Dengue Seroprevalence and Factors Associated with Dengue Seropositivity in Petaling District, Malaysia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
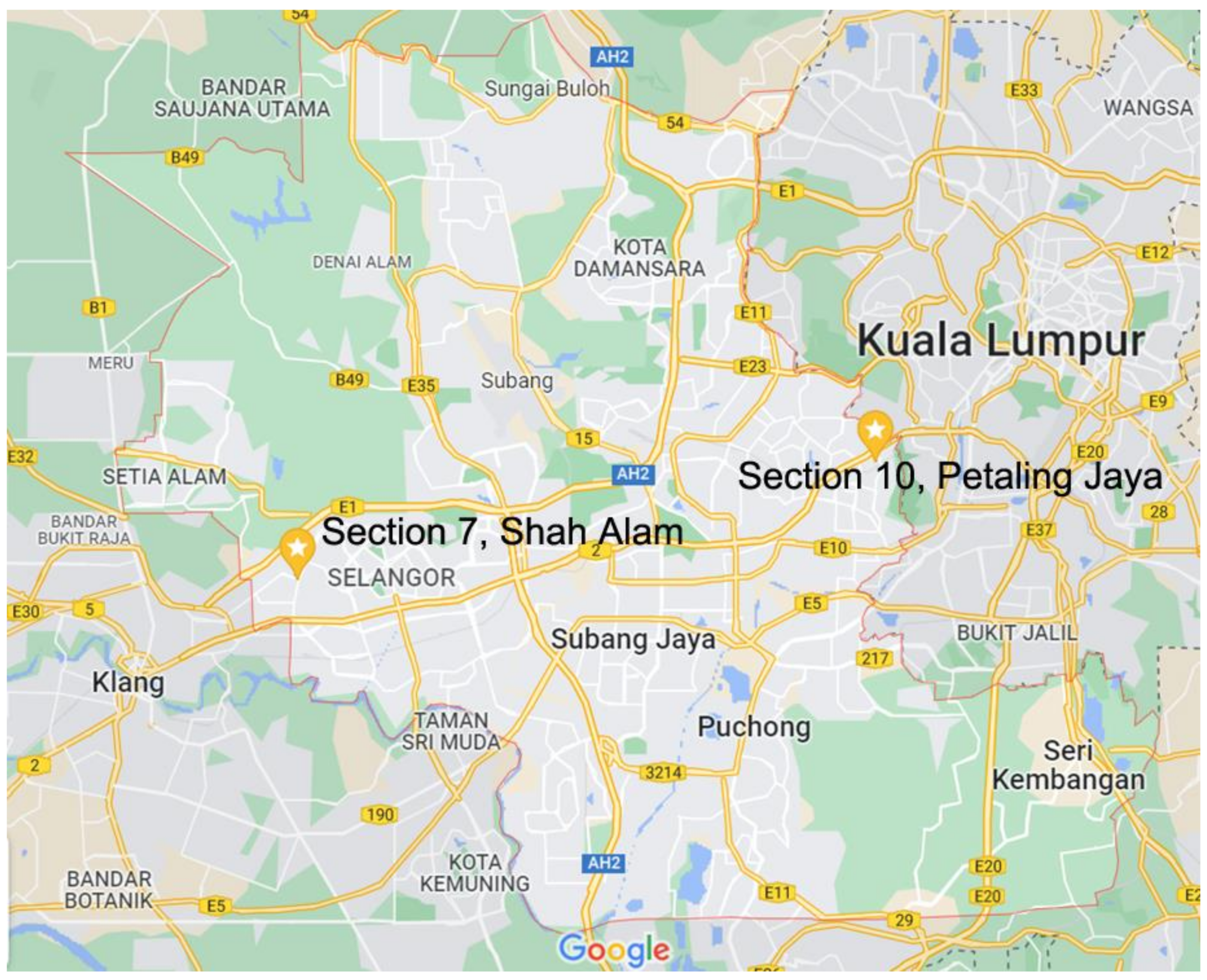
2.2. Study Setting and Study Population
2.3. DENV Serological Analysis
2.4. Data Collection
2.5. Data Analysis
3. Results
3.1. Characteristics and DENV Seroprevalence of the Study Participants
3.1.1. Socio-Demographic Factors
3.1.2. Environmental Factors
3.1.3. Preventive Practices
3.1.4. Knowledge
3.2. Factors Associated with DENV Seropositivity
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dhanoa, A.; Syed Hassan, S.; Jahan, N.K.; Reidpath, D.D.; Quek, K.F.; Ahmad, M.P.; Cheong, Y.M.; Lau, W.M.; Zain, A.Z.; Phipps, M.E.; et al. Seroprevalence of dengue among healthy adults in a rural community in Southern Malaysia: A pilot study. Infect. Dis. Poverty 2018, 7, 50–62. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Strategy for Dengue Prevention and Control 2012–2020; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Moi, M.L.; Takasaki, T.; Kurane, I. Human antibody response to dengue virus: Implications for dengue vaccine design. Trop. Med. Health 2016, 44, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shepard, D.S.; Undurraga, E.A.; Halasa, Y.A. Economic and Disease Burden of Dengue in Southeast Asia. PLoS Negl. Trop. Dis. 2013, 7, e2055. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- La Ruche, G.; Souarès, Y.; Armengaud, A.; Peloux-Petiot, F.; Delaunay, P.; Desprès, P.; Lenglet, A.; Jourdain, F.; Leparc-Goffart, I.; Charlet, F.; et al. First two autochthonous dengue virus infections in metropolitan France, September 2010. Eurosurveillance 2010, 15, 19676. [Google Scholar] [CrossRef]
- Mudin, R.N. Dengue Incidence and the Prevention and Control Program in Malaysia. IIUM Med. J. Malaysia 2015, 14, 5–10. [Google Scholar] [CrossRef]
- Mohd-Zaki, A.H.; Brett, J.; Ismail, E.; L’Azou, M. Epidemiology of Dengue Disease in Malaysia (2000–2012): A Systematic Literature Review. PLoS Negl. Trop. Dis. 2014, 8, e3159. [Google Scholar] [CrossRef]
- Syed Zakaria, S.Z.; Mohamad Roslan, N.A.; Mohktar, M.; Hadi, A.S.; Razman, M.R.; Md. Jahi, J.; Ramli, Z.; Nordin, N.H. Environmental Management in Dealing with Dengue Fever Cases Towards Urban Sustainability: Study on the Prevention and Control of Infectious Diseases Act 1988 (Act 342). Soc. Sci. 2013, 8, 295–299. [Google Scholar] [CrossRef]
- World Health Organization Regional Office for Southeast Asia. Comprehensive Guidelines for Prevention and Control of Dengue and Dengue Haemorrhagic Fever: Revised and Expanded Edition; World Health Organization Regional Office for Southeast Asia: New Delhi, India, 2011; ISBN 978-92-9022-387-0. [Google Scholar]
- Woon, Y.L.; Hor, C.P.; Lee, K.Y.; Mohd Anuar, S.F.Z.; Mudin, R.N.; Sheikh Ahmad, M.K.; Komari, S.; Amin, F.; Jamal, R.; Chen, W.S.; et al. Estimating dengue incidence and hospitalization in Malaysia, 2001 to 2013. BMC Public Health 2018, 18, 946. [Google Scholar] [CrossRef] [Green Version]
- Chew, C.H.; Woon, Y.L.; Amin, F.; Adnan, T.H.; Abdul Wahab, A.H.; Ahmad, Z.E.; Bujang, M.A.; Abdul Hamid, A.M.; Jamal, R.; Chen, W.S.; et al. Rural-urban comparisons of dengue seroprevalence in Malaysia. BMC Public Health 2016, 16, 824. [Google Scholar] [CrossRef] [Green Version]
- Imai, N.; Dorigatti, I.; Cauchemez, S.; Ferguson, N.M. Estimating Dengue Transmission Intensity from Sero-Prevalence Surveys in Multiple Countries. PLoS Negl. Trop. Dis. 2015, 9, e0003719. [Google Scholar] [CrossRef] [Green Version]
- Azami, N.A.M.; Moi, M.L.; Salleh, S.A.; Neoh, H.; Kamaruddin, M.A.; Jalal, N.A.; Ismail, N.; Takasaki, T.; Kurane, I.; Jamal, R. Dengue epidemic in Malaysia: Urban versus rural comparison of dengue immunoglobulin G seroprevalence among Malaysian adults aged 35–74 years. Trans. R. Soc. Trop. Med. Hyg. 2020, 114, 798–811. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. World Medical Association Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ng, A.; Mohamed Firouz, A.M.; Khalidi, J.R.; Muhtar, M.A.; Tumin, S.A.; Tan, K.M.; Tan, T.T.; Tan, G.Z. The State of Households 2018: Different Realities; Khazanah Research Institute: Kuala Lumpur, Malaysia, 2018. [Google Scholar]
- Zainudin, Z.; Shamsuddin, S.M. Predictive analytics in Malaysian dengue data from 2010 until 2015 using BigML. Int. J. Adv. Soft Comput. Its Appl. 2016, 8, 18–30. [Google Scholar]
- Ghani, N.; Shohaimi, S.; Hee, A.; Chee, H.-Y.; Emmanuel, O.; Alaba Ajibola, L. Comparison of Knowledge, Attitude, and Practice among Communities Living in Hotspot and Non-Hotspot Areas of Dengue in Selangor, Malaysia. Trop. Med. Infect. Dis. 2019, 4, 37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malaysian Space Agency. Disease Control Division MOH Malaysia iDengue—Dengue Definition. Available online: https://idengue.mysa.gov.my/ide_v3/definition.html#page=6 (accessed on 20 August 2021).
- ESRI. Malaysia Average Household Size. Available online: https://www.arcgis.com/home/item.html?id=69f2d666483f4bf79e3e7b9c42a12d39 (accessed on 4 November 2016).
- Chatchen, S.; Sabchareon, A.; Sirivichayakul, C. Serodiagnosis of asymptomatic dengue infection. Asian Pac. J. Trop. Med. 2017, 10, 11–14. [Google Scholar] [CrossRef]
- Chong, Z.L.; Soe, H.J.; Ismail, A.A.; Mahboob, T.; Chandramathi, S.; Sekaran, S.D. Evaluation of the Diagnostic Accuracy of a New Biosensors-Based Rapid Diagnostic Test for the Point-Of-Care Diagnosis of Previous and Recent Dengue Infections in Malaysia. Biosensors 2021, 11, 129. [Google Scholar] [CrossRef]
- Lukman, N.; Salim, G.; Kosasih, H.; Susanto, N.H.; Parwati, I.; Fitri, S.; Alisjahbana, B.; Widjaja, S.; Williams, M. Comparison of the Hemagglutination Inhibition Test and IgG ELISA in Categorizing Primary and Secondary Dengue Infections Based on the Plaque Reduction Neutralization Test. Biomed Res. Int. 2016, 2016, 5253842. [Google Scholar] [CrossRef] [Green Version]
- Maeda, A.; Maeda, J. Review of diagnostic plaque reduction neutralization tests for flavivirus infection. Vet. J. 2013, 195, 33–40. [Google Scholar] [CrossRef]
- World Health Organization. Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control—New Edition; World Health Organization: Geneva, Switzerland, 2009; ISBN 978-92-4-154787-1. [Google Scholar]
- McHugh, M.L. Cramér’s V Coefficient. In The SAGE Encyclopedia of Educational Research, Measurement, and Evaluation; Frey, B.B., Ed.; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2018; ISBN 978-1-50632-615-3. [Google Scholar]
- Low, S.-L.; Lam, S.; Wong, W.-Y.; Teo, D.; Ng, L.-C.; Tan, L.-K. Dengue Seroprevalence of Healthy Adults in Singapore: Serosurvey Among Blood Donors, 2009. Am. J. Trop. Med. Hyg. 2015, 93, 40–45. [Google Scholar] [CrossRef]
- Coudeville, L.; Baurin, N.; Shepard, D.S. The potential impact of dengue vaccination with, and without, pre-vaccination screening. Vaccine 2020, 38, 1363–1369. [Google Scholar] [CrossRef]
- World Health Organization. Dengue vaccine: WHO position paper, September 2018—Recommendations. Vaccine 2019, 37, 4848–4849. [Google Scholar] [CrossRef] [PubMed]
- Selvarajoo, S.; Liew, J.W.K.; Tan, W.; Lim, X.Y.; Refai, W.F.; Zaki, R.A.; Sethi, N.; Wan Sulaiman, W.Y.; Lim, Y.A.L.; Vadivelu, J.; et al. Knowledge, attitude and practice on dengue prevention and dengue seroprevalence in a dengue hotspot in Malaysia: A cross-sectional study. Sci. Rep. 2020, 10, 9534. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.S.; Wong, C.H.; Cillekens, L. Dengue Antibodies in a Suburban Community in Malaysia. Med. J. Malays. 2003, 58, 142–143. [Google Scholar]
- International Organization for Migration. Overview of Internal Migration in Malaysia; International Organization for Migration: Bangkok, Thailand, 2016. [Google Scholar]
- Tam, C.C.; O’Driscoll, M.; Taurel, A.F.; Nealon, J.; Hadinegoro, S.R. Geographic variation in dengue seroprevalence and force of infection in the urban paediatric population of Indonesia. PLoS Negl. Trop. Dis. 2018, 12, e006935. [Google Scholar] [CrossRef] [Green Version]
- Yew, Y.W.; Tun, Y.; Ang, L.W.; Ng, L.C.; Yap, G.; James, L.; Chew, S.K.; Goh, K.T. Seroepidemiology of dengue virus infection among adults in Singapore. Ann. Acad. Med. Singap. 2009, 38, 667–675. [Google Scholar] [PubMed]
- Ang, L.W.; Cutter, J.; James, L.; Goh, K.T. Seroepidemiology of dengue virus infection in the adult population in tropical Singapore. Epidemiol. Infect. 2015, 143, 1585–1593. [Google Scholar] [CrossRef]
- Lopez, A.L.; Adams, C.; Ylade, M.; Jadi, R.; Daag, J.V.; Molloy, C.T.; Agrupis, K.A.; Kim, D.R.; Silva, M.W.; Yoon, I.-K.; et al. Determining dengue virus serostatus by indirect IgG ELISA compared with focus reduction neutralisation test in children in Cebu, Philippines: A prospective population-based study. Lancet Glob. Health 2021, 9, e44–e51. [Google Scholar] [CrossRef]
- Doum, D.; Overgaard, H.J.; Mayxay, M.; Suttiprapa, S.; Saichua, P.; Ekalaksananan, T.; Tongchai, P.; Rahman, M.S.; Haque, U.; Phommachanh, S.; et al. Dengue Seroprevalence and Seroconversion in Urban and Rural Populations in Northeastern Thailand and Southern Laos. Int. J. Environ. Res. Public Health 2020, 17, 9134. [Google Scholar] [CrossRef]
- Chiaravalloti-Neto, F.; da Silva, R.A.; Zini, N.; da Silva, G.C.D.; da Silva, N.S.; Parra, M.C.P.; Dibo, M.R.; Estofolete, C.F.; Fávaro, E.A.; Dutra, K.R.; et al. Seroprevalence for dengue virus in a hyperendemic area and associated socioeconomic and demographic factors using a cross-sectional design and a geostatistical approach, state of São Paulo, Brazil. BMC Infect. Dis. 2019, 19, 441. [Google Scholar] [CrossRef]
- Velasco-Salas, Z.I.; Sierra, G.M.; Guzmán, D.M.; Zambrano, J.; Vivas, D.; Comach, G.; Wilschut, J.C.; Tami, A. Dengue Seroprevalence and Risk Factors for Past and Recent Viral Transmission in Venezuela: A Comprehensive Community-Based Study. Am. J. Trop. Med. Hyg. 2014, 91, 1039–1048. [Google Scholar] [CrossRef] [Green Version]
- Velandia-Romero, M.L.; Coronel-Ruiz, C.; Castro-Bonilla, L.; Camacho-Ortega, S.; Calderón-Peláez, M.A.; Castellanos, A.; Olano, V.A.; Porras, A.; Arevalo-Herrera, M.; Villamil-Gómez, W.; et al. Prevalence of dengue antibodies in healthy children and adults in different Colombian endemic areas. Int. J. Infect. Dis. 2020, 91, 9–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muhammad Azami, N.A.; Salleh, S.A.; Neoh, H.; Syed Zakaria, S.Z.; Jamal, R. Dengue epidemic in Malaysia: Not a predominantly urban disease anymore. BMC Res. Notes 2011, 4, 216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abdul-Ghani, R.; Mahdy, M.A.K.; Al-Eryani, S.M.A.; Fouque, F.; Lenhart, A.E.; Alkwri, A.; Al-Mikhlafi, A.M.; Wilke, A.B.B.; Thabet, A.A.Q.; Beier, J.C. Impact of population displacement and forced movements on the transmission and outbreaks of Aedes-borne viral diseases: Dengue as a model. Acta Trop. 2019, 197, 105066. [Google Scholar] [CrossRef] [PubMed]
- Tsuzuki, A.; Ron Duoc, V.T.; Sunahara, T.; Suzuki, M.; Oan Le, N.H.; Higa, Y.; Yoshida, L.-M.; Hasebe, F.; Phong, T.V.; Minakawa, N. Possible association between recent migration and hospitalisation for dengue in an urban population: A prospective case-control study in northern Vietnam. Trop. Biomed. 2014, 31, 698–708. [Google Scholar] [PubMed]
- Padmanabha, H.; Correa, F.; Rubio, C.; Baeza, A.; Osorio, S.; Mendez, J.; Jones, J.H.; Diuk-Wasser, M.A. Human Social Behavior and Demography Drive Patterns of Fine-Scale Dengue Transmission in Endemic Areas of Colombia. PLoS ONE 2015, 10, e0144451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matangkasombut, P.; Manopwisedjaroen, K.; Pitabut, N.; Thaloengsok, S.; Suraamornkul, S.; Yingtaweesak, T.; Duong, V.; Sakuntabhai, A.; Paul, R.; Singhasivanon, P. Dengue viremia kinetics in asymptomatic and symptomatic infection. Int. J. Infect. Dis. 2020, 101, 90–97. [Google Scholar] [CrossRef]
- Reiner, R.C.; Stoddard, S.T.; Scott, T.W. Socially structured human movement shapes dengue transmission despite the diffusive effect of mosquito dispersal. Epidemics 2014, 6, 30–36. [Google Scholar] [CrossRef] [Green Version]
- Wong, L.P.; AbuBakar, S.; Chinna, K. Community Knowledge, Health Beliefs, Practices and Experiences Related to Dengue Fever and Its Association with IgG Seropositivity. PLoS Negl. Trop. Dis. 2014, 8, e2789. [Google Scholar] [CrossRef] [Green Version]
- Jamjoom, G.A.; Azhar, E.I.; Kao, M.A.; Radadi, R.M. Seroepidemiology of Asymptomatic Dengue Virus Infection in Jeddah, Saudi Arabia. Virol. Res. Treat. 2016, 7, VRT.S34187. [Google Scholar] [CrossRef] [Green Version]
- Prayitno, A.; Taurel, A.-F.; Nealon, J.; Satari, H.I.; Karyanti, M.R.; Sekartini, R.; Soedjatmiko, S.; Gunardi, H.; Medise, B.E.; Sasmono, R.T.; et al. Dengue seroprevalence and force of primary infection in a representative population of urban dwelling Indonesian children. PLoS Negl. Trop. Dis. 2017, 11, e0005621. [Google Scholar] [CrossRef] [Green Version]
- Khetarpal, N.; Khanna, I. Dengue Fever: Causes, Complications, and Vaccine Strategies. J. Immunol. Res. 2016, 2016, 6803098. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Halstead, S.B.; Dans, L.F. Dengue infection and advances in dengue vaccines for children. Lancet Child Adolesc. Health 2019, 3, 734–741. [Google Scholar] [CrossRef]
- Biswal, S.; Reynales, H.; Saez-Llorens, X.; Lopez, P.; Borja-Tabora, C.; Kosalaraksa, P.; Sirivichayakul, C.; Watanaveeradej, V.; Rivera, L.; Espinoza, F.; et al. Efficacy of a Tetravalent Dengue Vaccine in Healthy Children and Adolescents. N. Engl. J. Med. 2019, 381, 2009–2019. [Google Scholar] [CrossRef] [PubMed]
- Takeda Pharmaceutical Company Limited. Potential Impact of Takeda’s Dengue Vaccine Candidate Reinforced by Long-Term Safety and Efficacy Results. Available online: https://www.takeda.com/newsroom/newsreleases/2021/potential-impact-of-takedas-dengue-vaccine-candidate-reinforced-by--long-term-safety-and-efficacy-results/ (accessed on 20 August 2021).
- Pan, Y.-H.; Liao, M.-Y.; Chien, Y.-W.; Ho, T.-S.; Ko, H.-Y.; Yang, C.-R.; Chang, S.-F.; Yu, C.-Y.; Lin, S.-Y.; Shih, P.-W.; et al. Use of seroprevalence to guide dengue vaccination plans for older adults in a dengue non-endemic country. PLoS Negl. Trop. Dis. 2021, 15, e0009312. [Google Scholar] [CrossRef] [PubMed]
- Ding, C.H.; Rashid, Z.Z.; Rahman, M.M.; Khang, N.; Low, W.N.; Hussin, N.; Marzuki, M.I.; Jaafar, A.N.; Roslan, N.A.N.; Chandrasekaran, T. Seroprevalence of Acute Dengue in a Malaysian Tertiary Medical Centre. Pak. J. Med. Sci. 2016, 32, 495–498. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, R.; Suzilah, I.; Najdah, W.M.A.W.; Topek, O.; Mustafakamal, I.; Lee, H.L. Factors determining dengue outbreak in Malaysia. PLoS ONE 2018, 13, e0193326. [Google Scholar] [CrossRef]
- Li, C.; Wu, X.; Sheridan, S.; Lee, J.; Wang, X.; Yin, J.; Han, J. Interaction of climate and socio-ecological environment drives the dengue outbreak in epidemic region of China. PLoS Negl. Trop. Dis. 2021, 15, e0009761. [Google Scholar] [CrossRef]

| Characteristics | n (%) | No. of People DENV Seropositive (% of n) | No. of People DENV Seronegative (% of n) |
|---|---|---|---|
| Total | 500 (100.0) | 395 (79.0) | 105 (21.0) |
| Socio-demographic factors | |||
| Age Group | |||
| 22 (4.4) | 5 (22.7) | 17 (77.3) |
| 25 (5.0) | 19 (76.0) | 6 (24.0) |
| 88 (17.6) | 71 (80.7) | 17 (19.3) |
| 139 (27.8) | 103 (74.1) | 36 (25.9) |
| 52 (10.4) | 39 (75.0) | 13 (25.0) |
| 76 (15.2) | 67 (88.2) | 9 (11.8) |
| 59 (11.8) | 54 (91.5) | 5 (8.5) |
| 39 (7.8) | 37 (94.9) | 2 (5.1) |
| Gender | |||
| 260 (52.0) | 207 (79.6) | 53 (20.4) |
| 240 (48.0) | 188 (78.3) | 52 (21.7) |
| Location | |||
| 91 (18.2) | 66 (72.5) | 25 (27.5) |
| 409 (81.8) | 329 (80.4) | 80 (19.6) |
| Ethnicity | |||
| 380 (76.0) | 306 (80.5) | 74 (19.5) |
| 36 (7.2) | 29 (80.6) | 7 (19.4) |
| 54 (10.8) | 41 (75.9) | 13 (24.1) |
| 30 (6.0) | 19 (65.3) | 11 (36.7) |
| Nationality | |||
| 478 (95.6) | 379 (79.3) | 99 (20.7) |
| 22 (4.4) | 16 (72.7) | 6 (27.3) |
| Marital Status | |||
| 286 (57.2) | 210 (73.4) | 76 (26.6) |
| 214 (42.8) | 185 (86.5) | 29 (13.5) |
| Education status (n = 498) | |||
| 92 (18.4) | 63 (68.5) | 29 (31.5) |
| 182 (36.6) | 156 (85.7) | 26 (14.3) |
| 224 (45.0) | 174 (77.7) | 50 (22.3) |
| Occupation (n = 483) | |||
| 144 (29.8) | 109 (75.7) | 35 (24.3) |
| 254 (52.6) | 213 (83.9) | 41 (16.1) |
| 85 (17.6) | 65 (76.5) | 20 (23.5) |
| Household size | |||
| 64 (12.8) | 56 (87.5) | 8 (12.5) |
| 280 (56.0) | 215 (76.8) | 65 (23.2) |
| 156 (31.2) | 124 (79.5) | 32 (20.5) |
| Environmental factors | |||
| Type of house | |||
| 91 (18.2) | 66 (72.5) | 25 (27.5) |
| 409 (81.8) | 329 (80.4) | 80 (19.6) |
| House level (n = 499) | |||
| 91 (18.2) | 66 (72.5) | 25 (27.5) |
| 155 (31.1) | 133 (85.8) | 22 (14.2) |
| 253 (50.7) | 195 (77.1) | 58 (22.9) |
| Indoor potted plants | |||
| 55 (11.0) | 41 (74.6) | 91 (20.4) |
| 445 (89.0) | 354 (79.6) | 14 (25.4) |
| Preventive practices | |||
| Usage of screened windows | |||
| 53 (10.6) | 43 (81.1) | 10 (18.9) |
| 447 (89.4) | 352 (78.8) | 95 (21.2) |
| Usage of screened doors | |||
| 18 (3.6) | 14 (77.8) | 4 (22.2) |
| 482 (96.4) | 381 (79.1) | 101 (20.9) |
| Usage of bed net | |||
| 5 (1.0) | 5 (100.0) | 0 (0.0) |
| 495 (99.0) | 390 (78.8) | 105 (21.2) |
| Usage of mosquito coil/mat/liquid vaporiser | |||
| 182 (36.4) | 144 (79.1) | 38 (20.9) |
| 318 (63.6) | 251 (78.9) | 67 (21.1) |
| Usage of insecticide aerosol spray | |||
| 411 (82.2) | 318 (77.4) | 93 (22.6) |
| 89 (17.8) | 77 (86.5) | 12 (13.5) |
| Usage of air conditioner at home | |||
| 206 (41.2) | 165 (80.1) | 41 (19.9) |
| 294 (58.8) | 230 (78.2) | 64 (21.8) |
| Usage of mosquito repellent cream/spray | |||
| 69 (13.8) | 54 (78.3) | 15 (21.7) |
| 431 (86.2) | 341 (79.1) | 90 (20.9) |
| Usage of larvicide (n = 499) | |||
| 179 (35.9) | 159 (88.8) | 20 (11.2) |
| 239 (47.9) | 188 (78.7) | 51 (21.3) |
| 81 (16.2) | 47 (58.0) | 34 (42.0) |
| Eliminate stagnant water indoor | |||
| 37 (7.4) | 29 (78.4) | 8 (21.6) |
| 104 (20.8) | 86 (82.7) | 18 (17.3) |
| 234 (46.8) | 193 (82.5) | 41 (17.5) |
| 125 (25.0) | 87 (69.6) | 38 (30.4) |
| Eliminate stagnant water outdoor | |||
| 36 (7.2) | 29 (80.6) | 7 (19.4) |
| 84 (16.8) | 70 (83.3) | 14 (16.7) |
| 165 (33.0) | 134 (81.2) | 31 (18.8) |
| 215 (43.0) | 162 (75.4) | 53 (24.6) |
| Knowledge (Aedes biting time) | |||
| Good knowledge (Aedes biting time) 1 | |||
| 133 (26.6) | 114 (85.7) | 19 (14.3) |
| 367 (73.4) | 281 (76.6) | 86 (23.4) |
| Characteristics | Univariable Analysis | Multivariable Analysis | ||||
|---|---|---|---|---|---|---|
| Crude OR | 95% CI | p-Value | Adjusted OR | 95% CI | p-Value | |
| Age Group * | ||||||
| 1.00 | Reference | 1.00 | Reference | ||
| 18.71 | 3.63–96.35 | <0.001 | 13.43 | 2.77–65.22 | 0.001 |
| 27.95 | 6.66–117.25 | <0.001 | 23.81 | 5.61–101.12 | <0.001 |
| 19.50 | 4.98–76.33 | <0.001 | 12.75 | 2.85–57.00 | 0.001 |
| 20.84 | 4.80–90.41 | <0.001 | 15.24 | 3.13–74.29 | 0.001 |
| 53.63 | 11.51–249.83 | <0.001 | 35.06 | 6.62–185.59 | <0.001 |
| 81.93 | 15.47–433.92 | <0.001 | 94.63 | 14.36–623.77 | <0.001 |
| 165.98 | 20.43–1348.46 | <0.001 | 384.77 | 39.27–3769.97 | <0.001 |
| Gender | ||||||
| 1.00 | Reference | ||||
| 0.81 | 0.48–1.36 | 0.429 | |||
| Location | ||||||
| 1.00 | Reference | ||||
| 1.46 | 0.70–3.07 | 0.314 | |||
| Ethnicity | ||||||
| 1.00 | Reference | ||||
| 1.01 | 0.33–3.13 | 0.985 | |||
| 0.75 | 0.30–1.92 | 0.556 | |||
| 0.49 | 0.16–1.54 | 0.223 | |||
| Nationality | ||||||
| 1.00 | Reference | ||||
| 1.16 | 0.28–4.81 | 0.834 | |||
| Marital Status | ||||||
| 1.00 | Reference | ||||
| 2.87 | 1.62–5.07 | <0.001 | |||
| Educational Status (n = 498) | ||||||
| 1.00 | Reference | ||||
| 3.22 | 1.55–6.67 | 0.002 | |||
| 1.85 | 0.95–3.60 | 0.072 | |||
| Occupation (n = 483) | ||||||
| 1.00 | Reference | ||||
| 2.24 | 1.17–4.28 | 0.015 | |||
| 1.01 | 0.46–2.20 | 0.988 | |||
| Household size | ||||||
| 1.00 | Reference | 1.00 | Reference | ||
| 0.42 | 0.16–1.12 | 0.083 | 0.66 | 0.24–1.80 | 0.420 |
| 0.52 | 0.18–1.53 | 0.233 | 0.66 | 0.22–2.00 | 0.463 |
| Type of house | ||||||
| 1.00 | Reference | ||||
| 1.46 | 0.70–3.07 | 0.314 | |||
| House level (n = 499) | ||||||
| 1.00 | Reference | 1.00 | Reference | ||
| 2.36 | 0.97–5.74 | 0.059 | 8.98 | 3.16–25.12 | <0.001 |
| 1.13 | 0.52–2.46 | 0.750 | 4.82 | 1.89–12.32 | 0.001 |
| Indoor potted plants | ||||||
| 0.77 | 0.31–1.88 | 0.560 | |||
| 1.00 | Reference | ||||
| Usage of screened windows | ||||||
| 1.00 | Reference | ||||
| 0.72 | 0.27–1.94 | 0.513 | |||
| Usage of screened doors | ||||||
| 1.00 | Reference | ||||
| 1.23 | 0.25–6.12 | 0.802 | |||
| Usage of bed net | ||||||
| NA 1 | - | ||||
| ||||||
| Usage of mosquito coil/mat/liquid vaporiser | ||||||
| 1.00 | Reference | ||||
| 1.05 | 0.57–1.91 | 0.881 | |||
| Usage of insecticide aerosol spray | ||||||
| 1.00 | Reference | 1.00 | Reference | ||
| 2.13 | 0.96–4.70 | 0.062 | 1.96 | 0.85–4.52 | 0.116 |
| Use of air conditioner at home | ||||||
| 1.00 | Reference | ||||
| 0.89 | 0.48–1.63 | 0.696 | |||
| Usage of mosquito repellent cream/spray | ||||||
| 1.00 | Reference | ||||
| 1.10 | 0.51–2.37 | 0.813 | |||
| Usage of larvicide (n = 499) | ||||||
| 1.00 | Reference | ||||
| 0.54 | 0.28–1.03 | 0.062 | |||
| 0.15 | 0.07–0.32 | <0.001 | |||
| Eliminate stagnant water indoor | ||||||
| 1.00 | Reference | 1.00 | Reference | ||
| 1.16 | 0.38–3.56 | 0.789 | 1.02 | 0.33–3.22 | 0.967 |
| 1.09 | 0.40–2.97 | 0.867 | 1.13 | 0.41–3.15 | 0.811 |
| 0.44 | 0.15–1.26 | 0.127 | 1.21 | 0.37–3.96 | 0.756 |
| Eliminate stagnant water outdoor | ||||||
| 1.00 | Reference | ||||
| 1.41 | 0.43–4.64 | 0.574 | |||
| 0.95 | 0.32–2.78 | 0.925 | |||
| 0.57 | 0.20–1.65 | 0.299 | |||
| Good knowledge (Aedes biting time) | ||||||
| 1.00 | Reference | 1.00 | Reference | ||
| 0.50 | 0.27–0.94 | 0.031 | 0.59 | 0.30–1.18 | 0.135 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ng, R.J.; Chong, Z.L.; Abdul Mutalip, M.H.; Ng, C.-W. Dengue Seroprevalence and Factors Associated with Dengue Seropositivity in Petaling District, Malaysia. Int. J. Environ. Res. Public Health 2022, 19, 7170. https://doi.org/10.3390/ijerph19127170
Ng RJ, Chong ZL, Abdul Mutalip MH, Ng C-W. Dengue Seroprevalence and Factors Associated with Dengue Seropositivity in Petaling District, Malaysia. International Journal of Environmental Research and Public Health. 2022; 19(12):7170. https://doi.org/10.3390/ijerph19127170
Chicago/Turabian StyleNg, Rui Jie, Zhuo Lin Chong, Mohd Hatta Abdul Mutalip, and Chiu-Wan Ng. 2022. "Dengue Seroprevalence and Factors Associated with Dengue Seropositivity in Petaling District, Malaysia" International Journal of Environmental Research and Public Health 19, no. 12: 7170. https://doi.org/10.3390/ijerph19127170
APA StyleNg, R. J., Chong, Z. L., Abdul Mutalip, M. H., & Ng, C.-W. (2022). Dengue Seroprevalence and Factors Associated with Dengue Seropositivity in Petaling District, Malaysia. International Journal of Environmental Research and Public Health, 19(12), 7170. https://doi.org/10.3390/ijerph19127170






