EmERGE mHealth Platform: Implementation and Technical Evaluation of a Digital Supported Pathway of Care for Medically Stable HIV
Abstract
1. Introduction
2. Materials and Methods
2.1. Technology Used
2.2. EmERGE Platform Development Methodology
2.3. EmERGE Platform Evaluation Methodology
- I think that I would like to use this system frequently.
- I found the system unnecessarily complex.
- I thought the system was easy to use.
- I think that I would need the support of a technical person to be able to use this system.
- I found the various functions in this system were well-integrated.
- I thought there was too much inconsistency in this system.
- I would imagine that most people would learn to use this system very quickly.
- I found the system very cumbersome to use.
- I felt very confident using the system.
- I needed to learn a lot of things before I could get going with this system.
- “How would you rate your overall satisfaction with the EmERGE service?” (Excellent/Good/Satisfactory/Poor/Very poor).
- “Would you recommend the EmERGE service to a friend?” (Yes/No).
3. Results
3.1. EmERGE Platform Specification
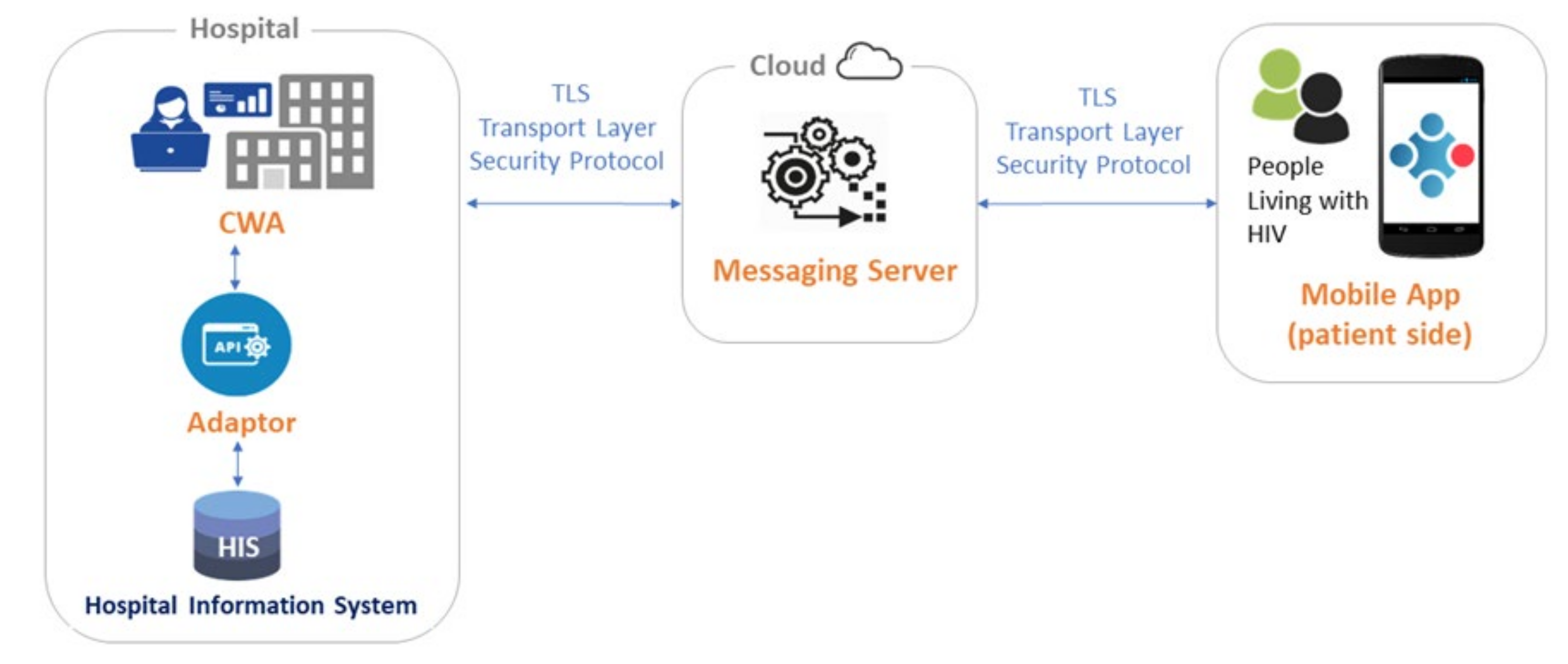
3.2. Architecture
3.3. User Interfaces and Graphical Design
3.4. Security and Privacy
3.5. Evaluation of the EmERGE platform
3.5.1. Usage Data
3.5.2. Impact on Acceptability and Usability
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- eHealth Action Plan 2012–2020-Innovative Healthcare for the 21st Century. Communication from the Commission to the European Parliament, the Council, the European Economic and Social Committee and the Committee of the Regions. Available online: https://ec.europa.eu/digital-single-market/en/news/ehealth-action-plan-2012-2020-innovative-healthcare-21st-century#:~:text=The%20European%20Commission’s%20eHealth%20Action,and%20patient%2Dcentred%20health%20services (accessed on 9 February 2021).
- Sim, I. Mobile Devices and Health. N. Engl. J. Med. 2019, 381, 956–968. [Google Scholar] [CrossRef]
- Whitehead, L.; Seaton, P. The Effectiveness of Self-Management Mobile Phone and Tablet Apps in Long-term Condition Management: A Systematic Review. J. Med. Internet Res. 2016, 18, e97. [Google Scholar] [CrossRef]
- Lee, J.A.; Choi, M.; Lee, S.A.; Jiang, N. Effective behavioral intervention strategies using mobile health applications for chronic disease management: A systematic review. BMC Med. Inform. Decis. Mak. 2018, 18, 12. [Google Scholar] [CrossRef]
- Siddiqui, J.; Herchline, T.; Kahlon, S.; Moyer, K.; Scott, J.; Wood, B.; Young, J. Infectious Diseases Society of America Position Statement on Telehealth and Telemedicine as Applied to the Practice of Infectious Diseases. Clin. Infect. Dis. 2017, 64, 237–242. [Google Scholar] [CrossRef]
- WHO. Global Diffusion of eHealth: Making Universal Health Coverage Achievable. Report of the Third Global Survey on eHealth; World Health Organization: Geneva, Switzerland, 2016; ISBN 978-92-4-151178-0. [Google Scholar]
- EU4Health 2021–2027–a Vision for a Healthier European Union. Available online: https://ec.europa.eu/health/funding/eu4health_en (accessed on 9 February 2021).
- Europe mHealth Market Research Report. Available online: https://www.marketdataforecast.com/market-reports/europe-mobile-health-market (accessed on 9 February 2021).
- Retention Rate on Day 1 and Day 30 of Mobile App Installs Worldwide as of August 2020, by Category. Available online: https://www.statista.com/statistics/259329/ios-and-android-app-user-retention-rate/ (accessed on 9 February 2021).
- Patient Adoption of mHealth. Use, Evidence and Remaining Barriers to Mainstream Acceptance; IMS Institute for Healthcare Informatics: Parsippany, NJ, USA, 2015. [Google Scholar]
- Leigh, S.; Ashall-Payne, L. The role of health-care providers in mHealth adoption. Lancet Digit. Health 2019, 1, e58–e59. [Google Scholar] [CrossRef]
- Jacob, C.; Sanchez-Vazquez, A.; Ivory, C. Social, Organizational, and Technological Factors Impacting Clinicians’ Adoption of Mobile Health Tools: Systematic Literature Review. JMIR Mhealth Uhealth 2020, 8, e15935. [Google Scholar] [CrossRef]
- Hall, B.J.; Sou, K.L.; Beanland, R.; Lacky, M.; Tso, L.S.; Ma, Q.; Doherty, M.; Tucker, J.D. Barriers and Facilitators to Interventions Improving Retention in HIV Care: A Qualitative Evidence Meta-Synthesis. AIDS Behav. 2017, 21, 1755–1767. [Google Scholar] [CrossRef] [PubMed]
- Ko, D.; Bratzke, L.C.; Roberts, T. Self-management assessment in multiple chronic conditions: A narrative review of literature. Int. J. Nurs. Stud. 2018, 83, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Bulsara, S.M.; Wainberg, M.L.; Newton-John, T.R.O. Predictors of Adult Retention in HIV Care: A Systematic Review. AIDS Behav. 2018, 22, 752–764. [Google Scholar] [CrossRef] [PubMed]
- May, M.; Gompels, M.; Delpech, V.; Porter, K.; Orkin, C.; Kegg, S.; Hay, P.; Johnson, M.; Palfreeman, A.; Gilson, R.; et al. Impact on life expectancy of HIV-1 positive individuals of CD4+ cell count and viral load response to antiretroviral therapy: UK cohort study. AIDS 2014, 28, 1192–1202. [Google Scholar] [CrossRef] [PubMed]
- Global HIV & AIDS Statistics—2019 Fact Sheet. UNAIDS. Available online: https://www.unaids.org/en/resources/fact-sheet (accessed on 18 February 2020).
- EACS Guidelines Version 10.0. November 2019. Available online: https://www.eacsociety.org/files/2019_guidelines-10.0_final.pdf (accessed on 18 February 2020).
- Dillingham, R.; Ingersoll, K.; Flickinger, T.E.; Waldman, A.L.; Grabowski, M.; Laurence, C.; Wispelwey, E.; Reynolds, G.; Conaway, M.; Cohn, W.F. PositiveLinks: A Mobile Health Intervention for Retention in HIV Care and Clinical Outcomes with 12-Month Follow-Up. AIDS Patient Care STDS 2018, 32, 241–250. [Google Scholar] [CrossRef]
- Venter, W.; Coleman, J.; Chan, V.L.; Shubber, Z.; Phatsoane, M.; Gorgens, M.; Stewart-Isherwood, L.; Carmona, S.; Fraser-Hurt, N. Improving Linkage to HIV Care Through Mobile Phone Apps: Randomized Controlled Trial. JMIR MHealth UHealth 2018, 6, e155. [Google Scholar] [CrossRef]
- Venter, W.; Fischer, A.; Lalla-Edward, S.T.; Coleman, J.; Lau Chan, V.; Shubber, Z.; Phatsoane, M.; Gorgens, M.; Stewart-Isherwood, L.; Carmona, S.; et al. Improving Linkage to and Retention in Care in Newly Diagnosed HIV-Positive Patients Using Smartphones in South Africa: Randomized Controlled Trial. JMIR MHealth UHealth 2019, 7, e12652. [Google Scholar] [CrossRef]
- Cooper, V.; Clatworthy, J.; Whetham, J.; Consortium, E. mHealth Interventions to Support Self-Management in HIV: A Systematic Review. Open AIDS J. 2017, 11, 119–132. [Google Scholar] [CrossRef] [PubMed]
- Muessig, K.E.; Nekkanti, M.; Bauermeister, J.; Bull, S.; Hightow-Weidman, L.B. A systematic review of recent smartphone, Internet and Web 2.0 interventions to address the HIV continuum of care. Curr. HIV AIDS Rep. 2015, 12, 173–190. [Google Scholar] [CrossRef] [PubMed]
- Caceres, C.; Gomez, E.J.; Garcia, F.; Gatell, J.M.; del Pozo, F. An integral care telemedicine system for HIV/AIDS patients. Int. J. Med. Inform. 2006, 75, 638–642. [Google Scholar] [CrossRef] [PubMed]
- León, A.; Cáceres, C.; Fernández, E.; Chausa, P.; Martin, M.; Codina, C.; Rousaud, A.; Blanch, J.; Mallolas, J.; Martinez, E.; et al. A New Multidisciplinary Home Care Telemedicine System to Monitor Stable Chronic Human Immunodeficiency Virus-Infected Patients: A Randomized Study. PLoS ONE 2011, 21, e14515. [Google Scholar] [CrossRef]
- Whetham, J.; Jones, C.; Bremner, S.; Apers, L.; Begovac, J.; Borges, M.; Leon, A.; Vera, J.; Zekan, S.; West, B.; et al. EmERGE: Feasibility and uptake of a co-designed digital health supported pathway of care for people living with medically stable HIV. P111. J. Int. AIDS Soc. 2020, 23, 95. Available online: https://onlinelibrary.wiley.com/doi/10.1002/jia2.25616 (accessed on 18 March 2021).
- EmERGE Project Website. Available online: https://www.emergeproject.eu/ (accessed on 9 February 2021).
- EmERGE Project on the Community Research and Development Information Service Website. Available online: https://cordis.europa.eu/project/id/643736 (accessed on 9 February 2021).
- Ruby on Rails Website. Available online: https://rubyonrails.org/ (accessed on 9 February 2021).
- Ruby Website. Available online: https://www.ruby-lang.org/en/ (accessed on 9 February 2021).
- Ionic website. Available online: https://ionicframework.com/ (accessed on 9 February 2021).
- Heroku Website. Available online: https://www.heroku.com/ (accessed on 9 February 2021).
- Santos, A.R.; Kroll, J.; Sales, A.; Fernandes, P.; Wildt, D. Investigating the Adoption of Agile Practices in Mobile Application Development. ICEIS 2016. [Google Scholar] [CrossRef]
- Flora, H.K.; Chande, S.V. A review and analysis on mobile application development processes using agile methodologies. Int. J. Res. Comput. Sci. 2013, 3, 9–18. [Google Scholar] [CrossRef]
- Marent, B.; Henwood, F.; Darking, M.; on behalf of the EmERGE Consortium. Ambivalence in digital health: Co-designing an mHealth platform for HIV care. Soc. Sci. Med. 2018, 215, 133–241. [Google Scholar] [CrossRef] [PubMed]
- Marent, B.; Henwood, F.; Darking, M.; EmERGE Consortium. Development of an mHealth platform for HIV Care: Gathering User Perspectives Through Co-Design Workshops and Interviews. JMIR Mhealth Uhealth 2018, 6, e184. [Google Scholar] [CrossRef] [PubMed]
- Kidholm, K.; Ekeland, A.G.; Jensen, L.K.; Rasmussen, J.; Pedersen, C.D.; Bowes, A.; Flottorp, S.A.; Bech, M. A model for assessment of telemedicine applications: Mast. Int. J. Technol. Assess Health Care 2012, 28, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Brooke, J.B. SUS-a quick and dirty usability scale. In Usability Evaluation in Industry; Jordan, P., Thomas, B., Weerdmeester, B., McLelland, I., Eds.; Taylor and Francis: London, UK, 1996. [Google Scholar]
- SUS: A ‘quick and dirty’ usability scale. In Usability Evaluation in Industry, 1st ed.; McClelland, L., Jordan, W., Thomas, B., Weerdmeester, A., Eds.; Taylor & Francis: London, UK, 1996; pp. 189–194. [Google Scholar]
- Bangor, A.; Kortum, P.; Miller, J. Determining What Individual SUS Scores Mean: Adding an Adjective Rating Scale. J. Usability Stud. 2009, 4, 114–123. [Google Scholar]
- World Health Organization. People-Centred and Integrated Health Services: An Overview of the Evidence. 2015. Available online: https://apps.who.int/iris/bitstream/handle/10665/155004/WHO_HIS_SDS_2015.7_eng.pdf?sequence=1 (accessed on 9 February 2021).
- WHO Global Strategy on People-Centred and Integrated Health Services. World Health Organization. 2015. Available online: https://apps.who.int/iris/bitstream/handle/10665/155002/WHO_HIS_SDS_2015.6_eng.pdf?sequence=1 (accessed on 9 February 2021).
- Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the Protection of Natural Persons with Regard to the Processing of Personal Data and on the Free Movement of such Data, and Repealing Directive 95/46/EC (General Data Protection Regulation). Available online: https://eur-lex.europa.eu/eli/reg/2016/679/oj (accessed on 18 March 2021).
- Hill, P. mHealth: A cost-effective solution to chronic problems? J. Med. Therap. 2018, 2, 2–4. [Google Scholar] [CrossRef]
- van den Berk, G.E.L.; Leoni, M.C.; Behrens, G.M.N.; Taljaard, J.; Arends, J.E. Improving HIV-related care through eHealth. Lancet HIV 2019, 7, e8–e10. [Google Scholar] [CrossRef]





| Functionality | Description | User |
|---|---|---|
| Authentication | Users are required to login into the platform on each use | All users |
| Patient/device registration | Registration of patients and the associated mobile devices | Administrators and clinicians |
| All patient visualization | Search and filtering of all registered patients | Administrators and clinicians |
| Patient data visualization | Overview of each patient user: current medication list (name, dose/frequency and date of commencement); blood test results (graphically and in a table format) and appointment lists | Administrators and clinicians |
| “Virtual clinics” appointment management | Send data to the mobile application; rebook the patient for a future revision; pause the patient in the system | Administrators and clinicians |
| Messaging | Messaging from Hospital clinicians | All users |
| FAQ management | Provision of Frequently Ask Questions | Administrators |
| User management | Creation and elimination of users and assignment of roles | Administrators |
| Medication visualization | Visualization of medication list (name of medication, dose/frequency and date of commencement). Link to external Liverpool HIV drugs interaction webpage | PLWH |
| Blood test results visualization | Visualization of blood test results: current and historical data; evolution graphs | PLWH |
| Appointments | Visualization of next appointments. Integration with patient mobile calendar | PLWH |
| Help desk and information | Support and access to FAQs | PLWH |
| Application Settings | Erase application data, change passcode, change security question, ask for a new password, study withdrawal | PLWH |
| Requirement | Description |
|---|---|
| Usability | Easy to be used and learnt, easy to be remembered, efficient and able to generate satisfaction in the users. Intuitive interfaces, readable and adapted to users, different web browsers and device resolution screens |
| Adaptability | Platform to be introduced in systems of different hospitals. It must be easy to implement and easy to readapt to different characteristics and requirements |
| Scalability | System architecture should be designed to appropriately handle increasing and decreasing workloads and prepared for a rapid expansion in number of clinical sites and number of users |
| Security | Information should be sent in a secure way. Stored data only accessible by authorized health staff. System only accessible to registered and validated users |
| Performance | The response time in operations must be the expected time of any web application |
| Multiplatform | The platform should be accessible through mobile applications (iOS and Android) or any of the existing web browsers depending on the role of the user |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gárate, F.J.; Chausa, P.; Whetham, J.; Jones, C.I.; García, F.; Cáceres, C.; Sánchez-González, P.; Wallitt, E.; Gómez, E.J.; on behalf of the EmERGE Consortium. EmERGE mHealth Platform: Implementation and Technical Evaluation of a Digital Supported Pathway of Care for Medically Stable HIV. Int. J. Environ. Res. Public Health 2021, 18, 3156. https://doi.org/10.3390/ijerph18063156
Gárate FJ, Chausa P, Whetham J, Jones CI, García F, Cáceres C, Sánchez-González P, Wallitt E, Gómez EJ, on behalf of the EmERGE Consortium. EmERGE mHealth Platform: Implementation and Technical Evaluation of a Digital Supported Pathway of Care for Medically Stable HIV. International Journal of Environmental Research and Public Health. 2021; 18(6):3156. https://doi.org/10.3390/ijerph18063156
Chicago/Turabian StyleGárate, Francisco J., Paloma Chausa, Jennifer Whetham, Christopher Iain Jones, Felipe García, César Cáceres, Patricia Sánchez-González, Edward Wallitt, Enrique J. Gómez, and on behalf of the EmERGE Consortium. 2021. "EmERGE mHealth Platform: Implementation and Technical Evaluation of a Digital Supported Pathway of Care for Medically Stable HIV" International Journal of Environmental Research and Public Health 18, no. 6: 3156. https://doi.org/10.3390/ijerph18063156
APA StyleGárate, F. J., Chausa, P., Whetham, J., Jones, C. I., García, F., Cáceres, C., Sánchez-González, P., Wallitt, E., Gómez, E. J., & on behalf of the EmERGE Consortium. (2021). EmERGE mHealth Platform: Implementation and Technical Evaluation of a Digital Supported Pathway of Care for Medically Stable HIV. International Journal of Environmental Research and Public Health, 18(6), 3156. https://doi.org/10.3390/ijerph18063156






