Measurement Methods of Fatigue, Sleepiness, and Sleep Behaviour Aboard Ships: A Systematic Review
Abstract
:1. Introduction
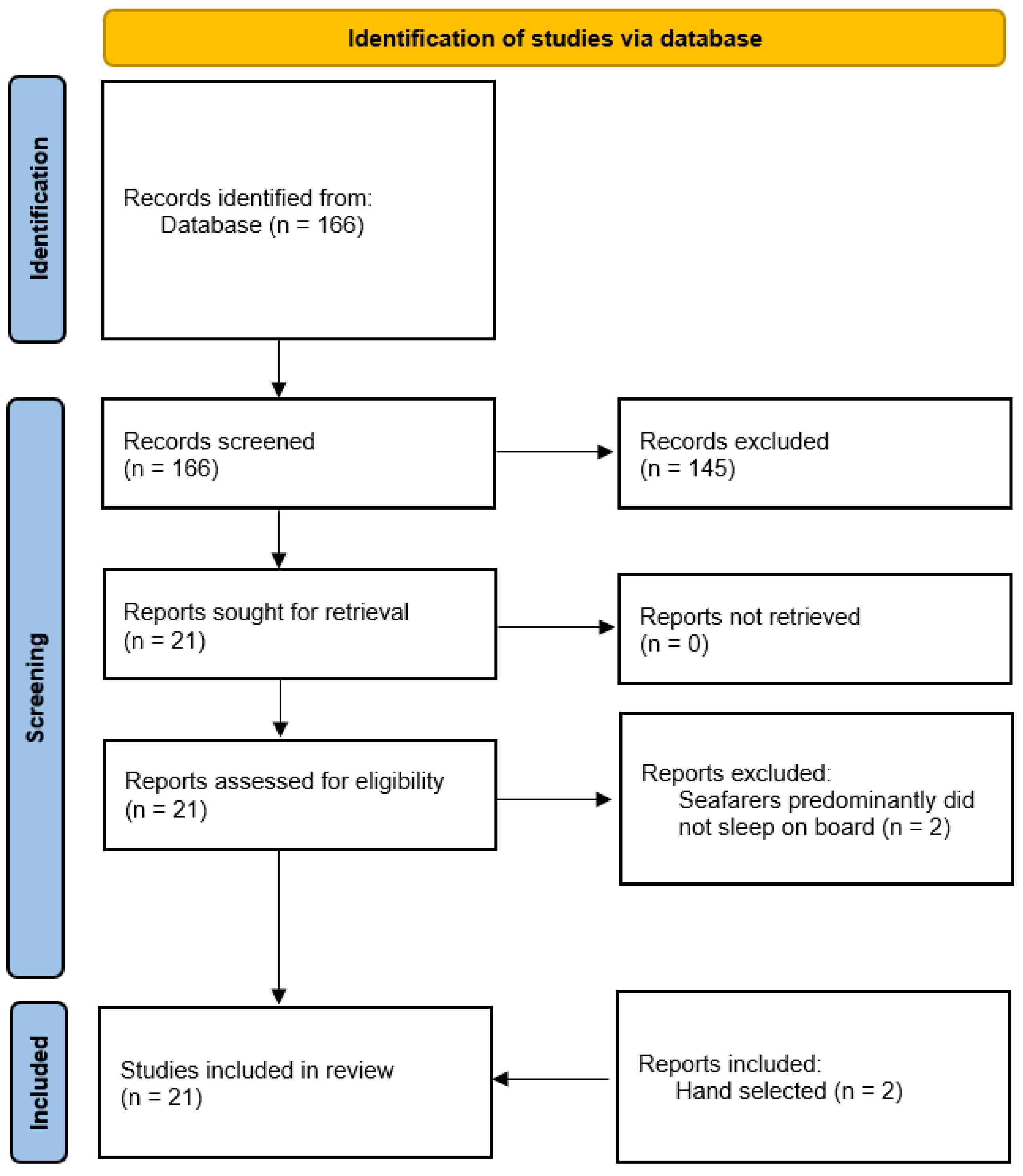
2. Materials and Methods
3. Results
3.1. Subjective Measurement Methods
3.2. Objective Measurement Methods
4. Discussion
4.1. Subjective Measurement Methods and Limitations
4.1.1. Questionnaires
4.1.2. Diaries
4.2. Objective Measurement Methods, Differences and Limitations
4.2.1. Actigraphy
4.2.2. Electrooculography (EOG)
4.2.3. Pupillometry
4.2.4. Reaction Time Tests (RTT)
4.2.5. Polysomnography (PSG)
4.3. Comparison of Actigraphy and PSG
4.4. Comparison of Subjective and Objective Measurement Methods
4.5. Influences of Stress on Fatigue, Sleepiness, and Sleep Behaviour
4.6. Further Factors That Should Be Considered in Measurements of Fatigue, Sleep, and Sleep Behaviour on Board
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BIS | Bergen Insomnia Scale |
| CSS | Crew Status Survey |
| EEG | Electroencephalography |
| EOG | Electrooculography |
| ESS | Epworth Sleepiness Scale |
| FNE | First Night Effect |
| FSS | Fatigue Severity Scale |
| IMO | International Maritime Organization |
| ISI | Insomnia Severity Index |
| KSQ | Karolinska Sleep Questionnaire |
| KSS | Karolinska Sleepiness Scale |
| MEQ | Morningness-Eveningness Questionnaire |
| NFR | Need for Recovery Scale |
| OSA | Obstructive Sleep Apnoea |
| POMS | Profile of Mood States |
| PSG | Polysomnography |
| PSQI | Pittsburgh Sleep Quality Index |
| PsyCap | Psychological Capital |
| PUI | Pupil Unrest Index |
| PVT | Psychomotor Vigilance Test |
| RTT | Reaction Time Test |
| SE% | Sleep Efficiency |
| SOFI | Swedish Occupational Fatigue Inventory |
| SOL | Sleep Onset Latency |
| SPFS | Samn-Perelli Fatigue Scale |
| SSS | Stanford Sleepiness Scale |
| TSD | Total Sleep Debt |
| TST | Total Sleep Time |
Appendix A
| Actiwatch 2 (Philips Respironics) | Actiwatch Spectrum (Philips Respironics) | Actiwatch Spectrum Plus (Philips Respironics) | Motionlogger Watch (Ambulatory Monitoring, Inc.) | ActiGraph GT9X Link (ActiGraph) | |
|---|---|---|---|---|---|
| Size (cm) | 4.3 × 2.3 × 1.0 | 4.8 × 3.7 × 1.4 | 4.8 × 3.7 × 1.5 | 4.4 × 1.8 × 1.5 | 3.5 × 3.5 × 1.0 |
| Weight (g) | 16 | 30 | 31 | 65.2 | 14 |
| Battery Life | 30 days | 8 months | 60 days | over 30 days | 14 days |
| Water Resistance | 1 m for 30 min per IPX7IEC 60529 | 1 m for 30 min per IPX7IEC 60529 | 1 m for 30 min per IPX7IEC 60529 | 50 M | IP27 1 m, 30 min |
| Wrist Detection | x | x | x | x | |
| Light Sensor | x | x | x | x | |
| Event Marker | x | x | x | x | |
| Mean Temperature | x | ||||
| PVT Reaction Time Rest | x | ||||
| Sensitivity compared to PSG a | 90.8% 1 | 95.0% 2 | - | 96.6% 3 | - |
| Specificity compared to PSG b | 65.6% 1 | 34.0% 2 | - | 65.9% 3 | - |
References
- Oldenburg, M.; Baur, X.; Schlaich, C. Occupational risks and challenges of seafaring. J. Occup. Health 2010, 52, 249–256. [Google Scholar] [CrossRef] [Green Version]
- Matsangas, P.; Shattuck, N.L. Habitability in Berthing Compartments and Well-Being of Sailors Working on U.S. Navy Surface Ships. Hum. Factors 2020, 63, 462–473. [Google Scholar] [CrossRef]
- IMO. Guidelines on Fatigue. Available online: https://www.imo.org/en/OurWork/HumanElement/Pages/Fatigue.aspx (accessed on 23 April 2021).
- Phillips, R. Sleep, watchkeeping and accidents: A content analysis of incident at sea reports. Transp. Res. Part F Traffic Psychol. Behav. 2000, 3, 229–240. [Google Scholar] [CrossRef]
- Jepsen, J.R.; Zhao, Z.; van Leeuwen, W.M. Seafarer fatigue: A review of risk factors, consequences for seafarers’ health and safety and options for mitigation. Int. Marit. Health 2015, 66, 106–117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lützhöft, M.; Dahlgren, A.; Kircher, A.; Thorslund, B.; Gillberg, M. Fatigue at sea in Swedish shipping-a field study. Am. J. Ind. Med. 2010, 53, 733–740. [Google Scholar] [CrossRef]
- Shahid, A.; Shen, J.; Shapiro, C.M. Measurements of sleepiness and fatigue. J. Psychosom. Res. 2010, 69, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Johns, M. Rethinking the assessment of sleepiness. Sleep Med. Rev. 1998, 2, 3–15. [Google Scholar] [CrossRef]
- Phillips, R.O. What is Fatigue and How Does It Affect the Safety Performance of Human Transport Operators?—Fatigue in Transport Report I; 1351/2014; Institute of Transport Economics (TØI): Oslo, Norway, 2014. [Google Scholar]
- Matsangas, P.; Shattuck, N.L. Discriminating Between Fatigue and Sleepiness in the Naval Operational Environment. Behav. Sleep Med. 2018, 16, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Weeß, H.-G. Diagnostische Methoden. In Praxis der Schlafmedizin: Diagnostik, Differenzialdiagnostik und Therapie bei Erwachsenen und Kindern, 3rd ed.; Stuck, B.A., Maurer, J.T., Schlarb, A.A., Schredl, M., Weeß, H.G., Eds.; Springer: Berlin, Germany, 2017; Volume 3, pp. 23–85. [Google Scholar]
- Allen, P.; Wadsworth, E.; Smith, A. Seafarers’ fatigue: A review of the recent literature. Int. Marit. Health 2008, 59, 81–92. [Google Scholar] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Dohrmann, S.B.; Herttua, K.; Leppin, A. Fatigue in ferry shipping employees: The role of work-family conflict and supervisor support. BMC Public Health 2019, 19, 1693. [Google Scholar] [CrossRef]
- Dohrmann, S.B.; Herttua, K.; Leppin, A. Is physical and psychological work stress associated with fatigue in Danish ferry ship employees? Int. Marit. Health 2020, 71, 46–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Leeuwen, W.M.; Kircher, A.; Dahlgren, A.; Lützhöft, M.; Barnett, M.; Kecklund, G.; Åkerstedt, T. Sleep, sleepiness, and neurobehavioral performance while on watch in a simulated 4 hours on/8 hours off maritime watch system. Chronobiol. Int. 2013, 30, 1108–1115. [Google Scholar] [CrossRef] [PubMed]
- Léger, D.; Elbaz, M.; Raffray, T.; Metlaine, A.; Bayon, V.; Duforez, F. Sleep management and the performance of eight sailors in the Tour de France à la voile yacht race. J. Sports Sci. 2008, 26, 21–28. [Google Scholar] [CrossRef]
- SIGN. SIGN 50: A Guideline Developer’s Handbook, Annex B: Key to Evidence Statements and Grades of Recommendations. Available online: https://www.sign.ac.uk/assets/sign50_2011.pdf (accessed on 23 April 2021).
- Bridger, R.S.; Brasher, K.; Dew, A. Work demands and need for recovery from work in ageing seafarers. Ergonomics 2010, 53, 1006–1015. [Google Scholar] [CrossRef] [PubMed]
- Harris, E.; Taylor, M.K.; Drummond, S.P.; Larson, G.E.; Potterat, E.G. Assessment of Sleep Disruption and Sleep Quality in Naval Special Warfare Operators. Mil. Med. 2015, 180, 803–808. [Google Scholar] [CrossRef] [Green Version]
- Hurdiel, R.; Van Dongen, H.P.; Aron, C.; McCauley, P.; Jacolot, L.; Theunynck, D. Sleep restriction and degraded reaction-time performance in Figaro solo sailing races. J. Sports Sci. 2014, 32, 172–174. [Google Scholar] [CrossRef]
- Hystad, S.W.; Eid, J. Sleep and Fatigue Among Seafarers: The Role of Environmental Stressors, Duration at Sea and Psychological Capital. Saf. Health Work 2016, 7, 363–371. [Google Scholar] [CrossRef]
- Hystad, S.W.; Saus, E.R.; Sætrevik, B.; Eid, J. Fatigue in seafarers working in the offshore oil and gas re-supply industry: Effects of safety climate, psychosocial work environment and shift arrangement. Int. Marit. Health 2013, 64, 72–79. [Google Scholar]
- Jaipurkar, R.; Mahapatra, S.S.; Bobdey, S.; Banerji, C. Work-rest pattern, alertness and performance assessment among naval personnel deployed at sea: A cross sectional study. Med. J. Armed Forces India 2019, 75, 158–163. [Google Scholar] [CrossRef]
- Matsangas, P.; Shattuck, N.L. Sleep Quality, Occupational Factors, and Psychomotor Vigilance Performance in U.S. Navy Sailors. Sleep 2020, 43, zsaa118. [Google Scholar] [CrossRef] [PubMed]
- Nordmo, M.; Hystad, S.W.; Sanden, S.; Johnsen, B.H. The effect of hardiness on symptoms of insomnia during a naval mission. Int. Marit. Health 2017, 68, 147–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oldenburg, M.; Jensen, H.J. Sleepiness of day workers and watchkeepers on board at high seas: A cross-sectional study. BMJ Open 2019, 9, e028449. [Google Scholar] [CrossRef] [PubMed]
- Shattuck, N.L.; Matsangas, P. Operational assessment of the 5-h on/10-h off watchstanding schedule on a US Navy ship: Sleep patterns, mood and psychomotor vigilance performance of crewmembers in the nuclear reactor department. Ergonomics 2016, 59, 657–664. [Google Scholar] [CrossRef]
- Shattuck, N.L.; Matsangas, P. Sunlight Exposure, Work Hours, Caffeine Consumption, and Sleep Duration in the Naval Environment. Aerosp. Med. Hum. Perform. 2017, 88, 579–585. [Google Scholar] [CrossRef]
- Shattuck, N.L.; Matsangas, P. Does the quality of life differ for shift workers compared to day workers? Chronobiol. Int. 2020, 37, 1299–1303. [Google Scholar] [CrossRef]
- Sunde, E.; Bratveit, M.; Pallesen, S.; Moen, B.E. Noise and sleep on board vessels in the Royal Norwegian Navy. Noise Health 2016, 18, 85–92. [Google Scholar] [CrossRef]
- Thomas, M.J.W.; Paterson, J.L.; Jay, S.M.; Matthews, R.W.; Ferguson, S.A. More than hours of work: Fatigue management during high-intensity maritime operations. Chronobiol. Int. 2019, 36, 143–149. [Google Scholar] [CrossRef]
- Valdersnes, K.B.; Eid, J.; Hystad, S.W.; Nielsen, M.B. Does psychological capital moderate the relationship between worries about accidents and sleepiness? Int. Marit. Health 2017, 68, 245–251. [Google Scholar] [CrossRef]
- Youn, I.H.; Lee, J.M. Seafarers’ Physical Activity and Sleep Patterns: Results from Asia-Pacific Sea Routes. Int. J. Environ. Res. Public Health 2020, 17, 7266. [Google Scholar] [CrossRef]
- Gawron, V.J. Overview of Self-Reported Measures of Fatigue. Int. J. Aviat. Psychol. 2016, 26, 120–131. [Google Scholar] [CrossRef]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Quante, M.; Kaplan, E.R.; Rueschman, M.; Cailler, M.; Buxton, O.M.; Redline, S. Practical considerations in using accelerometers to assess physical activity, sedentary behavior, and sleep. Sleep Health 2015, 1, 275–284. [Google Scholar] [CrossRef] [PubMed]
- Carney, C.E.; Buysse, D.J.; Ancoli-Israel, S.; Edinger, J.D.; Krystal, A.D.; Lichstein, K.L.; Morin, C.M. The Consensus Sleep Diary: Standardizing Prospective Sleep Self-Monitoring. Sleep 2012, 35, 287–302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCambridge, J.; Witton, J.; Elbourne, D.R. Systematic review of the Hawthorne effect: New concepts are needed to study research participation effects. J. Clin. Epidemiol. 2014, 67, 267–277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ong, C.; Hutch, M.; Smirnakis, S. The Effect of Ambient Light Conditions on Quantitative Pupillometry. Neurocrit. Care 2019, 30, 316–321. [Google Scholar] [CrossRef]
- Ferris, M.; Bowles, K.A.; Bray, M.; Bosley, E.; Rajaratnam, S.M.W.; Wolkow, A.P. The impact of shift work schedules on PVT performance in naturalistic settings: A systematic review. Int. Arch. Occup. Environ. Health 2021, 94, 1475–1494. [Google Scholar] [CrossRef]
- Jay, S.M.; Dawson, D.; Lamond, N. Train drivers’ sleep quality and quantity during extended relay operations. Chronobiol. Int. 2006, 23, 1241–1252. [Google Scholar] [CrossRef]
- Signal, T.L.; Gander, P.H.; van den Berg, M.J.; Graeber, R.C. In-flight sleep of flight crew during a 7-hour rest break: Implications for research and flight safety. Sleep 2013, 36, 109–115. [Google Scholar] [CrossRef] [Green Version]
- Mitler, M.M.; Miller, J.C.; Lipsitz, J.J.; Walsh, J.K.; Wylie, C.D. The sleep of long-haul truck drivers. N. Engl. J. Med. 1997, 337, 755–761. [Google Scholar] [CrossRef]
- Mairesse, O.; MacDonald-Nethercott, E.; Neu, D.; Tellez, H.F.; Dessy, E.; Neyt, X.; Meeusen, R.; Pattyn, N. Preparing for Mars: Human sleep and performance during a 13 month stay in Antarctica. Sleep 2019, 42, zsy206. [Google Scholar] [CrossRef] [PubMed]
- Zinkhan, M.; Berger, K.; Hense, S.; Nagel, M.; Obst, A.; Koch, B.; Penzel, T.; Fietze, I.; Ahrens, W.; Young, P.; et al. Agreement of different methods for assessing sleep characteristics: A comparison of two actigraphs, wrist and hip placement, and self-report with polysomnography. Sleep Med. 2014, 15, 1107–1114. [Google Scholar] [CrossRef] [PubMed]
- Morgenthaler, T.; Alessi, C.; Friedman, L.; Owens, J.; Kapur, V.; Boehlecke, B.; Brown, T.; Chesson, A., Jr.; Coleman, J.; Lee-Chiong, T.; et al. Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: An update for 2007. Sleep 2007, 30, 519–529. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, M.T.; McCrae, C.S.; Cheung, J.; Martin, J.L.; Harrod, C.G.; Heald, J.L.; Carden, K.A. Use of Actigraphy for the Evaluation of Sleep Disorders and Circadian Rhythm Sleep-Wake Disorders: An American Academy of Sleep Medicine Clinical Practice Guideline. J. Clin. Sleep Med. 2018, 14, 1231–1237. [Google Scholar] [CrossRef] [Green Version]
- AASM. International Classification of Sleep Disorders, 3rd ed.; American Academy of Sleep Medicine: Darien, IL, USA, 2014. [Google Scholar]
- Conradt, R.; Brandenburg, U.; Ploch, T.; Peter, J.H. Aktigraphie: Methodische Begrenzungen für die Beurteilung von Schlafstadien und Schlafstruktur gesunder Probanden [Actigraphy: Methodological limits for evaluation of sleep stages and sleep structure of healthy probands]. Pneumologie 1997, 51 (Suppl. 3), 721–724. [Google Scholar]
- Ancoli-Israel, S.; Cole, R.; Alessi, C.; Chambers, M.; Moorcroft, W.; Pollak, C.P. The role of actigraphy in the study of sleep and circadian rhythms. Sleep 2003, 26, 342–392. [Google Scholar] [CrossRef] [Green Version]
- Marino, M.; Li, Y.; Rueschman, M.N.; Winkelman, J.W.; Ellenbogen, J.M.; Solet, J.M.; Dulin, H.; Berkman, L.F.; Buxton, O.M. Measuring Sleep: Accuracy, Sensitivity, and Specificity of Wrist Actigraphy Compared to Polysomnography. Sleep 2013, 36, 1747–1755. [Google Scholar] [CrossRef]
- Mayer, G.; Arzt, M.; Braumann, B. S3-Leitlinie Nicht erholsamer Schlaf/Schlafstörungen—Kapitel “Schlafbezogene Atmungsstörungen”. Somnologie 2017, 20, 97–180. [Google Scholar] [CrossRef]
- Andrade, L.; Paiva, T. Ambulatory Versus Laboratory Polysomnography in Obstructive Sleep Apnea: Comparative Assessment of Quality, Clinical Efficacy, Treatment Compliance, and Quality of Life. J. Clin. Sleep Med. 2018, 14, 1323–1331. [Google Scholar] [CrossRef] [Green Version]
- Iber, C.; Redline, S.; Kaplan Gilpin, A.M.; Quan, S.F.; Zhang, L.; Gottlieb, D.J.; Rapoport, D.; Resnick, H.E.; Sanders, M.; Smith, P. Polysomnography performed in the unattended home versus the attended laboratory setting—Sleep Heart Health Study methodology. Sleep 2004, 27, 536–540. [Google Scholar] [CrossRef]
- Miettinen, T.; Myllymaa, K.; Hukkanen, T.; Töyräs, J.; Sipilä, K.; Myllymaa, S. Home Polysomnography Reveals a First-Night Effect in Patients With Low Sleep Bruxism Activity. J. Clin. Sleep Med. 2018, 14, 1377–1386. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R. Gibt es Einen First Night Effect bei Ambulanter Polysomnographie? Eine Untersuchung an Fünfundzwanzig Schlafgesunden Probanden. Ph.D. Thesis, Rheinisch-Westfälische Technische Hochschule Aachen, Aachen, Germany, 2005. [Google Scholar]
- Veauthier, C.; Piper, S.K.; Gaede, G.; Penzel, T.; Paul, F. The first night effect in multiple sclerosis patients undergoing home-based polysomnography. Nat. Sci. Sleep 2018, 10, 337–344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schumann, A.; Kietzer, S.; Ebel, J.; Bär, K.J. Sympathetic and Parasympathetic Modulation of Pupillary Unrest. Front. Neurosci. 2020, 14, 178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kelbsch, C.; Strasser, T.; Chen, Y.; Feigl, B.; Gamlin, P.D.; Kardon, R.; Peters, T.; Roecklein, K.A.; Steinhauer, S.R.; Szabadi, E.; et al. Standards in Pupillography. Front. Neurol. 2019, 10, 129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boyne, K.; Sherry, D.D.; Gallagher, P.R.; Olsen, M.; Brooks, L.J. Accuracy of computer algorithms and the human eye in scoring actigraphy. Sleep Breath. 2013, 17, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Pougnet, R.; Pougnet, L.; Loddé, B.; Canals, L.; Bell, S.; Lucas, D.; Dewitte, J.D. Consumption of addictive substances in mariners. Int. Marit. Health 2014, 65, 199–204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shahid, A.; Wilkinson, K.; Marcu, S.; Shapiro, C.M. STOP, THAT and One Hundred Other Sleep Scales; Springer Science & Business Media: New York, NY, USA, 2012. [Google Scholar]
- Tamura, Y.; Horiyasu, T.; Sano, Y.; Chonan, K.; Kawada, T.; Sasazawa, Y.; Kuroiwa, M.; Suzuki, S. Habituation of sleep to a ship’s noise as determined by actigraphy and a sleep questionnaire. J. Sound Vib. 2002, 250, 107–113. [Google Scholar] [CrossRef]
- DGAUM. S2k-Leitlinie Gesundheitliche Aspekte und Gestaltung von Nacht- und Schichtarbeit. Available online: https://www.awmf.org/uploads/tx_szleitlinien/002-030l_S2k_Gesundheitliche-Aspekte-Gestaltung-Nacht-und-Schichtarbeit_2020-03.pdf (accessed on 23 April 2021).
- Arendt, J.; Middleton, B.; Williams, P.; Francis, G.; Luke, C. Sleep and circadian phase in a ship’s crew. J. Biol. Rhythm. 2006, 21, 214–221. [Google Scholar] [CrossRef]
- Oldenburg, M.; Jensen, H.J. Stress and strain among merchant seafarers differs across the three voyage episodes of port stay, river passage and sea passage. PLoS ONE 2019, 14, e0217904. [Google Scholar] [CrossRef]
- Pigeon, W.R.; Taylor, M.; Bui, A.; Oleynk, C.; Walsh, P.; Bishop, T.M. Validation of the Sleep-Wake Scoring of a New Wrist-Worn Sleep Monitoring Device. J. Clin. Sleep Med. 2018, 14, 1057–1062. [Google Scholar] [CrossRef]
- Quante, M.; Kaplan, E.R.; Cailler, M.; Rueschman, M.; Wang, R.; Weng, J.; Taveras, E.M.; Redline, S. Actigraphy-based sleep estimation in adolescents and adults: A comparison with polysomnography using two scoring algorithms. Nat. Sci. Sleep 2018, 10, 13–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rupp, T.L.; Balkin, T.J. Comparison of Motionlogger Watch and Actiwatch actigraphs to polysomnography for sleep/wake estimation in healthy young adults. Behav. Res. Methods 2011, 43, 1152–1160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Author (Year) | SIGN-Criteria | Study Aim | Population | Year of Investigation | Measuring Method of Fatigue, Sleepiness, or Sleep Behaviour | |||
|---|---|---|---|---|---|---|---|---|
| Subjective | Objective | |||||||
| Actigraphy | RTT | Other | ||||||
| Bridger et al. (2010) [19] | 2+ | To investigate the relationship between age, job demands, and recreational needs in the maritime industry | 322 employees on seven Royal Fleet Auxiliary vessels | November 2008–July 2009 | NFR | |||
| Harris et al. (2015) [20] | 2− | To document characteristics of sleep disturbances; to examine the relationship between objectively derived and self-reported sleep indices and sleep quality | 29 active-duty male Naval Special Forces | Sleep log | Motionlogger Watch (Ambulatory Monitoring, Inc., Ardsley, NY, USA) | |||
| Hurdiel et al. (2014) [21] | 2+ | To evaluate sleep during solo offshore sailing races and compare reaction times during a reaction time test before and after these races | Twelve professional sailors on yachts (10-m Figaro 2 Beneteau) | Sleep log | GT3X (ActiGraph, Pensacola, FL, USA) | 5-min PVT | ||
| Hystad and Eid (2016) [22] | 2+ | To assess the effects of duration at sea, seafaring experience, environmental stressors, and psychological capital (PsyCap) on sleep quality and fatigue | 742 seafarers (402 in the offshore supply industry and 340 aboard combined passenger roll-on/roll-off ferries and cargo ships) on 22 different vessels in the North Sea and Southeast Asia | SOFI (revised 20-item version) PSQI (only Ro-Ro-ferry) | ||||
| Hystad et al. (2013) [23] | 2+ | To investigate the effects of safety climate and psychosocial work environment on reported fatigue | 402 seafarers working in offshore oil and gas industry on 22 vessels operating in the North Sea and Southeast Asia | SOFI (revised 20-item version) | ||||
| Jaipurkar et al. (2019) [24] | 2− | To assess and compare sailors’ work-rest rhythms and alertness levels during sailing and non-sailing days; to compare ‘‘sleep duration’’ data as recorded in the sleep diary with actigraphy sleep data | 32 male participants from a large Indian naval vessel | Sleep log Activity log | Actiwatch (Philips Respironics, Bend, OR, USA) | 5-min PVT | Pulse und blood pressure | |
| Léger et al. (2008) [17] | 2+ | To observe how sailors manage their sleep and alertness before and during competition in a long-distance regatta | Eight sailors on yachts during the race Tour de France à la Voile (Atlantic and Mediterranean) | 2002 | Sleep log | PSG: Brainwalker (Medatec software, Braine-le-Château, Belgium) Night Cap: REM view (Respironics, Inc., Bend, OR, USA) | ||
| Lützhöft et al. (2010) [6] | 2+ | To investigate the degree of fatigue on board and compare 6:6 with 4:8 shift schedules | 30 watchkeeping nautical officers on 13 Swedish cargo ships (bulk carriers, car carriers, and tankers; 2300 to 11,000 DWT) | 2005–2007 | KSS | Actiwatch (Cambridge Neurotechnology Ltd., Cambridge, UK) | 6-min (RTT-type not specified) | EOG |
| Matsangas and Shattuck (2018) [10] | 2− | To assess similarities and differences between subjective reports of fatigue/sleepiness; to assess predictors of sleepiness/fatigue; to measure sleepiness/fatigue | 767 crew members (predominantly watchkeepers) on a U.S. Navy aircraft carrier (NIMITZ, CNV-68) | Spring 2014 | ESS FSS | |||
| Matsangas and Shattuck (2020) [2] | 2+ | To assess the prevalence of disruptive factors in the sleep environment; to assess whether these disruptive factors affect sleep and well-being | 1269 sailors (661 watchkeepers and 231 non-watchkeepers) on five ships (one Nimitz-class aircraft carrier, one Ticonderoga-class cruiser, three Arleigh Burke-class Flight IIA destroyers) | 2014–2017 | ESS PSQI POMS ISI Activity log | Motionlogger Watch (Ambulatory Monitoring, Inc., Ardsley, NY, USA) Spectrum Plus (Philips Respironics, Bend, OR, USA) | ||
| Matsangas and Shattuck (2020) [25] | 2+ | To assess sleep quality and examine whether Pittsburgh Sleep Quality Index (PSQI) scores are influenced by occupational factors and sleep attributes and whether PSQI can predict impaired PVT performance | 872 USN sailors (666 watchkeepers and 206 non-watchkeepers) on seven USN “surface combatants” (one Nimitz-class aircraft carrier, one Ticonderoga-class cruiser, and five Arleigh Burke-class destroyers) | Six periods (December 2012, May 2013, June and November 2014, June 2017, December 2017–January 2018) | PSQI Sleep log Activity log | Motionlogger Watch (Ambulatory Monitoring, Inc., Ardsley, NY, USA) Actiwatch Spectrum (Philips Respironics, Bend, OR, USA) | 3-min PVT | |
| Nordmo et al. (2017) [26] | 2− | To examine the association between hardiness and reported insomnia symptoms in a maritime military environment | 281 sailors, officers, and enlisted personnel on a Royal Norwegian Navy frigate during a 4-month naval deployment to combat piracy in the Gulf of Aden | BSI | ||||
| Oldenburg and Jensen (2019) [27] | 2+ | To assess the prevalence of drowsiness in seafarers during sea passage with a distinction between day workers and watchkeepers | 75 day workers and 123 watchkeepers during 18 voyages on 18 different container ships | ESS SSS | SenseWear armband activity monitor (BodyMedia, Inc., Pittsburgh, PA, USA) | Pupillometry | ||
| Shattuck and Matsangas (2016) [28] | 2− | To assess mood, sleep patterns, daytime sleepiness, and psychomotor vigilance performance during a 5/10 watch | 77 Reactor Division (RX) participants on the aircraft carrier USS Nimitz (CVN-68) | 10–27 June 2014 | ESS POMS Activity log | Motionlogger Watch (Ambulatory Monitoring, Inc., Ardsley, NY, USA) Actiwatch Spectrum (Philips Respironics, Bend, OR, USA) | 3-min PVT | |
| Shattuck and Matsangas (2017) [29] | 2− | To assess the impact of sunlight, long working hours, and caffeinated beverages on average daily sleep duration | 91 U.S. Navy crew members (65 men) on the aircraft carrier USS Nimitz | 3–14 November 2014 | ESS Activity log | Motionlogger Watch (Ambulatory Monitoring, Inc., Ardsley, NY, USA) | ||
| Shattuck and Matsangas (2020) [30] | 2+ | To compare the well-being and sleep of dayworkers and shift workers | 804 sailors (78.4% male) on seven U.S. Navy ships | ESS PSQI POMS ISI Activity log | Motionlogger Watch (Ambulatory Monitoring, Ardsley, NY, USA) Spectrum Plus (Philips Respironics, Bend, OR, USA) | |||
| Sunde et al. (2016) [31] | 2+ | To assess relationships between noise exposure during sleep and actigraphy-derived sleep parameter | 72 participants from different occupational groups on board (engineers, navigators, cooks, etc.) on 21 Royal Norwegian Navy ships | April 2012–June 2013 | Actiwatch AW4 (Cambridge Neurotechnology Ltd., Cambridge, UK) Actiwatch 2 (Philips Respironics, Bend, OR, USA) | |||
| Thomas et al. (2019) [32] | 2− | To investigate the consequences of fatigue and workload associated with increased operational stress | 12 senior staff on board a roll-on roll-off ferry in Australia | CSS/SPFS | Unspecified device (Philips Respironics, Bend, OR, USA) | 5-min PVT | ||
| Valdersnes et al. (2017) [33] | 2+ | To investigate the relationship between worries about possible accidents and sleepiness in seafarers; to investigate PsyCap as a protective factor in this context | 397 seafarers from a Norwegian company in the offshore oil and gas industry on 22 ships in the North Sea and Southeast Asia | 2012 | SOFI | |||
| van Leeuwen et al. (2013) [16] | 2− | To investigate sleep, sleepiness, and neuro-behavioural performance in a simulated 4:8 watch system and the effects of disrupting a single free watch simulating a condition of overtime work | 30 bridge officers (29 men) measured with a bridge simulator at Chalmers University of Technology, Gothenburg, who slept on the passenger ship “Origo” | KSQ KSS KSD | 5-min PVT | PSG: Vitaport 3 recorders (TEMEC, Kerkrade, The Netherlands) | ||
| Youn and Lee (2020) [34] | 2+ | To compare the physical activity intensity and sleep patterns under three conditions: (1) moored versus sailing, (2) on-navigation duty and off-navigation duty, and (3) day versus night navigation duty | 51 senior naval students (10 female and 41 male) of the navigation department on training vessels of Mokpo National Maritime University in South Korea on three sea voyages | ActiGraph GT9X Link (ActiGraph, Pensacola, FL, USA) | ||||
| Questionnaires | Number of Studies |
|---|---|
| Fatigue | 9 |
| 3 3 1 1 1 |
| Sleepiness | 9 |
| 6 2 1 |
| Sleep behaviour | 8 |
| 4 2 1 1 |
| Method | Strengths | Weaknesses | Weaknesses in the Maritime-Specific Setting |
|---|---|---|---|
| Subjective in general | Suitable for large collectives Cost-effective No investigator on board necessary Suitable for long-term studies | Lack of motivation and compliance | |
| Questionnaires | Different questionnaires for special questions (e.g., fatigue, sleepiness, sleep quality) | Recall bias Use of different cut-off values Risk of social desirability with time contracts or interviewer presence | Designed for land context (ESS contains question on road behaviour) |
| Activity and sleep diaries | Easy individual adaptation to study design Supplementation of missing actigraphy data | Often poor comparability due to inconsistent format Sleep duration and quality often overestimated | |
| Objective in general | Independent of motivation, recall bias, social desirability | Study population limited by number of devices Investigator on board necessary | |
| Reaction Time Test (RTT)/Psychomotor Vigilance Test (PVT) | Cost-effective Gold standard for detecting sleepiness-related vigilance reduction | Only captures effect of sleepiness (Ship) movement and noise can falsify measurements | |
| Pupillometry | Fast, uncomplicated handling | Only measures effect of sleepiness (Ship) motion, noise, ambient light can falsify measurements | |
| Electrooculography (EOG) | Motion artifacts Interindividual different blinking characteristics Time-consuming evaluation | ||
| Actigraphy | Cost-effective Suitable for long-term studies Hardly any first-night effect Good agreement with PSG in TST, SOL, SE% | No display of sleep architecture Overestimation of sleep periods Underestimation of the wake stage | Motion artifacts due to strong sea state/high speed |
| Ambulatory Polysomnography (PSG) | Comparable with stationary PSG (gold standard of sleep diagnostics) Display of sleep architecture Possibly hardly/less first night effect (in contrast to stationary PSG) | Cost intensive Time-consuming measurement and evaluation |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kerkamm, F.; Dengler, D.; Eichler, M.; Materzok-Köppen, D.; Belz, L.; Neumann, F.A.; Zyriax, B.C.; Harth, V.; Oldenburg, M. Measurement Methods of Fatigue, Sleepiness, and Sleep Behaviour Aboard Ships: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 120. https://doi.org/10.3390/ijerph19010120
Kerkamm F, Dengler D, Eichler M, Materzok-Köppen D, Belz L, Neumann FA, Zyriax BC, Harth V, Oldenburg M. Measurement Methods of Fatigue, Sleepiness, and Sleep Behaviour Aboard Ships: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(1):120. https://doi.org/10.3390/ijerph19010120
Chicago/Turabian StyleKerkamm, Fiona, Dorothee Dengler, Matthias Eichler, Danuta Materzok-Köppen, Lukas Belz, Felix Alexander Neumann, Birgit Christiane Zyriax, Volker Harth, and Marcus Oldenburg. 2022. "Measurement Methods of Fatigue, Sleepiness, and Sleep Behaviour Aboard Ships: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 1: 120. https://doi.org/10.3390/ijerph19010120
APA StyleKerkamm, F., Dengler, D., Eichler, M., Materzok-Köppen, D., Belz, L., Neumann, F. A., Zyriax, B. C., Harth, V., & Oldenburg, M. (2022). Measurement Methods of Fatigue, Sleepiness, and Sleep Behaviour Aboard Ships: A Systematic Review. International Journal of Environmental Research and Public Health, 19(1), 120. https://doi.org/10.3390/ijerph19010120







