Mental Load and Fatigue Assessment Instruments: A Systematic Review
Abstract
:1. Introduction
The Present Study
2. Materials and Methods
2.1. Eligibility Criteria and Search Strategy
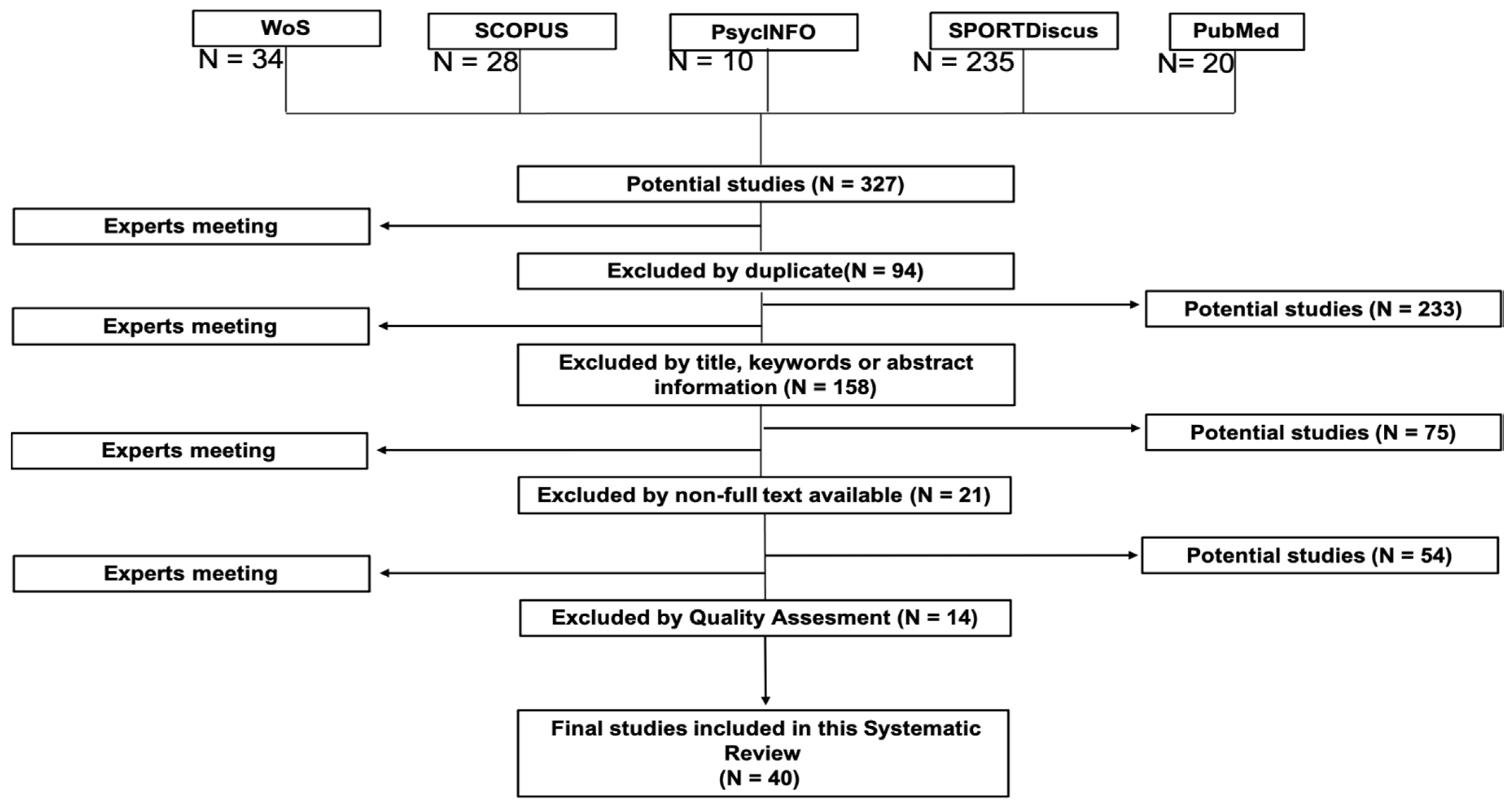
2.2. Study Selection and Data Collection Process
2.3. Data Synthesis
2.4. Quality Assessment
3. Results
3.1. Mental Load and Mental Fatigue Assessment Instruments for Subjective Derivations
3.2. Mental Load and Fatigue Assessment Instruments for Behavioral Derivations
3.3. Mental Load and Fatigue Assessment Instruments for Physiological Derivations
4. Discussion
4.1. Mental Load and Mental Fatigue Assessment Instruments for Subjective Derivations
4.2. Mental Load and Fatigue Assessment Instruments for Behavioral Derivations
4.3. Mental Load and Fatigue Assessment Instruments for Physiological Derivations
5. Strengths and Limitations
6. Practical Applications and Future Research
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ishii, A.; Tanaka, M.; Watanabe, Y. Neural mechanisms of mental fatigue. Rev. Neurosci. 2014, 25, 469–479. [Google Scholar] [CrossRef]
- Van Cutsem, J.; Roelands, B.; Pluym, B.; Tassignon, B.; Verschueren, J.O.; De Pauw, K.; Meeusen, R. Can creatine combat the mental fatigue-associated decrease in visuomotor skills? Med. Sci. Sports Exerc. 2020, 52, 120–130. [Google Scholar] [CrossRef]
- Pageaux, B.; Lepers, R. The effects of mental fatigue on sport-related performance. Prog. Brain Res. 2018, 240, 291–315. [Google Scholar] [PubMed]
- Hopstaken, J.F.; van der Linden, D.; Bakker, A.B.; Kompier, M.A. A multifaceted investigation of the link between mental fatigue and task disengagement. Psychophysiology 2015, 52, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Tran, Y.; Craig, A.; Craig, R.; Chai, R.; Nguyen, H. The influence of mental fatigue on brain activity: Evidence from a systematic review with meta-analyses. Psychophysiology 2020, 57, e13554. [Google Scholar] [CrossRef] [PubMed]
- Van Cutsem, J.; Marcora, S.; De Pauw, K.; Bailey, S.; Meeusen, R.; Roelands, B. The effects of mental fatigue on physical performance: A systematic review. Sport Med. 2017, 47, 1569–1588. [Google Scholar] [CrossRef] [Green Version]
- Van Cutsem, J.; Marcora, S. The effects of mental fatigue on sport performance. In Motivation and Self-Regulation in Sport and Exercise; Routledge: London, UK, 2021; pp. 134–148. [Google Scholar]
- Russell, S.; Kelly, V.G.; Halson, S.L.; Jenkins, D.G. Cognitive load in sport. Human Factors and Ergonomics in Sport: Applications and Future Directions; CRC Press: London, UK, 2020; pp. 181–200. [Google Scholar]
- McMorris, T. Cognitive fatigue effects on physical performance: The role of interoception. Sport Med. 2020, 50, 1703–1708. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Li, H.; Wang, H.; Umer, W.; Fu, H.; Xing, X. Evaluating the impact of mental fatigue on construction equipment operators’ ability to detect hazards using wearable eye-tracking technology. Autom. Constr. 2019, 105, 102835. [Google Scholar] [CrossRef]
- Ceballos-Vásquez, P.; Rolo-González, G.; Hernández-Fernaud, E.; Díaz-Cabrera, D.; Paravic-Klijn, T.; Burgos-Moreno, M.; Barriga, O. Validation of the Subjective Scale of Mental Workload (ESCAM) in health professionals in Chile. Univ. Psychol. 2016, 15, 261–270. [Google Scholar]
- Krell, M. Evaluating an instrument to measure mental load and mental effort considering different sources of validity evidence. Cogent Educ. 2017, 4, 1280256. [Google Scholar] [CrossRef]
- Sampei, K.; Ogawa, M.; Torres, C.; Sato, M.; Miki, N. Mental fatigue monitoring using a wearable transparent eye detection system. Micromachines 2016, 7, 20. [Google Scholar] [CrossRef] [Green Version]
- Käthner, I.; Wriessnegger, S.C.; Müller-Putz, G.R.; Kübler, A.; Halder, S. Effects of mental workload and fatigue on the P300, alpha and theta band power during operation of an ERP (P300) brain-computer interface. Biol. Psychol. 2014, 102, 118–129. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Lim, J.; Meng, J.; Kwok, K.; Thakor, N.; Bezerianos, A. Discriminative analysis of brain functional connectivity patterns for mental fatigue classification. Ann. Biomed. Eng. 2014, 42, 2084–2094. [Google Scholar] [PubMed]
- Grant, M.J.; Booth, A. A typology of reviews: An analysis of 14 review types and associated method-ologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, 332–336. [Google Scholar] [CrossRef] [Green Version]
- Booth, A. The pros and pros of registration on PROSPERO. BJOG Int. J. Obstet. Gynaecol. 2012, 119, 904–905. [Google Scholar]
- Booth, A.; Clarke, M.; Dooley, G.; Ghersi, D.; Moher, D.; Petticrew, M.; Stewart, L. PROSPERO at one year: An evaluation of its utility. Syst. Rev. 2013, 2, 4–11. [Google Scholar] [CrossRef] [Green Version]
- Gough, D.; Oliver, S.; Thomas, J. An Introduction to Systematic Reviews, 2nd ed.; SAGE: London, UK, 2012. [Google Scholar]
- Chalmers, I.; Altman, D.G. Systematic Reviews, 1st ed.; BMJ Publications: London, UK, 1995. [Google Scholar]
- Cohen, J. Weighted kappa: Nominal scale agreement with provision for scaled disagreement or partial credit. Psychol. Bull. 1968, 70, 213–220. [Google Scholar] [CrossRef]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Patel, A.N.; Howard, M.D.; Roach, S.M.; Jones, A.P.; Bryant, N.B.; Robinson, C.S.H.; Clark, V.P.; Pilly, P.K. Mental state assessment and validation using personalized physiological biometrics. Front. Hum. Neurosci. 2018, 12, 221. [Google Scholar] [PubMed]
- Kmet, L.M.; Lee, R.C. Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields; Edmont Alberta Herritage Foundation for Medical Research: Edmonton, AB, Canada, 2004. [Google Scholar]
- Chilcot, J.; Norton, S.; Kelly, M.E.; Moss-Morris, R. The Chalder Fatigue Questionnaire is a valid and reliable measure of perceived fatigue severity in multiple sclerosis. Mult. Scler. J. 2016, 22, 677–684. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.J.; Costa, E.; Menezes, P.R.; Chalder, T.; Bhugra, D.; Wessely, S. Cross-cultural validation of the Chalder Fatigue Questionnaire in Brazilian primary care. J. Psychosom. Res. 2007, 62, 301–304. [Google Scholar] [PubMed]
- Chiu, H.Y.; Li, W.; Lin, J.H.; Su, Y.K.; Lin, E.Y.; Tsai, P.S. Measurement properties of the Chinese version of the Mental Fatigue Scale for patients with traumatic brain injury. Brain Inj. 2018, 32, 652–664. [Google Scholar] [PubMed]
- Duan, W.; Mu, W. Validation of a Chinese version of the stress overload scale-short and its use as a screening tool for mental health status. Qual. Life Res. 2018, 27, 411–421. [Google Scholar] [PubMed]
- Fong, T.C.; Chan, J.S.; Chan, C.L.; Ho, R.T.; Ziea, E.T.; Wong, V.C.; Ng, B.F.; Ng, S.M. Psychometric properties of the Chalder Fatigue Scale revisited: An exploratory structural equation modeling approach. Qual. Life Res. 2015, 24, 2273–2278. [Google Scholar] [PubMed] [Green Version]
- Visser-Keizer, A.C.; Hogenkamp, A.; Westerhof-Evers, H.J.; Egberink, I.J.; Spikman, J.M. Dutch multifactor fatigue scale: A new scale to measure the different aspects of fatigue after acquired brain injury. Arch. Phys. Med. Rehabil. 2015, 96, 1056–1063. [Google Scholar] [CrossRef]
- Friedrich, M.; Nowe, E.; Hofmeister, D.; Kuhnt, S.; Leuteritz, K.; Sender, A.; Stobel-Richer, Y.; Geue, K. Psychometric properties of the fatigue questionnaire EORTC QLQ-FA12 and proposal of a cut-off value for young adults with cancer. Health Qual. Life Outcomes 2018, 16, 125. [Google Scholar] [CrossRef] [Green Version]
- Knobel, H.; Loge, J.H.; Brenne, E.; Fayers, P.; Hjermstad, M.J.; Kaasa, S. The validity of EORTC QLQ-C30 fatigue scale in advanced cancer patients and cancer survivors. Palliat. Med. 2003, 17, 664–672. [Google Scholar] [CrossRef] [PubMed]
- Porro, B.; Michel, A.; Zinzindohoué, C.; Bertrand, P.; Monrigal, E.; Trentini, F.; Baussard, L.; Cousson-Gélie, F. Quality of life, fatigue and changes therein as predictors of return to work during breast cancer treatment. Scand. J. Caring Sci. 2019, 33, 467–477. [Google Scholar] [PubMed]
- Zhang, M.; Sparer, E.H.; Murphy, L.A.; Dennerlein, J.T.; Fang, D.; Katz, J.N.; Caban-Martinez, A.J. Development and validation of a Fatigue Assessment Scale for U.S. construction workers. Am. J. Ind. Med. 2015, 58, 220–228. [Google Scholar] [CrossRef] [Green Version]
- Kauffman, B.Y.; Garey, L.; Nordan, A.; Jardin, C.; Mayorga, N.A.; Robles, Z.; Zvolensky, M.J. The development and initial validation of the Fatigue Sensitivity Questionnaire. Cogn. Behav. Ther. 2019, 48, 419–429. [Google Scholar] [CrossRef]
- Kumamoto, K.; Arai, Y. Validation of “personal strain” and “role strain”: Subscales of the short version of the Japanese version of the Zarit Burden Interview (J-ZBI_8). Psychiatry Clin. Neurosci. 2004, 58, 606–610. [Google Scholar] [CrossRef] [Green Version]
- Dębska, G.; Wilczek-Ruzyczka, E.; Foryś, Z.; Małgorzata, P. Psychometric properties assessment of the Meister questionnaire (Polish version) used in evaluating mental load among nurses. Med. Pracy 2013, 64, 349–358. [Google Scholar] [CrossRef]
- Bertram, D.A.; Hersey, C.O.; Opila, D.A.; Quirin, O. A measure of physician mental work load in internal medicine ambulatory care clinics. Med. Care 1990, 28, 458–467. [Google Scholar] [CrossRef]
- Chuang, L.L.; Chuang, Y.F.; Hsu, M.J.; Huang, Y.Z.; Wong, A.M.; Chang, Y.J. Validity and reliability of the traditional Chinese version of the multidimensional fatigue inventory in general population. PLoS ONE 2018, 13, e0189850. [Google Scholar] [CrossRef] [Green Version]
- Chung, K.F.; Yu, B.Y.M.; Yung, K.P.; Yeung, W.F.; Ng, T.H.; Ho, F.Y.Y. Assessment of fatigue using the Multidimensional Fatigue Inventory in patients with major depressive disorder. Compr. Psychiatry 2014, 55, 1671–1678. [Google Scholar] [CrossRef] [PubMed]
- Elbers, R.G.; van Wegen, E.E.H.; Verhoef, J.; Kwakkel, G. Reliability and structural validity of the Multidimensional Fatigue Inventory (MFI) in patients with idiopathic Parkinson’s disease. Park. Relat. Disord. 2012, 18, 532–536. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hagelin, C.; Wengström, Y.; Runesdotter, S.; Fürst, C. The psychometric properties of the Swedish Multidimensional Fatigue Inventory MFI-20 in four different populations. Acta Oncol. 2007, 46, 97–104. [Google Scholar] [PubMed]
- Gentile, S.; Delaroziere, J.C.; Favre, R.; Sambuc, R.; San Marco, J.L. Validation of the French “multidimensional fatigue inventory” (MFI 20). Eur. J. Cancer Care 2003, 12, 58–64. [Google Scholar] [CrossRef]
- Munch, T.N.; Strömgren, A.S.; Pedersen, L.; Petersen, M.A.; Hoermann, L.; Groenvold, M. Multidimensional measurement of fatigue in advanced cancer patients in palliative care: An application of the Multidimensional Fatigue Inventory. J. Pain Symptom Manag. 2006, 31, 533–541. [Google Scholar] [CrossRef] [PubMed]
- Schubart, J.R.; Schaefer, E.; Hakim, A.J.; Francomano, C.A.; Bascom, R. Use of cluster analysis to delineate symptom profiles in an Ehlers-Danlos Syndrome patient population. J. Pain Symptom Manag. 2019, 58, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Burke, S.E.; Samuel, I.B.H.; Zhao, Q.; Cagle, J.; Cohen, R.A.; Kluger, B.; Ding, M. Task-based cognitive fatigability for older adults and validation of mental fatigability subscore of pittsburgh fatigability scale. Front. Aging Neurosci. 2018, 10, 327. [Google Scholar] [PubMed] [Green Version]
- Lin, Y.; Cai, H. A method for building a real-time cluster-based continuous mental workload scale. Issues Erg. Sci. 2009, 10, 531–543. [Google Scholar]
- Yang, C.M.; Wu, C.H. The Situational Fatigue Scale: A different approach to measuring fatigue. Qual. Life Res. 2005, 14, 1357–1362. [Google Scholar]
- Couvy-Duchesne, B.; Davenport, T.A.; Martin, N.G.; Wright, M.J.; Hickie, I.B. Validation and psychometric properties of the Somatic and Psychological HEalth REport (SPHERE) in a young Australian-based population sample using non-parametric item response theory. BMC Psychiatry 2017, 17, 279. [Google Scholar] [CrossRef]
- Shuman-Paretsky, M.; Zemon, V.; Foley, F.W.; Holtzer, R. Development and validation of the State-Trait Inventory of Cognitive Fatigue in community-dwelling older adults. Arch. Phys. Med. Rehabil. 2017, 98, 766–773. [Google Scholar] [CrossRef] [Green Version]
- MeAuley, E.; Courneya, K.S. The Subjective Exercise Experiences Scale (SEES): Development and preliminary validation. J. Sport Exerc. Psychol. 1994, 16, 163–177. [Google Scholar]
- Abma, F.I.; Van Der Klink, J.J.; Bültmann, U. The Work Role Functioning Questionnaire 2.0 (Dutch Version): Examination of its reliability, validity and responsiveness in the general working population. J. Occup. Rehabil. 2013, 23, 135–147. [Google Scholar]
- Cimprich, B.; Visovatti, M.; Ronis, D.L. The attentional function index-a self-report cognitive measure. Psycho-Oncology 2011, 20, 194–202. [Google Scholar] [CrossRef] [Green Version]
- Di Stasi, L.L.; Renner, R.; Catena, A.; Cañas, J.J.; Velichkovsky, B.M.; Pannasch, S. Towards a driver fatigue test based on the saccadic main sequence: A partial validation by subjective report data. Transp. Res. Part C Emerg. Technol. 2012, 21, 122–133. [Google Scholar] [CrossRef]
- Puspasari, M.A.; Iridiastadi, H.; Sutalaksana, I.Z.; Sjafruddin, A. Effect of driving duration on EEG fluctuations. Int. J. Technol. 2017, 8, 1089–1096. [Google Scholar] [CrossRef] [Green Version]
- Price, E.; Moore, G.; Galway, L.; Linden, M. Validation of a smartphone-based approach to in situ cognitive fatigue assessment. JMIR mHealth uHealth 2017, 5, e125. [Google Scholar]
- Crocetta, T.B.; Viana, R.L.; Silva, D.E.; Monteiro, C.B.D.M.; Arab, C.; Andrade, A. Validade de software para medição do tempo de reação total com estímulo simples-TRT_S. J. Hum. Growth Dev. 2014, 24, 295–303. [Google Scholar]
- Neal, A.; Hannah, S.; Sanderson, P.; Bolland, S.; Mooij, M.; Murphy, S. Development and validation of a multilevel model for predicting workload under routine and nonroutine conditions in an air traffic management center. Hum. Factors 2014, 56, 287–305. [Google Scholar]
- Liu, J.; Gardi, A.; Ramasamy, S.; Lim, Y.; Sabatini, R. Cognitive pilot-aircraft interface for single-pilot operations. Knowledge-Based Syst. 2016, 112, 37–53. [Google Scholar]
- Gharagozlou, F.; Saraji, G.N.; Mazloumi, A.; Nahvi, A.; Nasrabadi, A.M.; Foroushani, A.R.; Kheradmand, A.; Ashouri, M.; Samavati, M. Detecting driver mental fatigue based on EEG Alpha power changes during simulated driving. Iran. J. Public Health 2015, 44, 1693–1700. [Google Scholar]
- Barte, J.C.M.; Nieuwenhuys, A.; Geurts, S.A.E.; Kompier, M.A.J. Motivation counteracts fatigue-induced performance decrements in soccer passing performance. J. Sports Sci. 2019, 37, 1189–1196. [Google Scholar] [CrossRef] [PubMed]
- Key, A.P.; Gustafson, S.J.; Rentmeester, L.; Hornsby, B.W.Y.; Bess, F.H. Speech-processing fatigue in children: Auditory event-related potential and behavioral measures. J. Speech Lang. Hear. Res. 2017, 60, 2090–2104. [Google Scholar] [CrossRef] [PubMed]
- Thompson, C.J.; Noon, M.; Towlson, C.; Perry, J.; Coutts, A.J.; Harper, L.D.; Skorski, S.; Smith, M.R.; Barrett, S.; Meyer, T. Understanding the presence of mental fatigue in English academy soccer players. J. Sports Sci. 2020, 38, 1524–1530. [Google Scholar] [CrossRef] [PubMed]
- Russell, S.; Jenkins, D.; Rynne, S.; Halson, S.L.; Kelly, V. What is mental fatigue in elite sport? Perceptions from athletes and staff. Eur. J. Sport Sci. 2019, 19, 1367–1376. [Google Scholar] [CrossRef] [PubMed]
- Van Cutsem, J.; De Pauw, K.; Buyse, L.; Marcora, S.; Meeusen, R.; Roelands, B. Effects of mental fatigue on endurance performance in the heat. Med. Sci. Sports Exerc. 2017, 49, 294–306. [Google Scholar] [CrossRef] [PubMed]
| Study | A | B | C | D | E | F | G | H | I | J | K | L | M | N | Quality Score | Quality Classification |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chilcot et al. (2016) [27] | 2 | 1 | 2 | 1 | N/A | N/A | N/A | 2 | 1 | 2 | 2 | N/A | 2 | 2 | 0.77 | Strong |
| Cho et al. (2007) [28] | 2 | 2 | 2 | 2 | N/A | N/A | N/A | 2 | 2 | 1 | 1 | N/A | 2 | 1 | 0.77 | Strong |
| Chiu et al. (2018) [29] | 2 | 2 | 2 | 2 | N/A | N/A | N/A | 2 | 1 | 2 | 1 | 2 | 2 | 2 | 0.91 | Strong |
| Duan and Mu (2018) [30] | 2 | 2 | 2 | 2 | 0 | N/A | 0 | 2 | 2 | 2 | 2 | N/A | 2 | 2 | 0.83 | Strong |
| Fong et al. (2015) [31] | 2 | 2 | 2 | 2 | 1 | N/A | N/A | 2 | 2 | 2 | 2 | N/A | 2 | 2 | 0.95 | Strong |
| Visser-Keizer et al. (2015) [32] | 2 | 2 | N/A | 2 | N/A | N/A | N/A | 2 | N/A | 2 | 2 | N/A | 2 | 2 | 1 | Strong |
| Friedrich et al. (2018) [33] | 2 | 2 | 2 | 2 | N/A | N/A | N/A | 2 | 2 | 2 | 2 | N/A | 2 | 2 | 1 | Strong |
| Knobel et al. (2003) [34] | 2 | 2 | 2 | 2 | 2 | N/A | N/A | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | Strong |
| Porro et al. (2019) [35] | 2 | 2 | 1 | 1 | N/A | N/A | N/A | 2 | 1 | 2 | 2 | N/A | 2 | 2 | 0.85 | Strong |
| Zhang et al. (2015) [36] | 2 | 2 | 1 | 2 | N/A | N/A | 0 | 0 | 1 | 2 | N/A | N/A | 1 | 2 | 0.65 | Moderate |
| Kauffman et al. (2019) [37] | 2 | 2 | 2 | 2 | N/A | N/A | N/A | 2 | 2 | 2 | 2 | N/A | 2 | 2 | 1 | Strong |
| Kumamoto and Arai (2004) [38] | 2 | 2 | 1 | 1 | N/A | N/A | N/A | 2 | 1 | 1 | 2 | N/A | 1 | 2 | 0.75 | Strong |
| Dębska et al. (2013) [39] | 2 | 2 | 1 | 1 | N/A | 0 | 0 | 1 | 2 | 2 | 0 | N/A | 2 | 2 | 0.75 | Strong |
| Bertram et al. (1990) [40] | 2 | 2 | 1 | 1 | N/A | N/A | N/A | 2 | 1 | 2 | 2 | N/A | 2 | 2 | 0.85 | Strong |
| Chuang et al. (2018) [41] | 2 | 2 | 2 | 2 | N/A | N/A | N/A | 2 | 2 | 2 | 2 | N/A | 2 | 2 | 1 | Strong |
| Chung et al. (2014) [42] | 2 | 2 | 2 | 2 | 2 | N/A | N/A | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 0.96 | Strong |
| Elbers et al. (2012) [43] | 2 | 2 | 2 | 2 | 2 | N/A | N/A | 2 | 1 | 2 | 2 | 1 | 2 | 2 | 0.92 | Strong |
| Hagelin et al. (2007) [44] | 2 | 2 | 2 | 1 | 1 | N/A | N/A | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 0.83 | Strong |
| Gentile et al. (2003) [45] | 2 | 2 | 2 | 2 | N/A | N/A | N/A | 1 | 2 | 2 | 2 | N/A | 2 | 2 | 1 | Strong |
| Munch et al. (2006) [46] | 2 | 2 | 2 | 1 | N/A | N/A | N/A | 2 | 2 | 2 | 2 | N/A | 2 | 2 | 0.95 | Strong |
| Schubart et al. (2019) [47] | 2 | 2 | 2 | 2 | N/A | N/A | N/A | 2 | 2 | 2 | 2 | N/A | 2 | 2 | 1 | Strong |
| Burke et al. (2018) [48] | 2 | 2 | 2 | 2 | N/A | N/A | N/A | 2 | 2 | 2 | 0 | N/A | 2 | 2 | 0.90 | Strong |
| Krell (2017) [12] | N/A | 2 | 2 | 2 | N/A | N/A | N/A | 2 | 2 | 2 | 2 | N/A | 2 | 2 | 0.90 | Strong |
| Lin and Cai, (2009) [49] | 2 | 1 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 0 | N/A | N/A | 0 | 0 | 0.30 | Weak |
| Yang and Wu (2005) [50] | 2 | 2 | 2 | 2 | N/A | N/A | N/A | 2 | 2 | 2 | N/A | N/A | 2 | 2 | 0.90 | Strong |
| Couvy-Duchesne et al. (2017) [51] | 2 | 2 | 2 | 1 | 2 | N/A | N/A | 1 | 2 | 2 | 1 | 1 | 2 | 2 | 0.83 | Strong |
| Shuman-Paretsky et al. (2017) [52] | 2 | 2 | 2 | 2 | N/A | N/A | N/A | 2 | 2 | 2 | 2 | N/A | 2 | 2 | 1 | Strong |
| Ceballos-Vásquez et al. (2016) [11] | 2 | 1 | 2 | 2 | N/A | N/A | N/A | 1 | 2 | 1 | 0 | N/A | 2 | 2 | 0.75 | Moderate |
| MeAuley and Courneya (1994) [53] | 1 | 2 | 2 | 2 | N/A | N/A | N/A | 1 | 2 | 1 | 2 | N/A | 2 | 2 | 0.85 | Strong |
| Abma et al. (2013) [54] | 2 | 2 | 2 | 0 | N/A | 0 | N/A | 2 | 2 | 2 | N/A | N/A | 2 | 2 | 0.80 | Strong |
| Cimprich et al. (2011) [55] | 2 | 2 | 2 | 2 | N/A | N/A | N/A | 1 | 2 | 2 | 2 | N/A | 2 | 2 | 0.79 | Strong |
| Di Stasi et al. (2012) [56] | 2 | 1 | 1 | 2 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | N/A | 2 | 2 | 0.46 | Weak |
| Puspasari et al. (2017) [57] | 2 | 2 | 1 | 1 | 0 | 0 | 0 | 2 | 1 | 2 | 1 | N/A | 2 | 2 | 0.62 | Moderate |
| Price et al. (2017) [58] | 1 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 0 | 2 | 1 | N/A | 2 | 2 | 0.77 | Strong |
| Crocetta et al. (2014) [59] | 2 | 1 | 2 | 2 | N/A | N/A | N/A | 2 | 2 | 2 | 2 | N/A | 2 | 2 | 0.95 | Strong |
| Neal et al. (2014) [60] | 2 | 2 | 1 | 2 | 0 | 0 | 0 | 2 | 1 | 2 | 2 | N/A | 2 | 2 | 0.69 | Moderate |
| Liu et al. (2016) [61] | 2 | 2 | N/A | 1 | N/A | N/A | N/A | N/A | N/A | 2 | N/A | N/A | 2 | 2 | 0.69 | Moderate |
| Gharagozlou et al. (2015) [62] | 2 | 2 | 2 | 1 | N/A | 0 | 0 | 0 | 1 | 2 | 0 | N/A | 2 | 2 | 0.58 | Moderate |
| Patel et al. (2018) [25] | 2 | 2 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 2 | 1 | N/A | 1 | 2 | 0.54 | Moderate |
| Sun et al. (2014) [15] | 1 | N/A | N/A | 2 | N/A | N/A | N/A | 2 | N/A | 2 | 2 | N/A | 2 | 2 | 0.59 | Moderate |
| Mental Load or Fatigue Instrument | Authors | Sample | Instruments Used to Compare | Results | Conclusions |
|---|---|---|---|---|---|
| Chalder Fatigue Questionnaire (CFQ) | Chilcot et al. (2016) | 444 participants with multiple sclerosis (M = 45.15, SD = 12.35). |
| Reliability coefficients for mental and physical subscales were both 0.96. | CFQ is a valid and reliable instrument to measure fatigue severity in people with multiple sclerosis. |
| Cho et al. (2007) | 207 primary care patients, between 18 and 45 years old. |
| The Brazilian CFQ’s internal consistency improved slightly from the pilot study to the validation study: Cronbach’s alpha from 0.86 to 0.88. | Brazilian CFQ had good reliability and validity, which have improved during the intercultural adaptation and validation process. | |
| Chinese Mental Fatigue Scale (CMFS) | Chiu et al. (2018) | 150 traumatic brain-injured adults for 6 months (M = 50.90). |
| Correlations between the items and the total scores ranged from 0.48 to 0.81 for the 13-item MFS (all p < 0.001). | CMFS has satisfactory statistical properties to quantify mental fatigue in traumatic brain-injured patients. |
| Chinese version of Stress Overload Scale-Short(SOS-SC) | Duan and Mu (2018) | 1364 adults (M = 40.00; SD = 7.60). |
| Personal vulnerability and workload were positively and significantly correlated with the score of SOS-SC. | SOS-SC can be used to measure stress and mental health status in the Chinese population. |
| Chronic Fatigue Syndrome (CFS) Chinese Version | Chiu et al. (2018) | 150 traumatic brain-injured adults for 6 months (M = 50.90). |
| Correlations between the items and the total scores ranged from 0.39 to 0.81 for the 14-item CMFS (p < 0.001) | CFS has satisfactory statistical properties to quantify mental fatigue in traumatic brain-injured patients. |
| Fong et al. (2015) | 1259 adults from different jobs (M = 43.0, SD = 8.0). |
| Three factors of CFS (physical fatigue, low energy, and mental fatigue) were positively correlated with anxiety (r = 0.32–0.47, p < 0.01), depression (r = 0.31–0.50, p < 0.01), and exhaustion (r = 0.41–0.59, p < 0.01), and weakly correlated with sleep disorders (r = 0.21 –0.30, p < 0.01). | CFS is a valid measure of fatigue symptoms in the general population. | |
| Dutch Multifactor Fatigue Scale | Visser-Keizer et al. (2015) | 148 participants, 9 with stroke, 5 with traumatic brain injury, 55 with ischemic stroke, 22 with hemorrhagic stroke, 22 with acquired brain injury, and 35 with traumatic brain injury. | No | Good reliability is shown for mental fatigue (ICC > 0.80). Patients without injuries reported significantly greater mental fatigue than patients with injury. | This questionnaire diagnoses fatigue. |
| EORTC QLQ-FA12 quality of life questionnaire | Friedrich et al. (2018) | 577 participants (M = 30.3, SD = 6.1). |
| The cognitive fatigue items’ reliability ranged from 0.45 to 0.73. The correlations between the three scales ranged between 0.63 and 0.70. Cronbach’s alpha for cognitive fatigue was 0.73. | This instrument can discriminate between physical, emotional, and cognitive fatigue. |
| Knobel et al. (2003) | 238 advanced cancer patients and 128 cancer survivors (M = 52.50). |
| FA scale correlated between 0.49 and 0.75 at all assessment points with the Physical Fatigue (PF) and Mental Fatigue (MF) scales of the FQ. | EORTC QLQ C30 fatigue scale meaasures fatigue as part of an overall fatigue assessment. | |
| Porro et al. (2019) | 68 breast cancer patients (M = 46.97, SD = 6.92). |
| Univariate analyzes showed Return To Work (RTW) probability was reduced by high scores for mental fatigue, r = 0.85, p <0.05. Only the change in mental fatigue during treatment influenced the RTW probability. | Attention should be paid to the use of validated scales to evaluate mental constructs. | |
| Fatigue Assessment Scale for Construction Workers (FASCW). | Zhang et al. (2015) | 144 unionized construction workers in New England, from 19 to 60 years (M = 42.4; SD = 10.3). |
| Results indicated significant high correlations between FASCW and the Fatigue subscale of POMS and the measure of RPE. | FASCW is a promising instrument for assessing a general concept of fatigue. |
| Functional Status Questionnaire | Kauffman et al. (2019) | 1287 undergraduate students (M = 21.68, SD = 4.54). |
| FSQ had excellent internal consistency (α = 0.92). Total FSQ score was positively associated with anxiety sensitivity (r = 0.49), general depression (r = 0.37), social anxiety (r = 0.40), panic (r = 0.43), and negative affectivity (r = 0.37). | FSQ may be a valid and promising approach to better understand the implications of fatigue in real-world contexts (e.g., primary care). |
| J-ZBI-8 Questionnaire | Kumamoto and Arai (2004) | 315 subjects who lived with primary caregivers (M = 81.2, SD = 7.5). | No | No clear relationship between the nursing care load and nursing time was found. This relationship is significantly related to the attention load. | The J-ZBI _ 8 questionnaire has two subscales whose factorial structure is clearly defined. |
| Meister Questionnaire | Dębska et al. (2013) | 211 nurses (M = 43.1, SD = 7.26). |
| Cronbach’s alpha was 0.83 for the total score. | Meister questionnaire meets the psychometric criteria of reliability and validity to assess mental load in nurses. |
| Mental WorkLoad Instrument. | Bertram et al. (1990) | 48 patients admitted to clinical care, between 31 and 45 years old. | No | Significant correlations were observed between the work demand, satisfaction, and self-perceived performance. | Mental workload correlated directly and inversely with both satisfaction and the self-rated quality of the patient care provided. |
| MFI | Chuang et al. (2018) | 123 participants (43 males and 80 females; M = 46.12, SD = 18.40). |
| Results showed moderate convergent validity by correlating fatigue with quality of life, including sleep. | Results support the use of the MFI traditional Chinese version as an integral instrument to measure specific fatigue aspects. |
| Chung et al. (2014) | 137 major depressive disorder (MDD) patients (M = 49.6, SD = 9.6). |
| MFI-20 has good internal consistency (Cronbach’s alpha = 0.89). Suitable concurrent validity, significant correlations between MFI-20 scores and depressive and anxiety symptoms, general health, and quality of life. | MFI-20 is a valid and reliable instrument to assess fatigue in MDD patients with residual symptoms. | |
| Elbers et al. (2012) | 153 patients diagnosed with Parkinson’s disease (M = 67.07, SD = 7.54). | No | All subscales showed suitable internal consistency reflected by a Cronbach range of 0.74 to 0.92. | MFI is a reliable and valid instrument to evaluate the multidimensional aspects of fatigue in Parkinson patients. | |
| Hagelin et al. (2007) | 594 cancer patients (M = 59.50). |
| Cronbach values in the MFI-20 ranged between 0.67 and 0.94. The correlation between the MFI-20 subscales and the CR-10 scores ranged between 0.37 and 0.74. | MFI-20 Swedish version is a valid and reliable instrument for measuring fatigue in different patient populations and in healthy individuals. | |
| Gentile et al. (2003) | 225 participants (M = 52, SD = 15). |
| Correlations between each subscale and VAS are highly significant (p < 0.001). | MFI French version shows that this instrument is valid for clinical application. | |
| Munch et al. (2006) | 278 advanced cancer patients (M = 64). |
| The two psychological subscales of MFI-20, Mental Fatigue and Reduced Motivation, were significantly associated with each other. Only General Fatigue and Mental Fatigue correlated significantly with the HADS Anxiety subscale. | MFI-20 may be a useful tool for further research on fatigue etiology. | |
| Schubart et al. (2019) | 175 patients with Ehlers-Danlos Syndromes (M = 42.40). |
| Mental fatigue was correlated with pain (r = 0.16), night sleep (r = 0.20), daily sleep (r = 0.35), and dysautonomia (r = 0.36). | This research shows the relation between mental fatigue and other constructs. | |
| Pittsburgh Fatigability Scale (PFS). | Burke et al. (2018) | 35 healthy old people (M = 73.77, SD = 5.9). |
| PFS mental fatigue subscores highly correlated with the EES scores (ρ = 0.63, p < 0.001). PFS mental fatigue scores also correlated with the MFIS cognitive score (ρ = 0.36, p = < 0.05). | The lack of correlation between task-based fatigability measures and the PFS Mental subscale may indicate that mental fatigue is difficult to capture using questions about fatigue based on previous or imaginary experiences. |
| Mental Load (ML) and Mental Effort (ME) Questionnaire of Students in Biology Education (StuMMBE-Q). | Krell (2017) | 602 students (9 and 10 school grades; from 13 to 18 years old; 52% females). | No | Results suggest that StuMMBE-Q classifies students who report low, medium, and high levels of ML and ME. | Findings suggest that the questionnaire measures two theoretically established cognitive load dimensions (mental load and mental effort) well. |
| Rating Scale Mental Effort (RSME) | Lin and Cai (2009) | Drivers. |
| Correlation coefficient between RSME and ECG is 0.85. ECG and CBC-MWL measurement show a high correlation with the RSME score. | Proposed method is consistent with the RSME method but RSME cannot be completed in real time. |
| Situational Fatigue Scale | Yang and Wu (2005) | 96 patients (M = 31.10, SD = 10.0) and 62 university students (M = 21.0, SD = 1.99). |
| Cronbach coefficients indicated good internal consistency for the global scale (0.90), as well as for the PFSubescale (0.88) and the MFS (0.89). | SFS presents a new way to measure fatigue dimension that is different from what is measured with conventional fatigue rating scales. |
| Somatic and Psychological Health Report. | Couvy-Duchesne et al. (2017) | 5148 participants (M = 15.52; SD = 0.75). | No | Questionnaire could be reduced to 21 items. | This questionnaire could be relevant to assess anxiety, depression, and chronic fatigue. |
| State-Trait Inventory for Cognitive Fatigue (STI-CF). | Shuman-Paretsky et al. (2017) | 175 participants, over 65 years old (M = 77.35, SD = 6.91). |
RBANS | The 4 components (cognitive fatigue, mental effort, motivation, and boredom) had good reliability. Strong positive relationship between cognitive fatigue and a subjective measure of general fatigue (p < 0.001). | The STI-CF had significant relationships in the expected direction with several variables of cognitive and health outcomes. |
| Subjective Exercise Experiences Scale (SEES). | MeAuley and Courneya (1994) | 454 university students (M = 20.78; SD = 2.18). | No | The comparison between the three scales of SEES showed their reliability: Positive Well-Being (PWB) α = 0.36, Psychological Distress (PD) α = 0.25, and Fatigue α = 0.88. | Three dimensions of the SEES provide initial support for the multidimensional measurement of the capacity of psychological response to the properties of exercise stimulus: Positive well-being, psychological distress, and fatigue. |
| Subjective Scale of Mental Workload (SCA) | Ceballos-Vásquez et al. (2016) | 379 workers (M = 37.36; SD = 10.53) of Critical Patient Units (UPC) of three Chilean hospitals. |
| There are positive and significant correlations between the global mental load scores and all the psychosocial dimensions of the SUSESO-ISTAS 21 (p < 0.05). | SCAM presents high reliability and suitable validity in a Chilean sample for mental load evaluation. |
| WRFQ | Abma et al. (2013) | 553 workers between 18 and 64 years old who worked 12 h weekly. |
| Cronbach’s alpha coefficients were calculated for each WRFQ subscale and the total score (ideal, between 0.70 and 0.95). | WRFQ 2.0 is a reliable and valid instrument to measure the health-related work functioning in the working population in general. |
| Mental Load or Fatigue Instrument | Authors | Sample | Instruments Used to Compare | Results | Conclusions |
|---|---|---|---|---|---|
| Attentional Function Index (AFI) | Cimprich et al. (2011) | 172 women diagnosed with breast cancer. Ages between 27 and 86 years old. | No | Internal consistency coefficient (Cronbach’s α) for the revised 13-item scale was 0.92, indicating satisfactory reliability. | Findings indicate that AFI is a valid and reliable measure to assess the perceived detrimental effects of cognitive dysfunction in chronic and life-threatening diseases, such as breast cancer. |
| Eyelink 1000 Remote Eye Tracking System | Di Stasi et al. (2012) | 10 healthy volunteers. Five women and five men (M = 23.9, SD = 4.9). |
| The peak velocity of saccadic eye movements decreased after driving (p < 0.05), due to mental fatigue. | Saccadic eye parameters, particularly the peak velocity, are a sensitive indicator of mental fatigue. |
| Logitech Driving Simulator with Citycar Driving software | Puspasari et al. (2017) | Seven commercial drivers, between 25 and 35 years old. |
| All measured parameters showed significant changes related to driving duration (p < 0.05). | Results show alpha, beta, theta, and delta bands are significantly different before and after driving, with an increase in the theta-delta band and a decrease in the alpha-beta band. These correlate with poor driving performance. |
| Psychomotor Vigilance Test (PVT) | Price et al. (2017) | 21 participants (M = 22, SD = 4). |
| Only the mobile test PVT is valid and reliable to assess cognitive accuracy. The arithmetic test does not show a strong correlation with MFS. | The mobile application is considered a potentially effective tool for the individual assessment of cognitive fatigue levels More continuity in time is needed and the test must be carried out daily. |
| TRT_S software | Crocetta et al. (2014) | 216 university students, between 17 and 45 years old (M = 24, SD = 6). |
| Intraclass coefficient correlation of TRT in young adults showed a strong correlation between Simple TRT and VTS (r = 0.72). | Results confirmed the TRT_S 2012 software’s validity, as a reliable cognitive test to assess the influence of mental fatigue on cognitive performance. |
| Mental Load or Fatigue Instrument | Authors | Sample | Instruments Used to Compare | Results | Conclusions |
|---|---|---|---|---|---|
| Air Traffic Workload Input Technique | Neal et al. (2014) | 16 licensed air traffic controllers. |
| The model explained 42% of the variance in workload after controlling for differences among raters. | The final model provided a reasonable fit to the data, despite including only five predictors. It can thus be considered a multilevel unified dynamic density model. |
| Cognitive Pilot-Aircraft Interface (CPAI) procedures. | Liu et al. (2016) | Airplane pilots. | No | Higher heart rates are related to higher fatigue levels and the flickering speed demonstrates a similar relationship. For mental fatigue, the heart rate is more important than the blink rate. | Simulation results demonstrate a preliminary validity of CPAI system for this purpose. Estimated human cognitive states are consistent both with external conditions and physiological states. |
| EEG | Gharagozlou et al. (2015) | 12 healthy male drivers (M = 23.8, SD =1.44; from 20 to 30 years old). Subjects had a valid driver’s license with at least 2 years driving experience and had no brain injuries history. |
| Significant increase in absolute alpha power (p = 0.006), as well as in F-VAS scores were observed during the final driving section (p = 0.001). | The study suggested that variations in alpha power could be a good indicator of drivers’ mental fatigue. |
| Patel et al. (2018) | 18 participants of different jobs |
| The use of EEG spectral power in all bands obtains better performance for mental fatigue assessment (p < 0.001). | The use of EEG spectral power characteristics across the entire range of physiological bands allows a better representation of all mental states. | |
| Sun et al. (2014) | 26 right-handed and neurologically normal participants (M = 22.20; SD = 1.53). | No | Few functional connections were significantly associated with mental fatigue (p > 0.05). | Viability demonstration of a method of assessing mental fatigue based on functional connectivity. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Díaz-García, J.; González-Ponce, I.; Ponce-Bordón, J.C.; López-Gajardo, M.Á.; Ramírez-Bravo, I.; Rubio-Morales, A.; García-Calvo, T. Mental Load and Fatigue Assessment Instruments: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 419. https://doi.org/10.3390/ijerph19010419
Díaz-García J, González-Ponce I, Ponce-Bordón JC, López-Gajardo MÁ, Ramírez-Bravo I, Rubio-Morales A, García-Calvo T. Mental Load and Fatigue Assessment Instruments: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(1):419. https://doi.org/10.3390/ijerph19010419
Chicago/Turabian StyleDíaz-García, Jesús, Inmaculada González-Ponce, José Carlos Ponce-Bordón, Miguel Ángel López-Gajardo, Iván Ramírez-Bravo, Ana Rubio-Morales, and Tomás García-Calvo. 2022. "Mental Load and Fatigue Assessment Instruments: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 1: 419. https://doi.org/10.3390/ijerph19010419
APA StyleDíaz-García, J., González-Ponce, I., Ponce-Bordón, J. C., López-Gajardo, M. Á., Ramírez-Bravo, I., Rubio-Morales, A., & García-Calvo, T. (2022). Mental Load and Fatigue Assessment Instruments: A Systematic Review. International Journal of Environmental Research and Public Health, 19(1), 419. https://doi.org/10.3390/ijerph19010419









