]
- Ortuño-Sierra, J.; Aritio-Solana, R.; Fonseca-Pedrero, E. Mental health difficulties in children and adolescents: The study of the SDQ in the Spanish National Health Survey 2011–2012. Psychiatry Res. 2018, 259, 236–242. [Google Scholar] [CrossRef] [PubMed]
- Althoff, R.R.; Verhulst, F.C.; Rettew, D.C.; Hudziak, J.J.; van der Ende, J. Adult outcomes of childhood dysregulation: A 14-year follow-up study. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 1105–1116. [Google Scholar] [CrossRef] [PubMed]
- Holtmann, M.; Buchmann, A.F.; Esser, G.; Schmidt, M.H.; Banaschewski, T.; Laucht, M. The Child Behavior Checklist-Dysregulation Profile predicts substance use, suicidality, and functional impairment: A longitudinal analysis. J. Child Psychol. Psychiatry 2011, 52, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Mohammadzadeh, A.; Ganji, Z.; Khosravani, V.; Ardakan, A.M.; Amirinezhad, A. Direct and indirect associations between perception of childhood trauma and suicidal ideation through emotion dysregulation in males who use heroin. Addict. Behav. 2019, 106011. [Google Scholar] [CrossRef]
- Neacsiu, A.D.; Fang, C.M.; Rodriguez, M.; Rosenthal, M.Z. Suicidal behavior and problems with emotion regulation. Suicide Life-Threat. Behav. 2018, 48, 52–74. [Google Scholar] [CrossRef]
- Pisetsky, E.M.; Haynos, A.F.; Lavender, J.M.; Crow, S.J.; Peterson, C.B. Associations between emotion regulation difficulties, eating disorder symptoms, non-suicidal self-injury, and suicide attempts in a heterogeneous eating disorder sample. Compr. Psychiatry 2017, 73, 143–150. [Google Scholar] [CrossRef] [Green Version]
- Bridge, J.A.; Reynolds, B.; McBee-Strayer, S.M.; Sheftall, A.H.; Ackerman, J.; Stevens, J.; Mendoza, K.; Campo, J.V.; Brent, D.A. Impulsive aggression, delay discounting, and adolescent suicide attempts: Effects of current psychotropic medication use and family history of suicidal behavior. J. Child Adolesc. Psychopharmacol. 2015, 25, 114–123. [Google Scholar] [CrossRef] [Green Version]
- Perez, N.M.; Jennings, W.G.; Piquero, A.R.; Baglivio, M.T. Adverse childhood experiences and suicide attempts: The mediating influence of personality development and problem behaviors. J. Youth Adolesc. 2016, 45, 1527–1545. [Google Scholar] [CrossRef] [PubMed]
- Felitti, V.J.; Anda, R.F.; Nordenberg, D.; Williamson, D.F.; Spitz, A.M.; Edwards, V.; Koss, M.P.; Marks, J.S. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. Am. J. Prev. Med. 2019, 56, 774–786. [Google Scholar] [CrossRef]
- O’Connor, R.C.; Nock, M.K. The psychology of suicidal behaviour. Lancet Psychiatry 2014, 1, 73–85. [Google Scholar] [CrossRef]
- O’Connor, R.; Platt, S.; Gordon, J. (Eds.) Introduction. In International Handbook of Suicide Prevention: Research, Policy and Practice; Wiley Blackwell: Hoboken, NJ, USA, 2011; pp. 1–6. [Google Scholar]
- Turecki, G.; Brent, D.A. Suicide and suicidal behaviour. Lancet 2016, 387, 1227–1239. [Google Scholar] [CrossRef]
- Deutz, M.H.; Geeraerts, S.B.; van Baar, A.L.; Deković, M.; Prinzie, P. The Dysregulation Profile in middle childhood and adolescence across reporters: Factor structure, measurement invariance, and links with self-harm and suicidal ideation. Eur. Child Adolesc. Psychiatry 2016, 25, 431–442. [Google Scholar] [CrossRef] [Green Version]
- Fonseca-Pedrero, E.; Inchausti, F.; Pérez-Gutierrez, L.; Aritio, R.; Ortuño-Sierra, J.; Sánchez-García, M.A.; Lucas, B.; Domínguez, M.C.; Foncea, D.; Espinosa, V.; et al. Suicidal ideation in a community-derived sample of Spanish adolescents. Rev. Psiquiatr. Salud 2018, 11, 76–85. [Google Scholar] [CrossRef]
- Hinshaw, S.P.; Owens, E.B.; Zalecki, C.; Huggins, S.P.; Montenegro-Nevado, A.J.; Schrodek, E.; Swanson, E.N. Prospective follow-up of girls with attention–deficit/hyperactivity disorder into early adulthood: Continuing impairment includes elevated risk for suicide attempts and self–injury. J. Consult. Clin. Psychiatry 2012, 80, 1041–1051. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Y.Y.; Chen, Y.L.; Gau, S.S.F. Attention–deficit hyperactivity disorder and suicidality: The mediating effects of psychiatric comorbidities and family function. J. Affect. Disord. 2019, 242, 96–104. [Google Scholar] [CrossRef] [PubMed]
- Park, N.; Peterson, C.; Seligman, M.E. Strengths of character and well-being. J. Soc. Clin. Psychol. 2004, 23, 603–619. [Google Scholar] [CrossRef] [Green Version]
- Balistreri, K.S.; Alvira-Hammond, M. Adverse childhood experiences, family functioning and adolescent health and emotional well–being. Public Health 2016, 132, 72–78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delfabbro, P.; Stevenson, J.; Malvaso, C.; Duong, D.; Winefield, H.; Winefield, A.; Hammarström, A. Who is doing well: Age 15 predictors of psychological and physical health in young adulthood? Aust. Psychol. 2019, 54, 114–124. [Google Scholar] [CrossRef]
- Khaleghinezhad, S.A.; Shabani, M.; Hakimzadeh, R.; Shaker, H.N.; Amerian, M. Prediction of high school students’ life satisfaction and academic performance based on locus of control and self-esteem. Int. J. School Health 2016, 3, e60223. [Google Scholar] [CrossRef]
- Moksnes, U.K.; Eilertsen, M.E.B.; Ringdal, R.; Bjørnsen, H.N.; Rannestad, T. Life satisfaction in association with self-efficacy and stressor experience in adolescents-self-efficacy as a potential moderator. Scand. J. Caring Sci. 2018, 33, 222–230. [Google Scholar] [CrossRef]
- Yap, S.T.; Baharudin, R. The relationship between adolescents’ perceived parental involvement, self-efficacy beliefs, and subjective well-being: A multiple mediator model. Soc. Indic. Res. 2016, 126, 257–278. [Google Scholar] [CrossRef]
- Lester, L.; Cross, D. The relationship between school climate and mental and emotional wellbeing over the transition from primary to secondary school. Psychol. Well-Being 2015, 5, 9. [Google Scholar] [CrossRef] [Green Version]
- Kjeldsen, A.; Nilsen, W.; Gustavson, K.; Skipstein, A.; Melkevik, O.; Karevold, E.B. Predicting Well-Being and Internalizing Symptoms in Late Adolescence From Trajectories of Externalizing Behavior Starting in Infancy. J. Res. Adolesc. 2016, 26, 991–1008. [Google Scholar] [CrossRef] [PubMed]
- Heizomi, H.; Allahverdipour, H.; Jafarabadi, M.A.; Safaian, A. Happiness and its relation to psychological well-being of adolescents. Asian J. Psychiatry 2015, 16, 55–60. [Google Scholar] [CrossRef]
- Rebellon, C.; Brown, J.; Keyes, C.L.M. Mental illness and suicide. In The Encyclopedia of Criminology and Deviant Behavior; Bryant, C.D., Ed.; Routledge: Philadelphia, PA, USA, 2000; Volume 4, pp. 426–429. [Google Scholar]
- Richardson, B.; Fuller-Tyszkiewicz, M.D.; Tomyn, A.J.; Cummins, R.A. The psychometric equivalence of the Personal Wellbeing Index for normally functioning and homeostatically defeated Australian adults. J. Happiness Stud. 2015, 17, 627–641. [Google Scholar] [CrossRef]
- Sharma, S.; Tomer, S. Psychosocial antecedents of prosocial behavior and its relationship with subjective well-being in adolescents. Indian J. Posit. Psychol. 2018, 9, 14–21. [Google Scholar] [CrossRef]
- Callaghan, T.; Corbit, J. Early prosocial development across cultures. Curr. Opin. Psychol. 2018, 20, 102–106. [Google Scholar] [CrossRef]
- Klein, N.; Grossman, I.; Uskul, A.K.; Kraus, A.; Epley, N. It pays to be nice, but not really nice: Asymmetric evaluations of prosociality across seven cultures. Judgm. Decis. Mak. 2015, 10, 355–364. [Google Scholar]
- Snippe, E.; Jeronimus, B.F.; Aan het Rot, M.; Bos, E.H.; de Jonge, P.; Wichers, M. The reciprocity of prosocial behavior and positive affect in daily life. J. Pers. 2018, 86, 139–146. [Google Scholar] [CrossRef]
- Van Hoorn, J.; van Dijk, E.; Meuwese, R.; Rieffe, C.; Crone, E.A. Peer influence on prosocial behavior in adolescence. J. Res. Adolesc. 2016, 26, 90–100. [Google Scholar] [CrossRef]
- Padilla-Walker, L.M.; Carlo, G.; Nielson, M.G. Does helping keep teens protected? Longitudinal bidirectional relations between prosocial behavior and problem behavior. Child Dev. 2015, 86, 1759–1772. [Google Scholar] [CrossRef]
- Palmier-Claus, J.E.; Taylor, P.J.; Varese, F.; Pratt, D. Does unstable mood increase risk of suicide? Theory, research and practice. J. Affect. Disord. 2012, 143, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Hauser, M.; Galling, B.; Correll, C.U. Suicidal ideation and suicide attempts in children and adolescents with bipolar disorder: A systematic review of prevalence and incidence rates, correlates, and targeted interventions. Bipolar Disord. 2013, 15, 507–523. [Google Scholar] [CrossRef] [Green Version]
- Goldstein, T.R.; Ha, W.; Axelson, D.A.; Goldstein, B.I.; Liao, F.; Gill, M.K.; Ryan, N.D.; Yen, S.; Hunt, J.; Hower, H.; et al. Predictors of prospectively examined suicide attempts among youth with bipolar disorder. Arch. Gen. Psychiatry 2012, 69, 1113–1122. [Google Scholar] [CrossRef] [Green Version]
- Antypa, N.; Antonioli, M.; Serretti, A. Clinical, psychological and environmental predictors of prospective suicide events in patients with Bipolar Disorder. J. Psychiatr. Res. 2013, 47, 1800–1808. [Google Scholar] [CrossRef] [PubMed]
- Isometsä, E. Suicidal behaviour in mood disorders—Who, when, and why? Can. J. Psychiatry 2014, 59, 120–130. [Google Scholar] [CrossRef] [Green Version]
- Hayes, J.F.; Miles, J.; Walters, K.; King, M.; Osborn, D.P.J. A systematic review and meta-analysis of premature mortality in bipolar affective disorder. Acta Psychiatr. Scand. 2015, 131, 417–425. [Google Scholar] [CrossRef] [PubMed]
- MacKinnon, D.F.; Pies, R. Affective instability as rapid cycling: Theoretical and clinical implications for borderline personality and bipolar spectrum disorders. Bipolar Disord. 2006, 8, 1–14. [Google Scholar] [CrossRef]
- Merikangas, K.R.; Jin, R.; He, J.P.; Kessler, R.C.; Lee, S.; Sampson, N.A.; Viana, M.C.; Andrade, L.H.; Hu, C.; Karam, E.G.; et al. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch. Gen. Psychiatry 2011, 68, 241–251. [Google Scholar] [CrossRef]
- Fonseca-Pedrero, E.; Ortuno-Sierra, J.; Paino, M.; Muñiz, J. Screening the risk of bipolar spectrum disorders: Validity evidence of the Mood Disorder Questionnaire in adolescents and young adults. Rev. Psiquiatr. Salud Ment. 2016, 9, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Aragonés, E.; López-Rodríguez, J.A.; Escobar-Rabadán, F.; Téllez-Lapeira, J.; Mínguez, J.; Párraga, I.; Suárez-Hernández, T.; Piñero, M.J.; Guzón, M.M. Cribado para el trastorno bipolar en pacientes de atención primaria que presentan síntomas psicológicos. Aten. Primaria 2015, 47, 167–174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fumero, A.; Marrero, R.J.; Fonseca-Pedrero, E. Well-being in schizotypy: The effect of subclinical psychotic experiences. Psicothema 2018, 30, 177–182. [Google Scholar] [CrossRef]
- Goldstein, B.I.; Birmaher, B.; Carlson, G.A.; DelBello, M.P.; Findling, R.L.; Fristad, M.; Kowatch, R.A.; Miklowitz, D.J.; Nery, F.G.; Perez-Algorta, G.; et al. The International Society for Bipolar Disorders Task Force report on pediatric bipolar disorder: Knowledge to date and directions for future research. Bipolar Disor. 2017, 19, 524–543. [Google Scholar] [CrossRef] [Green Version]
- Goodman, R. The strengths and difficulties questionnaire: A research note. J. Child Psychol. Psychiatry 1997, 38, 581–586. [Google Scholar] [CrossRef]
- Ortuño-Sierra, J.; Fonseca-Pedrero, E.; Inchausti, F.; Sastre i Riba, S.S. Evaluación de dificultades emocionales y comportamentales en población infanto-juvenil: El cuestionario de capacidades y dificultades (SDQ). Pap. Psicólogo 2016, 37, 14–26. [Google Scholar]
- Ortuño-Sierra, J.; Fonseca-Pedrero, E.; Paino, M.; Sastre i Riba, S.S.; Muñiz, J. Screening mental health problems during adolescence: Psychometric properties of the Spanish version of the Strengths and Difficulties Questionnaire. J. Adolesc. 2015, 38, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Cummins, R.A.; Lau, A.L. Personal Wellbeing Index–School Children; Deakin University: Melbourne, Australia, 2005. [Google Scholar]
- González-Carrasco, M.; Casas, F.; Malo, S.; Viñas, F.; Dinisman, T. Changes with age in subjective well-being through the adolescent years: Differences by gender. J. Happiness Stud. 2017, 18, 63–88. [Google Scholar] [CrossRef]
- Fonseca-Pedrero, E. Bienestar Emocional en Adolescentes Riojanos; Emotional Well-Being in Adolescents of La Rioja; Universidad de La Rioja: Logroño, Spain, 2018. [Google Scholar]
- Paykel, E.S.; Myers, J.K.; Lindenthal, J.J.; Tanner, J. Suicidal feelings in the general population: A prevalence study. Br. J. Psychiatry 1974, 214, 460–469. [Google Scholar] [CrossRef]
- Hirschfeld, R.M.; Williams, J.B.; Spitzer, R.L.; Calabrese, J.R.; Flynn, L.; Keck, P.E.J.; Lewis, L.; McElroy, S.L.; Post, R.M.; Rapport, D.J.; et al. Development and validation of a screening instrument for bipolar spectrum disorder: The Mood Disorder Questionnaire. Am. J. Psychiatry 2000, 157, 1873–1875. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM–5); American Psychiatric Publishing: Arlington, UK, 2013. [Google Scholar]
- Fonseca-Pedrero, E.; Lemos-Giráldez, S.; Paino, M.; Villazón-García, U.; Muñiz, J. Validation of the Schizotypal Personality Questionnaire Brief form in adolescents. Schizophr. Res. 2009, 111, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Preacher, K.J.; Hayes, A.F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods 2008, 40, 879–891. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2016. [Google Scholar]
- Rosseel, Y. Lavaan: An R package for structural equation modeling. J. Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef] [Green Version]
- Hernández, J.A.; Betancort, M. ULLRToolbox. 2016. Available online: https://sites.google.com/site/ullrtoolbox/ (accessed on 15 March 2021).
- Bono, R.; Blanca, M.J.; Arnau, J.; Gómez-Benito, J. Non-normal distributions commonly used in health, education, and social sciences: A systematic review. Front. Psychol. 2017, 8, 1602. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maas, C.; Hox, J.J. The influence of violations of assumptions on multilevel parameter estimates and their standard errors. Comput. Stat. Data Anal. 2004, 46, 427–440. [Google Scholar] [CrossRef]
- Morrell, H.E.; Lapsley, D.K.; Halpern-Felsher, B.L. Subjective invulnerability and perceptions of tobacco-related benefits predict adolescent smoking behavior. J. Early Adolesc. 2016, 36, 679–703. [Google Scholar] [CrossRef] [Green Version]
- Barnett, J.H.; Huang, J.; Perlis, R.H.; Young, M.M.; Rosenbaum, J.F.; Nierenberg, A.A.; Sachs, A.; Nimgaonkar, V.L.; Miklowitz, D.J.; Smoller, J.W. Personality and bipolar disorder: Dissecting state and trait associations between mood and personality. Psychol. Med. 2011, 41, 1593–1604. [Google Scholar] [CrossRef] [PubMed]
- De Haan, A.; De Pauw, S.; van den Akker, A.; Deković, M.; Prinzie, P. Long-term developmental changes in children’s lower-order Big Five personality facets. J. Personal. 2017, 85, 616–631. [Google Scholar] [CrossRef] [Green Version]
- Rouquette, A.; Pingault, J.B.; Fried, E.I.; Orri, M.; Falissard, B.; Kossakowski, J.J.; Vitaro, F.; Tremblay, R.; Cote, S.M.; Borsboom, D. Emotional and behavioral symptom network structure in elementary school girls and association with anxiety disorders and depression in adolescence and early adulthood: A network analysis. JAMA Psychiatry 2018, 75, 1173–1181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uddin, R.; Burton, N.W.; Maple, M.; Khan, S.R.; Khan, A. Suicidal ideation, suicide planning, and suicide attempts among adolescents in 59 low-income and middle-income countries: A population-based study. Lancet Child Adolesc. Health 2019, 3, 223–233. [Google Scholar] [CrossRef] [Green Version]
- Jones, A.C.; Schinka, K.C.; van Dulmen, M.H.; Bossarte, R.M.; Swahn, M.H. Changes in loneliness during middle childhood predict risk for adolescent suicidality indirectly through mental health problems. J. Clin. Child Adolesc. Psychol. 2011, 40, 818–824. [Google Scholar] [CrossRef]
- Van Eck, K.; Ballard, E.; Hart, S.; Newcomer, A.; Musci, R.; Flory, K. ADHD and suicidal ideation: The roles of emotion regulation and depressive symptoms among college students. J. Atten. Disord. 2015, 19, 703–714. [Google Scholar] [CrossRef]
- Victor, S.E.; Hipwell, A.E.; Stepp, S.D.; Scott, L.N. Parent and peer relationships as longitudinal predictors of adolescent non-suicidal self-injury onset. Child Adolesc. Psychiatry Ment. Health 2019, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- Cleare, S.; Gumley, A.; O’Connor, R.C. Self-compassion, self-forgiveness, suicidal ideation and self-harm: A systematic review. Clin. Psychol. Psychother. 2019, 26, 511–530. [Google Scholar] [CrossRef]
- Lin, C.C. The effects of gratitude on suicidal ideation among late adolescence: A mediational chain. Curr. Psychol. 2019, 1–9. [Google Scholar] [CrossRef]
- Rey, L.; Quintana-Orts, C.L.; Mérida-López, S.; Extremera, N. Being Bullied at School: Gratitude as Potential Protective Factor for Suicide Risk in Adolescents. Front. Psychol. 2019, 10, 662. [Google Scholar] [CrossRef] [Green Version]
- Memmott-Elison, M.K.; Holmgren, H.G.; Padilla-Walker, L.M.; Hawkins, A.J. Associations between prosocial behavior, externalizing behaviors, and internalizing symptoms during adolescence: A meta-analysis. J. Adolesc. 2020, 80, 98–114. [Google Scholar] [CrossRef]
- Telzer, E.H.; Fuligni, A.J. Positive daily family interactions eliminate gender differences in internalizing symptoms among adolescents. J. Youth Adolesc. 2013, 42, 1498–1511. [Google Scholar] [CrossRef] [PubMed]
- Abad, J.; Forns, M.; Gómez, J. Emotional and behavioral problems as measured by the YSR: Gender and age differences in Spanish adolescents. Eur. J. Psychol. Assess. 2002, 18, 149–157. [Google Scholar] [CrossRef]
- Rocchino, G.H.; Dever, B.V.; Telesford, A.; Fletcher, K. Internalizing and externalizing in adolescence: The roles of academic self-efficacy and gender. Psychol. Schools 2017, 54, 905–917. [Google Scholar] [CrossRef]
- Muñiz, J.; Fonseca-Pedrero, E. Ten steps for test development. Psicothema 2019, 31, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Díez-Gómez, A.; Pérez-Albéniz, A.; Ortuño-Sierra, J.; Fonseca-Pedrero, E. SENTIA: An Adolescent Suicidal Behavior Assessment Scale. Psicothema 2020, 32, 382–389. [Google Scholar] [CrossRef] [PubMed]
- Seven, Ü.S.; Stoll, M.; Dubbert, D.; Kohls, C.; Werner, P.; Kalbe, E. Perception, Attitudes, and Experiences Regarding Mental Health Problems and Web Based Mental Health Information Amongst Young People with and without Migration Background in Germany. A Qualitative Study. Int. J. Environ. Res. Public Health 2021, 18, 81. [Google Scholar] [CrossRef] [PubMed]
| Predictors | Adolescents without Bipolar Experiences N = 1039 | Adolescents with Bipolar Experiences N = 467 | F | η2 | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Emotional symptoms | 3.37 | 2.43 | 4 | 2.44 | 21.04 *** | 0.014 |
| Behavioral problems | 1.68 | 1.48 | 2.59 | 1.82 | 106.95 *** | 0.066 |
| Peer problems | 1.41 | 1.53 | 1.77 | 1.61 | 17.06 *** | 0.011 |
| Hyperactivity | 4 | 2.13 | 5.03 | 2.09 | 77.39 *** | 0.049 |
| Prosocial behavior | 8.63 | 1.45 | 8.51 | 1.49 | 2.39 | - |
| Suicide risk | 0.79 | 1.25 | 1.15 | 1.45 | 21.10 *** | 0.016 |
| Subjective well-being | 55.38 | 9.17 | 54.46 | 8.61 | 3.41 * | 0.002 |
| Variables | Gender a | Age b | Suicide Risk b |
|---|---|---|---|
| Emotional symptoms | 0.33 *** | −0.004 | 0.44 *** |
| Behavioral problems | −0.07 | −0.13 ** | 0.19 *** |
| Peer problems | −0.03 | 0.03 | 0.29 *** |
| Hyperactivity | 0.05 | −0.05 | 0.18 *** |
| Total difficulties | −0.02 | 0.02 | −0.11 * |
| Subjective well-being | 0.14 ** | −0.06 | 0.46 *** |
| Prosocial behavior | −0.14 ** | −0.04 | −0.33 *** |
| Bipolar experience | −0.05 | 0.04 | 0.16 *** |
| Suicide risk | 0.10 * | −0.10 * |
| Paths between Variables | Path Symbols | Coefficient SE | p | Bootstrap 90% CI | ||
|---|---|---|---|---|---|---|
| Total difficulties | ||||||
| Bipolar experiences → Total difficulties | a1 | 0.88 | 0.17 | <0.001 | 0.600 | 1.15 |
| Bipolar experiences → Subjective well-being | a2 | −0.62 | 0.29 | <0.05 | −1.09 | −0.14 |
| Total difficulties → Suicide risk | b1 | 0.10 | 0.01 | <0.001 | 0.08 | 0.12 |
| Subjective well-being → Suicide risk | b2 | −0.03 | 0.01 | <0.001 | −0.05 | 0.02 |
| Bipolar experiences → Suicide risk | c | 0.06 | 0.05 | 0.20 | −0.02 | 0.14 |
| Gender → Suicide risk | c1 | 0.01 | 0.12 | 0.92 | −0.19 | 0.21 |
| Gender X Total difficulties → Suicide risk | c2 | 0.01 | 0.03 | 0.63 | −0.03 | 0.06 |
| Gender X Subjective well-being → Suicide risk | c3 | −0.01 | 0.02 | 0.78 | −0.03 | 0.02 |
| Age (covariate) | −0.10 | 0.05 | <0.05 | −0.18 | −0.03 | |
| R2 = 0.21 | <0.001 | |||||
| Emotional symptoms | ||||||
| Bipolar experiences → Emotional symptoms | a1 | 0.17 | 0.07 | <0.05 | 0.05 | 0.29–0.15 |
| Bipolar experiences → Subjective well-being | a2 | −0.62 | 0.28 | <0.05 | −1.07 | 0.27 |
| Emotional symptoms → Suicide risk | b1 | 0.22 | 0.03 | <0.001 | 0.18 | −0.02 |
| Subjective well-being → Suicide risk | b2 | −0.04 | 0.01 | <0.05 | −0.05 | 0.19 |
| Bipolar experiences → Suicide risk | c | 0.11 | 0.05 | 0.08 | 0.02 | −0.01 |
| Gender → Suicide risk | c1 | −0.21 | 0.12 | 0.23 | −0.41 | 0.03 |
| Gender X Emotional symptoms→ Suicide risk | c2 | −0.07 | 0.06 | 0.47 | −0.16 | 0.02 |
| Gender X Subjective well-being → Suicide risk | c3 | −0.01 | 0.02 | <0.01 | −0.04 | −0.06 |
| Age (covariate) | −0.13 | 0.04 | <0.001 | −0.20 | ||
| R2 = 0.24 | ||||||
| Behavioral problems | ||||||
| Bipolar experiences → Behavioral problems | a1 | 0.17 | 0.07 | <0.05 | 0.05 | 0.29 |
| Bipolar experiences → Subjective well-being | a2 | −0.62 | 0.28 | <0.05 | −1.07 | −0.15 |
| Behavioral Problems → Suicide risk | b1 | 0.22 | 0.03 | <0.001 | 0.18 | 0.27 |
| Subjective well-being → Suicide risk | b2 | −0.04 | 0.01 | <0.001 | −0.05 | −0.02 |
| Bipolar experiences → Suicide risk | c | 0.11 | 0.05 | <0.05 | 0.02 | 0.19 |
| Gender → Suicide risk | c1 | −0.21 | 0.12 | 0.08 | −0.41 | −0.01 |
| Gender X Behavioral Problems → Suicide risk | c2 | −0.07 | 0.06 | 0.23 | −0.16 | 0.03 |
| Gender X Subjective well-being → Suicide risk | c3 | −0.01 | 0.02 | 0.47 | −0.04 | 0.02 |
| Age (covariate) | −0.13 | 0.04 | <0.01 | −0.20 | −0.06 | |
| R2 = 0.24 | <0.05 | |||||
| Peer problems | ||||||
| Bipolar experiences → Peer problems | a1 | 0.17 | 0.06 | <0.01 | 0.07 | 0.27 |
| Bipolar experiences → Subjective well-being | a2 | −0.62 | 0.29 | <0.05 | −1.09 | −0.14 |
| Peer problems → Suicide risk | b1 | 0.21 | 0.05 | <0.001 | 0.13 | 0.29 |
| Subjective well-being → Suicide risk | b2 | −0.04 | 0.01 | <0.001 | −0.05 | −0.03 |
| Bipolar experiences → Suicide risk | c | 0.11 | 0.05 | <0.05 | 0.03 | 0.19 |
| Gender → Suicide risk | c1 | 0.15 | 0.13 | 0.24 | −0.06 | 0.35 |
| Gender X Peer problems→ Suicide risk | c2 | 0.07 | 0.10 | 0.47 | −0.10 | 0.24 |
| Gender X Subjective well-being → Suicide risk | c3 | −0.01 | 0.02 | 0.80 | −0.03 | 0.02 |
| Age (covariate) | −0.14 | 0.05 | <0.01 | −0.21 | −0.06 | |
| R2 = 0.16 | <0.001 | |||||
| Hyperactivity | ||||||
| Bipolar experiences → Hyperactivity | a1 | 0.34 | 0.06 | <0.001 | 0.24 | 0.44 |
| Bipolar experiences → Subjective well-being | a2 | −0.62 | 0.28 | <0.05 | −1.08 | −0.15 |
| Hyperactivity → Suicide risk | b1 | 0.08 | 0.03 | <0.01 | 0.03 | 0.12 |
| Subjective well-being → Suicide risk | b2 | −0.05 | 0.01 | <0.001 | −0.07 | −0.04 |
| Bipolar experiences → Suicide risk | c | 0.12 | 0.05 | <0.5 | 0.03 | 0.20 |
| Gender → Suicide risk | c1 | 0.10 | 0.13 | 0.43 | −0.11 | 0.31 |
| Gender X Hyperactivity → Suicide risk | c2 | −0.02 | 0.06 | 0.80 | −0.12 | 0.09 |
| Gender X Subjective well-being → Suicide risk | c3 | −0.02 | 0.02 | 0.31 | −0.05 | 0.01 |
| Age (covariate) | −0.13 | 0.04 | <0.01 | −0.20 | −0.05 | |
| R2 = 0.16 | <0.001 | |||||
| Prosocial behavior | ||||||
| Bipolar experiences → Prosocial behavior | a1 | −0.09 | 0.05 | 0.10 | −0.17 | |
| Bipolar experiences → Subjective well-being | a2 | −0.62 | 0.29 | <0.05 | −1.09 | −0.13 |
| Prosocial behavior → Suicide risk | b1 | −0.04 | 0.05 | 0.43 | −0.11 | 0.04 |
| Subjective well-being → Suicide risk | b2 | −0.05 | 0.01 | <0.001 | −0.07 | −0.04 |
| Bipolar experiences → Suicide risk | c | 0.14 | 0.05 | <0.01 | 0.05 | 0.22 |
| Gender → Suicide risk | c1 | 0.12 | 0.13 | 0.35 | −0.09 | 0.33 |
| Gender X Prosocial behavior → Suicide risk | c2 | 0.02 | 0.10 | 0.88 | −0.15 | 0.18 |
| Gender X Subjective well-being → Suicide risk | c3 | −0.02 | 0.02 | 0.26 | −0.05 | 0.01 |
| Age (covariate) | −0.13 | 0.05 | <0.01 | −0.21 | −0.06 | |
| R2 = 0.15 | <0.001 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fumero, A.; Marrero, R.J.; Pérez-Albéniz, A.; Fonseca-Pedrero, E. Adolescents’ Bipolar Experiences and Suicide Risk: Well-being and Mental Health Difficulties as Mediators. Int. J. Environ. Res. Public Health 2021, 18, 3024. https://doi.org/10.3390/ijerph18063024
Fumero A, Marrero RJ, Pérez-Albéniz A, Fonseca-Pedrero E. Adolescents’ Bipolar Experiences and Suicide Risk: Well-being and Mental Health Difficulties as Mediators. International Journal of Environmental Research and Public Health. 2021; 18(6):3024. https://doi.org/10.3390/ijerph18063024
Chicago/Turabian StyleFumero, Ascensión, Rosario J. Marrero, Alicia Pérez-Albéniz, and Eduardo Fonseca-Pedrero. 2021. "Adolescents’ Bipolar Experiences and Suicide Risk: Well-being and Mental Health Difficulties as Mediators" International Journal of Environmental Research and Public Health 18, no. 6: 3024. https://doi.org/10.3390/ijerph18063024






