The Great Lockdown in the Wake of COVID-19 and Its Implications: Lessons for Low and Middle-Income Countries
Abstract
:1. Introduction
2. Methodology
2.1. Case Study Area
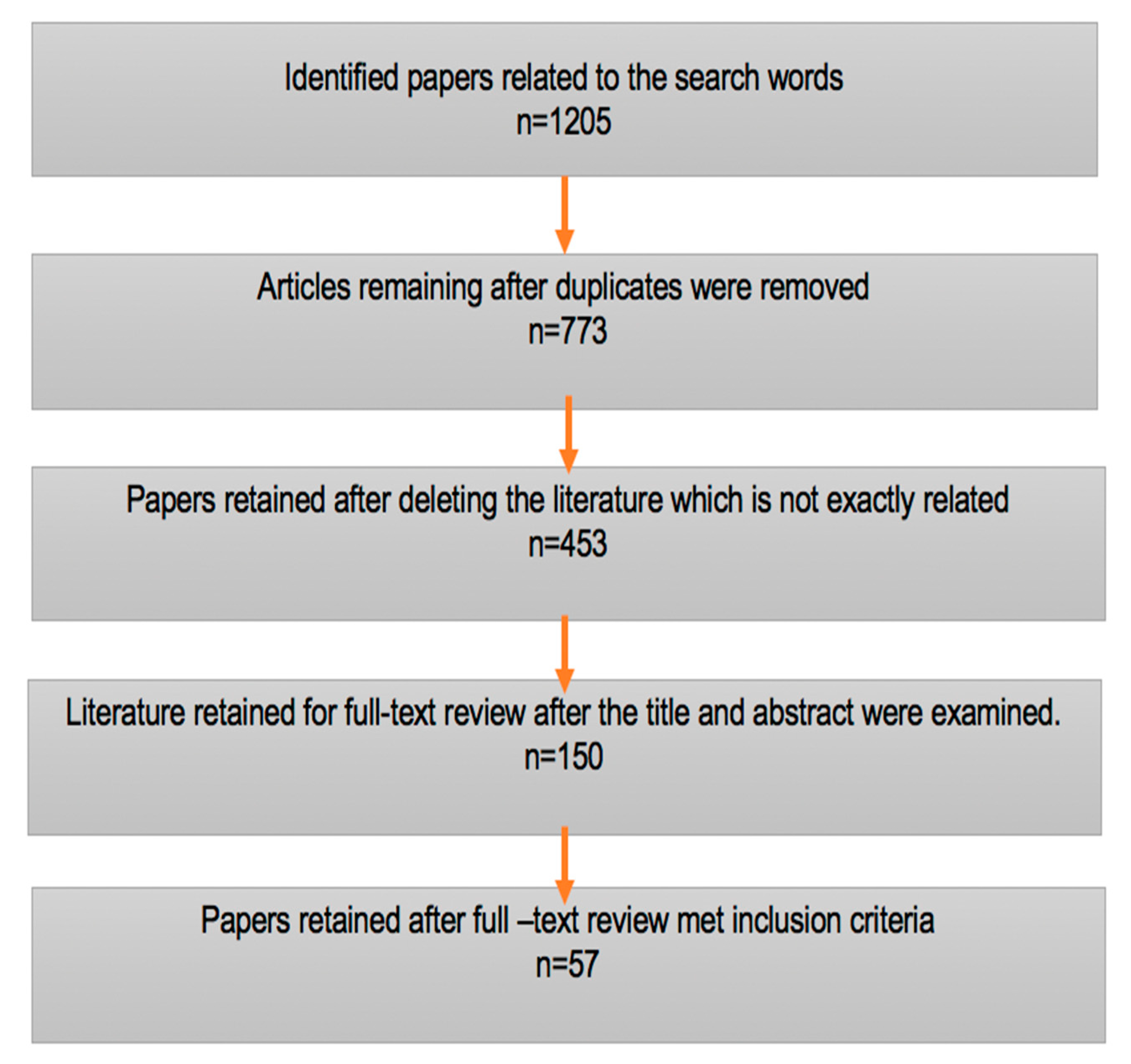
2.2. Literature Searches
- COVID-19 and India
- Lockdown and India
- Lockdown and health impacts in rural India
- Migrants and greater lockdown
2.3. Study Limitations
3. Results and Discussion
3.1. The Great Lockdown and Its Economic Impact
3.2. Implications of the Lockdown
3.3. Migrant Workers
3.3.1. Road Traffic Accidents
3.3.2. Lockdown and Travel Home
3.4. Health Implications
- Sudden job losses have resulted in the depletion of income and severe difficulties for millions of urban and rural populations, most of whom work without contracts in the informal sector [36]. As a consequence, several million informal workers and their families have experienced poverty, hunger and acute undernourishment.
- Domestic conflict, violence and depression have also increased [37].
- Health inequalities have exposed vulnerable groups to more risk. It is time to recognise the contribution of the informal sector to the national economy. Lockdown has shattered the mental health of a large population and has increased chances of exposure to a disturbed daily routine, which results in reduced human happiness and well-being [15].
- The approaches to address COVID-19 and management of COVID 19 may generate inequalities, as well as problems in health services, interrupt essential regular operations and require redistribution of existing healthcare workers across health systems. The impact of the pandemic also has consequences for routine non-COVID-19 health services. In low-income contexts, this has meant people spending excessive amounts of time waiting for, e.g., antenatal treatment, contraceptive counselling or reproductive health facilities in crowded hospitals, which further raises the risk of spreading infection.
- Fear and stress result in a higher risk to individuals of experiencing both physical and mental health issues [11].
- Misinformation related to COVID-19 has been spread partly due to fear, stigma and anxieties [38].
- People suspected of having COVID-19 infections experience an increased level of stigma [39].
- The ICMR stated that India tests 24 people per one positive, while Japan tests 11 people for one positive, Italy tests 24 people for seven positives and the USA tests 24 people for 5.3 positives; in comparison with other countries, there have been fewer COVID-19 cases per test in India [42].
- During the pandemic, one out of every ten women in India polled needed domestic abuse services.
- Mid-day meals were stopped in schools, which has disproportionately affected poorer children’s health, as well as malnutrition among children [43].
3.5. What Is Special in the ‘Shramik Special’?
4. Policy Implications for Migrant Workers
5. Policy Implications and the Critical Role of the Public Sector
- Individuals should have easy access to critical pandemic-fighting goods, like face masks and hand sanitizer, and adequate testing facilities should be provided to the public [50].
- The COVID-19 pandemic complicates the existing healthcare service delivery system. Interdisciplinary research and scientific investigation are necessary to understand the situation. To minimize the pandemic impact, the neglected tropical diseases community, particularly in low- and middle-income countries, must respond quickly, wisely and collaboratively with decision makers and key stakeholders across sectors [13].
- To address the pandemic situation, which necessitates new and innovative responses from stakeholders, multi-stakeholder participation in pandemic management must be investigated. Multi-stakeholder and spatial decision support systems have proven to be an effective model for identifying potential pandemic sources and regulating worldwide spread. To address COVID-19, transdisciplinary approaches to structuring and decision making tend to be very helpful. Furthermore, conceptual multi-stakeholder and spatial decision support systems can help enrich crisis-management decision making by bringing out a synergic link amongst multi-stakeholders [19].
- Increasing capacity for income generation, improving working conditions for labour and easy access to public services are required. Tailored packages for vulnerable populations (informal sector, small and micro-entrepreneurs, women, indigenous populations) have to be created to support them.
- Empirical analysis suggests that proper management of reverse migrants and an increased role of people’s participation in adhering to social distancing are important for restricting COVID 19 cases [18].
- The government has a crucial role in encouraging and facilitating participation of the public. With the unlocking process in force, migrant workers will again try to move to seek jobs. The government needs to ensure they have databases of labour movements and safety and social distancing measures in the workplace.
- The concept of health has to be expanded beyond biomedicine and hospital costs to reflect the direct and indirect cost of health impacts.
- The pandemic challenges of the international community have to be handled with global cooperation and security.
- Investment in emergency preparedness is needed to manage the crisis. Coordinated funding in public health emergencies can improve access to measurement, prevention, treatment and control of the virus.
- Funding the resumption of economic activity requires financial supports, such as by providing easy access to credit through the Credit Guarantee Fund Trust Scheme to SMES (small and medium enterprises).
- The government and the Reserve Bank of India (RBI) have taken a number of steps, including a moratorium loan forgiveness regulatory forbearance, updated NPA (non-performing asset) laws and easing the credit cycle, but these steps must be implemented properly.
- If necessary, measures are not taken to manage the crisis, it can lead to a national emergency. Linkages between all levels of state and non-state actors are critical for ensuring the population’s health and safety. The need for early public health countermeasures and mitigation of the spread of the virus has highlighted the appropriateness of support by state, local and other health departments.
6. Scope for Future Research
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Di Gennaro, F.; Pizzol, D.; Marotta, C.; Antunes, M.; Racalbuto, V.; Veronese, N.; Smith, L. Coronavirus diseases (COVID-19) current status and future perspectives: A narrative review. Int. J. Environ. Res. Public Health 2020, 17, 2690. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferguson, N.; Laydon, D.; Nedjati Gilani, G.; Imai, N.; Ainslie, K.; Baguelin, M.; Bhatia, S.; Boonyasiri, A.; Cucunuba Perez, Z.; Cuomo-Dannenburg, G. Report 9: Impact of Non-Pharmaceutical Interventions (NPIs) to Reduce COVID-19 Mortality and Healthcare Demand. 2020. Available online: https://int.artloft.co/wp-content/uploads/2021/07/Imperial-College-COVID19-NPI-modelling-16-03-2020.pdf (accessed on 6 April 2021).
- LePan, N. A Visual History of Pandemics, Word Economic Forum: 2020. Available online: https://www.weforum.org/agenda/2020/03/a-visual-history-of-pandemics (accessed on 6 April 2021).
- Awasthi, P. COVID-19 is 3.5 times deadlier than influenza: Study. The Hindu: Business Line, 12 February 2021. [Google Scholar]
- WHO. COVID-19 World Helath Organization—Country India. Available online: https://covid19.who.int/region/searo/country/in (accessed on 22 December 2021).
- Gov.India. COVID-19 Cases across India. Available online: https://www.mygov.in/covid-19 (accessed on 22 December 2021).
- Deshpande, A. What Does Work-From-Home Mean for Women? Econ. Political Wkly. 2020, 55, 1–7. [Google Scholar]
- UNCTAD. From the Great Lockdown to the Great Meltdown: Developing Country Debt in the Time of COVID-19. Trade and Development Report Update; United Nations Conference on Trade and Development: Geneva, Switzerland, 2020; pp. 1–16. Available online: https://digitallibrary.un.org/record/3866343?ln=en (accessed on 28 July 2020).
- Hevia, C.; Neumeyer, A. A Conceptual Framework for Analyzing the Economic Impact of COVID-19 and Its Policy Implications. 2020, pp. 1–18. Available online: https://www.latinamerica.undp.org/content/rblac/en/home/library/crisis_prevention_and_recovery/a-conceptual-framework-for-analyzing-the-economic-impact-of-covi.html (accessed on 18 September 2020).
- Aneja, R.; Ahuja, V. An assessment of socioeconomic impact of COVID-19 pandemic in India. J. Public Affairs 2021, 21, e2266. [Google Scholar] [CrossRef]
- Bhat, B.A.; Khan, S.; Manzoor, S.; Niyaz, A.; Tak, H.; Anees, S.; Gull, S.; Ahmad, I. A study on impact of COVID-19 lockdown on psychological health, economy and social life of people in Kashmir. Int. J. Sci. Healthc. Res. 2020, 5, 36–46. [Google Scholar]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. Available online: https://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(20)30460-8.pdf (accessed on 18 September 2020). [CrossRef] [Green Version]
- Ehrenberg, J.P.; Utzinger, J.; Fontes, G.; da Rocha, E.M.M.; Ehrenberg, N.; Zhou, X.-N.; Steinmann, P. Efforts to mitigate the economic impact of the COVID-19 pandemic: Potential entry points for neglected tropical diseases. Infect. Dis. Poverty 2021, 10, 1–10. [Google Scholar] [CrossRef]
- Lau, H.; Khosrawipour, V.; Kocbach, P.; Mikolajczyk, A.; Schubert, J.; Bania, J.; Khosrawipour, T. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J. Travel Med. 2020, 27, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Posel, D.; Oyenubi, A.; Kollamparambil, U. Job loss and mental health during the COVID-19 lockdown: Evidence from South Africa. PLoS ONE 2021, 16, e0249352. [Google Scholar] [CrossRef] [PubMed]
- Ramaci, T.; Barattucci, M.; Ledda, C.; Rapisarda, V. Social stigma during COVID-19 and its impact on HCWs outcomes. Sustainability 2020, 12, 3834. [Google Scholar] [CrossRef]
- Sengupta, S.; Jha, M.K. Social Policy, COVID-19 and Impoverished Migrants: Challenges and Prospects in Locked Down India. Int. J. Community Soc. Dev. 2020, 2, 152–172. [Google Scholar] [CrossRef]
- Varkey, R.S.; Joy, J.; Sarmah, G.; Panda, P.K. Socioeconomic determinants of COVID-19 in Asian countries: An empirical analysis. J. Public Affairs 2020. [Google Scholar] [CrossRef] [PubMed]
- Panneer, S.; Kantamaneni, K.; Pushparaj, R.R.B.; Shekhar, S.; Bhat, L.; Rice, L. Multistakeholder Participation in Disaster Management—The Case of the COVID-19 Pandemic. Healthcare 2021, 9, 203. [Google Scholar] [CrossRef]
- Dev, S.M.; Sengupta, R. Covid-19: Impact on the Indian Economy. 2020, pp. 1–50. Available online: http://www.igidr.ac.in/pdf/publication/WP-2020-013.pdf (accessed on 15 November 2020).
- Sen, A.; Rajan, R.; Banerjee, A. Huge Numbers May Be Pushed into Dire Poverty or Starvation… We Need to Secure Them. The Indian Express, 17 April 2020. Available online: https://indianexpress.com/article/opinion/coronavirus-india-lockdown-economy-amartya-sen-raghuram-rajan-abhijit-banerjee-6364521/(accessed on 18 September 2020).
- Hossain, M.M.; Purohit, N.; Sharma, R.; Bhattacharya, S.; McKyer, E.L.J.; Ma, P. Suicide of a Farmer Amid COVID-19 in India: Perspectives on Social Determinants of Suicidal Behavior and Prevention Strategies. 2020. Available online: https://www.researchgate.net/publication/341284739_Suicide_of_a_farmer_amid_COVID-19_in_India_Perspectives_on_social_determinants_of_suicidal_behavior_and_prevention_strategies (accessed on 18 September 2020).
- Narayanan, S. Food and Agriculture during a Pandemic: Managing the Consequence. Available online: https://www.ideasforindia.in/topics/agriculture/food-and-agriculture-during-a-pandemic-managing-the-consequences.html (accessed on 16 December 2020).
- Shrestha, N.; Shad, M.Y.; Ulvi, O.; Khan, M.H.; Karamehic-Muratovic, A.; Nguyen, U.-S.D.T.; Baghbanzadeh, M.; Wardrup, R.; Aghamohammadi, N.; Cervantes, D.; et al. The impact of COVID-19 on globalization. One Health 2020, 11, 100180. [Google Scholar] [CrossRef]
- Flaxman, S.; Mishra, S.; Gandy, A.; Unwin, H.J.T.; Mellan, T.A.; Coupland, H.; Whittaker, C.; Zhu, H.; Berah, T.; Eaton, J.W. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature 2020, 584, 257–261. [Google Scholar] [CrossRef]
- Grechyna, D. Health Threats Associated with Children Lockdown in Spain during COVID-19. Available online: https://ssrn.com/abstract=3567670 (accessed on 16 December 2020).
- ILO. COVID-19 and the World of Work; International Labour Organization: Geneva, Switzerland, 2020; Available online: http://oit.org/wcmsp5/groups/public/---dgreports/---dcomm/documents/briefingnote/wcms_743146.pdf (accessed on 16 December 2020).
- Chen, M. To Die from Hunger or the Virus. An All Too real Dilemma for the Poor in India and (Elsewhere). Available online: https://www.wider.unu.edu/publication/die-hunger-or-virus (accessed on 18 September 2020).
- Scroll. 18 Migrant Workers Found Travelling Inside Cement Mixer in Madhya Pradesh. 2 May 2020. Available online: https://scroll.in/latest/960862/coronavirus-18-migrant-workers-found-travelling-inside-cement-mixer-in-madhya-pradesh (accessed on 20 October 2020).
- Dutta, A. 198 Migrant Workers Killed in Road Accidents during Lockdown: Report. Hindustan Times, 22 December 2021. Available online: https://www.hindustantimes.com/india-news/198-migrant-workers-killed-in-road-accidents-during-lockdown-report/story-hTWzAWMYn0kyycKw1dyKqL.html(accessed on 20 October 2020).
- Acharya, S.S. Dignity of Informal Labour and Traveling Home in the Times of COVID-19. Available online: https://countercurrents.org/2020/06/dignity-of-informal-labour-and-traveling-home-in-the-times-of-covid-19/ (accessed on 16 October 2021).
- Khanna, A. Impact of migration of labour force due to global COVID-19 pandemic with reference to India. J. Health Manag. 2020, 22, 181–191. [Google Scholar] [CrossRef]
- Yen, D.A.W.; Cappellini, B.; Yang, H.P.; Gupta, S. Coping with Coping: International Migrants’ Experiences of the Covid-19 Lockdown in the UK. Br. J. Manag. 2021, 32, 1219–1241. [Google Scholar] [CrossRef]
- Onmanorama. Vande Bharat Mission Phase 1: Last Flight to Kerala Lands at Kochi. Onmanorama, 14 May 2020. Available online: https://www.onmanorama.com/news/kerala/2020/05/14/vande-bharat-mission-phase-1-last-flight-to-kerala-lands-at-koch.html(accessed on 6 July 2020).
- Roche, E. Private Airlines Included in Second Phase of ‘Vande Bharat’ Mission. Mint, 29 May 2020. Available online: https://www.livemint.com/news/india/private-airlines-included-in-second-phase-of-vande-bharat-mission-11590695508453.html(accessed on 8 November 2020).
- ILO As Job Losses Escalate, Nearly Half of Global Workforce at Risk of Losing Livelihoods. Available online: https://www.ilo.org/global/about-the-ilo/newsroom/news/WCMS_743036/lang--en/index.htm (accessed on 21 September 2020).
- Galea, S.; Merchant, R.M.; Lurie, N. The mental health consequences of COVID-19 and physical distancing: The need for prevention and early intervention. JAMA Intern. Med. 2020, 180, 817–818. [Google Scholar] [CrossRef] [Green Version]
- Bodrud-Doza, M.; Shammi, M.; Bahlman, L.; Islam, A.R.M.; Rahman, M. Psychosocial and socio-economic crisis in Bangladesh due to COVID-19 pandemic: A perception-based assessment. Front. Public Health 2020, 8, 341. [Google Scholar] [CrossRef]
- Yuan, Y.; Zhao, Y.-J.; Zhang, Q.-E.; Zhang, L.; Cheung, T.; Jackson, T.; Jiang, G.-Q.; Xiang, Y.-T. COVID-19-related stigma and its sociodemographic correlates: A comparative study. Glob. Health 2021, 17, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Bhatti, O.A.; Rauf, H.; Aziz, N.; Martins, R.S.; Khan, J.A. Violence against healthcare workers during the COVID-19 pandemic: a review of incidents from a lower-middle-income country. Anna. Global Health 2021, 87. [Google Scholar] [CrossRef]
- Arafa, A.; Shehata, A.; Youssef, M.; Senosy, S. Violence against healthcare workers during the COVID-19 pandemic: a cross-sectional study from Egypt. Arch. Environ. Occup. Health 2021, 1–7. [Google Scholar] [CrossRef]
- Chandna, H. Only 1 in 24 Indians Testing Positive for Covid, ICMR Says This Shows Our Strategy’s Working. The Print, 16 April 2020. Available online: https://theprint.in/health/only-1-in-24-indians-testing-positive-for-covid-icmr-says-this-shows-our-strategys-working/403181/(accessed on 15 November 2020).
- Al Dahdah, M.; Ferry, M.; Guérin, I.; Venkatasubramanian, G. The COVID-19 Crisis in India. 2020. Available online: https://booksandideas.net/The-Covid-19-Crisis-in-India.html (accessed on 6 June 2020).
- Hindu. 9.27 Lakh Severely Acute Malnourished Children Identified Till November Last Year: RTI. The HINDU, 6 June 2021. Available online: https://www.thehindu.com/news/national/927-lakh-severely-acute-malnourished-children-identified-till-november-last-year-rti/article34743642.ece(accessed on 20 November 2020).
- Dash, A. Malnutrition, the Silent Pandemic. The Indian Express, 25 September 2020. Available online: https://indianexpress.com/article/opinion/malnutrition-the-silent-pandemic-6610858/(accessed on 25 November 2020).
- Global Hunger Index—India. Available online: https://www.globalhungerindex.org/india.html (accessed on 18 October 2021).
- Abiad, A.; Arao, R.M.; Dagli, S. The Economic Impact of the COVID-19 Outbreak on Developing Asia. 2020. Available online: https://www.adb.org/publications/economic-impact-covid19-developing-asia (accessed on 25 November 2020).
- Lockdown 4.0: Migrant Workers Face Woes in Online Registration of ‘Shramik Special’ Trains. The New Indian Express, 20 May 2020. Available online: https://www.newindianexpress.com/nation/2020/may/20/lockdown-40-migrant-workers-face-woes-in-online-registration-of-shramik-special-trains-2145713.html(accessed on 7 July 2020).
- 800 ‘Shramik Special’ Trains Run So Far, 10 Lakh Migrants Ferried Home: Railways. The Times of India, 20 May 2020. Available online: https://timesofindia.indiatimes.com/india/800-shramik-special-trains-run-so-far-10-lakh-migrants-ferried-home-railways/articleshow/75738219.cms(accessed on 7 July 2020).
- Roy, S. Economic Impact of Covid-19 Pandemic. 2020, pp. 1–20. Available online: https://www.researchgate.net/profile/Shohini-Roy/publication/343222400_ECONOMIC_IMPACT_OF_COVID-19_PANDEMIC/links/5fa1e11e92851c14bc036d68/ECONOMIC-IMPACT-OF-COVID-19-PANDEMIC.pdf (accessed on 5 July 2021).
- Bhattacharyya, O.; Khor, S.; McGahan, A.; Dunne, D.; Daar, A.S.; Singer, P.A. Innovative health service delivery models in low and middle income countries-what can we learn from the private sector? Health Res. Policy Syst. 2010, 8, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Djalante, R.; Shaw, R.; DeWit, A. Building resilience against biological hazards and pandemics: COVID-19 and its implications for the Sendai Framework. Prog. Disaster Sci. 2020, 6, 100080. [Google Scholar] [CrossRef]
| Number | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| 1 | Articles published in between 2019–2021 | Articles published before 2019 |
| 2 | Articles published on COVID-19, lockdown, health impacts and improvement strategies, India | Articles that are relevant but too technical (mathematics and lab results), such as vaccine development |
| 3 | Articles directly or indirectly related to the search words | Articles not very relevant to the search words |
| 4 | Articles with new results, which should be applicable to any geographical area | Articles that are complicated to understand, with incomplete or biased results |
| 5 | Other pandemics related to the COVID-19 pandemic | Overly technical papers or papers on unrelated pandemics |
| No | Source | Article Title | Article Type | Article Information |
|---|---|---|---|---|
| 1 | [10] | “An assessment of socioeconomic impact of COVID-19 pandemic in India.” | Review | The COVID-19 epidemic has caused tremendous losses worldwide, but India, as an emerging country, is likely to be disproportionately affected in every industry. The service sector, which is the main driver of financial development and the biggest contributor to GDP, has been severely harmed as a result of various limitations on mobility, such as the temporary suspension of tourism and hospitality, the limited availability of transportation, the closure of schools and colleges, etc. The total economic and sectoral losses are determined by the intensity and duration of the crisis. In addition to economic damage, the societal impact of this coronavirus outbreak and unparalleled crisis is harsh, with substantial social and psychological issues. |
| 2 | [11] | “A study on impact of COVID-19 lockdown on psychological health, economy and social life of people in Kashmir.” | Original research | COVID-19 lockdown has an adverse impact on the mental health of different categories of people, particularly public, casual employees, students and health workers. |
| 3 | [12] | “The psychological impact of quarantine and how to reduce it: rapid review of the evidence.” | Review | The global spread of COVID-19 has also contributed to many mental health issues and a decline in general well-being. |
| 4 | [13] | “Efforts to mitigate the economic impact of the COVID-19 pandemic: potential entry points for neglected tropical diseases.” | Review | The COVID-19 pandemic complicates existing healthcare service delivery systems. To minimize the pandemic impact, the neglected tropical diseases community, particularly in low- and middle-income countries, must respond quickly, wisely and collaboratively with decision-makers and key stakeholders across sectors. |
| 5 | [14] | “The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China.” | Original research | Restrictions on movement of people and public gatherings and shutdown of economic activities help stop spreading infections and restrict the number of positive cases and COVID-19 vulnerability. As a result of the lockdown, there seems to be a substantial reduction in cases. |
| 6 | [15] | “Job loss and mental health during the COVID-19 lockdown: Evidence from South Africa.” | Original research | Health inequalities have required vulnerable groups to live more riskily. Recognising the informal sector’s contribution to the national economy, lockdown has shattered the mental health of a large part of the population and has increased chances of exposure to disrupted daily routines, which results in reducing human happiness and well-being. |
| 7 | [16] | “Social stigma during COVID-19 and its impact on HCWs outcomes.” | Original research | The pandemic situation has changed the workplace atmosphere drastically, leading to increased work hours and unfavourable and stressful interactions for healthcare professionals. When required to manage living as a healthcare practitioner and as a family member, working with highly infectious clients has subjected family members to infection. |
| 8 | [17] | “Social policy, COVID-19 and impoverished migrants: challenges and prospects in locked down India.” | Review | Unorganized workforce and circular migrants who work on informal and temporary contracts are growing in numbers as the most insecure (socio-economic) and at considerable community risk. Migrant informal workers face difficulties, including job losses, starvation and persecution by state containment officials. |
| 9 | [18] | “Socioeconomic determinants of COVID-19 in Asian countries: An empirical analysis.” | Original research | The proper management of reverse migrants (returning back from urban places to native (rural) places) and an increased role of people’s participation in adhering to social distancing are important for restricting COVID-19. Government is crucial to successful participation by society. When lockdowns ease, migrant workers again move to seek jobs. The government needs to have databases of labour movements and ensure safety and social distancing measures in the workplace. |
| 10 | [19] | “Multistakeholder Participation in Disaster Management—The Case of the COVID-19 Pandemic.” | Review | The combination of multi-stakeholder and spatial decision support systems has shown to be the most effective model for identifying probable pandemic sources and controlling global spread. Multi-stakeholder and spatial decision support systems can help enable crisis-management decision-making by bringing out a synergic link amongst multi-stakeholders. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Panneer, S.; Kantamaneni, K.; Akkayasamy, V.S.; Susairaj, A.X.; Panda, P.K.; Acharya, S.S.; Rice, L.; Liyanage, C.; Pushparaj, R.R.B. The Great Lockdown in the Wake of COVID-19 and Its Implications: Lessons for Low and Middle-Income Countries. Int. J. Environ. Res. Public Health 2022, 19, 610. https://doi.org/10.3390/ijerph19010610
Panneer S, Kantamaneni K, Akkayasamy VS, Susairaj AX, Panda PK, Acharya SS, Rice L, Liyanage C, Pushparaj RRB. The Great Lockdown in the Wake of COVID-19 and Its Implications: Lessons for Low and Middle-Income Countries. International Journal of Environmental Research and Public Health. 2022; 19(1):610. https://doi.org/10.3390/ijerph19010610
Chicago/Turabian StylePanneer, Sigamani, Komali Kantamaneni, Vigneshwaran Subbiah Akkayasamy, A. Xavier Susairaj, Prasant Kumar Panda, Sanghmitra Sheel Acharya, Louis Rice, Champika Liyanage, and Robert Ramesh Babu Pushparaj. 2022. "The Great Lockdown in the Wake of COVID-19 and Its Implications: Lessons for Low and Middle-Income Countries" International Journal of Environmental Research and Public Health 19, no. 1: 610. https://doi.org/10.3390/ijerph19010610
APA StylePanneer, S., Kantamaneni, K., Akkayasamy, V. S., Susairaj, A. X., Panda, P. K., Acharya, S. S., Rice, L., Liyanage, C., & Pushparaj, R. R. B. (2022). The Great Lockdown in the Wake of COVID-19 and Its Implications: Lessons for Low and Middle-Income Countries. International Journal of Environmental Research and Public Health, 19(1), 610. https://doi.org/10.3390/ijerph19010610









