Explore How Online Healthcare Can Influence Willingness to Seek Offline Care
Abstract
:1. Introduction
2. Theoretical Background and Research Basis
2.1. Internet Healthcare Industry
2.2. Online Healthcare Platform Usage Behaviour
2.3. Online to Offline
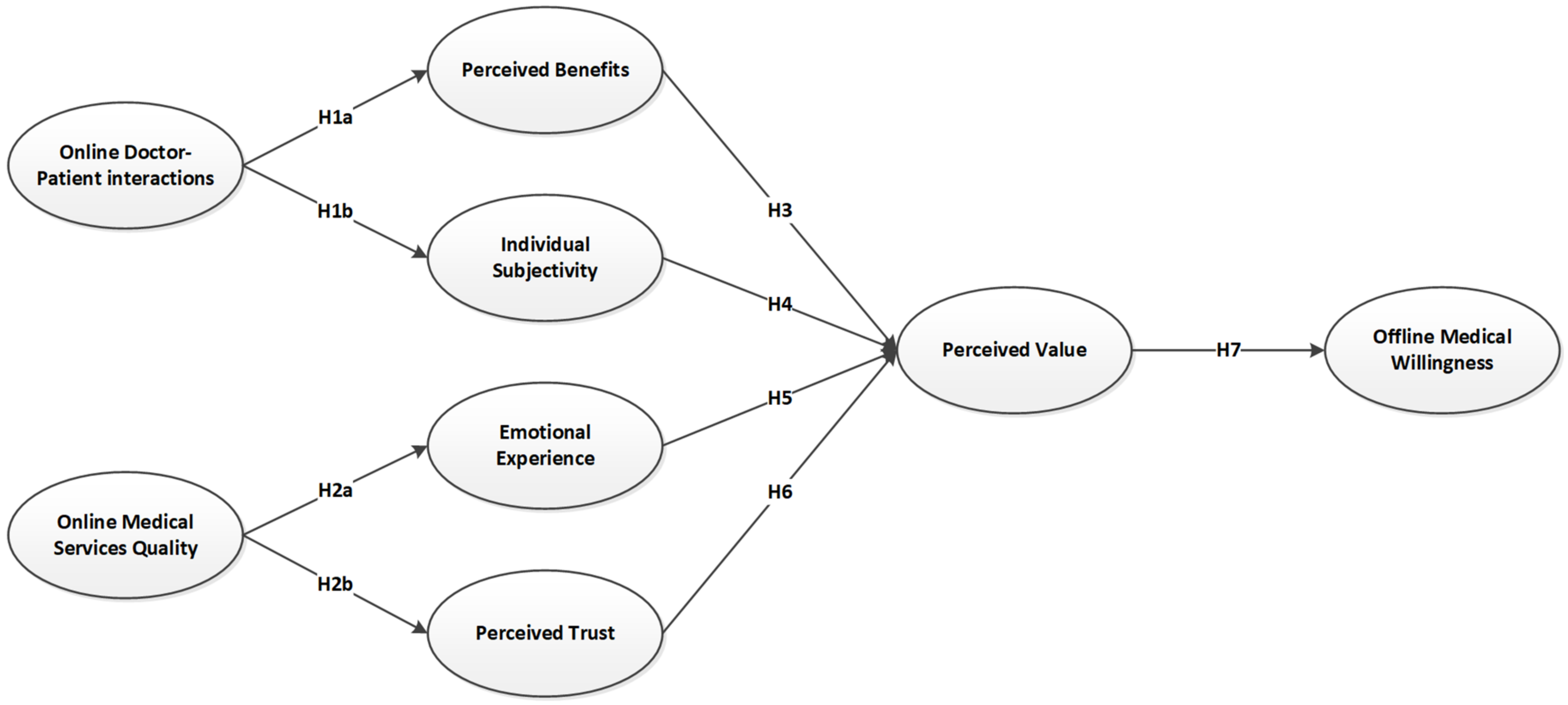
3. Research Model and Hypothesis
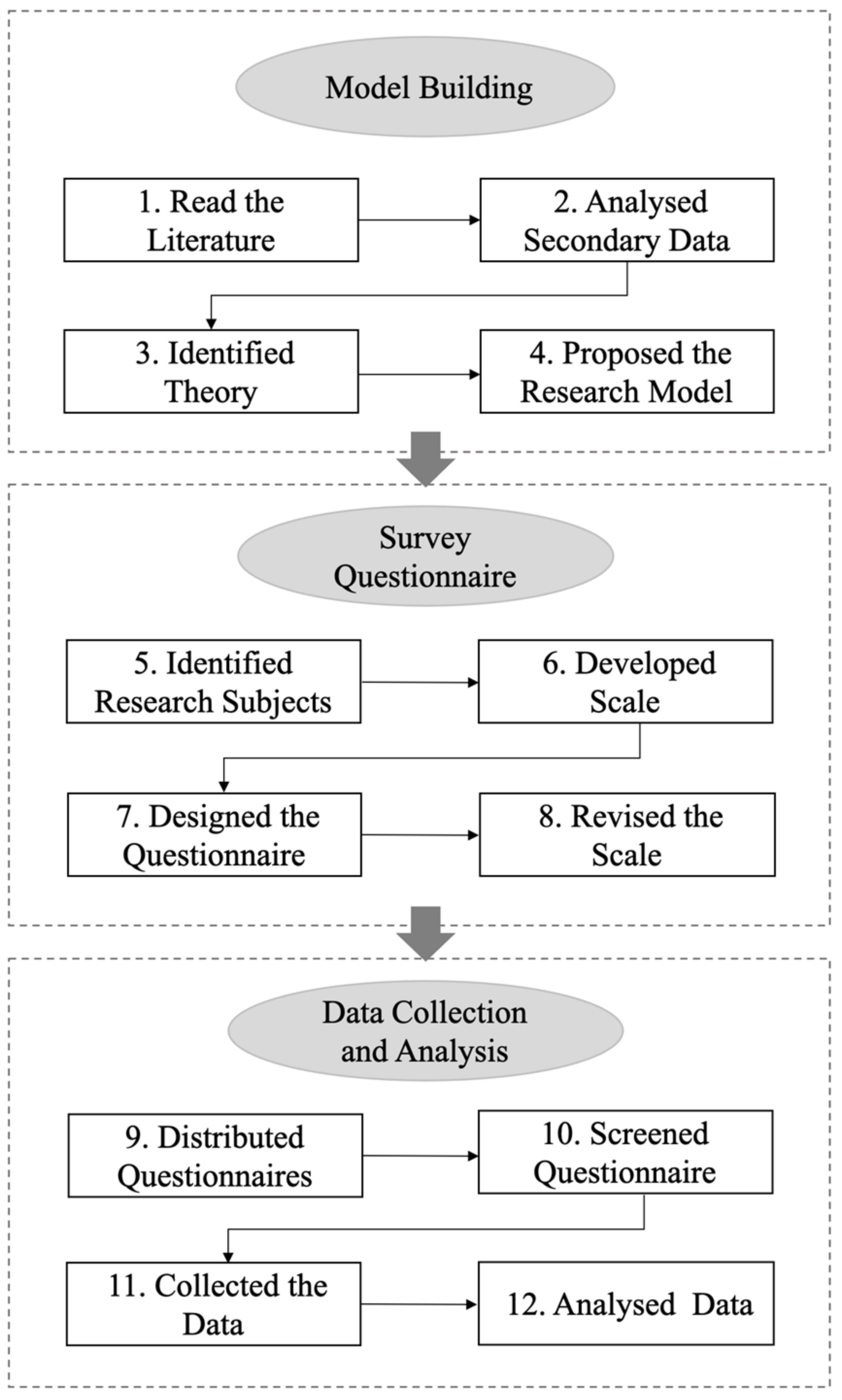
4. Methodology
4.1. Sample
4.2. Measures
4.3. Data Analysis
5. Results
5.1. Measurement Model
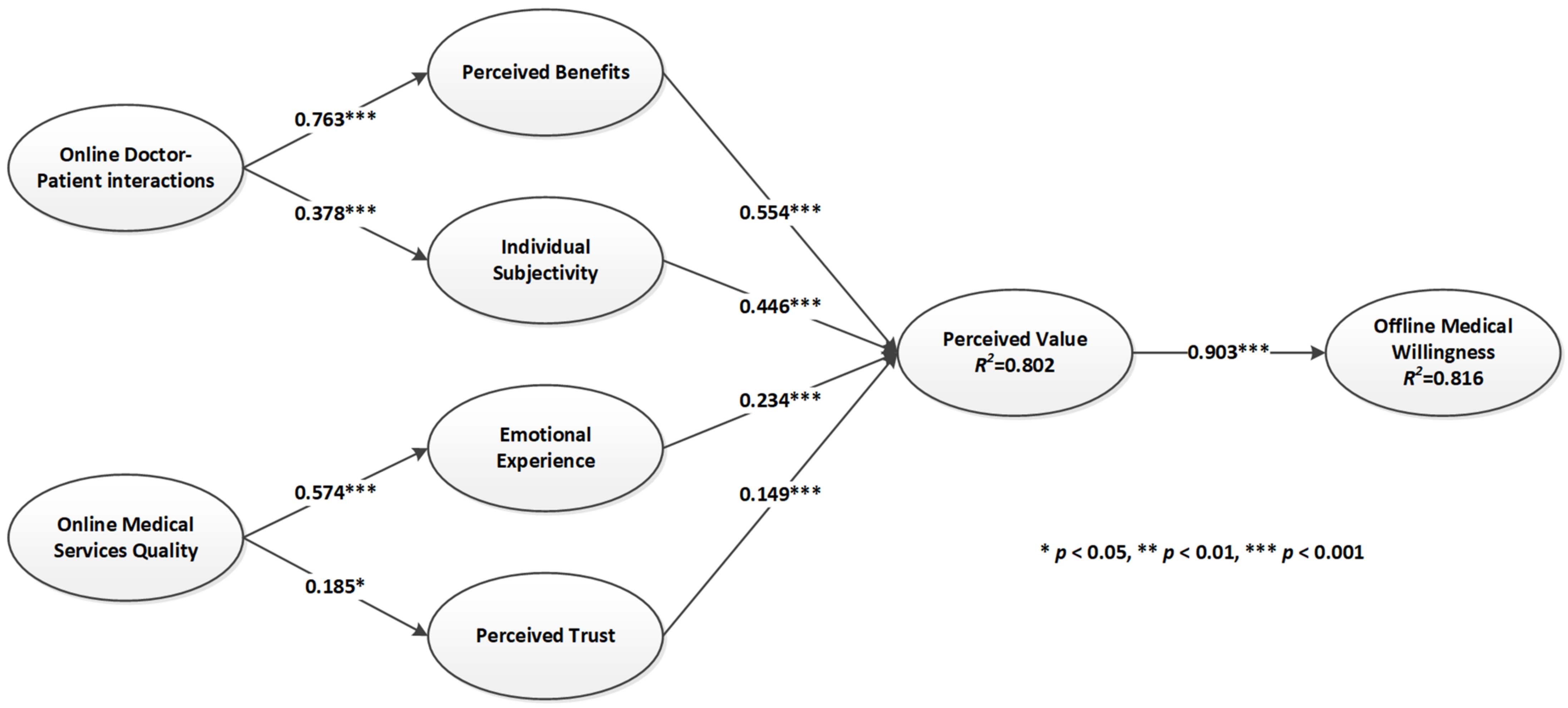
5.2. Structural Model
5.3. Assessing Global Model Fit
6. Discussion
7. Limitations and Future Research
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Ethical Review
Appendix B. Measurement Items
| Factors | Definition | No. of Items | Items | Source |
|---|---|---|---|---|
| Offline Medical Willingness | The willingness and behavior of patients to make offline hospital and doctor choices following information obtained from online healthcare platforms. | 2 | 1. I am likely to visit a doctor in hospital in the future. 2. I have the desire to visit a doctor in hospital in the future. | [60] |
| Perceived Value | The individual’ s overall evaluation of perceived benefits and cost effectiveness in obtaining products or services. | 2 | 1. Online healthcare platforms can make my life easier. 2. Online healthcare platforms can solve my disease consultation problems. | [43] |
| Perceived Benefits | The sum of the material and spiritual benefits felt by the customer in the transaction or through consumption. | 3 | 1. The information obtained from online healthcare was in line with my expectations. 2. The online doctor was trustworthy. 3. Using the internet to consult on this platform is a good idea. | [51,58] |
| Individual Subjectivity | Active engagement behavior of patients during online consultations | 3 | 1. I will proactively ask questions to doctors on healthcare platforms. 2. I will ask the doctor to explain the procedure to me in detail. 3. I take the lead in communication with the doctor. | [47] |
| Emotional Experience | The emotions of pleasure and delight experienced when consumers use a service. | 3 | 1. I feel good when I use online healthcare platform. 2. Online healthcare platform gives me pleasure. 3. Using online healthcare platform is enjoyable. | [48] |
| Perceived Trust | Users’ trust in the security of the online platform and in the reliability of the services provided by online doctors. | 3 | 1. This online healthcare platform is trustworthy. 2. The online doctor’s services met my expectations. 3. I trust this online healthcare platform keeps my best interests in mind. | [51] |
| Online Doctor-Patient Interaction | Online communication between doctors and patients, including proactive disclosure and feedback of information. | 3 | 1. I will disclose private information about my condition to my doctor. 2. The doctor can provide me with valuable information. 3. My communication with the doctor was smooth. | [57] |
| Online Medical Service Quality | Patients’ evaluation of the design and safety of the online platform and whether the information provided meets the patient’s expectations. | 3 | 1. The online doctor was very quick to reply to me. 2. The online doctor is highly qualified. 3. Online healthcare platform is easy to operate. | [59] |
References
- McMullan, M. Patients using the Internet to obtain health information: How this affects the patient–health professional relationship. Patient Educ. Couns. 2006, 63, 24–28. [Google Scholar] [CrossRef]
- Cocosila, M.; Archer, N. Adoption of mobile ICT for health promotion: An empirical investigation. Electron. Mark. 2010, 20, 241–250. [Google Scholar] [CrossRef]
- Yi, M.Y.; Yoon, J.J.; Davis, J.M.; Lee, T. Untangling the antecedents of initial trust in Web-based health information: The roles of argument quality, source expertise, and user perceptions of information quality and risk. Decis. Support Syst. 2013, 55, 284–295. [Google Scholar] [CrossRef]
- Huang, N.; Yan, Z.; Yin, H. Effects of Online–Offline Service Integration on e-Healthcare Providers: A Quasi-Natural Experiment. Prod. Oper. Manag. 2021, 30, 2359–2378. [Google Scholar] [CrossRef]
- Takao, H.; Murayama, Y.; Ishibashi, T.; Karagiozov, K.L.; Abe, T. A New Support System Using a Mobile Device (Smartphone) for Diagnostic Image Display and Treatment of Stroke. Stroke 2012, 43, 236–239. [Google Scholar] [CrossRef] [Green Version]
- Berndt, R.D.; Takenga, M.C.; Kuehn, S.; Preik, P.; Dubbermann, D.; Juenger, M. Development of a Mobile Teledermatology System. Telemed. E-Health 2012, 18, 668–673. [Google Scholar] [CrossRef]
- Kim, D.-K.; Yoo, S.K.; Park, I.-C.; Choa, M.; Bae, K.Y.; Kim, Y.-D.; Heo, J.-H. A mobile telemedicine system for remote consultation in cases of acute stroke. J. Telemed. Telecare 2009, 15, 102–107. [Google Scholar] [CrossRef]
- Figueredo, M.V.M.; Dias, J.S. Mobile Telemedicine System for Home Care and Patient Monitoring. In Proceedings of the 26th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Francisco, CA, USA, 1–5 September 2004; pp. 3387–3390. [Google Scholar]
- Arnhold, M.; Quade, M.; Kirch, W. Mobile Applications for Diabetics: A Systematic Review and Expert-Based Usability Evaluation Considering the Special Requirements of Diabetes Patients Age 50 Years or Older. J. Med. Internet Res. 2014, 16, 34–51. [Google Scholar] [CrossRef] [Green Version]
- Con, D.; De Cruz, P. Mobile Phone Apps for Inflammatory Bowel Disease Self-Management: A Systematic Assessment of Content and Tools. JMIR mHealth uHealth 2016, 4, 312–328. [Google Scholar] [CrossRef]
- Eysenbach, G. Medicine 2.0: Social Networking, Collaboration, Participation, Apomediation, and Openness. J. Med. Internet Res. 2008, 10, 10. [Google Scholar] [CrossRef]
- Goh, J.M.; Gao, G.D.; Agarwal, R. Evolving Work Routines: Adaptive Routinization of Information Technology in Healthcare. Inf. Syst. Res. 2011, 22, 565–585. [Google Scholar] [CrossRef]
- Das, A.; Faxvaag, A.; Svanaes, D. The Impact of an eHealth Portal on Health Care Professionals’ Interaction with Patients: Qualitative Study. J. Med. Internet Res. 2015, 17, 12. [Google Scholar] [CrossRef] [Green Version]
- Roettl, J.; Bidmon, S.; Terlutter, R. What Predicts Patients’ Willingness to Undergo Online Treatment and Pay for Online Treatment? Results from a Web-Based Survey to Investigate the Changing Patient-Physician Relationship. J. Med. Internet Res. 2016, 18, 15. [Google Scholar] [CrossRef]
- Raghupathi, W.; Raghupathi, V. Big data analytics in healthcare: Promise and potential. Health Inf. Sci. Syst. 2014, 2, 3. [Google Scholar] [CrossRef]
- Munoz, R.F. Using Evidence-Based Internet Interventions to Reduce Health Disparities Worldwide. J. Med. Internet Res. 2010, 12, 9. [Google Scholar] [CrossRef]
- Goh, J.M.; Gao, G.D.; Agarwal, R. The creation of social value: Can an online health community reduce rural-urban health disparities? MIS Q. 2016, 40, 247–263. [Google Scholar] [CrossRef] [Green Version]
- Hewitt-Taylor, J.; Bond, C.S. What E-patients Want From the Doctor-Patient Relationship: Content Analysis of Posts on Discussion Boards. J. Med. Internet Res. 2012, 14, 301–309. [Google Scholar] [CrossRef] [Green Version]
- Detz, A.; Lopez, A.; Sarkar, U. Long-Term Doctor-Patient Relationships: Patient Perspective From Online Reviews. J. Med. Internet Res. 2013, 15, 157–166. [Google Scholar] [CrossRef]
- Neslin, S.A.; Grewal, D.; Leghorn, R.; Shankar, V.; Teerling, M.L.; Thomas, J.S.; Verhoef, P.C. Challenges and opportunities in multichannel customer management. J. Serv. Res. 2006, 9, 95–112. [Google Scholar] [CrossRef]
- Falk, T.; Schepers, J.; Hammerschmidt, M.; Bauer, H.H. Identifying cross-channel dissynergies for multichannel service providers. J. Serv. Res. 2007, 10, 143–160. [Google Scholar] [CrossRef] [Green Version]
- Yang, S.Q.; Lu, Y.B.; Zhao, L.; Gupta, S. Empirical investigation of customers’ channel extension behavior: Perceptions shift toward the online channel. Comput. Hum. Behav. 2011, 27, 1688–1696. [Google Scholar] [CrossRef]
- Wu, H.; Lu, N.J. Online written consultation, telephone consultation and offline appointment: An examination of the channel effect in online health communities. Int. J. Med. Inform. 2017, 107, 107–119. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.C.; Kang, I.; McKnight, D.H. Transfer from offline trust to key Online perceptions: An empirical study. IEEE Trans. Eng. Manag. 2007, 54, 729–741. [Google Scholar] [CrossRef]
- Lu, W.; Wu, H. How Online Reviews and Services Affect Physician Outpatient Visits: Content Analysis of Evidence From Two Online Health Care Communities. JMIR Med. Inform. 2019, 7, 373–394. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.F.; Ma, X.M.; Song, J.J.; Yang, Y.B.; Ju, X.F. Exploring the Effects of Online Rating and the Activeness of Physicians on the Number of Patients in an Online Health Community. Telemed. E-Health 2019, 25, 1090–1098. [Google Scholar] [CrossRef]
- Yang, H.L.; Guo, X.T.; Wu, T.S.; Ju, X.F. Exploring the effects of patient-generated and system-generated information on patients’ online search, evaluation and decision. Electron. Commer. Res. Appl. 2015, 14, 192–203. [Google Scholar] [CrossRef]
- Kim, H.W.; Chan, H.C.; Gupta, S. Value-based adoption of mobile internet: An empirical investigation. Decis. Support Syst. 2007, 43, 111–126. [Google Scholar] [CrossRef]
- Davis, F.D. Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef] [Green Version]
- Mehrabian, A.; Russell, J.A. An Approach to Environmental Psychology; The MIT Press: Cambridge, MA, USA, 1974; pp. xii, 266. [Google Scholar]
- Reingen, P.H.; Foster, B.L.; Brown, J.J.; Seidman, S.B. Brand Congruence in Interpersonal Relations: A Social Network Analysis. J. Consum. Res. 1984, 11, 771–783. [Google Scholar] [CrossRef]
- Umar, N.; Litaker, D.; Schaarschmidt, M.L.; Peitsch, W.K.; Schmieder, A.; Terris, D.D. Outcomes associated with matching patients’ treatment preferences to physicians’ recommendations: Study methodology. BMC Health Serv. Res. 2012, 12, 10. [Google Scholar] [CrossRef] [Green Version]
- Dunn, K. A qualitative investigation into the online counselling relationship: To meet or not to meet, that is the question. Couns. Psychother. Res. 2012, 12, 316–326. [Google Scholar] [CrossRef]
- May, C. The Clinical Encounter and the Problem of Context. Sociology 2007, 41, 29–45. [Google Scholar] [CrossRef]
- Murray, E.; Lo, B.; Pollack, L.; Donelan, K.; Catania, J.; White, M.; Zapert, K.; Turner, R. The impact of health in formation on the Internet on the physician-patient relationship—Patient perceptions. Arch. Intern. Med. 2003, 163, 1727–1734. [Google Scholar] [CrossRef] [Green Version]
- Anderson, J.G.; Rainey, M.R.; Eysenbach, G. The Impact of CyberHealthcare on the Physician–Patient Relationship. J. Med. Syst. 2003, 27, 67–84. [Google Scholar] [CrossRef]
- Zeithaml, V.A.; Parasuraman, A.; Malhotra, A. Service Quality Delivery through Web Sites: A Critical Review of Extant Knowledge. J. Acad. Mark. Sci. 2002, 30, 362–375. [Google Scholar] [CrossRef] [Green Version]
- Gronroos, C. Marketing as promise management: Regaining customer management for marketing. J. Bus. Ind. Mark. 2009, 24, 351–359. [Google Scholar] [CrossRef]
- Jia, L.; Cegielski, C.G.; Zhang, Q. The Effect of Trust on Customers’ Online Repurchase Intention in Consumer-to-Consumer Electronic Commerce. In Web-Based Services: Concepts, Methodologies, Tools, and Applications; Iran Project Management Association, Ed.; IGI Global: Hershey, PA, USA, 2016; pp. 1534–1555. [Google Scholar]
- Nel, J.; Boshoff, C. Development of application-based mobile-service trust and online trust transfer: An elaboration likelihood model perspective. Behav. Inf. Technol. 2017, 36, 809–826. [Google Scholar] [CrossRef]
- Gong, Y.; Wang, H.; Xia, Q.; Zheng, L.; Shi, Y. Factors that determine a Patient’s willingness to physician selection in online healthcare communities: A trust theory perspective. Technol. Soc. 2021, 64, 101510. [Google Scholar] [CrossRef]
- Madu, C.N.; Madu, A.A. Dimensions of e-quality. Int. J. Qual. Reliab. 2002, 19, 246–258. [Google Scholar] [CrossRef]
- Zeithaml, V.A. Consumer Perceptions of Price, Quality, and Value: A Means-End Model and Synthesis of Evidence. J. Mark. 1988, 52, 2–22. [Google Scholar] [CrossRef]
- Chaitchik, S.; Kreitler, S.; Shared, S.; Schwartz, I.; Rosin, R. Doctor-patient communication in a cancer ward. J. Cancer Educ. 1992, 7, 41–54. [Google Scholar] [CrossRef]
- Roter, D.L.; Stewart, M.; Putnam, S.M.; Lipkin, M., Jr.; Stiles, W.; Inui, T.S. Communication Patterns of Primary Care Physicians. J. Am. Med. Assoc. 1997, 277, 350–356. [Google Scholar] [CrossRef]
- Emanuel, E.J.; Emanuel, L.L. Four Models of the Physician-Patient Relationship. J. Am. Med. Assoc. 1992, 267, 2221–2226. [Google Scholar] [CrossRef]
- Xiang, J.; Stanley, S.J. From online to offline: Exploring the role of e-health consumption, patient involvement, and patient-centered communication on perceptions of health care quality. Comput. Hum. Behav. 2017, 70, 446–452. [Google Scholar] [CrossRef]
- Deng, Z.H.; Lu, Y.B.; Wei, K.K.; Zhang, J.L. Understanding customer satisfaction and loyalty: An empirical study of mobile instant messages in China. Int. J. Inf. Manag. 2010, 30, 289–300. [Google Scholar] [CrossRef]
- Childers, T.L.; Carr, C.L.; Peck, J.; Carson, S. Hedonic and utilitarian motivations for online retail shopping behavior. J. Retail. 2001, 77, 511–535. [Google Scholar] [CrossRef]
- Keeney, R.L. The value of Internet commerce to the customer. Manag. Sci. 1999, 45, 533–542. [Google Scholar] [CrossRef]
- Jarvenpaa, S.L.; Tractinsky, N.; Vitale, M. Consumer trust in an Internet store. Inf. Technol. Manag. 2000, 1, 45–71. [Google Scholar] [CrossRef]
- Jones, K.; Leonard, L.N.K. Factors influencing buyer’s trust in consumer-to-consumer e commmerce. J. Comput. Inf. Syst. 2014, 54, 71–79. [Google Scholar] [CrossRef]
- Choi, K.S.; Cho, W.H.; Lee, S.; Lee, H.; Kim, C. The relationships among quality, value, satisfaction and behavioral intention in health care provider choice: A South Korean study. J. Bus. Res. 2004, 57, 913–921. [Google Scholar] [CrossRef]
- Boulding, W.; Glickman, S.W.; Manary, M.P.; Schulman, K.A.; Staelin, R. Relationship Between Patient Satisfaction With Inpatient Care and Hospital Readmission Within 30 Days. Am. J. Manag. Care 2011, 17, 41–48. [Google Scholar] [PubMed]
- Kumar, A.; Telang, R. Does the Web Reduce Customer Service Cost? Empirical Evidence from a Call Center. Inf. Syst. Res. 2012, 23, 721–737. [Google Scholar] [CrossRef] [Green Version]
- Cannon, E.; Cipriani, G.P. Quantifying halo effects in students’ evaluation of teaching. Assess. Eval. High. Educ. 2022, 47, 1–14. [Google Scholar] [CrossRef]
- Song, J.; Zahedi, F. A theoretical approach to web design in E-commerce: A belief reinforcement model. Manag. Sci. 2005, 51, 1219–1235. [Google Scholar] [CrossRef]
- Colquitt, J.A. On the dimensionality of organizational justice: A construct validation of a measure. J. Appl. Psychol. 2001, 86, 386–400. [Google Scholar] [CrossRef] [Green Version]
- Parasuraman, A.; Zeithaml, V.A.; Berry, L.L. A Conceptual Model of Service Quality and Its Implications for Future Research. J. Mark. 1985, 49, 41–50. [Google Scholar] [CrossRef]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User Acceptance of Information Technology: Toward a Unified View. MIS Q. 2003, 27, 425–478. [Google Scholar] [CrossRef] [Green Version]
- Hair, J.F.; Sarstedt, M.; Ringle, C.M. Rethinking some of the rethinking of partial least squares. Eur. J. Mark. 2019, 53, 566–584. [Google Scholar] [CrossRef]
- Lin, H.M.; Lee, M.H.; Liang, J.C.; Chang, H.Y.; Huang, P.; Tsai, C.C. A review of using partial least square structural equation modeling in e-learning research. Br. J. Educ. Technol. 2020, 51, 1354–1372. [Google Scholar] [CrossRef]
- Ali, F.; Rasoolimanesh, S.M.; Sarstedt, M.; Ringle, C.M.; Ryu, K. An assessment of the use of partial least squares structural equation modeling (PLS-SEM) in hospitality research. Int. J. Contemp. Hosp. Manag. 2018, 30, 514–538. [Google Scholar] [CrossRef] [Green Version]
- Barroso, C.; Carrión, G.C.; Roldán, J.L. Applying Maximum Likelihood and PLS on Different Sample Sizes: Studies on SERVQUAL Model and Employee Behavior Model. In Handbook of Partial Least Squares: Concepts, Methods and Applications; Esposito Vinzi, V., Chin, W.W., Henseler, J., Wang, H., Eds.; Springer: Berlin/Heidelberg, Germany, 2010; pp. 427–447. [Google Scholar]
- Ketchen, D.J. A Primer on Partial Least Squares Structural Equation Modeling. Long Range Plan. 2013, 46, 184–185. [Google Scholar] [CrossRef]
- Bagozzi, R.P.; Yi, Y. On the evaluation of structural equation models. J. Acad. Mark. Sci. 1988, 16, 74–94. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Evaluating Structural Equation Models with Unobservable Variables and Measurement Error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Cox, D.R.; Wermuth, N. A Comment on the Coefficient of Determination for Binary Responses. Am. Stat. 1992, 46, 1–4. [Google Scholar] [CrossRef]
- Tenenhaus, M.; Vinzi, V.E.; Chatelin, Y.-M.; Lauro, C. PLS path modeling. Comput. Stat. Data. Anal. 2005, 48, 159–205. [Google Scholar] [CrossRef]
- Wetzels, M.; Odekerken-Schröder, G.; Van Oppen, C. Using PLS Path Modeling for Assessing Hierarchical Construct Models: Guidelines and Empirical Illustration. MIS Q. 2009, 33, 177–195. [Google Scholar] [CrossRef]
- Henseler, J.; Ringle, C.M.; Sarstedt, M. Testing measurement invariance of composites using partial least squares. Int. Mark. Rev. 2016, 33, 405–431. [Google Scholar] [CrossRef]
- Dijkstra, T.K.; Henseler, J. Consistent and asymptotically normal PLS estimators for linear structural equations. Comput. Stat. Data. Anal. 2015, 81, 10–23. [Google Scholar] [CrossRef] [Green Version]
- Hu, L.-T.; Bentler, P.M. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychol. Methods 1998, 3, 424–453. [Google Scholar] [CrossRef]
- Chester, A.; Glass, C.A. Online counselling: A descriptive analysis of therapy services on the Internet. Br. J. Guid. Counc. 2006, 34, 145–160. [Google Scholar] [CrossRef]
- Hong, I.B.; Cho, H. The impact of consumer trust on attitudinal loyalty and purchase intentions in B2C e-marketplaces: Intermediary trust vs. seller trust. Int. J. Inf. Manag. 2011, 31, 469–479. [Google Scholar] [CrossRef]
- Lee, C.M.Y.; Thomas, E.; Norman, R.; Wells, L.; Shaw, T.; Nesbitt, J.; Frean, I.; Baxby, L.; Bennett, S.; Robinson, S. Educational attainment and willingness to use technology for health and to share health information—The reimagining healthcare survey. Int. J. Med. Inform. 2022, 164, 104803. [Google Scholar] [CrossRef]
- Aghaei, P.; Bayramzadeh, S.; Ahmadpour, S. Drive-Through Urgent Care Centers: Could They Be the Future of Healthcare Facilities? Herd-Health Env. Res. Des. J. 2022, 11, 19375867221087360. [Google Scholar] [CrossRef]
| Measure | Category | N | Percent |
|---|---|---|---|
| Gender | Male | 172 | 60.78% |
| Female | 111 | 39.22% | |
| Age | <18 | 0 | 0.00% |
| 18–24 | 27 | 9.54% | |
| 25–34 | 76 | 26.86% | |
| 35–44 | 81 | 28.62% | |
| 45–54 | 61 | 21.55% | |
| 55–64 | 29 | 10.25% | |
| Over 65 | 9 | 3.18% | |
| Education | High School | 46 | 16.25% |
| College | 79 | 27.92% | |
| Undergraduate | 101 | 35.69% | |
| Postgraduate | 57 | 20.14% |
| CA | CR | AVE | |
|---|---|---|---|
| Offline Medical Willingness (Will) | 0.921 | 0.962 | 0.927 |
| Perceived Value (Valu) | 0.912 | 0.958 | 0.919 |
| Perceived Benefits (Bene) | 0.902 | 0.939 | 0.837 |
| Individual subjectivity (Subj) | 0.970 | 0.980 | 0.943 |
| Emotional Experience (Expe) | 0.922 | 0.951 | 0.866 |
| Perceived Trust (Trus) | 0.916 | 0.947 | 0.856 |
| Online Doctor-Patient Interactions (Inte) | 0.841 | 0.904 | 0.759 |
| Online Medical Service Quality (Qual) | 0.957 | 0.972 | 0.921 |
| Will | Valu | Bene | Subj | Expe | Trus | Inte | Qual | |
|---|---|---|---|---|---|---|---|---|
| Will.1 | 0.964 | 0.883 | 0.645 | 0.643 | 0.305 | 0.459 | 0.801 | 0.459 |
| Will.2 | 0.962 | 0.856 | 0.632 | 0.602 | 0.313 | 0.465 | 0.772 | 0.463 |
| Valu.1 | 0.891 | 0.961 | 0.691 | 0.561 | 0.328 | 0.561 | 0.804 | 0.461 |
| Valu.2 | 0.840 | 0.956 | 0.683 | 0.506 | 0.260 | 0.521 | 0.755 | 0.414 |
| Bene.1 | 0.655 | 0.685 | 0.924 | 0.167 | 0.060 | 0.610 | 0.724 | 0.003 |
| Bene.2 | 0.603 | 0.670 | 0.910 | 0.148 | 0.024 | 0.562 | 0.697 | −0.044 |
| Bene.3 | 0.559 | 0.608 | 0.910 | 0.049 | 0.039 | 0.515 | 0.672 | −0.061 |
| Subj.1 | 0.663 | 0.578 | 0.154 | 0.971 | 0.082 | 0.128 | 0.395 | 0.631 |
| Subj.2 | 0.617 | 0.534 | 0.134 | 0.975 | 0.052 | 0.118 | 0.368 | 0.607 |
| Subj.3 | 0.601 | 0.506 | 0.101 | 0.966 | 0.097 | 0.102 | 0.335 | 0.603 |
| Expe.1 | 0.306 | 0.291 | 0.050 | 0.081 | 0.936 | 0.064 | 0.301 | 0.528 |
| Expe.2 | 0.329 | 0.316 | 0.092 | 0.095 | 0.930 | 0.127 | 0.315 | 0.526 |
| Expe.3 | 0.259 | 0.250 | −0.018 | 0.045 | 0.926 | 0.057 | 0.271 | 0.547 |
| Trus.1 | 0.453 | 0.520 | 0.569 | 0.115 | 0.066 | 0.929 | 0.462 | 0.166 |
| Trus.2 | 0.459 | 0.550 | 0.564 | 0.129 | 0.105 | 0.934 | 0.456 | 0.203 |
| Trus.3 | 0.419 | 0.495 | 0.580 | 0.086 | 0.075 | 0.913 | 0.437 | 0.141 |
| Inte.1 | 0.738 | 0.724 | 0.680 | 0.369 | 0.266 | 0.454 | 0.871 | 0.228 |
| Inte.2 | 0.719 | 0.730 | 0.674 | 0.317 | 0.303 | 0.398 | 0.888 | 0.263 |
| Inte.3 | 0.675 | 0.671 | 0.639 | 0.300 | 0.262 | 0.423 | 0.853 | 0.254 |
| Qual.1 | 0.454 | 0.437 | −0.044 | 0.623 | 0.549 | 0.192 | 0.265 | 0.964 |
| Qual.2 | 0.437 | 0.414 | −0.054 | 0.594 | 0.547 | 0.150 | 0.252 | 0.953 |
| Qual.3 | 0.486 | 0.464 | −0.007 | 0.604 | 0.556 | 0.191 | 0.301 | 0.962 |
| Will | Valu | Bene | Subj | Expe | Trus | Inte | Qual | |
|---|---|---|---|---|---|---|---|---|
| Will | 0.963 | |||||||
| Valu | 0.903 | 0.959 | ||||||
| Bene | 0.663 | 0.717 | 0.915 | |||||
| Subj | 0.647 | 0.557 | 0.135 | 0.971 | ||||
| Expe | 0.321 | 0.307 | 0.045 | 0.079 | 0.930 | |||
| Trus | 0.480 | 0.565 | 0.616 | 0.120 | 0.089 | 0.925 | ||
| Inte | 0.817 | 0.814 | 0.763 | 0.378 | 0.318 | 0.488 | 0.871 | |
| Qual | 0.479 | 0.457 | −0.036 | 0.633 | 0.574 | 0.185 | 0.284 | 0.959 |
| Original Sample (O) | Sample Mean (M) | T Statistics (|O/STDEV|) | p Values | |
|---|---|---|---|---|
| Valu -> Will | 0.903 | 0.904 | 91.744 | 0.000 |
| Bene -> Valu | 0.554 | 0.553 | 14.503 | 0.000 |
| Subj-> Valu | 0.446 | 0.444 | 11.186 | 0.000 |
| Expe -> Valu | 0.234 | 0.234 | 7.729 | 0.000 |
| Trus -> Valu | 0.149 | 0.151 | 4.413 | 0.000 |
| Inte -> Bene | 0.763 | 0.766 | 41.007 | 0.000 |
| Inte -> Subj | 0.378 | 0.381 | 6.754 | 0.000 |
| Qual -> Expe | 0.574 | 0.573 | 12.242 | 0.000 |
| Qual -> Trus | 0.185 | 0.192 | 2.375 | 0.018 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ye, C.; Cao, C.; Yang, J.; Shao, X. Explore How Online Healthcare Can Influence Willingness to Seek Offline Care. Int. J. Environ. Res. Public Health 2022, 19, 7925. https://doi.org/10.3390/ijerph19137925
Ye C, Cao C, Yang J, Shao X. Explore How Online Healthcare Can Influence Willingness to Seek Offline Care. International Journal of Environmental Research and Public Health. 2022; 19(13):7925. https://doi.org/10.3390/ijerph19137925
Chicago/Turabian StyleYe, Chensang, Cong Cao, Jinjing Yang, and Xiuyan Shao. 2022. "Explore How Online Healthcare Can Influence Willingness to Seek Offline Care" International Journal of Environmental Research and Public Health 19, no. 13: 7925. https://doi.org/10.3390/ijerph19137925






