A Case Study in Attention-Deficit/Hyperactivity Disorder: An Innovative Neurofeedback-Based Approach
Abstract
:1. Introduction
1.1. Evaluation of ADHD
1.2. ADHD Intervention
2. Methodology
2.1. Description of the Case
2.1.1. Patient Identification
2.1.2. Reason for Consultation
2.1.3. History of the Problem
2.2. Proposed Evaluation and Intervention
2.2.1. Evaluation: Brainwave Analysis with the MiniQ Instrument
2.2.2. Intervention: Neurofeedback Protocols
3. Results
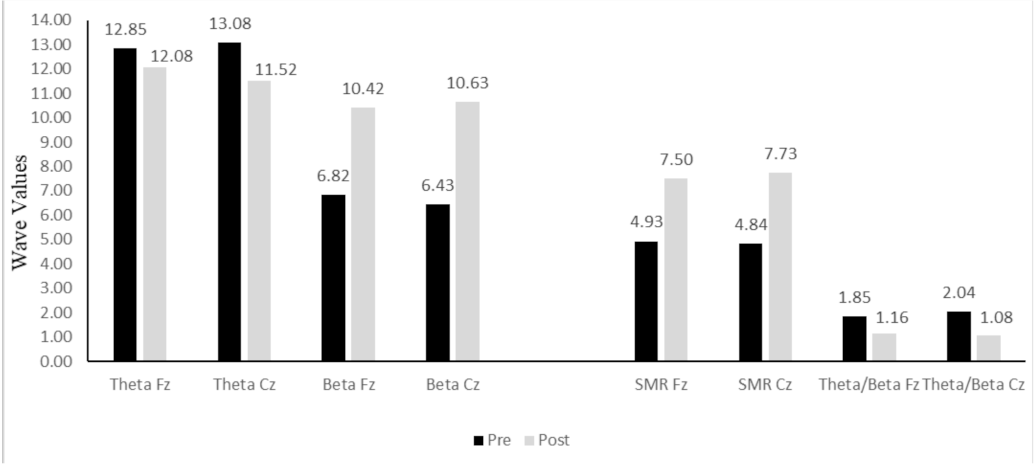
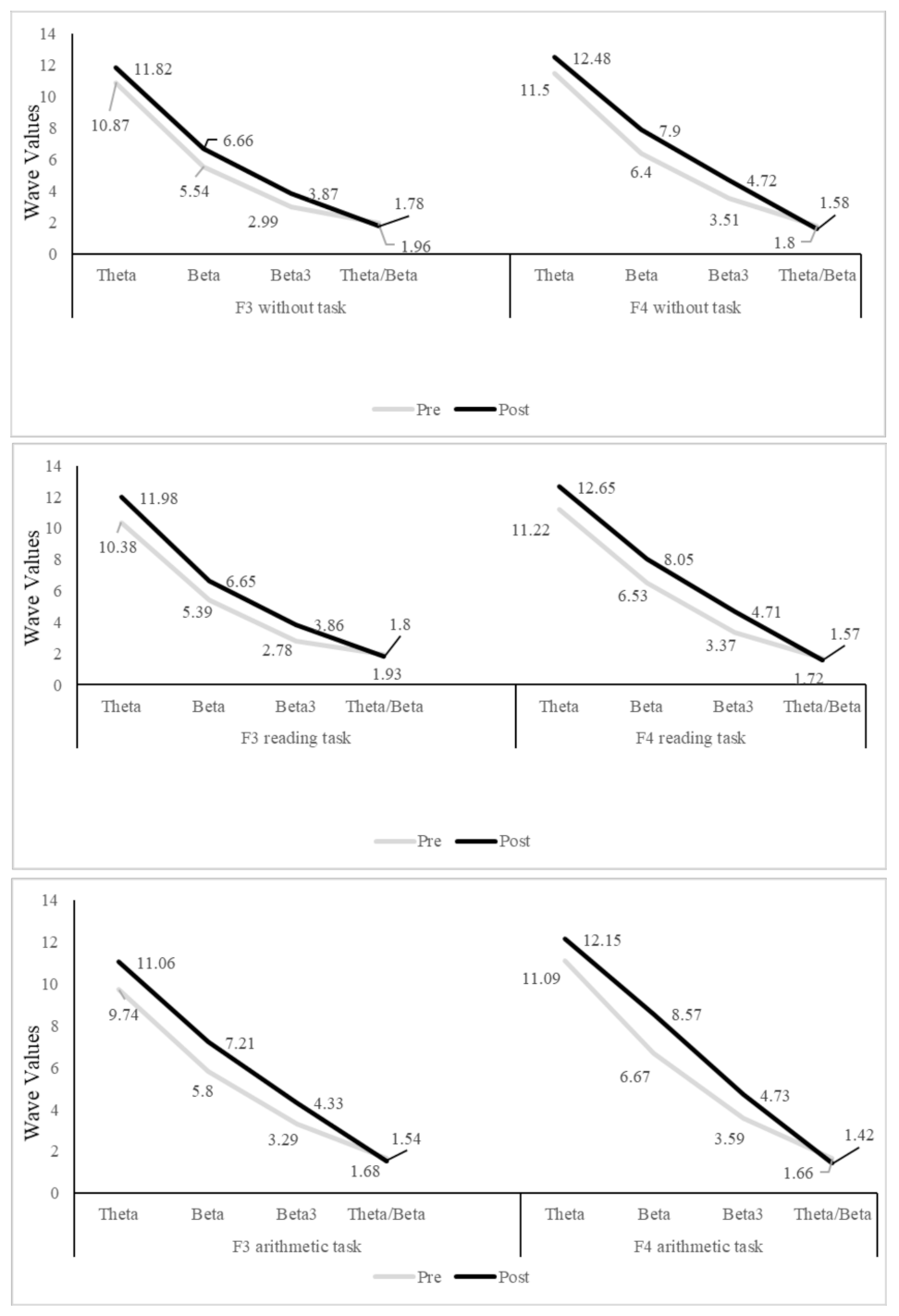
3.1. Brainwave Evaluation
3.2. Progression following Neurofeedback Intervention
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Mirsky, A.F. Disorders of attention: A neuropsychological perspective. In Attention, Memory and Executive Function; Lyon, R.G., Kranesgor, N.A., Eds.; Paul, H. Brookes: Baltimore, MD, USA, 1996; pp. 71–95. [Google Scholar]
- Barkley, R.A. Behavioral inhibition, sustained attention, and executive functions: Constructing a unifying theory of ADHD. Psychol. Bull. 1997, 121, 65–94. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 11th ed.; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Klem, G.H.; Lüders, H.O.; Jasper, H.H.; Elger, C. The ten-twenty electrode system of the International Federation. The International Federation of Clinical Neurophysiology. Electroencephalogr. Clin. Neurophysiol. 1999, 52, 3–6. [Google Scholar]
- Lubar, J.F. Neurofeedback for the management of attention deficit disorders. In Biofeedback: A Practitioner’s Guide, 3rd ed.; Schwartz, M.S., Andrasik, F., Eds.; Guilford Press: New York, USA, 2003; pp. 409–443. [Google Scholar]
- Monastra, V.J.; Lubar, J.F.; Linden, M.; VanDeusen, P.; Green, G.; Wing, W.; Phillips, A.; Fenger, T.N. Assessing attention deficit hyperactivity disorder via quantitative electroencephalography: An initial validation study. Neuropsychology. 1999, 13, 424–433. [Google Scholar] [CrossRef] [PubMed]
- Martella, D.; Aldunate, N.; Fuentes, L.J.; Sánchez-Pérez, N. Arousal and executive alterations in attention deficit hyperactivity disorder (ADHD). Front. Psychol. 2020, 11, 1991. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, C.; González-Castro, P.; Cueli, M.; Areces, D.; González-Pienda, J.A. Attention deficity/hyperactivity disorder (ADHD) diagnosis: An activation-execution model. Front. Psychol. 2016, 7, 1406. [Google Scholar] [CrossRef] [Green Version]
- Clarke, A.; Barry, R.; McCarthy, R.; Selikowitz, M. Age and sex effects in the EEG: Development of the normal child. Clin. Neurophysiol. 2001, 112, 806–814. [Google Scholar] [CrossRef]
- Clarke, A.R.; Barry, R.J.; Johnstone, S.J.; McCarthy, R.; Selikowitz, M. EEG development in attention deficit hyperactivity disorder: From child to adult. Clin. Neurophysiol. 2019, 130, 1256–1262. [Google Scholar] [CrossRef] [PubMed]
- Kerson, C.; deBeus, R.; Lightstone, H.; Arnold, L.E.; Barterian, J.; Pan, X.; Monastra, V.J. EEG theta/beta ratio calculations differ between various EEG neurofeedback and assessment software packages: Clinical interpretation. Clin. EEG Neurosci. 2020, 51, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Caye, A.; Swanson, J.M.; Coghill, D.; Rohde, L.A. Treatment strategies for ADHD: An evidence-based guide to select optimal treatment. Mol. Psychiatry 2019, 24, 390–408. [Google Scholar] [CrossRef] [PubMed]
- Arns, M.; Heinrich, H.; Strehl, U. Evaluation of neurofeedback in ADHD: The long and winding road. Biol. Psychol. 2014, 95, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Arns, M.; Clark, C.R.; Trullinger, M.; deBeus, R.; Mack, M.; Aniftos, M. Neurofeedback and attention-defcit/hyperactivity-disorder (ADHD) in children: Rating the evidence and proposed guidelines. Appl. Psychophysiol. Biofeedback 2020, 45, 39–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cueli, M.; Rodríguez, C.; Cabaleiro, P.; García, T.; González-Castro, P. Differential efficacy of neurofeedback in children with ADHD presentations. J. Clin. Med. 2019, 8, 204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lubar, J.F.; Shouse, M.N. EEG and behavioral changes in a hyperkinetic child concurrent with training ofthe sensorimotor rhythm (SMR): A preliminary report. Biofeedback Self-Regul. 1976, 1, 293–306. [Google Scholar] [CrossRef] [PubMed]
- González-Castro, P.; Cueli, M.; Rodríguez, C.; García, T.; Álvarez, L. Efficacy of neurofeedback versus pharmacological support in subjects with ADHD. Appl. Psychophysiol. Biofeedback 2016, 41, 17–25. [Google Scholar] [CrossRef]
- Lambez, B.; Harwood-Gross, A.; Golumbic, E.Z.; Rassovsky, Y. Non-pharmacological interventions for cognitive difficulties in ADHD: A systematic review and meta-analysis. J. Psychiatry Res. 2020, 120, 40–55. [Google Scholar] [CrossRef]
- Yan, L.; Wang, S.; Yuan, Y.; Zhang, J. Effects of neurofeedback versus methylphenidate for the treatment of ADHD: Systematic review ad meta-analysis of head-to-head trials. Medicine 2019, 97, 12623. [Google Scholar] [CrossRef] [PubMed]
- Van Doren, J.; Arns, M.; Heinrich, H.; Vollebregt, M.A.; Strehl, U.; Loo, L.K. Sustained effects of neurofeedback in ADHD: A systematic review and meta-analysis. Eur. Child Adolesc. Psychiatry 2019, 28, 293–305. [Google Scholar] [CrossRef] [Green Version]
- Vivani, G.; Vallesi, A. EEG-neurofeedback and executive function enhancement in healthy adults: A systematic review. Psychophysiology 2021, 58, 13874. [Google Scholar] [CrossRef] [PubMed]
- Danielson, M.L.; Visser, S.N.; Chronis-Tuscano, A.; DuPaul, G.J. A national description of treatment among United States children and adolescents with attention-deficit/hyperactivity disorder. J. Pediatrics 2018, 192, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Enriquez-Geppert, S.; Smit, D.; Garcia-Pimenta, M.; Arns, A. Neurofeedback as a treatment intervention in ADHD: Current evidence and practice. Curr. Psychiatry Rep. 2019, 21, 46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duric, N.S.; Abmus, J.; Elgen, I.B. Self-reported efficacy of neurofeedback treatment in a clinical randomized controlled study of ADHD children and adolescents. Neuropsychiatr. Dis. Treat. 2014, 10, 1645–1654. [Google Scholar] [CrossRef] [Green Version]
- Sterman, M.B. Epilepsy and its treatment with EEG feedback therapy. Ann. Behav. Med. 1986, 8, 21–25. [Google Scholar] [CrossRef]
- Jarrett, M.A.; Gable, P.A.; Rondon, A.T.; Neal, L.B.; Price, H.F.; Hilton, D.C. An EEG study of children with and without ADHD symptoms: Between-group differences and associations with sluggish cognitive tempo symptoms. J. Atten. Disord. 2017, 24, 1002–1010. [Google Scholar] [CrossRef]
- van Dijk, H.; deBeus, R.; Kerson, C.; Roley-Roberts, M.E.; Monastra, V.J.; Arnold, L.E.; Pan, X.; Arns, M. Different spectral analysis methods for the theta/beta ratio calculate different ratios but do not distinguish ADHD from controls. Appl. Psychophysiol. Biofeedback 2020, 45, 165–173. [Google Scholar] [CrossRef]
- Janssen, T.W.P.; Bink, M.; Weeda, W.D.; Geladé, K.; van Mourik, R.; Maras, A.; Oosterlaan, J. Learning curves of theta/beta neurofeedback in children with ADHD. Eur. Child Adolesc. Psychiatry 2017, 26, 573–582. [Google Scholar] [CrossRef] [Green Version]
- Doppelmayr, M.; Weber, E. Effects on SMR and theta/beta neurofeedback on reaction times, spatial abilities and creativity. J. Neurother. 2011, 15, 115–129. [Google Scholar] [CrossRef]
- Vernon, D.; Egner, T.; Cooper, N.; Compton, T.; Neilands, C.; Sheri, A.; Gruzelier, J. The effect of training distinct neurofeedback protocols on aspects of cognitive performance. Int. J. Psychophysiol. 2003, 47, 75–85. [Google Scholar] [CrossRef]
- Gevensleben, H.; Holl, B.; Albrecht, B.; Schlamp, D.; Kratz, O.; Studer, P.; Wangler, S.; Rothenberger, A.; Moll, G.H.; Heinrich, H. Distinct EEG effects related to neurofeedback training in children with ADHD: A randomized controlled trial. Int. J. Psychophysiol. 2009, 74, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Leins, U.; Goth, G.; Hinterberger, T.; Klinger, C.; Rumpf, N.; Strehl, U. Neurofeedback for children with ADHD: A comparison of SCP and theta/beta protocols. Appl. Psychophysiol. Biofeedback 2007, 32, 73–88. [Google Scholar] [CrossRef] [PubMed]
- Cortese, S.; Ferrin, M.; Brandeis, D.; Holtmann, M.; Aggensteiner, P.; Daley, D.; Santosh, P.; Simonoff, E.; Stevenson, J.; Stringaris, A.; et al. Neurofeedback for attention-deficit/hyperactivity disorder: Meta-Analysis of clinical and neuropsychological outcomes from randomized controlled trials. J. Am. Acad. Child Adolesc. Psychiatry 2016, 55, 444–455. [Google Scholar] [CrossRef] [Green Version]
- Logemann, H.N.; Lansbergen, M.M.; Van Os, T.W.; Bocker, K.B.; Kenemans, J.L. The effectiveness of EEG-feedback on attention, impulsivity and EEG: A sham feedback controlled study. Neurosci. Lett. 2010, 479, 49–53. [Google Scholar] [CrossRef] [PubMed]
- Holtmann, M.; Pniewski, B.; Wachtlin, D.; Wörz, S.; Strehl, U. Neurofeedback in children with attention-deficit/hyperactivity disorder (ADHD)–A controlled multicenter study of a non-pharmacological treatment approach. BMC Pediatrics 2014, 14, 202. [Google Scholar] [CrossRef] [Green Version]
- Su, Y.; Li, H.; Chen, Y.; Fang, F.; Xu, T.; Lu, H.; Xie, L.; Zhuo, J.; Qu, J.; Yang, L.; et al. Remission rate and functional outcomes during a 6-month treatment with osmotic-release oral-system methylphenidate in children with attention-deficit/hyperactivity disorder. J. Clin. Psychopharmacol. 2015, 35, 525–534. [Google Scholar] [CrossRef] [PubMed]
- Blume, F.; Hudak, J.; Dresler, T.; Ehlis, A.C.; Kühnhausen, J.; Renner, T.J.; Gawrilow, C. NIRS-based neurofeedback training in a virtual reality classroom for children with attention-deficit/hyperactivity disorder: Study protocol for a randomized controlled trial. Trials 2017, 18, 41. [Google Scholar] [CrossRef] [PubMed] [Green Version]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cabaleiro, P.; Cueli, M.; Cañamero, L.M.; González-Castro, P. A Case Study in Attention-Deficit/Hyperactivity Disorder: An Innovative Neurofeedback-Based Approach. Int. J. Environ. Res. Public Health 2022, 19, 191. https://doi.org/10.3390/ijerph19010191
Cabaleiro P, Cueli M, Cañamero LM, González-Castro P. A Case Study in Attention-Deficit/Hyperactivity Disorder: An Innovative Neurofeedback-Based Approach. International Journal of Environmental Research and Public Health. 2022; 19(1):191. https://doi.org/10.3390/ijerph19010191
Chicago/Turabian StyleCabaleiro, Paloma, Marisol Cueli, Laura M. Cañamero, and Paloma González-Castro. 2022. "A Case Study in Attention-Deficit/Hyperactivity Disorder: An Innovative Neurofeedback-Based Approach" International Journal of Environmental Research and Public Health 19, no. 1: 191. https://doi.org/10.3390/ijerph19010191
APA StyleCabaleiro, P., Cueli, M., Cañamero, L. M., & González-Castro, P. (2022). A Case Study in Attention-Deficit/Hyperactivity Disorder: An Innovative Neurofeedback-Based Approach. International Journal of Environmental Research and Public Health, 19(1), 191. https://doi.org/10.3390/ijerph19010191







