Correlation between the Photographic Cranial Angles and Radiographic Cervical Spine Alignment
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Photographic Measurements
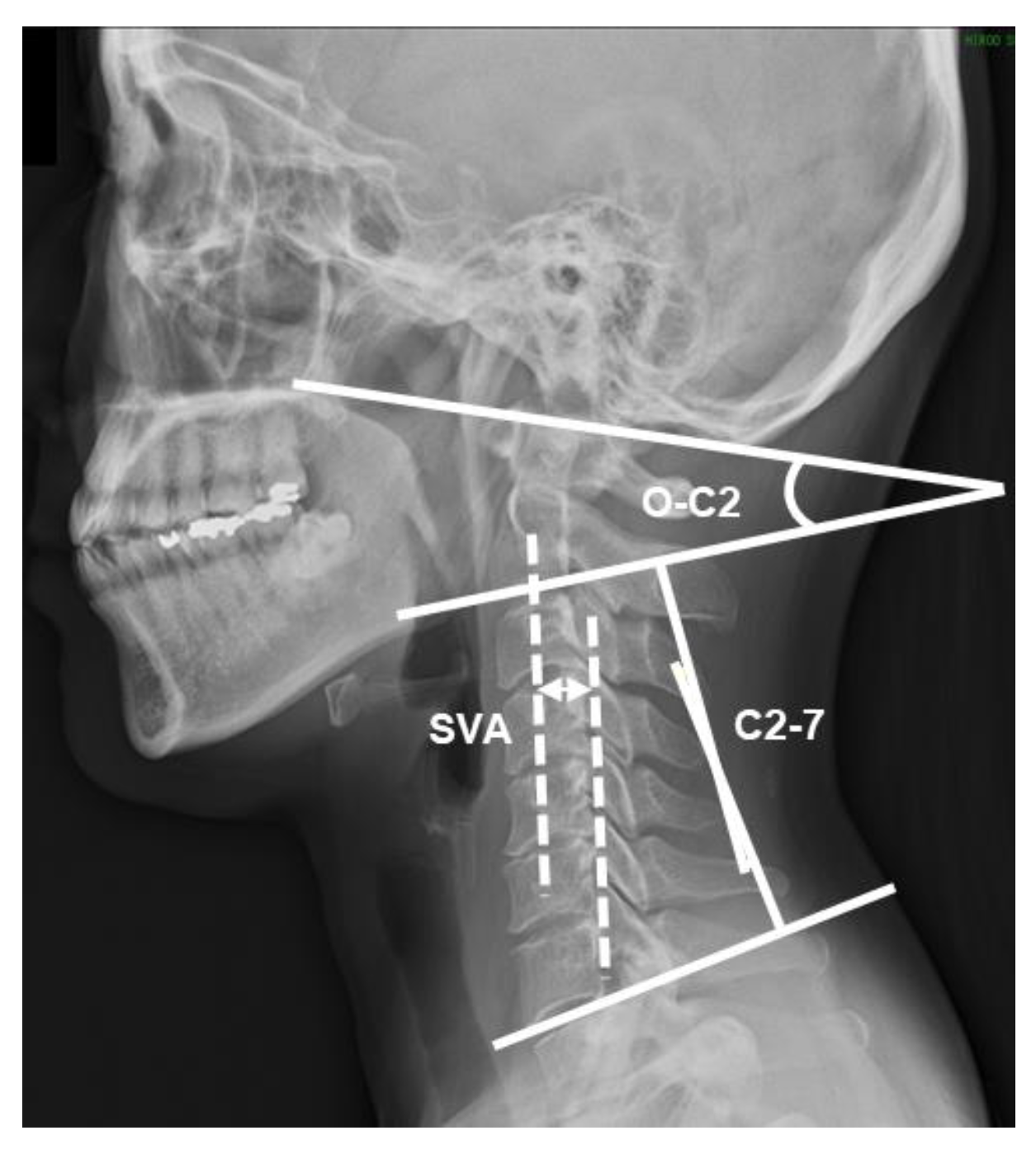
2.3. Radiographic Measurements
2.4. Statistical Analyses
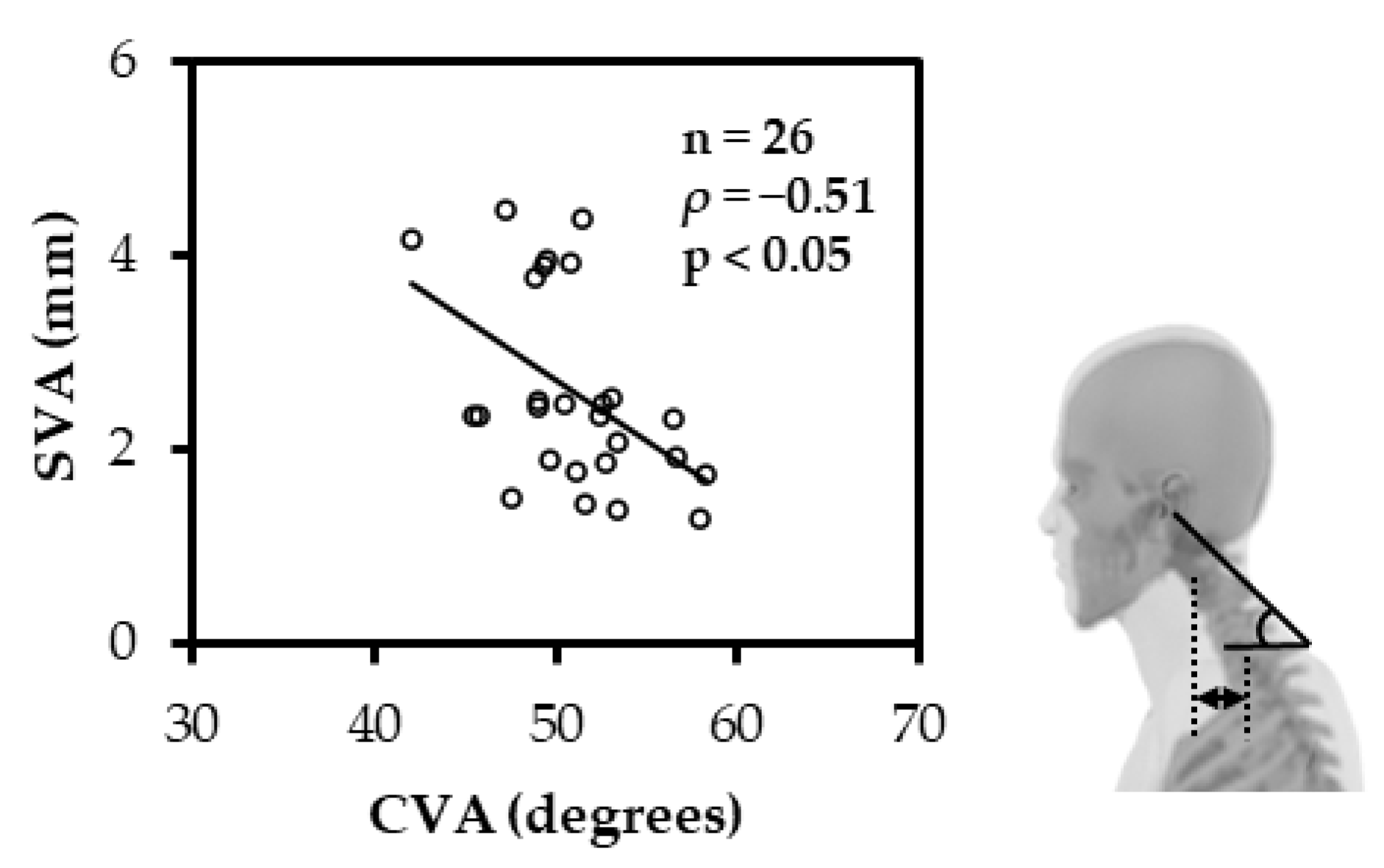
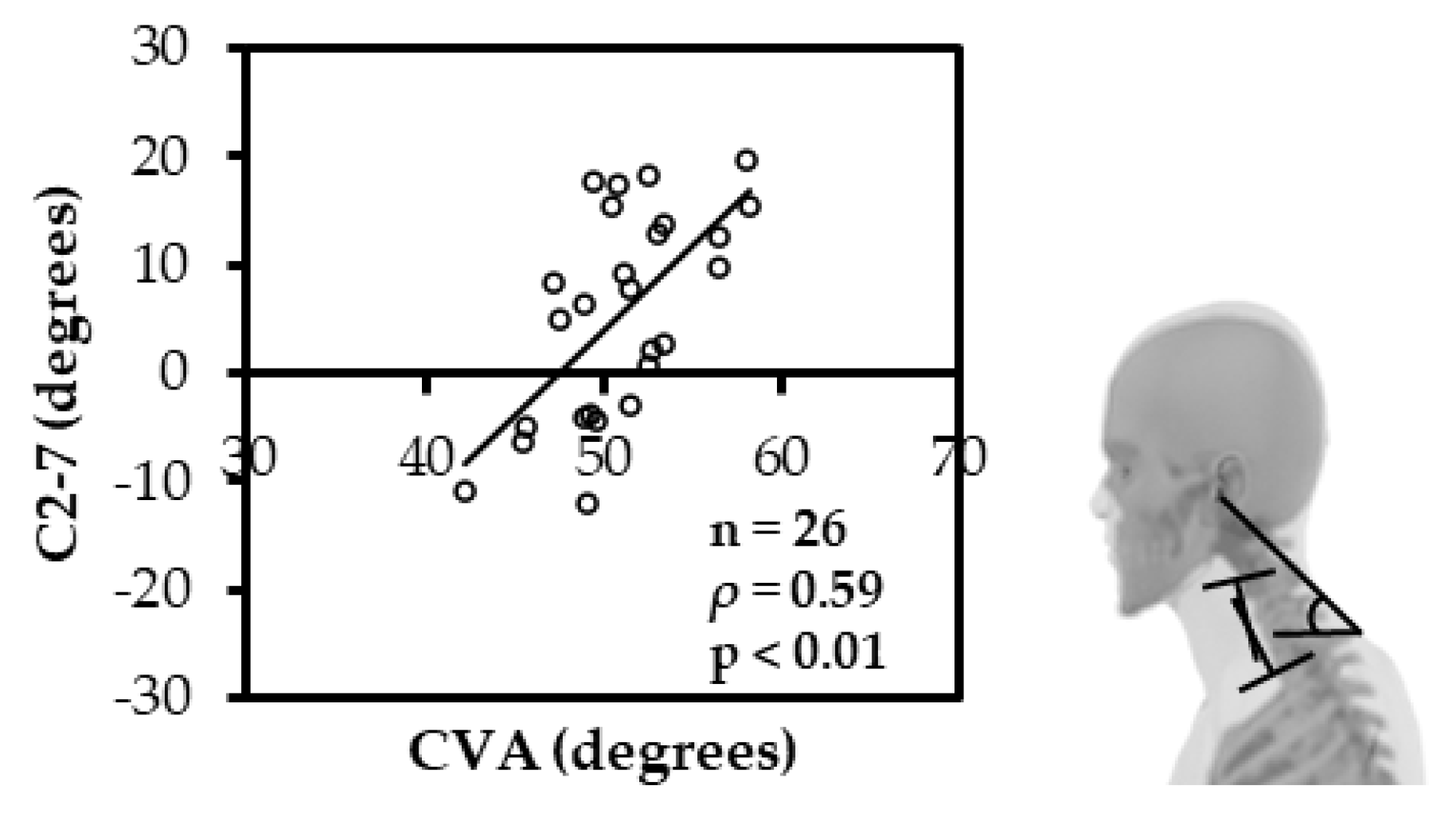
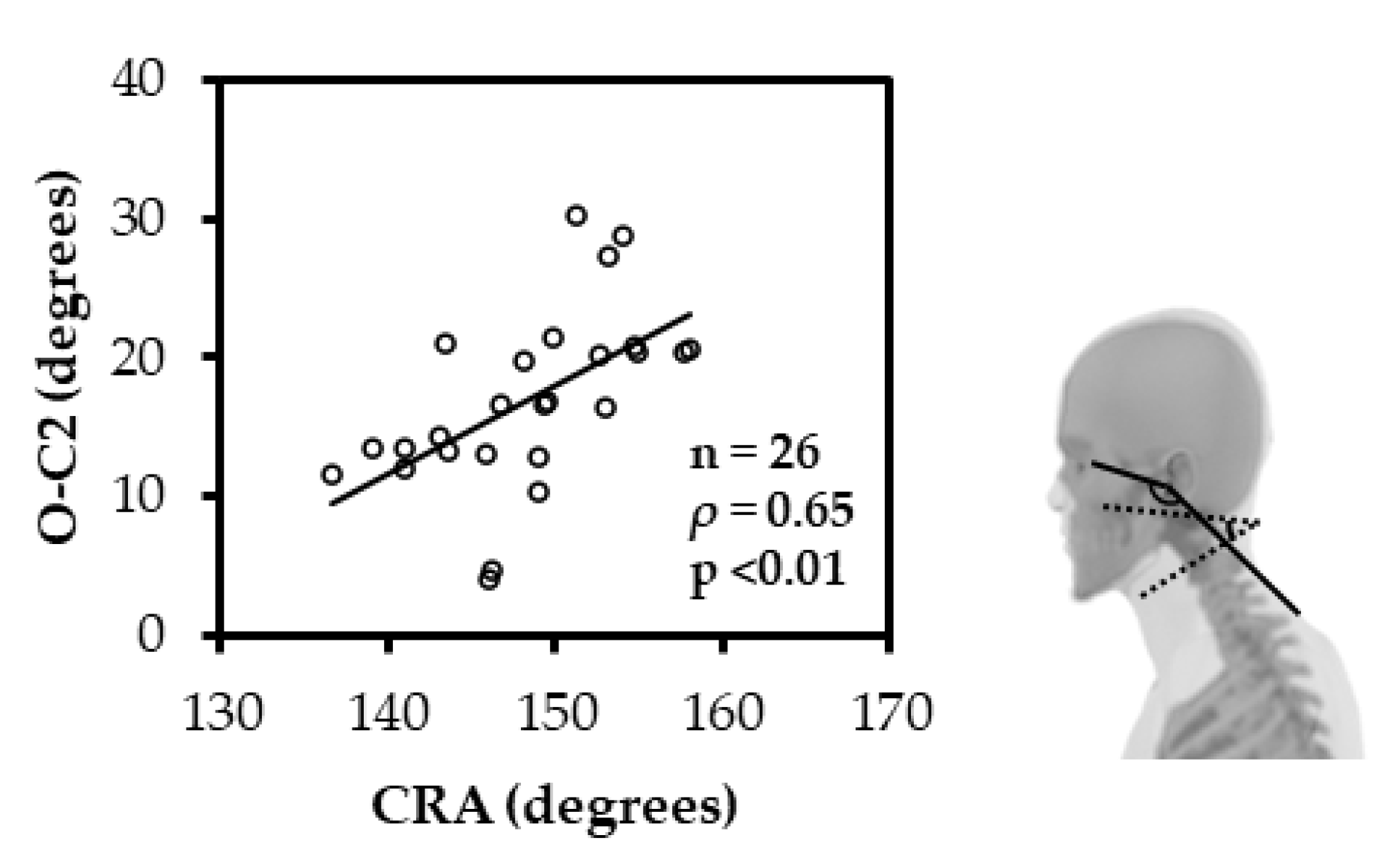
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Childs, J.D.; Cleland, J.A.; Elliott, J.M.; Teyhen, D.S.; Wainner, R.S.; Whitman, J.M.; Sopky, B.J.; Godges, J.J.; Flynn, T.W.; American Physical Therapy Association. Neck Pain: Clinical Practice Guidelines Linked to the International Classification of Functioning, Disability, and Health from the Orthopedic Section of the American Physical Therapy Association. J. Orthop. Sports Phys. Ther. 2008, 38, A1–A34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andersen, J.H.; Kaergaard, A.; Mikkelsen, S.; Jensen, U.F.; Frost, P.; Bonde, J.P.; Fallentin, N.; Thomsen, J.F. Risk Factors in the Onset of Neck/Shoulder Pain in a Prospective Study of Workers in Industrial and Service Companies. Occup. Environ. Med. 2003, 60, 649–654. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yip, C.H.T.; Chiu, T.T.W.; Poon, A.T.K. The Relationship Between Head Posture and Severity and Disability of Patients with Neck Pain. Man. Ther. 2008, 13, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Subbarayalu, A.V. Measurement of Craniovertebral Angle by the Modified Head Posture Spinal Curvature Instrument: A Reliability and Validity Study. Physiother. Theory Pract. 2016, 32, 144–152. [Google Scholar] [CrossRef]
- McAviney, J.; Schulz, D.; Bock, R.; Harrison, D.E.; Holland, B. Determining the Relationship Between Cervical Lordosis and Neck Complaints. J. Manip. Physiol. Ther. 2005, 28, 187–193. [Google Scholar] [CrossRef]
- Iyer, S.; Lenke, L.G.; Nemani, V.M.; Fu, M.; Shifflett, G.D.; Albert, T.J.; Sides, B.A.; Metz, L.N.; Cunningham, M.E.; Kim, H.J. Variations in Occipitocervical and Cervicothoracic Alignment Parameters Based on Age: A Prospective Study of Asymptomatic Volunteers Using Full-Body Radiographs. Spine 2016, 41, 1837–1844. [Google Scholar] [CrossRef]
- Valentin, J. Low-Dose Extrapolation of Radiation-Related Cancer Risk. Ann. ICRP 2005, 35, 1–140. [Google Scholar] [CrossRef]
- Cohen, L.; Kobayashi, S.; Simic, M.; Dennis, S.; Refshauge, K.; Pappas, E. Non-Radiographic Methods of Measuring Global Sagittal Balance: A Systematic Review. Scoliosis Spinal Disord. 2017, 12, 30. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5625601/ (accessed on 19 November 2020). [CrossRef] [Green Version]
- Silva, A.G.; Punt, T.D.; Sharples, P.; Vilas-Boas, J.P.; Johnson, M.I. Head Posture Assessment for Patients with Neck Pain: Is It Useful? Int. J. Ther. Rehabil. 2009, 16, 43–53. [Google Scholar] [CrossRef]
- Gallego-Izquierdo, T.; Arroba-Díaz, E.; García-Ascoz, G.; Val-Cano, M. del A.; Pecos-Martin, D.; Cano-de-la-Cuerda, R. Psychometric Proprieties of a Mobile Application to Measure the Craniovertebral Angle a Validation and Reliability Study. Int. J. Environ. Res. Public Health 2020, 17, 6521. [Google Scholar] [CrossRef]
- Lee, D.; Max, S.; Mark, S. Internal and external sagittal craniovertebral alignment: A comparison between radiological and photogrammetric approaches in asymptomatic participants. Musculoskelet Sci. Pract. 2019, 43, 12–17. [Google Scholar] [CrossRef]
- Kietrys, D.M.; McClure, P.W.; Fitzgerald, G.K. The Relationship Between Head and Neck Posture and VDT Screen Height in Keyboard Operators. Phys. Ther. 1998, 78, 395–403. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Ryan, D.J.; Stekas, N.D.; Ayres, E.W.; Moawad, M.A.; Balouch, E.; Vasquez-Montes, D.; Fischer, C.R.; Buckland, A.J.; Errico, T.J.; Protopsaltis, T.S. Clinical photographs in the assessment of adult spinal deformity: A comparison to radiographic parameters. J. Neurosurg. 2021, 35, 105–109. [Google Scholar] [CrossRef]
- Cohen, J. A Power Primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- UNSCEAR 2000 Report-Vol. I. Available online: https://www.unscear.org/unscear/en/publications/2000_1.html (accessed on 24 March 2022).
- Nayler, J.R. Clinical Photography: A Guide for the Clinician. J. Postgrad. Med. 2003, 49, 256–262. [Google Scholar]
- Ruivo, R.M.; Pezarat-Correia, P.; Carita, A.I. Cervical and Shoulder Postural Assessment of Adolescents Between 15 and 17 Years Old and Association with Upper Quadrant Pain. Braz. J. Phys. Ther. 2014, 18, 364–371. [Google Scholar] [CrossRef] [Green Version]
- Shin, S.; Yoon, D.M.; Yoon, K.B. Identification of the Correct Cervical Level by Palpation of Spinous Processes. Anesth. Analg. 2011, 112, 1232–1235. [Google Scholar] [CrossRef]
- Lee, J.; Lee, Y.; Kim, H.; Lee, J. The Effects of Cervical Mobilization Combined with Thoracic Mobilization on Forward Head Posture of Neck Pain Patients. J. Phys. Ther. Sci. 2013, 25, 7–9. [Google Scholar] [CrossRef] [Green Version]
- Ota, M.; Neo, M.; Aoyama, T.; Ishizaki, T.; Fujibayashi, S.; Takemoto, M.; Nakayama, T.; Nakamura, T. Impact of the O-C2 Angle on the Oropharyngeal Space in Normal Patients. Spine 2011, 36, E720–E726. [Google Scholar] [CrossRef]
- Yoshida, G.; Alzakri, A.; Pointillart, V.; Boissiere, L.; Obeid, I.; Matsuyama, Y.; Vital, J.M.; Gille, O. Global Spinal Alignment in Patients with Cervical Spondylotic Myelopathy. Spine 2018, 43, E154–E162. [Google Scholar] [CrossRef] [PubMed]
- Scheer, J.K.; Tang, J.A.; Smith, J.S.; Acosta, F.L.; Protopsaltis, T.S.; Blondel, B.; Bess, S.; Shaffrey, C.I.; Deviren, V.; Lafage, V.; et al. Cervical Spine Alignment, Sagittal Deformity, and Clinical Implications: A Review. J. Neurosurg. Spine 2013, 19, 141–159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tian, W.; Yu, J. The Role of C2–C7 and O–C2 Angle in the Development of Dysphagia After Cervical Spine Surgery. Dysphagia 2013, 28, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Ono, K.; Murata, S.; Matsushita, M.; Murakami, H. Cervical Lordosis Ratio as a Novel Predictor for the Loss of Cervical Lordosis After Laminoplasty. Neurospine 2021, 18, 311–318. [Google Scholar] [CrossRef]
- Yo, K.; Tsushima, E.; Oishi, Y.; Murase, M.; Ota, S.; Matsuda, Y.; Yamaoki, Y.; Morihisa, R.; Uchihira, T.; Omura, T. The Reliabilities of Several Measurement Methods of Cervical Sagittal Alignment in Cases with Cervical Spine Rotation Using X-Ray Findings in Cervical Spine Disorders. Spine Surg. Relat. Res. 2018, 2, 186–196. [Google Scholar] [CrossRef] [Green Version]
- Morimoto, Y.; Shigematsu, H.; Iwata, E.; Tanaka, M.; Okuda, A.; Masuda, K.; Yamamoto, Y.; Takeshima, T.; Nakagawa, Y.; Tanaka, Y. Evaluating Cervical Sagittal Alignment in Cervical Myelopathy: Are Sitting Cervical Radiographs and Standing Whole-Spine Radiographs Equally Useful? Glob. Spine J. 2019, 9, 591–597. [Google Scholar] [CrossRef] [Green Version]
- Harrison, A.L.; Barry-Greb, T.; Wojtowicz, G. Clinical Measurement of Head and Shoulder Posture Variables. J. Orthop. Sports Phys. Ther. 1996, 23, 353–361. [Google Scholar] [CrossRef]
- Lau, H.M.C.; Chiu, T.T.W.; Lam, T.H. Measurement of Craniovertebral Angle with Electronic Head Posture Instrument: Criterion Validity. J. Rehabil. Res. Dev. 2010, 47, 911–918. [Google Scholar] [CrossRef] [Green Version]
- Ordway, N.R.; Seymour, R.J.; Donelson, R.G.; Hojnowski, L.S.; Edwards, W.T. Cervical Flexion, Extension, Protrusion, and Retraction: A Radiographic Segmental Analysis. Spine 1999, 24, 240–247. [Google Scholar] [CrossRef]
- Raine, S.; Twomey, L.T. Head and Shoulder Posture Variations in 160 Asymptomatic Women and Men. Arch. Phys. Med. Rehabil. 1997, 78, 1215–1223. [Google Scholar] [CrossRef]
- Weber, P.; Castilhos, E.; Correa, E.; Milanesi, J.; Soares, J.; Trevisan, M. Craniocervical Posture: Cephalometric and Biophotogrammetric Analysis. Braz. J. Oral Sci. 2012, 11, 416–421. [Google Scholar]

| Demographic Variables | Median or Count (n) | IQR or % | Min | Max | |
|---|---|---|---|---|---|
| Sex | Male | 17 | 65 | ||
| female | 9 | 35 | |||
| Age, y (median (IQR)) | 21.5 | 2.8 | 18.0 | 36.0 | |
| Height, cm (median (IQR)) | 169.0 | 12.0 | 148.0 | 183.0 | |
| Weight, kg (median (IQR)) | 63.0 | 12.8 | 47.0 | 107.0 | |
| Body mass index, kg/m2 (median (IQR)) | 22.1 | 2.2 | 19.2 | 35.8 | |
| Cervical Sagittal Alignment | Total | Male | Female | |||||
|---|---|---|---|---|---|---|---|---|
| Median | IQR | Min/Max | Median | IQR | Median | IQR | p Value | |
| CVA (degrees) | 50.9 | 3.8 | 42.2/58.2 | 51.4 | 4.3 | 49.5 | 3.7 | 0.44 |
| CRA (degrees) | 148.9 | 8.7 | 136.6/158.1 | 148.9 | 7.4 | 149.3 | 7.8 | 0.81 |
| SVA (mm) | 2.3 | 1.9 | 1.3/4.5 | 2.1 | 0.7 | 2.5 | 1.4 | 0.06 |
| C2-7 (degrees) | 6.3 | 17.6 | −12.1/20.1 | 6.3 | 18.1 | 8.3 | 12.3 | 0.57 |
| O-C2 (degrees) | 16.6 | 7.7 | 4.1/30.3 | 14.3 | 8.2 | 19.8 | 4.6 | 0.13 |
| Age | Height | Weight | BMI | ||
|---|---|---|---|---|---|
| CVA | ρ | −0.40 * | −0.04 | −0.11 | −0.24 |
| 95%CI | −0.68–−0.02 | −0.42–0.35 | −0.48–0.29 | −0.57–0.16 | |
| CRA | ρ | 0.11 | −0.03 | 0.17 | 0.30 |
| 95%CI | −0.29–0.47 | −0.41–0.36 | −0.23–0.52 | −0.10–0.62 |
| Independent Variable | Partial Regression Coefficient | Standardized Partial Regression Coefficients | p Value | 95% Confidence Interval |
|---|---|---|---|---|
| Constants | 57.019 | 0.000 | 48.45–65.59 | |
| SVA (mm) | −1.514 | −0.392 | 0.019 | −2.76–−0.27 |
| C2-7 (degrees) | 0.187 | 0.464 | 0.012 | 0.05–0.33 |
| Age (years) | −0.137 | −0.164 | 0.334 | −0.42–0.15 |
| Independent Variable | Partial Regression Coefficient | Standardized Partial Regression Coefficients | p Value | 95% Confidence Interval |
|---|---|---|---|---|
| Constants | 139.867 | 0.000 | 134.4–145.4 | |
| O-C2 (degrees) | 0.500 | 0.568 | 0.002 | 0.20–0.81 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kawasaki, T.; Ohji, S.; Aizawa, J.; Sakai, T.; Hirohata, K.; Kuruma, H.; Koseki, H.; Okawa, A.; Jinno, T. Correlation between the Photographic Cranial Angles and Radiographic Cervical Spine Alignment. Int. J. Environ. Res. Public Health 2022, 19, 6278. https://doi.org/10.3390/ijerph19106278
Kawasaki T, Ohji S, Aizawa J, Sakai T, Hirohata K, Kuruma H, Koseki H, Okawa A, Jinno T. Correlation between the Photographic Cranial Angles and Radiographic Cervical Spine Alignment. International Journal of Environmental Research and Public Health. 2022; 19(10):6278. https://doi.org/10.3390/ijerph19106278
Chicago/Turabian StyleKawasaki, Tomoko, Shunsuke Ohji, Junya Aizawa, Tomoko Sakai, Kenji Hirohata, Hironobu Kuruma, Hirohisa Koseki, Atsushi Okawa, and Tetsuya Jinno. 2022. "Correlation between the Photographic Cranial Angles and Radiographic Cervical Spine Alignment" International Journal of Environmental Research and Public Health 19, no. 10: 6278. https://doi.org/10.3390/ijerph19106278
APA StyleKawasaki, T., Ohji, S., Aizawa, J., Sakai, T., Hirohata, K., Kuruma, H., Koseki, H., Okawa, A., & Jinno, T. (2022). Correlation between the Photographic Cranial Angles and Radiographic Cervical Spine Alignment. International Journal of Environmental Research and Public Health, 19(10), 6278. https://doi.org/10.3390/ijerph19106278






