Effects of Copenhagen Adduction Exercise on Muscle Architecture and Adductor Flexibility
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Research Design
2.2.1. Assessment of LA Architecture
2.2.2. Adductor Muscles Flexibility
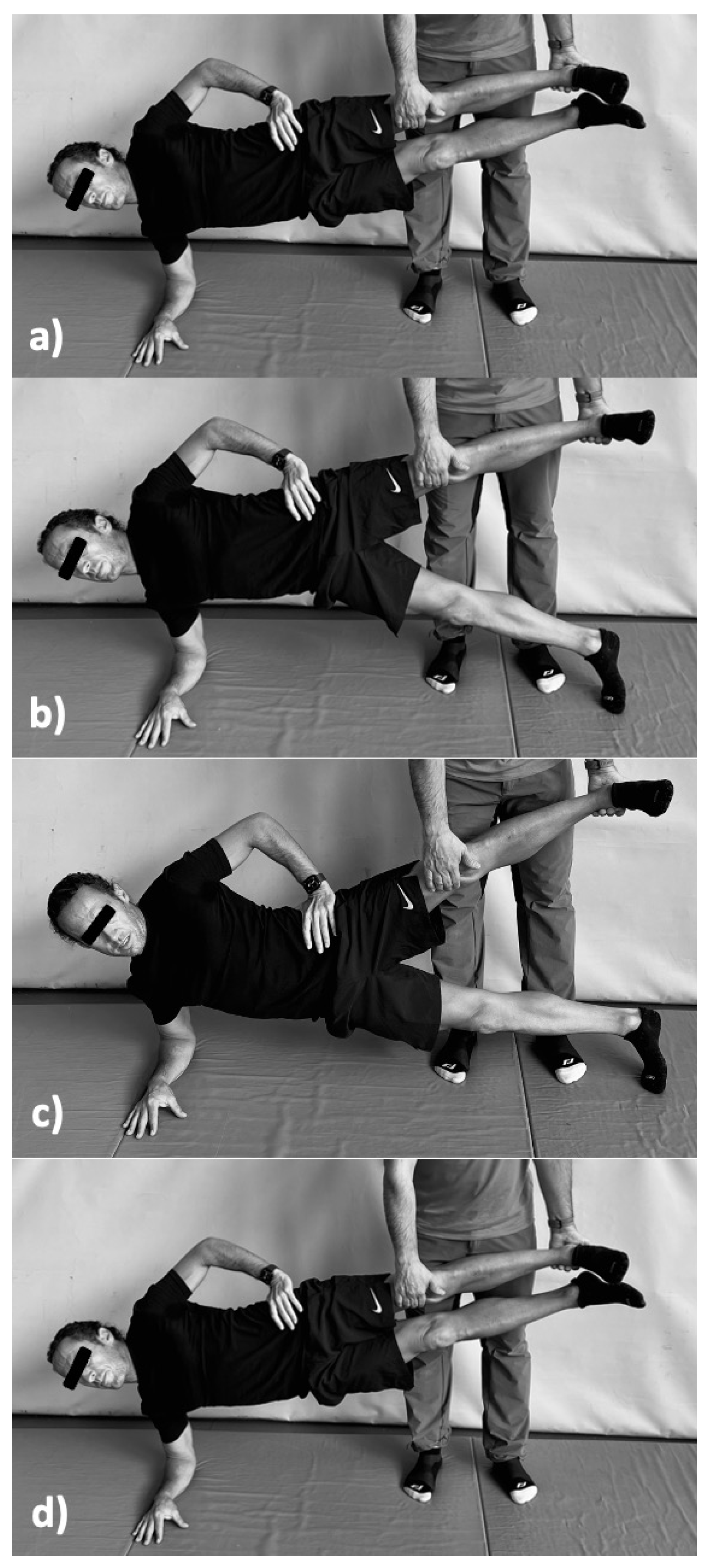
2.2.3. “Copenhagen Adduction Exercise”
2.3. Intervention
2.4. Statistical Analysis
3. Results
3.1. Muscle Architecture
3.2. Flexibility of Adductor Muscles
4. Discussion
5. Conclusions, Limitations and Future Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Su, B.Y.; Liu, M.S.; De Silva, P.V.; Østbye, T.; Jin, K.Z. Health-related quality of life in Chinese workers: A systematic review and meta-analysis. Glob. Health Res. Policy 2021, 6, 29. [Google Scholar] [CrossRef] [PubMed]
- Anwer, S.; Li, H.; Antwi-Afari, M.F.; Wong, A.Y.L. Associations between physical or psychosocial risk factors and work-related musculoskeletal disorders in construction workers based on literature in the last 20 years: A systematic review. Int. J. Ind. Ergon. 2021, 83, 103113. [Google Scholar] [CrossRef]
- Sass, A.C.; Stang, A. Population-based incidences of non-fatal injuries—Results of the German-wide telephone survey 2004. BMC Public Health 2013, 13, 376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brooks, J.H.M.; Fuller, C.W.; Kemp, S.P.T.; Reddin, D.B. Epidemiology of injuries in English professional rugby union: Part 1 match injuries. Br. J. Sports Med. 2005, 39, 757–766. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sammito, S.; Hadzic, V.; Karakolis, T.; Kelly, K.R.; Proctor, S.P.; Stepens, A.; White, G.; Zimmermann, W.O. Risk factors for musculoskeletal injuries in the military: A qualitative systematic review of the literature from the past two decades and a new prioritizing injury model. Mil. Med. Res. 2021, 8, 66. [Google Scholar] [CrossRef]
- Witvrouw, E.; Danneels, L.; Asselman, P.; D’Have, T.; Cambier, D. Muscle flexibility as a risk factor for developing muscle injuries in male professional soccer players. A prospective study. Am. J. Sports Med. 2003, 31, 41–46. [Google Scholar] [CrossRef]
- Ekstrand, J.; Gillquist, J. The avoidability of soccer injuries. Int. J. Sports Med. 1983, 4, 124–128. [Google Scholar] [CrossRef]
- Kenny, S.J.; Whittaker, J.L.; Emery, C.A. Risk factors for musculoskeletal injury in preprofessional dancers: A systematic review. Br. J. Sports Med. 2016, 50, 997–1003. [Google Scholar] [CrossRef]
- Kloskowska, P.; Morrissey, D.; Small, C.; Malliaras, P.; Barton, C. Movement Patterns and Muscular Function Before and After Onset of Sports-Related Groin Pain: A Systematic Review with Meta-analysis. Sports Med. 2016, 46, 1847–1867. [Google Scholar] [CrossRef] [Green Version]
- Whittaker, J.; Small, C.; Maffey, L.; Emery, C.A. Risk factors for groin injury in sport: An updated systematic review. Br. J. Sports Med. 2015, 49, 803–809. [Google Scholar] [CrossRef]
- Engebretsen, A.H.; Myklebust, G.; Holme, I.M.K.; Engebretsen, L.; Bahr, R. Intrinsic Risk Factors for Groin Injuries among Male Soccer Players. Am. J. Sports Med. 2010, 38, 2051–2057. [Google Scholar] [CrossRef] [PubMed]
- Douglas, J.; Pearson, S.; Ross, A.; McGuigan, M. Chronic adaptations to eccentric training: A systematic review. Sports Med. 2017, 47, 917–941. [Google Scholar] [CrossRef] [PubMed]
- LaStayo, P.C.; Woolf, J.M.; Lewek, M.D.; Snyder-Mackler, L.; Reich, T.; Lindstedt, S.L. Eccentric muscle contractions: Their contribution to injury, prevention, rehabilitation, and sport. J. Orthop. Sports Phys. Ther. 2003, 33, 557–571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roig, M.; O’Brien, K.; Kirk, G.; Murray, R.; McKinnon, P.; Shadgan, B.; Reid, W.D. The effects of eccentric versus concentric resistance training on muscle strength and mass in healthy adults: A systematic review with meta-analysis. Br. J. Sports Med. 2009, 43, 556–568. [Google Scholar] [CrossRef]
- Baroni, B.M.; Geremia, J.M.; Rodrigues, R.; De Acebedo, F.R.; Karamanidis, K.; Vaz, M.A. Muscle architecture adaptations to knee extensor eccentric training: Rectus femoris vs vastus lateralis. Muscle Nerve 2013, 48, 498–506. [Google Scholar] [CrossRef]
- Ema, R.; Wakahara, T.; Mogi, Y.; Miyamoto, N.; Komatsu, T.; Kanehisa, H.; Kawakami, Y. In vivomeasurement of human rectus femoris architecture by ultrasonography: Validity and applicability. Clin. Physiol. Funct. Imaging 2013, 33, 267–273. [Google Scholar] [CrossRef]
- Alonso-Fernandez, D.; Gutierrez-Sanchez, Á.; Garcia-Remeseiro, T.; Garganta, R. Effects of the Nordic hamstring exercise on the architecture of the semitendinosus. Isokinet. Exerc. Sci. 2018, 26, 81–88. [Google Scholar] [CrossRef]
- Alonso-Fernandez, D.; Docampo-Blanco, P.; Martinez-Fernandez, J. Changes in muscle architecture of biceps femoris induced by eccentric strength training with Nordic Hamstring exercise running. Isokinet. Exerc. Sci. 2018, 28, 88–94. [Google Scholar] [CrossRef]
- Bourne, M.N.; Duhig, S.J.; Timmins, R.G.; Williams, M.D.; Opar, D.A.; Al Najjar, A.; Kerr, G.K.; Shield, A.J. Impact of the Nordic hamstring and hip extension exercises on hamstring architecture and morphology: Implications for injury prevention. Br. J. Sports Med. 2017, 51, 469–477. [Google Scholar] [CrossRef] [Green Version]
- Timmins, R.G.; Shield, A.J.; Williams, M.D.; Lorenzen, C.; Opar, D.A. Biceps femoris long head architecture: A reliability and retrospective injury study. Med. Sci. Sports Exerc. 2015, 47, 905–913. [Google Scholar] [CrossRef] [Green Version]
- Alonso-Fernández, D.; Taboada-Iglesias, Y.; García-Remeseiro, T.; Gutiérrez-Sánchez, A. Effects of the Functional Heel Drop Exercise on the Muscle Architecture of the Gastrocnemius. J. Sport Rehabil. 2019, 29, 1053–1059. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Fernandez, D.; Fernandez-Rodriguez, R.; Abalo-Núñez, R. Changes in rectus femoris architecture induced by the reverse nordic hamstring exercises. J. Sports Med. Phys. Fit. 2019, 59, 640–647. [Google Scholar] [CrossRef] [PubMed]
- Harøy, J.; Thorborg, K.; Serner, A.; Bjørkheim, A.; Rolstad, L.E.; Hölmich, P.; Bahr, R.; Andersen, T.E. Including the Copenhagen Adduction Exercise in the FIFA 11+ Provides Missing Eccentric Hip Adduction Strength Effect in Male Soccer Players: A Randomized Controlled Trial. Am. J. Sports Med. 2017, 45, 3052–3059. [Google Scholar] [CrossRef] [PubMed]
- Ishøi, L.; Sørensen, C.N.; Kaae, N.M.; Jørgensen, L.B.; Hölmich, P.; Serner, A. Large eccentric strength increase using the Copenhagen Adduction exercise in football: A randomized controlled trial. Scand. J. Med. Sci. Sports 2015, 26, 1334–1342. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Calvete, A.; Lorenzo-Martínez, M.; Padrón-Cabo, A.; Rey, E. Effects of Copenhagen Adduction Exercise on the Architectural Characteristics of Adductors in U-17 Male Soccer Players: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 12956. [Google Scholar] [CrossRef] [PubMed]
- Blazevich, A.J.; Cannavan, D.; Coleman, D.R.; Horne, S. Influence of concentric and eccentric resistance training on architectural adaptation in human quadriceps muscles. J. Appl. Physiol. 2007, 103, 1565–1575. [Google Scholar] [CrossRef]
- Kellis, E.; Galanis, N.; Natsis, K.; Kapetanos, G. Validity of architectural properties of the hamstring muscles: Correlation of ultrasound findings with cadaveric dissection. J. Biomech. 2009, 42, 2549–2554. [Google Scholar] [CrossRef]
- Pesquer, L.; Reboul, G.; Silvestre, A.; Poussange, N.; Meyer, P.; Dallaudière, B. Imaging of adductor-related groin pain. Diagn. Interv. Imaging 2015, 96, 861–869. [Google Scholar] [CrossRef]
- Davis, J.A.; Stringer, M.D.; Woodley, S.J. New insights into the proximal tendons of adductor longus, adductor brevis and gracilis. Br. J. Sports Med. 2011, 46, 871–876. [Google Scholar] [CrossRef] [Green Version]
- Campbell, R. Ultrasound of the Athletic Groin. Semin. Musculoskelet. Radiol. 2013, 17, 34–42. [Google Scholar] [CrossRef]
- Klimstra, M.; Dowling, J.; Durkin, J.L.; MacDonald, M. The effect of ultrasound probe orientation on muscle architecture measurement. J. Electromyogr. Kinesiol. 2007, 17, 504–514. [Google Scholar] [CrossRef] [PubMed]
- Greene, W.B.; Heckman, J.D. (Eds.) The Clinical Measurement of Joint Motion; American Academy of Orthopedic Surgeons: Rosemont, IL, USA, 1994. [Google Scholar]
- Tyler, T.F.; Nicholas, S.J.; Campbell, R.J.; McHugh, M.P. The association of hip strength and flexibility with the incidence of adductor muscle strains in professional ice hockey players. Am. J. Sports Med. 2001, 29, 124–128. [Google Scholar] [CrossRef] [PubMed]
- Serner, A.; Jakobsen, M.D.; Andersen, L.L.; Holmich, P.; Sundstrup, E.; Thorborg, K. EMG evaluation of hip adduction exercises for soccer players: Implications for exercise selection in prevention and treatment of groin injuries. Br. J. Sports Med. 2014, 48, 1108–1114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schaber, M.; Guiser, Z.; Brauer, L.; Jackson, R.; Banyasz, J.; Miletti, R.; Hassen-Miller, A. The Neuromuscular Effects of the Copenhagen Adductor Exercise: A Systematic Review. Int. J. Sports Phys. Ther. 2021, 16, 1210–1221. [Google Scholar] [CrossRef]
- Hopkins, W.G. Measures of Reliability in Sports Medicine and Science. Sports Med. 2000, 30, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Ryan, J.; Deburca, N.; Mc Creesh, K. Risk factors for groin/hip injuries in field-based sports: A systematic review. Br. J. Sports Med. 2014, 48, 1089–1096. [Google Scholar] [CrossRef] [PubMed]
- Donaldson, A.; Cook, J.; Gabbe, B.; Lloyd, D.G.; Young, W.; Finch, C.F. Bridging the gap between content and context: Establishing expert consensus on the content of an exercise training program to prevent lower-limb injuries. Clin. J. Sport Med. 2015, 25, 221–229. [Google Scholar] [CrossRef]
- Dello Iacono, A.; Maffulli, N.; Laver, L.; Padulo, J. Successful treatment of groin pain syndrome in a pole-vault athlete with core stability exercise. J. Sports Med. Phys. Fit. 2017, 57, 1650–1659. [Google Scholar] [CrossRef]
- Polglass, G.; Burrows AWillett, M. Impact of a modified progressive Copenhagen adduction exercise programme on hip adduction strength and postexercise muscle soreness in professional footballers. BMJ Open Sport Exerc. Med. 2019, 5, e000570. [Google Scholar] [CrossRef] [Green Version]
- Kohavi, B.; Beato, M.; Laver, L.; Freitas, T.T.; Chung, L.H.; Iacono, A.D. Effectiveness of Field-Based Resistance Training Protocols on Hip Muscle Strength Among Young Elite Football Players. Clin. J. Sport Med. 2020, 30, 470–477. [Google Scholar] [CrossRef]
- Harøy, J.; Clarsen, B.; Wiger, E.G.; Øyen, M.G.; Serner, A.; Thorborg, K.; Holmich, P.; Andersen, T.E.; Bahr, R. The Adductor Strengthening Programme prevents groin problems among male football players: A cluster-randomised controlled trial. Br. J. Sports Med. 2018, 53, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Gleim, G.W.; McHugh, M.P. Flexibility and its effects on sports injury and performance. Sports Med. 1997, 24, 289–299. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Fernandez, D.; Martinez-Fernandez, J.; Docampo-Blanco, P.; Fernandez-Rodriguez, R. Impact of Askling L-PROTOCOL on muscle architecture, flexibility and sprint performance. Int. J. Sports Med. 2022, 43, 373–380. [Google Scholar] [CrossRef] [PubMed]
| Week | No. of Sessions/Week | Sets Per Side | Repetitions | Total Repetitions Per Side/Week | Rest Between Sets |
|---|---|---|---|---|---|
| 1 | 2 | 1 | 5 | 10 | - |
| 2 | 2 | 1 | 5 | 10 | - |
| 3 | 2 | 2 | 6 | 12 | 2 min |
| 4 | 2 | 2 | 7 | 14 | 2 min |
| 5 | 2 | 1 | 10 | 20 | - |
| 6 | 2 | 1 | 12 | 24 | - |
| 7 | 3 | 1 | 15 | 30 | - |
| 8 | 3 | 1 | 15 | 30 | - |
| Group | N | Age (Years Old) | Weight (kg) | Height (m) |
|---|---|---|---|---|
| EG | 25 | 26.3 ± 2.9 | 75.3 ± 11.2 | 1.76 ± 0.08 |
| CG | 20 | 25.8 ± 3.1 | 77.7 ± 10.8 | 1.74 ± 0.09 |
| M1 (Week 1) | M2 (Week 9) | M3 (Week 12) | % Change M1-M2 | % Change M2-M3 | |
|---|---|---|---|---|---|
| EG | |||||
| Add. Longus Muscular Thickness (cm) | |||||
| Left Leg | 0.718 ± 0.076 | 0.846 ± 0.081 ** | 0.722 ± 0.062 ## | +17.83 | −14.66 |
| Right Leg | 0.702 ± 0.081 | 0.831 ± 0.077 ** | 0.713 ± 0.069 ## | +18.38 | −14.20 |
| Hip abduction range (°) | |||||
| Left Leg | 57.6 ± 6.5 | 61.8 ± 6.2 * | 57.9 ± 5.3 # | +7.3 | −6.3 |
| Right Leg | 55.3 ± 7.5 | 59.2 ± 7.2 * | 56.3 ± 6.2 # | +7.1 | −4.9 |
| CG | |||||
| Add. Longus Muscular Thickness (cm) | |||||
| Left Leg | 0.689 ± 0.087 | 0.699 ± 0.077 | 0.672 ± 0.048 | +0.44 | −0.88 |
| Right Leg | 0.693 ± 0.091 | 0.690 ± 0.069 | 0.688 ± 0.059 | −0.43 | −0.29 |
| Hip abduction range (°) | |||||
| Left Leg | 53.1 ± 6.9 | 52.9 ± 8.2 | 51.6 ± 8.2 | −0.3 | −1.8 |
| Right Leg | 51.8 ± 7.3 | 52.2 ± 6.4 | 52.9 ± 7.1 | +0.8 | +1.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alonso-Fernández, D.; Fernández-Rodríguez, R.; Taboada-Iglesias, Y.; Gutiérrez-Sánchez, Á. Effects of Copenhagen Adduction Exercise on Muscle Architecture and Adductor Flexibility. Int. J. Environ. Res. Public Health 2022, 19, 6563. https://doi.org/10.3390/ijerph19116563
Alonso-Fernández D, Fernández-Rodríguez R, Taboada-Iglesias Y, Gutiérrez-Sánchez Á. Effects of Copenhagen Adduction Exercise on Muscle Architecture and Adductor Flexibility. International Journal of Environmental Research and Public Health. 2022; 19(11):6563. https://doi.org/10.3390/ijerph19116563
Chicago/Turabian StyleAlonso-Fernández, Diego, Rosana Fernández-Rodríguez, Yaiza Taboada-Iglesias, and Águeda Gutiérrez-Sánchez. 2022. "Effects of Copenhagen Adduction Exercise on Muscle Architecture and Adductor Flexibility" International Journal of Environmental Research and Public Health 19, no. 11: 6563. https://doi.org/10.3390/ijerph19116563
APA StyleAlonso-Fernández, D., Fernández-Rodríguez, R., Taboada-Iglesias, Y., & Gutiérrez-Sánchez, Á. (2022). Effects of Copenhagen Adduction Exercise on Muscle Architecture and Adductor Flexibility. International Journal of Environmental Research and Public Health, 19(11), 6563. https://doi.org/10.3390/ijerph19116563






