Health Needs and Their Relationship with Life Expectancy in People with and without Intellectual Disabilities in England
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources
2.2. Sample Population
2.3. Definition of Intellectual Disabilities and Health Needs
2.4. Statistical Methods
3. Results
3.1. Baseline Characteristics
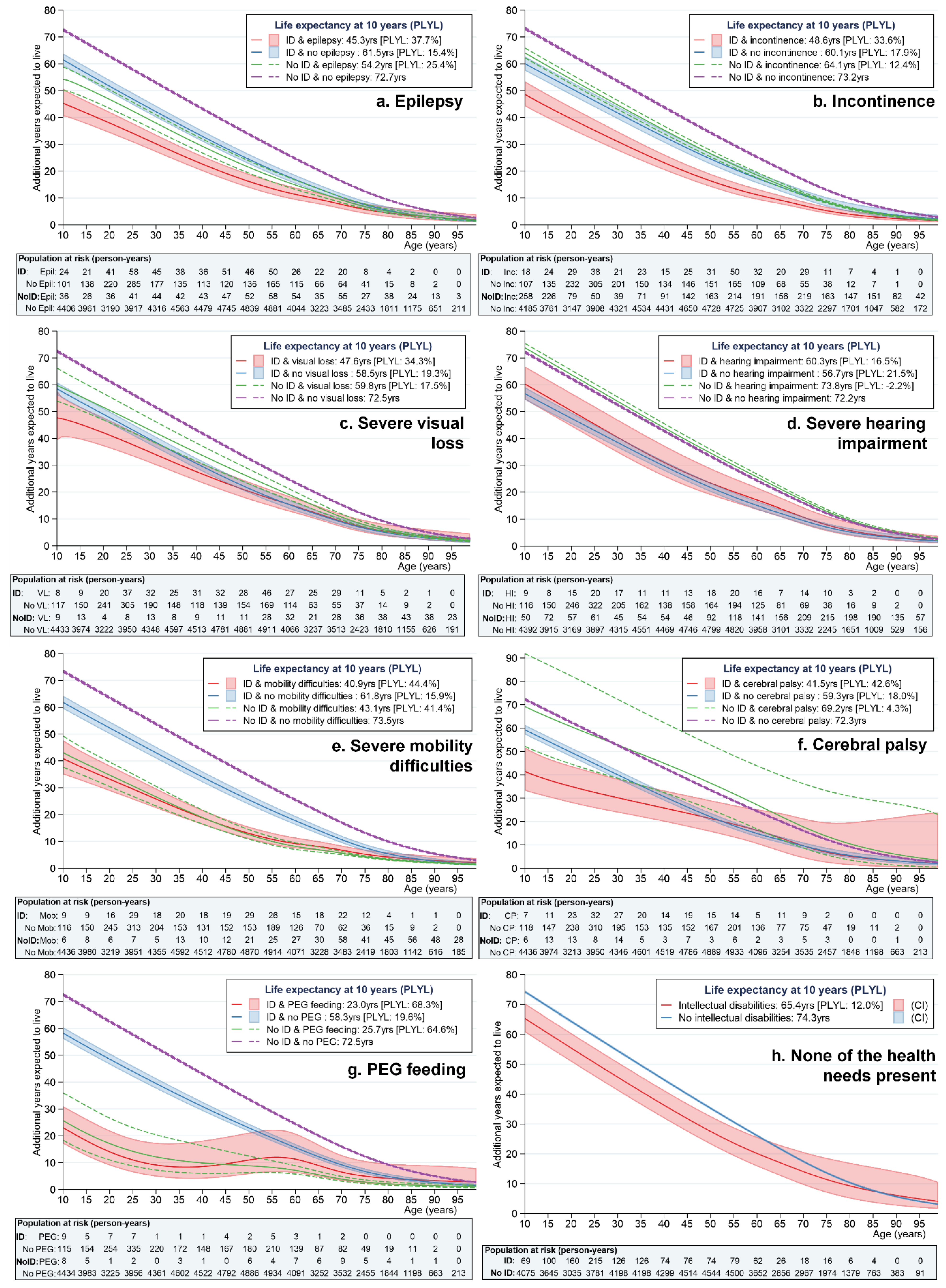
3.2. Life Expectancy
4. Discussion
4.1. Strengths and Limitations
4.2. Comparison with Existing Literature
4.3. Recommendations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization Commission on Social Determinants of Health. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health. 2008. Available online: https://www.who.int/social_determinants/thecommission/finalreport/en/ (accessed on 22 April 2021).
- United Nations General Assembly. Political Declaration of the High-Level Meeting on Universal Health Coverage: “Universal Health Coverage: Moving Together to Build a Healthier World” [A/RES/74/]. 2019. Available online: https://www.un.org/en/ga/74/resolutions.shtml (accessed on 22 April 2021).
- Department of Health and Social Care. Advancing Our Health: Prevention in the 2020s—Consultation Document. 2019. Available online: https://www.gov.uk/government/consultations/advancing-our-health-prevention-in-the-2020s/advancing-our-health-prevention-in-the-2020s-consultation-document (accessed on 27 July 2020).
- European Commission. The European Pillar of Social Rights in 20 Principles. 2017. Available online: https://ec.europa.eu/info/sites/default/files/social-summit-european-pillar-social-rights-booklet_en.pdf (accessed on 2 December 2021).
- European Commission. Union of Equality. Strategy for the Rights of Persons with Disabilities 2021–2030. 2021. Available online: https://ec.europa.eu/social/BlobServlet?docId=23707&langId=en (accessed on 30 November 2021).
- Office of Disease Prevention and Health Promotion; U.S. Department of Health and Human Services. Secretary’s Advisory Committee for Healthy People 2030. Report 7: Reviewing and Assessing the Set of Proposed Objectives for Healthy People 2030. 2019. Available online: https://www.healthypeople.gov/sites/default/files/Report%207_Reviewing%20Assessing%20Set%20of%20HP2030%20Objectives_Formatted%20EO_508_05.21.pdf (accessed on 30 November 2021).
- World Health Organization Regional Office for Europe. Better Health, Better Lives: Research Priorities. 2012. Available online: https://apps.who.int/iris/handle/10665/107303 (accessed on 3 December 2021).
- Australian Civil Society CRPD Shadow Report Working Group. Disability Rights Now. Australian Civil Society Shadow Report to the United Nations Committee on the Rights of Persons with Disabilities: UN CRPD Review. 2019. Available online: https://tbinternet.ohchr.org/Treaties/CRPD/Shared%20Documents/AUS/INT_CRPD_CSS_AUS_35639_E.pdf (accessed on 14 January 2022).
- Emerson, E.; Hatton, C. Health Inequalities and People with Intellectual Disabilities; Cambridge University Press: Cambridge, UK, 2014. [Google Scholar]
- Cooper, S.-A.; McLean, G.; Guthrie, B.; McConnachie, A.; Mercer, S.; Sullivan, F.; Morrison, J. Multiple physical and mental health comorbidity in adults with intellectual disabilities: Population-based cross-sectional analysis. BMC Fam. Pract. 2015, 16, 110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robertson, J.; Hatton, C.; Emerson, E.; Baines, S. The impact of health checks for people with intellectual disabilities: An updated systematic review of evidence. Res. Dev. Disabil. 2014, 35, 2450–2462. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tyrer, F.; Morriss, R.; Kiani, R.; Gangadharan, S.K.; Rutherford, M.J. Mortality disparities and deprivation among people with intellectual disabilities in England: 2000–2019. J. Epidemiol. Community Health 2022, 76, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Heslop, P.; Blair, P.; Fleming, P.; Hoghton, M.; Marriott, A.; Russ, L. Confidential Inquiry into Premature Deaths of People with Learning Disabilities (CIPOLD). Norah Fry Research Centre, University of Bristol. 2013. Available online: http://www.bristol.ac.uk/media-library/sites/cipold/migrated/documents/fullfinalreport.pdf (accessed on 14 January 2022).
- Trollor, J.; Srasuebkul, P.; Xu, H.; Howlett, S. Cause of death and potentially avoidable deaths in Australian adults with intellectual disability using retrospective linked data. BMJ Open 2017, 7, e013489. [Google Scholar] [CrossRef]
- Carey, I.M.; Hosking, F.J.; Harris, T.; DeWilde, S.; Beighton, C.; Cook, D.G. An evaluation of the effectiveness of annual health checks and quality of health care for adults with intellectual disability: An observational study using a primary care database. NIHR J. Libr. 2017, 9, 9. [Google Scholar] [CrossRef]
- Benchimol, E.I.; Smeeth, L.; Guttmann, A.; Harron, K.; Moher, D.; Petersen, I.; Sørensen, H.T.; von Elm, E.; Langan, S.M. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015, 12, e1001885. [Google Scholar] [CrossRef]
- Herrett, E.; Gallagher, A.M.; Bhaskaran, K.; Forbes, H.; Mathur, R.; van Staa, T.; Smeeth, L. Data resource profile: Clinical Practice Research Datalink (CPRD). Int. J. Epidemiol. 2015, 44, 827–836. [Google Scholar] [CrossRef]
- Florio, T.; Trollor, J. Mortality among a cohort of persons with an intellectual disability in New South Wales, Australia. J. Appl. Res. Intellect. Disabil. 2015, 28, 383–393. [Google Scholar] [CrossRef]
- Carey, I.M.; Shah, S.M.; Hosking, F.J.; DeWilde, S.; Harris, T.; Beighton, C.; Cook, D.G. Health characteristics and consultation patterns of people with intellectual disability: A cross-sectional database study in English general practice. Br. J. Gen. Pract. 2016, 66, e264. [Google Scholar] [CrossRef] [Green Version]
- Aaberg, K.M.; Gunnes, N.; Bakken, I.J.; Lund Søraas, C.; Berntsen, A.; Magnus, P.; Lossius, M.I.; Stoltenberg, C.; Chin, R.; Surén, P. Incidence and Prevalence of Childhood Epilepsy: A Nationwide Cohort Study. Pediatrics 2017, 139, e20163908. [Google Scholar] [CrossRef] [Green Version]
- National Institute for Health and Care Excellence (NICE). Epilepsies: Diagnosis and Management, Clinical Guideline [CG137] [updated May 2021]. 2012. Available online: https://www.nice.org.uk/guidance/cg137 (accessed on 18 March 2022).
- Blair, E.; Langdon, K.; McIntyre, S.; Lawrence, D.; Watson, L. Survival and mortality in cerebral palsy: Observations to the sixth decade from a data linkage study of a total population register and National Death Index. BMC Neurol. 2019, 19, 111. [Google Scholar] [CrossRef] [PubMed]
- Tyrer, F.; Bhaskaran, K.; Rutherford, M.J. Immortal time bias for life-long conditions in retrospective observational studies using electronic health records. BMC Med. Res. Methodol. 2022, 22, 86. [Google Scholar] [CrossRef] [PubMed]
- Tyrer, F.; Chudasama, Y.; Lambert, P.C.; Rutherford, M.J. Flexible Parametric Methods for Calculating Life Expectancy in Small Populations. 2022; under review. [Google Scholar]
- Chang, S.-R.; Lin, W.-A.; Lin, H.-H.; Lee, C.-N.; Chang, T.-C.; Lin, M.-I. Cumulative incidence of urinary incontinence and associated factors during pregnancy and after childbirth: A cohort study. Int. Urogynecology J. 2021. (online ahead of print). [Google Scholar] [CrossRef] [PubMed]
- Matta, R.; Hird, A.E.; Saskin, R.; Radomski, S.B.; Carr, L.; Kodama, R.T.; Nam, R.K.; Herschorn, S. Is There an Association between Urinary Incontinence and Mortality? A Retrospective Cohort Study. J. Urol. 2020, 203, 591–597. [Google Scholar] [CrossRef] [PubMed]
- Becker, R.; Nieczaj, R.; Egge, K.; Moll, A.; Meinhardt, M.; Schulz, R.J. Functional dysphagia therapy and PEG treatment in a clinical geriatric setting. Dysphagia 2011, 26, 108–116. [Google Scholar] [CrossRef]
- Tyrer, F.; Kiani, R.; Rutherford, M.J. Mortality, predictors and causes among people with intellectual disabilities: A systematic narrative review supplemented by machine learning. J. Intellect. Dev. Disabil. 2021, 46, 102–114. [Google Scholar] [CrossRef]
- Glasson, E.J.; Jacques, A.; Wong, K.; Bourke, J.; Leonard, H. Improved survival in Down syndrome over the last 60 years and the impact of perinatal Factors in recent decades. J. Pediatrics 2016, 169, 214–220. [Google Scholar] [CrossRef] [Green Version]
- Day, S.M.; Wu, Y.W.; Strauss, D.J.; Shavelle, R.M.; Reynolds, R.J. Causes of death in remote symptomatic epilepsy. Neurology 2005, 65, 216–222. [Google Scholar] [CrossRef] [Green Version]
- Public Health England. COVID-19 Deaths of People Identified as Having Learning Disabilities: Report; Public Health England: London, UK, 2020. Available online: https://www.gov.uk/government/publications/covid-19-deaths-of-people-with-learning-disabilities/covid-19-deaths-of-people-identified-as-having-learning-disabilities-summary (accessed on 23 February 2021).
- Read, J.M.; Green, C.A.; Harrison, E.M.; Docherty, A.B.; Funk, S.; Harrison, J.; Girvan, M.; Hardwick, H.E.; Turtle, L.; Dunning, J.; et al. Hospital-acquired SARS-CoV-2 infection in the UK’s first COVID-19 pandemic wave. Lancet 2021, 398, 1037–1038. [Google Scholar] [CrossRef]
- Hunskaar, S.; Arnold, E.P.; Burgio, K.; Diokno, A.C.; Herzog, A.R.; Mallett, V.T. Epidemiology and natural history of urinary incontinence. Int. Urogynecology J. Pelvic Floor Dysfunct. 2000, 11, 301–319. [Google Scholar] [CrossRef] [Green Version]
- Duralde, E.R.; Walter, L.C.; Van Den Eeden, S.K.; Nakagawa, S.; Subak, L.L.; Brown, J.S.; Thom, D.H.; Huang, A.J. Bridging the gap: Determinants of undiagnosed or untreated urinary incontinence in women. Am. J. Obstet. Gynecol. 2016, 214, e261–e266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanders, D.S.; Carter, M.J.; D’Silva, J.; James, G.; Bolton, R.P.; Willemse, P.J.; Bardhan, K.D. Percutaneous endoscopic gastrostomy: A prospective audit of the impact of guidelines in two district general hospitals in the United Kingdom. Am. J. Gastroenterol. 2002, 97, 2239–2245. [Google Scholar] [CrossRef] [PubMed]
- van Splunder, J.; Stilma, J.S.; Bernsen, R.M.; Evenhuis, H.M. Prevalence of visual impairment in adults with intellectual disabilities in the Netherlands: Cross-sectional study. Eye 2006, 20, 1004–1010. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Contrera, K.J.; Betz, J.; Genther, D.J.; Lin, F.R. Association of Hearing Impairment and Mortality in the National Health and Nutrition Examination Survey. JAMA Otolaryngol. Head Neck Surg. 2015, 141, 944–946. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oskoui, M.; Coutinho, F.; Dykeman, J.; Jetté, N.; Pringsheim, T. An update on the prevalence of cerebral palsy: A systematic review and meta-analysis. Dev. Med. Child Neurol. 2013, 55, 509–519. [Google Scholar] [CrossRef] [PubMed]
- Odding, E.; Roebroeck, M.E.; Stam, H.J. The epidemiology of cerebral palsy: Incidence, impairments and risk factors. Disabil. Rehabil. 2006, 28, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Reid, S.M.; Meehan, E.M.; Arnup, S.J.; Reddihough, D.S. Intellectual disability in cerebral palsy: A population-based retrospective study. Dev. Med. Child Neurol. 2018, 60, 687–694. [Google Scholar] [CrossRef]
- Tyrer, F.; Ling, S.; Bhaumik, S.; Gangadharan, S.K.; Khunti, K.; Gray, L.J.; Dunkley, A.J. Diabetes in adults with intellectual disability: Prevalence and associated demographic, lifestyle, independence and health factors. J. Intellect. Disabil. Res. 2020, 64, 287–295. [Google Scholar] [CrossRef]
- Melzer, D.; Lan, T.-Y.; Tom, B.D.M.; Deeg, D.J.H.; Guralnik, J.M. Variation in Thresholds for Reporting Mobility Disability Between National Population Subgroups and Studies. J. Gerontol. Ser. A 2004, 59, 1295–1303. [Google Scholar] [CrossRef] [Green Version]
| Characteristic | Intellectual Disability | No Intellectual Disability 1 | |||
|---|---|---|---|---|---|
| Number/ Median | Percent/ Range | Number/ Median | Percent/ Range | ||
| Total | 7794 | 100.0 | 176,807 | 100.0 | |
| Demographic characteristics | |||||
| Age (years) | 33.0 | 10–101 | 43.0 | 10–108 | |
| Gender | Male | 4448 | 57.1 | 86,669 | 49.0 |
| Female | 3346 | 42.9 | 90,138 | 51.0 | |
| Ethnicity | White | 6002 | 77.0 | 119,403 | 67.5 |
| South Asian | 211 | 2.7 | 7662 | 4.3 | |
| Black | 207 | 2.7 | 6236 | 3.5 | |
| Other | 280 | 3.6 | 8907 | 5.0 | |
| Not known | 1094 | 14.0 | 34,599 | 19.6 | |
| Observation period | |||||
| Length in cohort (years) | 1.5 | >0.0–2.7 | 1.9 | >0.0–2.7 | |
| Most common genetic/chromosomal syndromes 2 | |||||
| Down syndrome | 848 | 10.9 | - | ||
| Fragile X syndrome | 151 | 1.9 | - | ||
| Tuberous sclerosis | 60 | 0.8 | - | ||
| Edward syndrome | 29 | 0.4 | - | ||
| Prader–Willi syndrome | 27 | 0.3 | - | ||
| Severe health needs | |||||
| None (at baseline or follow-up) | 4174 | 53.6 | 159,716 | 90.3 | |
| Epilepsy | Baseline | 1456 | 18.7 | 2004 | 1.1 |
| during follow-up | 55 | 0.7 | 201 | 0.1 | |
| Incontinence | Baseline | 1039 | 13.3 | 6649 | 3.8 |
| during follow-up | 214 | 2.7 | 1177 | 0.7 | |
| Severe visual loss | Baseline | 1015 | 13.0 | 1075 | 0.6 |
| during follow-up | 227 | 2.9 | 204 | 0.1 | |
| Severe hearing impairment | Baseline | 551 | 7.1 | 5253 | 3.0 |
| during follow-up | 67 | 0.9 | 592 | 0.3 | |
| Severe mobility difficulties | Baseline | 818 | 10.5 | 1280 | 0.7 |
| during follow-up | 174 | 2.2 | 570 | 0.3 | |
| Cerebral palsy | Baseline | 658 | 8.4 | 261 | 0.1 |
| during follow-up | 20 | 0.3 | 6 | <0.1 | |
| PEG 3 feeding | Baseline | 132 | 1.7 | 180 | 0.1 |
| during follow-up | 20 | 0.3 | 54 | <0.1 | |
| Intellectual Disability | No Intellectual Disability | ||||||
|---|---|---|---|---|---|---|---|
| (11,631 Person-Years) | (296,324 Person-Years) | ||||||
| Health Need Present | Health Need Absent | Health Need Present | Health Need Absent | ||||
| Epilepsy: Additional years expected to live (95% CI): % life years lost 1 | |||||||
| At 10 years: | 45.3 (40.5–50.7) | 37.7% | 61.5 (59.2–63.9) | 15.4% | 54.2 (50.0–58.9) | 25.4% | 72.7 (72.3–73.1) |
| At 20 years: | 38.0 (34.2–42.1) | 39.3% | 51.7 (49.4–54.0) | 17.5% | 46.8 (43.4–50.4) | 25.4% | 62.8 (62.4–63.2) |
| At 40 years: | 22.6 (20.0–25.6) | 47.7% | 33.0 (31.0–35.1) | 23.8% | 29.3 (26.8–32.0) | 32.3% | 43.2 (42.9–43.6) |
| Incontinence: Additional years expected to live (95% CI): % life years lost 1 | |||||||
| At 10 years: | 48.6 (44.2–53.5) | 33.6% | 60.1 (57.5–62.8) | 17.9% | 64.1 (62.3–65.9) | 12.4% | 73.2 (72.8–73.7) |
| At 20 years: | 39.5 (35.5–43.9) | 37.3% | 50.8 (48.4–53.4) | 19.6% | 54.3 (52.5–56.0) | 14.2% | 63.3 (62.9–63.8) |
| At 40 years: | 23.2 (20.4–26.3) | 47.2% | 32.8 (30.6–35.1) | 25.2% | 35.3 (33.9–36.8) | 19.4% | 43.8 (43.4–44.2) |
| Severe visual loss: Additional years expected to live (95% CI): % life years lost 1 | |||||||
| At 10 years: | 47.6 (39.2–57.9) | 34.3% | 58.5 (56.2–60.9) | 19.3% | 59.8 (53.9–66.3) | 17.5% | 72.5 (72.1–73.0) |
| At 20 years: | 42.1 (37.1–47.8) | 32.8% | 49.0 (46.8–51.3) | 21.5% | 51.6 (46.9–56.8) | 17.6% | 62.7 (62.3–63.0) |
| At 40 years: | 27.6 (24.2–31.5) | 36.0% | 30.7 (28.8–32.7) | 28.9% | 34.7 (31.5–38.3) | 19.5% | 43.1 (42.8–43.5) |
| Severe hearing impairment: Additional years expected to live (95% CI): % life years lost 1 | |||||||
| At 10 years: | 60.3 (54.4–66.8) | 16.5% | 56.7 (54.4–59.1) | 21.5% | 73.8 (72.2–75.4) | −2.2% | 72.2 (71.8–72.6) |
| At 20 years: | 50.3 (44.5–56.9) | 19.0% | 47.5 (45.4–49.7) | 23.5% | 63.8 (62.2–65.4) | −2.4% | 62.3 (61.9–62.7) |
| At 40 years: | 31.1 (25.8–37.4) | 27.5% | 29.7 (27.9–31.6) | 30.6% | 44.0 (42.5–45.5) | −2.7% | 42.8 (42.5–43.2) |
| Severe mobility difficulties: Additional years expected to live (95% CI): % life years lost 1 | |||||||
| At 10 years: | 40.9 (35.0–47.8) | 44.4% | 61.8 (59.4–64.3) | 15.9% | 43.1 (37.7–49.3) | 41.4% | 73.5 (73.0–73.9) |
| At 20 years: | 33.2 (28.8–38.3) | 47.4% | 52.3 (50.0–54.7) | 17.5% | 34.7 (30.5–39.6) | 44.9% | 63.6 (63.2–64.0) |
| At 40 years: | 18.8 (16.2–21.7) | 57.4% | 34.0 (32.0–36.1) | 22.8% | 18.9 (16.5–21.7) | 57.0% | 44.1 (43.7–44.4) |
| Cerebral palsy: Additional years expected to live (95% CI): % life years lost 1 | |||||||
| At 10 years: | 41.5 (33.3–51.7) | 42.6% | 59.3 (57.2–61.4) | 18.0% | 69.2 (52.2–91.9) | 4.3% | 72.3 (71.9–72.7) |
| At 20 years: | 35.0 (28.0–43.8) | 44.0% | 49.6 (47.6–51.6) | 20.3% | 60.6 (44.6–82.3) | 3.2% | 62.5 (62.1–62.8) |
| At 40 years: | 25.8 (19.9–33.3) | 40.0% | 30.7 (28.9–32.5) | 28.6% | 44.9 (32.4–62.3) | −4.7% | 42.9 (42.6–43.3) |
| PEG 2 feeding: Additional years expected to live (95% CI): % life years lost 1 | |||||||
| At 10 years: | 23.0 (17.1–31.0) | 68.3% | 58.3 (56.2–60.5) | 19.6% | 25.7 (18.3–36.0) | 64.6% | 72.5 (72.1–72.9) |
| At 20 years: | 14.0 (9.0–22.0) | 76.8% | 48.6 (46.6–50.7) | 22.2% | 17.1 (11.0–26.6) | 72.0% | 62.6 (62.3–63.0) |
| At 40 years: | 8.5 (4.0–18.2) | 80.2% | 30.9 (29.2–32.7) | 28.3% | 9.9 (6.0–16.3) | 77.0% | 43.1 (42.8–43.5) |
| None of the health needs: Additional years expected to live (95% CI): % life years lost 1 | |||||||
| At 10 years: | - | 65.5 (60.3–71.1) | 12.0% | - | 74.3 (73.8–74.7) | ||
| At 20 years: | - | 55.5 (50.4–61.2) | 13.9% | - | 64.4 (63.9–64.8) | ||
| At 40 years: | - | 36.5 (31.5–42.3) | 19.0% | - | 44.8 (44.4–45.3) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tyrer, F.; Morriss, R.; Kiani, R.; Gangadharan, S.K.; Kundaje, H.; Rutherford, M.J. Health Needs and Their Relationship with Life Expectancy in People with and without Intellectual Disabilities in England. Int. J. Environ. Res. Public Health 2022, 19, 6602. https://doi.org/10.3390/ijerph19116602
Tyrer F, Morriss R, Kiani R, Gangadharan SK, Kundaje H, Rutherford MJ. Health Needs and Their Relationship with Life Expectancy in People with and without Intellectual Disabilities in England. International Journal of Environmental Research and Public Health. 2022; 19(11):6602. https://doi.org/10.3390/ijerph19116602
Chicago/Turabian StyleTyrer, Freya, Richard Morriss, Reza Kiani, Satheesh K. Gangadharan, Harish Kundaje, and Mark J. Rutherford. 2022. "Health Needs and Their Relationship with Life Expectancy in People with and without Intellectual Disabilities in England" International Journal of Environmental Research and Public Health 19, no. 11: 6602. https://doi.org/10.3390/ijerph19116602
APA StyleTyrer, F., Morriss, R., Kiani, R., Gangadharan, S. K., Kundaje, H., & Rutherford, M. J. (2022). Health Needs and Their Relationship with Life Expectancy in People with and without Intellectual Disabilities in England. International Journal of Environmental Research and Public Health, 19(11), 6602. https://doi.org/10.3390/ijerph19116602






