Using Artificial Intelligence to Enhance Ongoing Psychological Interventions for Emotional Problems in Real- or Close to Real-Time: A Systematic Review
Abstract
:1. Introduction
1.1. The Challenge of Treating Emotional Problems
1.2. The Role of Information and Communication Technologies (ICTs) in the Treatment of People with EDs
1.3. Limitations of (Internet-Based) Psychological Treatments for EDs and Contributions of Artificial Intelligence
2. Materials and Methods
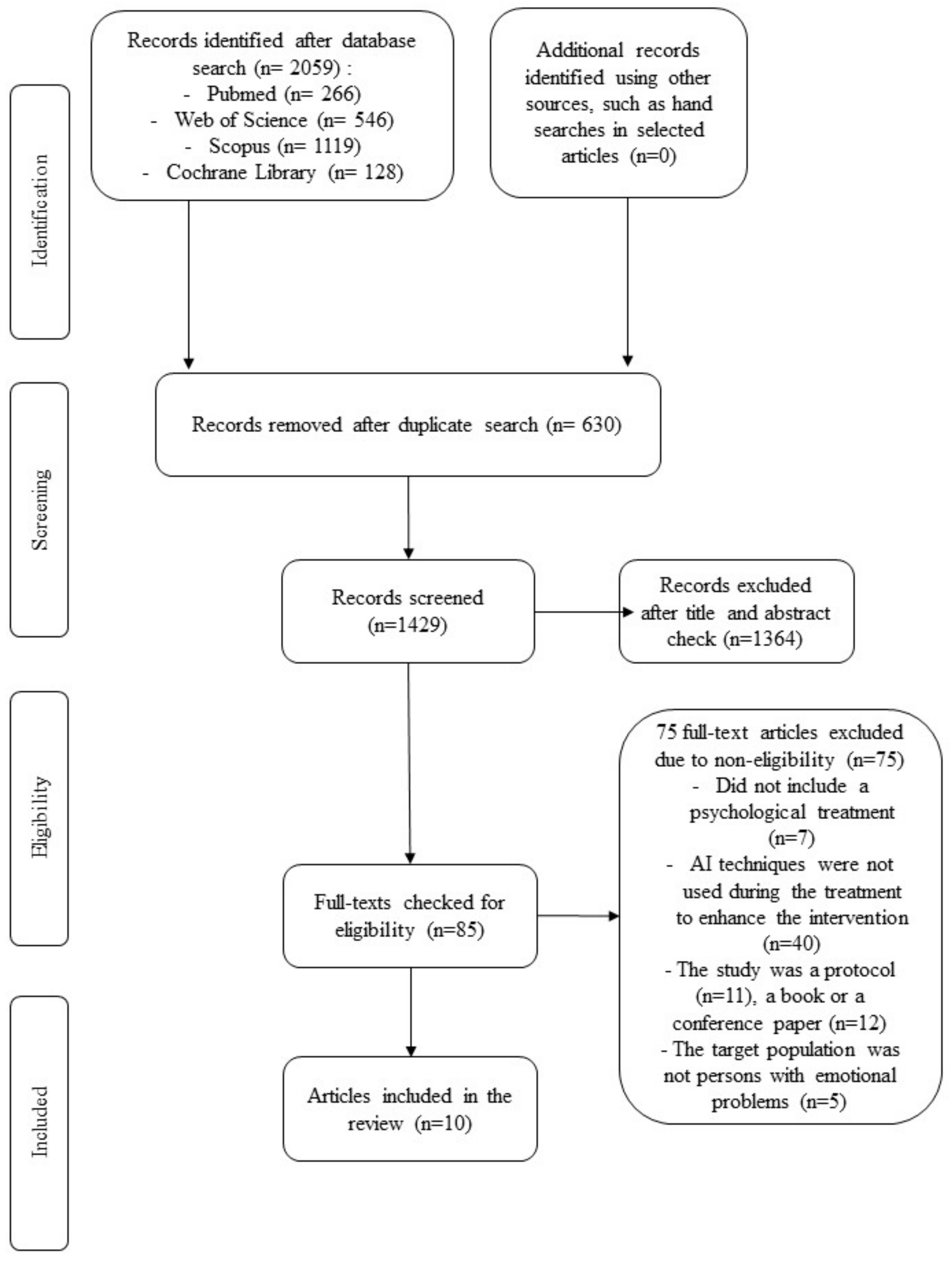
2.1. Identification and Selection of Studies
- An AI method is implemented.
- The target population is people with emotional problems. We included volunteers with daily stressors or emotional problems without a formal assessment of emotional disorder since we were interested in assessing changes in emotional symptomatology, regardless of the severity of the emotional problem. This was updated from the original PROSPERO registration since a number of studies using AI to enhance psychotherapy included this population that was originally ignored from our initial review plan.
- Psychological treatment is the main intervention.
- AI is implemented to improve an ongoing intervention.
- Data obtained with AI are not used to make changes in the treatment during therapy (e.g., predictors of treatment efficacy are evaluated at the end of an intervention for a group of individuals). This was not specifically stated in the original PROSPERO registration because of unintentional omission, but it represents an important exclusion criterion that was implicitly taken into account by the reviewers when selecting the included studies.
- The study is a protocol with no results available.
2.2. Search and Screening
2.3. Data Extraction
2.4. Risk of Bias Assessment
3. Results
3.1. Selection and Inclusion of Studies
3.2. Characteristics of Included Studies
3.2.1. Country Where the Study Was Conducted
3.2.2. Target Populations and Sample Sizes
3.2.3. Design and Treatment
3.2.4. Primary Outcomes
3.2.5. Characteristics of Artificial Intelligence procedures
3.2.6. Changes in Clinical Symptomatology
3.2.7. Engagement
3.2.8. Satisfaction with AI
3.2.9. Risk of Bias Assessment
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Bullis, J.R.; Boettcher, H.; Sauer-Zavala, S.; Barlow, D.H. What Is an Emotional Disorder? A Transdiagnostic Mechanistic Definition with Implications for Assessment, Treatment, and Prevention. Clin. Psychol. Sci. Pract. 2019, 26, e12278. [Google Scholar] [CrossRef]
- Baxter, A.J.; Scott, K.M.; Ferrari, A.; Norman, R.E.; Vos, T.; Whiteford, H. Challenging the myth of an “epidemic” of common mental disorders: Trends in the global prevalence of anxiety and depression between 1990 and 2010. Depress. Anxiety 2014, 31, 506–516. [Google Scholar] [CrossRef] [PubMed]
- Lim, G.Y.; Tam, W.W.; Lu, Y.; Ho, C.S.; Zhang, M.W.; Ho, R.C. Prevalence of Depression in the Community from 30 Countries between 1994 and 2014. Sci. Rep. 2018, 8, 2861. [Google Scholar] [CrossRef] [PubMed]
- Boyd, A.; Van de Velde, S.; Vilagut, G.; de Graaf, R.; O’Neill, S.; Florescu, S.; Alonso, J.; Kovess-Masfety, V. Gender Differences in Mental Disorders and Suicidality in Europe: Results from a Large Cross-Sectional Population-Based Study. J. Affect. Disord. 2015, 173, 245–254. [Google Scholar] [CrossRef]
- Wittchen, H.U.; Jacobi, F.; Rehm, J.; Gustavsson, A.; Svensson, M.; Jönsson, B.; Olesen, J.; Allgulander, C.; Alonso, J.; Faravelli, C.; et al. The Size and Burden of Mental Disorders and Other Disorders of the Brain in Europe 2010. Eur. Neuropsychopharmacol. 2011, 21, 655–679. [Google Scholar] [CrossRef] [Green Version]
- González-Blanch, C.; Umaran-Alfageme, O.; Cordero-Andrés, P.; Muñoz-Navarro, R.; Ruiz-Rodríguez, P.; Medrano, L.A.; Ruiz-Torres, M.; Dongil Collado, E.; Cano-Vindel, A. Tratamiento Psicológico de Los Trastornos Emocionales En Atención Primaria: El Manual de Tratamiento Transdiagnóstico Del Estudio PsicAP. Ansiedad Estrés 2018, 24, 1–11. [Google Scholar] [CrossRef]
- Goldberg, D.P.; Reed, G.M.; Robles, R.; Minhas, F.; Razzaque, B.; Fortes, S.; de Jesus Mari, J.; Lam, T.P.; Garcia, J.Á.; Gask, L.; et al. Screening for Anxiety, Depression, and Anxious Depression in Primary Care: A Field Study for ICD-11 PHC. J. Affect. Disord. 2017, 213, 199–206. [Google Scholar] [CrossRef] [Green Version]
- Vindel, A.C.; Salguero, J.M.; Wood, C.M.; Dongil, E.; Latorre, J.M.; Antonio, C.; Vindel, C. La Depresión En Atención Primaria: Prevalencia, Diagnóstico y Tratamiento. Pap. Psicólogo 2012, 33, 2–11. [Google Scholar]
- King, M.; Nazareth, I.; Levy, G.; Walker, C.; Morris, R.; Weich, S.; Bellón-Saameño, J.Á.; Moreno, B.; Švab, I.; Rotar, D.; et al. Prevalence of Common Mental Disorders in General Practice Attendees across Europe. Br. J. Psychiatry 2008, 192, 362–367. [Google Scholar] [CrossRef]
- Serrano-Blanco, A.; Palao, D.J.; Luciano, J.V.; Pinto-Meza, A.; Luján, L.; Fernández, A.; Roura, P.; Bertsch, J.; Mercader, M.; Haro, J.M. Prevalence of Mental Disorders in Primary Care: Results from the Diagnosis and Treatment of Mental Disorders in Primary Care Study (DASMAP). Soc. Psychiatry Psychiatr. Epidemiol. 2010, 45, 201–210. [Google Scholar] [CrossRef]
- World Health Assembly. Global Burden of Mental Disorders and the Need for a Comprehensive, Coordinated Response from Health and Social Sectors at the Country Level; Report by the Secretariat; World Health Organization: Geneva, Switzerland, 2012; Available online: https://apps.who.int/iris/handle/10665/78898 (accessed on 10 April 2022).
- Knapp, M.; Wong, G. Economics and Mental Health: The Current Scenario. World Psychiatry 2020, 19, 3–14. [Google Scholar] [CrossRef]
- Harvey, A.G.; Gumport, N.B. Evidence-Based Psychological Treatments for Mental Disorders: Modifiable Barriers to Access and Possible Solutions. Behav. Res. Ther. 2015, 68, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Wang, P.S.; Aguilar-Gaxiola, S.; Alonso, J.; Angermeyer, M.C.; Borges, G.; Bromet, E.J.; Bruffaerts, R.; de Girolamo, G.; de Graaf, R.; Gureje, O.; et al. Use of Mental Health Services for Anxiety, Mood, and Substance Disorders in 17 Countries in the WHO World Mental Health Surveys. Lancet 2007, 370, 841–850. [Google Scholar] [CrossRef] [Green Version]
- Samele, C.; Frew, S.; Urquía, N. Mental Health Systems in the European Union Member States, Status of Mental Health in Populations and Benefits to Be Expected from Investments into Mental Health; European Commission: Brussels, Belgium, 2013; Available online: https://ec.europa.eu/health/system/files/2016-11/europopp_full_en_0.pdf (accessed on 10 April 2022).
- Purebl, G.; Petrea, I.; Shields, L.; Tóth, M.D.; Székely, A.; Kurimay, T.; McDaid, D.; Arensman, E.; Granic, I.; Abello, K.M. Joint Action on Mental Health and Well-Being: Situation Analysis and Recommendations for Action; European Union: Brussels, Belgium, 2015; Available online: https://ec.europa.eu/health/system/files/2017-07/2017_depression_suicide_ehealth_en_0.pdf (accessed on 10 April 2022).
- Barbato, A.; Vallarino, M.; Rapisarda, F.; Lora, A.; Caldas de Almeida, J.M. Access to Mental Health Care in Europe. 2016. Available online: https://www.researchgate.net/publication/319329050_Access_to_Mental_Health_Care_in_Europe (accessed on 10 April 2022).
- Pikouli, Κ.; Konstantakopoulos, G.; Kalampaka Spilioti, P.; Fytrolaki, E.; Ploumpidis, D.; Economou, M. The Impact of the Recent Financial Crisis on the Users’ Profile of a Community Mental Health Unit. Psychiatriki 2019, 30, 97–107. [Google Scholar] [CrossRef]
- Wampold, B.E.; Budge, S.L.; Laska, K.M.; Del Re, A.C.; Baardseth, T.P.; Flűckiger, C.; Minami, T.; Kivlighan, D.M.; Gunn, W. Evidence-Based Treatments for Depression and Anxiety versus Treatment-as-Usual: A Meta-Analysis of Direct Comparisons. Clin. Psychol. Rev. 2011, 31, 1304–1312. [Google Scholar] [CrossRef]
- Bandelow, B.; Michaelis, S.; Wedekind, D. Treatment of Anxiety Disorders. Dialogues Clin. Neurosci. 2017, 19, 93–107. [Google Scholar] [CrossRef]
- American Psychological Association. Clinical Practice Guideline for the Treatment of Depression across Three Age Cohorts; American Psychological Association: Washington, DC, USA, 2019; Available online: https://www.apa.org/depression-guideline/guideline.pdf (accessed on 10 April 2022).
- Katzman, M.A.; Bleau, P.; Blier, P.; Chokka, P.; Kjernisted, K.; Van Ameringen, M.; Antony, M.M.; Bouchard, S.; Brunet, A.; Flament, M.; et al. Canadian Clinical Practice Guidelines for the Management of Anxiety, Posttraumatic Stress and Obsessive-Compulsive Disorders. BMC Psychiatry 2014, 14, S1. [Google Scholar] [CrossRef] [Green Version]
- Gautam, S.; Jain, A.; Gautam, M.; Vahia, V.; Grover, S. Clinical Practice Guidelines for the Management of Depression. Indian J. Psychiatry 2017, 59, S34–S50. [Google Scholar] [CrossRef]
- Sher, L. The Impact of the COVID-19 Pandemic on Suicide Rates. QJM 2020, 113, 707–712. [Google Scholar] [CrossRef]
- Moreno, C.; Wykes, T.; Galderisi, S.; Nordentoft, M.; Crossley, N.; Jones, N.; Cannon, M.; Correll, C.U.; Byrne, L.; Carr, S.; et al. How Mental Health Care Should Change as a Consequence of the COVID-19 Pandemic. Lancet Psychiatry 2020, 7, 813–824. [Google Scholar] [CrossRef]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of Stress, Anxiety, Depression among the General Population during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Global. Health 2020, 16, 57. [Google Scholar] [CrossRef]
- Ettman, C.K.; Abdalla, S.M.; Cohen, G.H.; Sampson, L.; Vivier, P.M.; Galea, S. Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Netw. Open 2020, 3, e2019686. [Google Scholar] [CrossRef]
- Fujiwara, D.; Dolan, P.; Lawton, R.; Behzadnejad, F.; Lagarde, A.; Maxwell, C.; Peytrignet, S. The Wellbeing Costs of COVID-19 in the UK; Report by Simetrica-Jacobs and the London School of Economics and Political Science. 2020. Available online: https://www.ceci.org.uk/wp-content/uploads/2020/05/jacobs-wellbeing-costs-of-covid-19-uk.pdf (accessed on 10 April 2022).
- McGinty, E.E.; Presskreischer, R.; Han, H.; Barry, C.L. Psychological Distress and Loneliness Reported by US Adults in 2018 and April 2020. JAMA 2020, 324, 93. [Google Scholar] [CrossRef]
- Lake, J.; Turner, M.S. Urgent Need for Improved Mental Health Care and a More Collaborative Model of Care. Perm. J. 2017, 21, 17–24. [Google Scholar] [CrossRef] [Green Version]
- Kazdin, A.E. Treatment as Usual and Routine Care in Research and Clinical Practice. Clin. Psychol. Rev. 2015, 42, 168–178. [Google Scholar] [CrossRef]
- Clark, D.M. Implementing NICE Guidelines for the Psychological Treatment of Depression and Anxiety Disorders: The IAPT Experience. Int. Rev. Psychiatry 2011, 23, 318–327. [Google Scholar] [CrossRef]
- Clark, D.M. Realizing the Mass Public Benefit of Evidence-Based Psychological Therapies: The IAPT Program. Annu. Rev. Clin. Psychol. 2018, 14, 159–183. [Google Scholar] [CrossRef] [Green Version]
- Mohr, D.C.; Weingardt, K.R.; Reddy, M.; Schueller, S.M. Three Problems with Current Digital Mental Health Research and Three Things We Can Do About Them. Psychiatr. Serv. 2017, 68, 427–429. [Google Scholar] [CrossRef]
- Miralles, I.; Granell, C.; Díaz-Sanahuja, L.; van Woensel, W.; Bretón-López, J.; Mira, A.; Castilla, D.; Casteleyn, S. Smartphone Apps for the Treatment of Mental Disorders: Systematic Review. JMIR mHealth uHealth 2020, 8, e14897. [Google Scholar] [CrossRef]
- Andersson, G. Internet-Delivered Psychological Treatments. Annu. Rev. Clin. Psychol. 2016, 12, 157–179. [Google Scholar] [CrossRef]
- Karyotaki, E.; Ebert, D.D.; Donkin, L.; Riper, H.; Twisk, J.; Burger, S.; Rozental, A.; Lange, A.; Williams, A.D.; Zarski, A.C.; et al. Do Guided Internet-Based Interventions Result in Clinically Relevant Changes for Patients with Depression? An Individual Participant Data Meta-Analysis. Clin. Psychol. Rev. 2018, 63, 80–92. [Google Scholar] [CrossRef] [PubMed]
- Andrews, G.; Basu, A.; Cuijpers, P.; Craske, M.G.; McEvoy, P.; English, C.L.; Newby, J.M. Computer Therapy for the Anxiety and Depression Disorders Is Effective, Acceptable and Practical Health Care: An Updated Meta-Analysis. J. Anxiety Disord. 2018, 55, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Carlbring, P.; Andersson, G.; Cuijpers, P.; Riper, H.; Hedman-Lagerlöf, E. Internet-Based vs. Face-to-Face Cognitive Behavior Therapy for Psychiatric and Somatic Disorders: An Updated Systematic Review and Meta-Analysis. Cogn. Behav. Ther. 2018, 47, 1–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Richards, D.; Enrique, A.; Eilert, N.; Franklin, M.; Palacios, J.; Duffy, D.; Earley, C.; Chapman, J.; Jell, G.; Sollesse, S.; et al. A Pragmatic Randomized Waitlist-Controlled Effectiveness and Cost-Effectiveness Trial of Digital Interventions for Depression and Anxiety. NPJ Digit. Med. 2020, 3, 85. [Google Scholar] [CrossRef]
- Massoudi, B.; Holvast, F.; Bockting, C.L.H.; Burger, H.; Blanker, M.H. The Effectiveness and Cost-Effectiveness of e-Health Interventions for Depression and Anxiety in Primary Care: A Systematic Review and Meta-Analysis. J. Affect. Disord. 2019, 245, 728–743. [Google Scholar] [CrossRef]
- Mehta, S.; Peynenburg, V.A.; Hadjistavropoulos, H.D. Internet-Delivered Cognitive Behaviour Therapy for Chronic Health Conditions: A Systematic Review and Meta-Analysis. J. Behav. Med. 2019, 42, 169–187. [Google Scholar] [CrossRef] [Green Version]
- Andrews, G.; Williams, A.D. Up-Scaling Clinician Assisted Internet Cognitive Behavioural Therapy (ICBT) for Depression: A Model for Dissemination into Primary Care. Clin. Psychol. Rev. 2015, 41, 40–48. [Google Scholar] [CrossRef]
- Andersson, G.; Carlbring, P.; Titov, N.; Lindefors, N. Internet Interventions for Adults with Anxiety and Mood Disorders: A Narrative Umbrella Review of Recent Meta-Analyses. Can. J. Psychiatry 2019, 64, 465–470. [Google Scholar] [CrossRef]
- Lambert, M.J. Psychotherapy Research and Its Achievements. In History of Psychotherapy: Continuity and Change, 2nd ed.; Norcross, J.C., VandenBos, G.R., Freedheim, D.K., Eds.; American Psychological Association: Washington, DC, USA, 2011; pp. 299–332. [Google Scholar]
- Barth, J.; Munder, T.; Gerger, H.; Nüesch, E.; Trelle, S.; Znoj, H.; Jüni, P.; Cuijpers, P. Comparative Efficacy of Seven Psychotherapeutic Interventions for Patients with Depression: A Network Meta-Analysis. PLoS Med. 2013, 10, e1001454. [Google Scholar] [CrossRef] [Green Version]
- Zhou, X.; Hetrick, S.E.; Cuijpers, P.; Qin, B.; Barth, J.; Whittington, C.J.; Cohen, D.; Del Giovane, C.; Liu, Y.; Michael, K.D.; et al. Comparative Efficacy and Acceptability of Psychotherapies for Depression in Children and Adolescents: A Systematic Review and Network Meta-Analysis. World Psychiatry 2015, 14, 207–222. [Google Scholar] [CrossRef] [Green Version]
- Kravitz, R.L.; Duan, N.; Niedzinski, E.J.; Hay, M.C.; Subramanian, S.K.; Weisner, T.S. What Ever Happened to N-of-1 Trials? Insiders’ Perspectives and a Look to the Future. Milbank Q. 2008, 86, 533–555. [Google Scholar] [CrossRef] [Green Version]
- Ebert, D.D.; Gollwitzer, M.; Riper, H.; Cuijpers, P.; Baumeister, H.; Berking, M. For Whom Does It Work? Moderators of Outcome on the Effect of a Transdiagnostic Internet-Based Maintenance Treatment After Inpatient Psychotherapy: Randomized Controlled Trial. J. Med. Internet Res. 2013, 15, e191. [Google Scholar] [CrossRef] [Green Version]
- Cuijpers, P.; Reijnders, M.; Huibers, M.J.H. The Role of Common Factors in Psychotherapy Outcomes. Annu. Rev. Clin. Psychol. 2019, 15, 207–231. [Google Scholar] [CrossRef] [Green Version]
- Evans, J.G. Evidence-Based and Evidence-Biased Medicine. Age Ageing 1995, 24, 461–463. [Google Scholar] [CrossRef]
- Fonagy, P. The Effectiveness of Psychodynamic Psychotherapies: An Update. World Psychiatry 2015, 14, 137–150. [Google Scholar] [CrossRef] [Green Version]
- Beutler, L.E.; Kimpara, S.; Edwards, C.J.; Miller, K.D. Fitting Psychotherapy to Patient Coping Style: A Meta-Analysis. J. Clin. Psychol. 2018, 74, 1980–1995. [Google Scholar] [CrossRef]
- Paul, G.L. Strategy of Outcome Research in Psychotherapy. J. Consult. Psychol. 1967, 31, 109–118. [Google Scholar] [CrossRef]
- Chorpita, B.F.; Rotheram-Borus, M.J.; Daleiden, E.L.; Bernstein, A.; Cromley, T.; Swendeman, D.; Regan, J. The Old Solutions Are the New Problem. Perspect. Psychol. Sci. 2011, 6, 493–497. [Google Scholar] [CrossRef]
- Păsărelu, C.R.; Andersson, G.; Bergman Nordgren, L.; Dobrean, A. Internet-Delivered Transdiagnostic and Tailored Cognitive Behavioral Therapy for Anxiety and Depression: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Cogn. Behav. Ther. 2017, 46, 1–28. [Google Scholar] [CrossRef]
- Gallo, K.P.; Barlow, D.H. Factors Involved in Clinician Adoption and Nonadoption of Evidence-based Interventions in Mental Health. Clin. Psychol. Sci. Pract. 2012, 19, 93–106. [Google Scholar] [CrossRef]
- Cook, S.C.; Schwartz, A.C.; Kaslow, N.J. Evidence-Based Psychotherapy: Advantages and Challenges. Neurotherapeutics 2017, 14, 537–545. [Google Scholar] [CrossRef] [Green Version]
- Myin-Germeys, I.; Klippel, A.; Steinhart, H.; Reininghaus, U. Ecological Momentary Interventions in Psychiatry. Curr. Opin. Psychiatry 2016, 29, 258–263. [Google Scholar] [CrossRef] [Green Version]
- Heron, K.E.; Smyth, J.M. Ecological Momentary Interventions: Incorporating Mobile Technology into Psychosocial and Health Behaviour Treatments. Br. J. Health Psychol. 2010, 15, 1–39. [Google Scholar] [CrossRef]
- Gee, B.L.; Griffiths, K.M.; Gulliver, A. Effectiveness of Mobile Technologies Delivering Ecological Momentary Interventions for Stress and Anxiety: A Systematic Review. J. Am. Med. Inform. Assoc. 2016, 23, 221–229. [Google Scholar] [CrossRef] [Green Version]
- Olff, M. Mobile Mental Health: A Challenging Research Agenda. Eur. J. Psychotraumatol. 2015, 6, 27882. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Price, M.; Yuen, E.K.; Goetter, E.M.; Herbert, J.D.; Forman, E.M.; Acierno, R.; Ruggiero, K.J. MHealth: A Mechanism to Deliver More Accessible, More Effective Mental Health Care. Clin. Psychol. Psychother. 2014, 21, 427–436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kazdin, A.E. Moderators, Mediators and Mechanisms of Change in Psychotherapy. In Quantitative and Qualitative Methods in Psychotherapy Research; Routledge: London, UK, 2014; pp. 87–101. [Google Scholar]
- Donker, T.; Batterham, P.J.; Warmerdam, L.; Bennett, K.; Bennett, A.; Cuijpers, P.; Griffiths, K.M.; Christensen, H. Predictors and Moderators of Response to Internet-Delivered Interpersonal Psychotherapy and Cognitive Behavior Therapy for Depression. J. Affect. Disord. 2013, 151, 343–351. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kazdin, A.E. Mediators and Mechanisms of Change in Psychotherapy Research. Annu. Rev. Clin. Psychol. 2007, 3, 1–27. [Google Scholar] [CrossRef] [Green Version]
- Luxton, D.D. Artificial Intelligence in Psychological Practice: Current and Future Applications and Implications. Prof. Psychol. Res. Pract. 2014, 45, 332–339. [Google Scholar] [CrossRef] [Green Version]
- Bach Xuan, T.; Giang Thu, V.; Giang Hai, H.; Quan-Hoang, V.; Manh-Tung, H.; Thu-Trang, V.; Viet-Phuong, L.; Manh-Toan, H.; Nghiem, K.-C.P.; Huong Lan Thi, N.; et al. Global Evolution of Research in Artificial Intelligence in Health and Medicine: A Bibliometric Study. J. Clin. Med. 2019, 8, 360. [Google Scholar] [CrossRef] [Green Version]
- De Mello, F.L.; de Souza, S.A. Psychotherapy and Artificial Intelligence: A Proposal for Alignment. Front. Psychol. 2019, 10, 263. [Google Scholar] [CrossRef] [Green Version]
- Horn, R.L.; Weisz, J.R. Can Artificial Intelligence Improve Psychotherapy Research and Practice? Adm. Policy Ment. Health Ment. Health Serv. Res. 2020, 47, 852–855. [Google Scholar] [CrossRef]
- Pintelas, E.G.; Kotsilieris, T.; Livieris, I.E.; Pintelas, P. A Review of Machine Learning Prediction Methods for Anxiety Disorders. In Proceedings of the 8th International Conference on Software Development and Technologies for Enhancing Accessibility and Fighting Info-Exclusion-DSAI 2018, Thessaloniki, Greece, 20–22 June 2018; Association for Computing Machinery (ACM): New York, NY, USA, 2018; pp. 8–15. [Google Scholar] [CrossRef]
- Aafjes-van Doorn, K.; Kamsteeg, C.; Bate, J.; Aafjes, M. A Scoping Review of Machine Learning in Psychotherapy Research. Psychother. Res. 2021, 31, 92–116. [Google Scholar] [CrossRef]
- Suso-Ribera, C.; Castilla, D.; Martínez-Borba, V.; Jaén, I.; Botella, C.; Baños, R.M.; García-Palacios, A. Technological Interventions for Pain Management. Ref. Modul. Neurosci. Biobehav. Psychol. 2022, 1–20. [Google Scholar] [CrossRef]
- Legler, S.; Celano, C.M.; Amador, A.; Novis, A.; Ebrahim, S.; Huffman, J.C. Development and Theoretical Approach to an Adaptive Text Message Program to Promote Well-Being and Health Behaviors in Primary Care Patients. Prim. Care Companion CNS Disord. 2018, 20, 18br02353. [Google Scholar] [CrossRef]
- Kelly, J.; Gooding, P.; Pratt, D.; Ainsworth, J.; Welford, M.; Tarrier, N. Intelligent Real-Time Therapy: Harnessing the Power of Machine Learning to Optimise the Delivery of Momentary Cognitivebehavioural Interventions. J. Ment. Health 2012, 21, 404–414. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Altman, D.G.; Antes, G.; Atkins, D.; Barbour, V.; Barrowman, N.; Berlin, J.A.; et al. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement (Chinese Edition). J. Chin. Integr. Med. 2009, 7, 889–896. [Google Scholar] [CrossRef]
- Burns, M.N.; Begale, M.; Duffecy, J.; Gergle, D.; Karr, C.J.; Giangrande, E.; Mohr, D.C. Harnessing Context Sensing to Develop a Mobile Intervention for Depression. J. Med. Internet Res. 2011, 13, e55. [Google Scholar] [CrossRef] [Green Version]
- Fulmer, R.; Joerin, A.; Gentile, B.; Lakerink, L.; Rauws, M. Using Psychological Artificial Intelligence (Tess) to Relieve Symptoms of Depression and Anxiety: Randomized Controlled Trial. JMIR Ment. Health 2018, 5, e64. [Google Scholar] [CrossRef]
- Paredes, P.; Berkeley, U.C.; Gilad-bachrach, R.; Czerwinski, M.; Roseway, A.; Hernandez, J. PopTherapy: Coping with Stress through Pop-Culture. In Proceedings of the 8th International Conference on Pervasive Computing Technologies for Healthcare, Oldenburg, Germany, 20 May 2014; pp. 109–117. [Google Scholar] [CrossRef] [Green Version]
- Bird, T.; Mansell, W.; Wright, J.; Gaffney, H.; Tai, S. Manage Your Life Online: A Web-Based Randomized Controlled Trial Evaluating the Effectiveness of a Problem-Solving Intervention in a Student Sample. Behav. Cogn. Psychother. 2018, 46, 570–582. [Google Scholar] [CrossRef] [Green Version]
- Inkster, B.; Sarda, S.; Subramanian, V. An Empathy-Driven, Conversational Artificial Intelligence Agent (Wysa) for Digital Mental Well-Being: Real-World Data Evaluation Mixed-Methods Study. JMIR mHealth uHealth 2018, 6, e12106. [Google Scholar] [CrossRef] [Green Version]
- Lutz, W.; Rubel, J.A.; Schwartz, B.; Schilling, V.; Deisenhofer, A.K. Towards Integrating Personalized Feedback Research into Clinical Practice: Development of the Trier Treatment Navigator (TTN). Behav. Res. Ther. 2019, 120, 103438. [Google Scholar] [CrossRef]
- Wahle, F.; Kowatsch, T.; Fleisch, E.; Rufer, M.; Weidt, S. Mobile Sensing and Support for People with Depression: A Pilot Trial in the Wild. JMIR mHealth uHealth 2016, 4, e111. [Google Scholar] [CrossRef] [Green Version]
- Cho, C.H.; Lee, T.; Lee, J.B.; Seo, J.Y.; Jee, H.J.; Son, S.; An, H.; Kim, L.; Lee, H.J. Effectiveness of a Smartphone App with a Wearable Activity Tracker in Preventing the Recurrence of Mood Disorders: Prospective Case-Control Study. JMIR Ment. Health 2020, 7, e21283. [Google Scholar] [CrossRef]
- Green, E.P.; Lai, Y.; Pearson, N.; Rajasekharan, S.; Rauws, M.; Joerin, A.; Kwobah, E.; Musyimi, C.; Jones, R.M.; Bhat, C.; et al. Expanding Access to Perinatal Depression Treatment in Kenya through Automated Psychological Support: Development and Usability Study. JMIR Form. Res. 2020, 4, e17895. [Google Scholar] [CrossRef]
- Liu, H.; Peng, H.; Song, X.; Xu, C.; Zhang, M. Using AI Chatbots to Provide Self-Help Depression Interventions for University Students: A Randomized Trial of Effectiveness. Internet Interv. 2022, 27, 100495. [Google Scholar] [CrossRef]
- Taubitz, F.-S.; Büdenbender, B.; Alpers, G.W. What the Future Holds: Machine Learning to Predict Success in Psychotherapy. Behav. Res. Ther. 2022, 104116. Available online: https://www.sciencedirect.com/science/article/pii/S0005796722000870 (accessed on 10 April 2022). [CrossRef]
- Russell, S.; Norvig, P. Artificial Intelligence: A Modern Approach, 3rd ed.; Prentice Hall: Saddle River, NJ, USA, 2009. [Google Scholar]
- Miner, A.S.; Shah, N.; Bullock, K.D.; Arnow, B.A.; Bailenson, J.; Hancock, J. Key Considerations for Incorporating Conversational AI in Psychotherapy. Front. Psychiatry 2019, 10, 746. [Google Scholar] [CrossRef] [Green Version]
- Sedlakova, J.; Trachsel, M. Conversational Artificial Intelligence in Psychotherapy: A New Therapeutic Tool or Agent? Am. J. Bioeth. 2022, 1–10. [Google Scholar] [CrossRef]
| References | Country | Sample Size | Study Design | Emotional Problem Evaluated | Psychological Intervention | Main Outcome | Type of AI Used |
|---|---|---|---|---|---|---|---|
| [77] | USA | 8 Tx | Pre-post study (no control) | MDD | Multimodal intervention (behavioral activation approach) | MINI, QIDS-C, PHQ-9, GAD-7 | The nearest neighbor Suppport Vector Machines and Random Forest Classifier |
| [78] | USA | 74 (24 cont. + 2-week 24 Tx + 4-week 26 Tx) | Parallel group RCT (1:1) | College students with daily stressors | CBT and other interventions | PHQ-9, GAD-7, and PANAS | AI chatbot: conversational Tess app |
| [79] | USA | 95 Tx (22 no selection-random intervention; 21 no selection-AI intervention; 26 selection-random; 26 selection-AI) | Controlled trial | Stress | Stress management micro-interventions (positive psychology, cognitive behavioral, meta-cognitive, and somatic) via app | PHQ-9 and CSQ | Reinforcement Learning algorithm |
| [80] | UK | 171 (85 Tx MYLO program + 86 cont. ELIZA program) | RCT | Volunteers with daily stressors | Web-based problem-solving intervention | Problem-related distress | AI chatbot; Manage Your Life Online (MYLO) |
| [81] | UK | 129 Tx | Quasi-experimental pre-post study | Self-report symptoms of MDD (nonclinical global population) | CBT together with other interventions via Wysa app | PHQ-9 | AI-chatbot: conversational Wysa app |
| [82] | Germany | 1234 Tx | Pre-post study (no control) | Affective and anxiety disorders (70%), and other disorders (30%) | CBT via Trier Treatment Navigator | OQ-30, ASC, ASQ, HSCL-11 | Random Forest Algorithm. |
| [83] | Switzerland | 126 Tx | Pre-post pilot study | Depressive symptoms | CBT intervention + MOSS app | PHQ-9 | LASSO (least absolute shrinkage and selection operator) |
| [84] | Korea | 43 Tx (10 CRM group + 33 non-CRM) | Prospective Case-control study | MDD, BD I and BD II | Feedback intervention of Behavioral guidance | Daily mood state on eMoodChart, mood episodes, circadian rhythm | Circadian rhythm-based algorithm based on data obtained with a wearable activity tracker |
| [85] | Kenya | 41 Tx (pregnant women and new mothers) | Nonconcurrent Multiple baseline SG | Non-clinical Perinatal Depression | CBT (Healthy Moms adaptation) | PHQ-9, feelings, and mood | AI chatbot: conversational Zuri app, Kenyan version of Tess |
| [86] | China | 83 university students (42 cont. + 41 Tx) | RCT (unblinded) | Depression | CBT intervention | PHQ-9, GAD-7, and PANAS | AI chatbot: conversational XioNan app) |
| References | Results |
|---|---|
| [77] | Clinical symptoms:
|
| [78] | Clinical symptoms:
|
| [79] | Clinical symptoms:
|
| [80] | Clinical symptoms:
|
| [81] | Clinical symptoms:
|
| [82] | Clinical symptoms:
|
| [83] | Clinical symptoms:
|
| [84] | Clinical symptoms:
|
| [85] | Clinical symptoms:
|
| [86] | Clinical symptoms:
|
| [77] | [81] | [82] | [83] | |
|---|---|---|---|---|
| 1. Was the study question or objective clearly stated? | Yes | Yes | Yes | Yes |
| 2. Were eligibility/selection criteria for the study population prespecified and clearly described? | Yes | Yes | Yes | Yes |
| 3. Were the participants in the study representative of those who would be eligible for the test/service/intervention in the general or clinical population of interest? | Yes | Yes | Yes | Yes |
| 4. Were all eligible participants that met the prespecified entry criteria enrolled? | No | Yes | Yes | Yes |
| 5. Was the sample size sufficiently large to provide confidence in the findings? | NR | Yes | Yes | NR |
| 6. Was the test/service/intervention clearly described and delivered consistently across the study population? | Yes | Yes | No | Yes |
| 7. Were the outcome measures prespecified, clearly defined, valid, reliable, and assessed consistently across all study participants? | Yes | Yes | Yes | Yes |
| 8. Were the people assessing the outcomes blinded to the participants’ exposures/interventions? | NA | Yes | NA | NA |
| 9. Was the loss to follow-up after baseline 20% or less? Were those lost to follow-up accounted for in the analysis? | Yes | Yes | No/Yes | No/No |
| 10. Did the statistical methods examine changes in outcome measures from before to after the intervention? Were statistical tests done that provided p values for the pre-to-post changes? | Yes | Yes | Yes | Yes |
| 11. Were outcome measures of interest taken multiple times before the intervention and multiple times after the intervention (i.e., did they use an interrupted time-series design)? | Yes | No | Yes | Yes |
| 12. If the intervention was conducted at a group level (e.g., a whole hospital, a community, etc.) did the statistical analysis consider the use of individual-level data to determine effects at the group level? | NA | NA | NA | NA |
| Total score (maximum 12 points) | 8 | 10 | 9 | 8 |
| [85] | |
|---|---|
| 1. Was the study question or objective clearly stated? | Yes |
| 2. Was the study population clearly and fully described, including a case definition? | Yes |
| 3. Were the cases consecutive? | Yes |
| 4. Were the subjects comparable? | Yes |
| 5. Was the intervention clearly described? | Yes |
| 6. Were the outcome measures clearly defined, valid, reliable, and implemented consistently across all study participants? | Yes |
| 7. Was the length of follow-up adequate? | NA |
| 8. Were the statistical methods well-described? | Yes |
| 9. Were the results well-described? | Yes |
| Total score (maximum 9 points) | 8 |
| [84] | |
|---|---|
| 1. Was the research question or objective in this paper clearly stated and appropriate? | Yes |
| 2. Was the study population clearly specified and defined? | Yes |
| 3. Did the authors include a sample size justification? | No |
| 4. Were controls selected or recruited from the same or similar population that gave rise to the cases (including the same timeframe)? | Yes |
| 5. Were the definitions, inclusion and exclusion criteria, algorithms or processes used to identify or select cases and controls valid, reliable, and implemented consistently across all study participants? | CD |
| 6. Were the cases clearly defined and differentiated from controls? | Yes |
| 7. If less than 100 percent of eligible cases and/or controls were selected for the study, were the cases and/or controls randomly selected from those eligible? | NR |
| 8. Was there use of concurrent controls? | No |
| 9. Were the investigators able to confirm that the exposure/risk occurred prior to the development of the condition or event that defined a participant as a case? | Yes |
| 10. Were the measures of exposure/risk clearly defined, valid, reliable, and implemented consistently (including the same time period) across all study participants? | Yes |
| 11. Were the assessors of exposure/risk blinded to the case or control status of participants? | No |
| 12. Were key potential confounding variables measured and adjusted statistically in the analyses? If matching was used, did the investigators account for matching during study analysis? | Yes |
| Total score (maximum 12 points) | 7 |
| [79] | [80] | [78] | [86] | |
|---|---|---|---|---|
| 1. Was the study described as randomized, a randomized trial, a randomized clinical trial, or an RCT? | No | Yes | Yes | Yes |
| 2. Was the method of randomization adequate (i.e., use of randomly generated assignment)? | NR | Yes | Yes | Yes |
| 3. Was the treatment allocation concealed (so that assignments could not be predicted)? | NR | Yes | Yes | Yes |
| 4. Were study participants and providers blinded to treatment group assignment? | NR | NR | Yes | No |
| 5. Were the people assessing the outcomes blinded to the participants’ group assignments? | Yes | Yes | Yes | No |
| 6. Were the groups similar at baseline on important characteristics that could affect outcomes (e.g., demographics, risk factors, or co-morbid conditions)? | NR | No | Yes | Yes |
| 7. Was the overall drop-out rate from the study at endpoint 20% or lower of the number allocated to treatment? | NR | No | Yes | No |
| 8. Was the differential drop-out rate (between treatment groups) at endpoint 15 percentage points or lower? | NR | Yes | Yes | Yes |
| 9. Was there high adherence to the intervention protocols for each treatment group? | NR | Yes | Yes | Yes |
| 10. Were other interventions avoided or similar in the groups (e.g., similar background treatments)? | NR | NR | Yes | Yes |
| 11. Were outcomes assessed using valid and reliable measures, implemented consistently across all study participants? | Yes | No | Yes | Yes |
| 12. Did the authors report that the sample size was sufficiently large to be able to detect a difference in the main outcome between groups with at least 80% power? | No | Yes | Yes | Yes |
| 13. Were outcomes reported or subgroups analyzed prespecified (i.e., identified before analyses were conducted)? | No | Yes | Yes | Yes |
| 14. Were all randomized participants analyzed in the group to which they were originally assigned, i.e., did they use an intention-to-treat analysis? | NR | No | Yes | Yes |
| Total score (maximum 14 points) | 2 | 8 | 14 | 9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gual-Montolio, P.; Jaén, I.; Martínez-Borba, V.; Castilla, D.; Suso-Ribera, C. Using Artificial Intelligence to Enhance Ongoing Psychological Interventions for Emotional Problems in Real- or Close to Real-Time: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 7737. https://doi.org/10.3390/ijerph19137737
Gual-Montolio P, Jaén I, Martínez-Borba V, Castilla D, Suso-Ribera C. Using Artificial Intelligence to Enhance Ongoing Psychological Interventions for Emotional Problems in Real- or Close to Real-Time: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(13):7737. https://doi.org/10.3390/ijerph19137737
Chicago/Turabian StyleGual-Montolio, Patricia, Irene Jaén, Verónica Martínez-Borba, Diana Castilla, and Carlos Suso-Ribera. 2022. "Using Artificial Intelligence to Enhance Ongoing Psychological Interventions for Emotional Problems in Real- or Close to Real-Time: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 13: 7737. https://doi.org/10.3390/ijerph19137737








