Online and Offline Intervention for the Prevention of Postpartum Depression among Rural-to-Urban Floating Women: Study Protocol for a Randomized Control Trial
Abstract
:1. Introduction
2. Methods
2.1. Aim
- (1)
- Reduced PPD symptoms and stigma;
- (2)
- Improved social support, quality of life, and mother–child bonding;
- (3)
- Great satisfaction with health care received during the postpartum period.
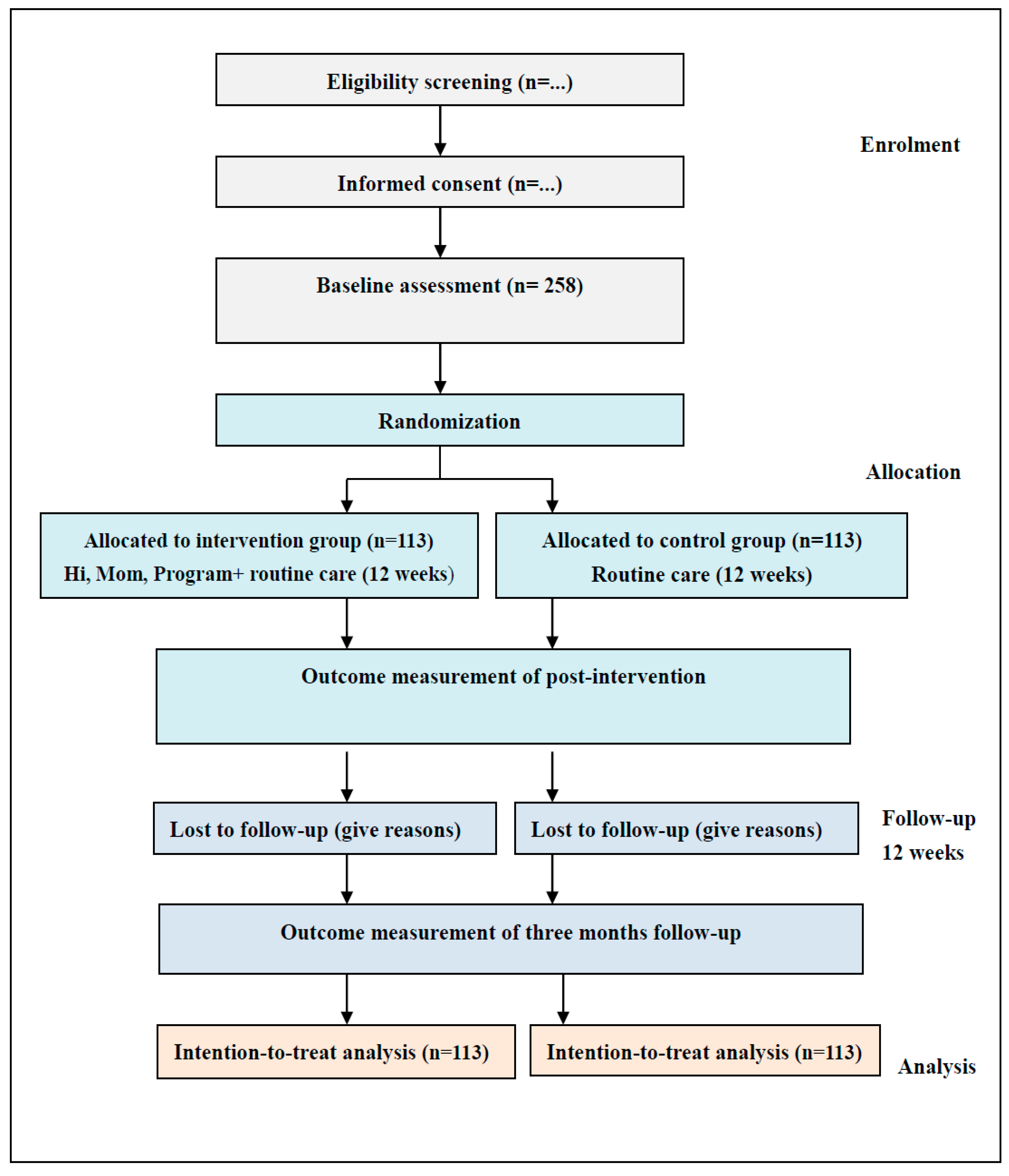
2.2. Design
2.3. Participants
2.4. Study Setting and Recruitment
2.5. Sample Size
2.6. Randomization and Blinding
2.7. Intervention
2.8. Measures
2.8.1. Social-Demographic and Clinical Data
2.8.2. Primary Outcome
2.8.3. Secondary Outcomes
2.9. Data Collection
2.10. Data Analysis
2.11. Ethical Consideration
2.12. Validity and Reliability
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cox, J.L.; Murray, D.; Chapman, G.A. A controlled study of the onset, duration and prevalence of postnatal depression. Br. J. Psych. 1993, 163, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Alba, B.M. CE: Postpartum Depression: A Nurse’s Guide. Am. J. Nurs. 2021, 121, 32–43. [Google Scholar] [CrossRef] [PubMed]
- Radzi, W.M.; Jenatabadi, H.S.; Samsudin, N. Postpartum depression symptoms in survey-based research: A structural equation analysis. BMC Public Health 2021, 21, 27. [Google Scholar] [CrossRef]
- Dadi, A.F.; Miller, E.R.; Mwanri, L. Postnatal depression and its association with adverse infant health outcomes in low-and middle-income countries: A systematic review and meta-analysis. BMC Pregnancy Childb. 2020, 20, 416. [Google Scholar] [CrossRef] [PubMed]
- Peñacoba Puente, C.; Suso-Ribera, C.; Blanco Rico, S.; Marín, D.; San Román Montero, J.; Catalá, P. Is the Association between postpartum depression and early maternal—Infant relationships contextually determined by avoidant coping in the mother? Int. J. Environ. Res. Public Health 2021, 18, 562. [Google Scholar] [CrossRef] [PubMed]
- Woldeyohannes, D.; Tekalegn, Y.; Sahiledengle, B.; Ermias, D.; Tekele Ejajo, T.; Mwanri, L. Effect of postpartum depression on exclusive breast-feeding practices in sub-Saharan Africa countries: A systematic review and meta-analysis. BMC Pregnancy Childb. 2021, 21, 113. [Google Scholar] [CrossRef]
- Branquinho, M.; Canavarro, M.C.; Fonseca, A. A blended cognitive–behavioral intervention for the treatment of postpartum depression: Study protocol for a randomized controlled trial. Int. J. Environ. Res. Public Health 2020, 17, 8631. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, Q.; Dai, X.; Xiao, G.; Luo, H. Effect of low-dose esketamine on pain control and postpartum depression after cesarean section: A retrospective cohort study. Ann. Palliat Med. 2022, 11, 45–57. [Google Scholar] [CrossRef]
- Sun, M.; Tang, S.Y.; Chen, J.; Li, Y.; Bai, W.H.; Plummer, V.; Lam, L.; Qin, C.; Cross, W.M. A study protocol of mobile phone appbased cognitive behaviour training for the prevention of postpartum depression among high-risk mothers. BMC Public Health 2019, 19, 710. [Google Scholar] [CrossRef] [Green Version]
- Chow, R.; Huang, E.; Li, A.; Li, S.; Fu, S.Y.; Son, J.S.; Foster, W.G. Appraisal of systematic reviews on interventions for postpartum depression: Systematic review. BMC Pregnancy Childbirth 2021, 21, 18. [Google Scholar] [CrossRef]
- Eberhard-Gran, M.; Eskild, A.; Opjordsmoen, S. Use of psychotropic medications in treating mood disorders during lactation-Practical recommendations. CNS Drugs 2006, 20, 187–198. [Google Scholar] [CrossRef] [PubMed]
- Walker, A.L.; de Rooij, S.R.; Dimitrova, M.V.; Witteveen, A.B.; Verhoeven, C.J.; de Jonge, A.; Vrijkotte, T.G.M.; Henrichs, J. Psychosocial and peripartum determinants of postpartum depression: Findings from a prospective population-based cohort. The ABCD study. Compr. Psychiatry 2021, 108, 152239. [Google Scholar] [CrossRef] [PubMed]
- Mu, T.Y.; Li, Y.H.; Xu, R.X.; Chen, J.; Wang, Y.Y.; Shen, C.Z. Internet-based interventions for postpartum depression: A systematic review and meta-analysis. Nurs. Open 2020, 8, 1125–1134. [Google Scholar] [CrossRef] [PubMed]
- Branquinho, M.; Rodriguez-Muñoz, M.F.; Maia, B.R.; Marques, M.; Matos, M.; Osma, J.; Moreno-Peral, P.; Conejo-Cerón, S.; Fonseca, A.; Vousoura, E. Effectiveness of psychological interventions in the treatment of perinatal depression: A systematic review of systematic reviews and meta-analyses. J. Affect. Disord. 2021, 291, 294–306. [Google Scholar] [CrossRef]
- Roman, M.; Constantin, T.; Bostan, C.M. The efficiency of online cognitive behavioral therapy for postpartum depressive symptomatology: A systematic review and meta-analysis. Women Health 2020, 60, 99–112. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, A.; van der Waerden, J.; Melchior, M.; Bolze, C.; El-Khoury, F.; Pryor, L. Physical activity during pregnancy and postpartum depression: Systematic review and meta-analysis. J. Affect. Disord. 2019, 246, 29–41. [Google Scholar] [CrossRef]
- Kolomanska-Bogucka, D.; Mazur-Bialy, A.I. Physical activity and the occurrence of postnatal depression-a systematic review. Medicina 2019, 55, 560. [Google Scholar] [CrossRef] [Green Version]
- Yahya, N.F.S.; Teng, N.I.M.F.; Das, S.; Juliana, N. Nutrition and physical activity interventions to ameliorate postpartum depression: A scoping review. Asia Pac. J. Clin. Nutr. 2021, 30, 662–674. [Google Scholar] [CrossRef]
- Peralta, L.R.; Cotton, W.G.; Dudley, D.A.; Hardy, L.L.; Yager, Z.; Prichard, I. Group-based physical activity interventions for postpartum women with children aged 0-5 years old: A systematic review of randomized controlled trials. BMC Womens Health 2021, 21, 435. [Google Scholar] [CrossRef]
- Henshaw, E.; Sabourin, B.; Warning, M. Treatment-seeking behaviors and attitudes survey among women at risk for perinatal depression or anxiety. J. Obs. Gynecol. Neonatal Nurs. 2013, 42, 168–177. [Google Scholar] [CrossRef]
- Gong, W.; Jin, X.; Cheng, K.; Caine, E.; Lehman, R.; Xu, D. Chinese Women’s Acceptance and Uptake of Referral after Screening for Perinatal Depression. Int. J. Environ. Res. Public Health 2020, 17, 8686. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, A.; Gorayeb, R.; Canavarro, M.C. Women’s help-seeking behaviours for depressive symptoms during the perinatal period: Socio-demographic and clinical correlates and perceived barriers to seeking professional help. Midwifery 2015, 31, 1177–1185. [Google Scholar] [CrossRef] [Green Version]
- Zhu, J.M.; Ebert, L.; Liu, X.Y.; Chan, W.C. A mobile application of breast cancer e-support program versus routine care in the treatment of Chinese women with breast cancer undergoing chemotherapy: Study protocol for a randomized controlled trial. BMC Cancer 2017, 17, 291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, V.; Xiao, S.Y.; Chen, H.H.; Hanna, F.; Dan, J.; Luo, D.; Parikh, R.; Sharma, E.; Usmani, S.; Yu, Y.; et al. The magnitude of and health system responses to the mental health treatment gap in adults in India and China. Lancet 2016, 388, 3074–3084. [Google Scholar] [CrossRef]
- Thomas, L.J.; Scharp, K.M.; Paxman, C.G. Stories of postpartum Depression: Exploring health constructs and help-seeking in mothers’ talk. Women Health 2014, 54, 373–387. [Google Scholar] [CrossRef] [PubMed]
- Vimarlund, V.; Koch, S.; Nøhr, C. Advances in E-Health. Life (Basel) 2021, 11, 468. [Google Scholar] [CrossRef]
- Lal, S.; Adair, C.E. E-mental health: A rapid review of the literature. Psychiatr. Serv. 2014, 65, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Andersson, G.; Titov, N. Advantages and limitations of Internet-based interventions for common mental disorders. World Psychiatry 2014, 13, 4–11. [Google Scholar] [CrossRef]
- Lee, E.W.; Denison, F.C.; Hor, K.; Reynolds, R.M. Web-based interventions for prevention and treatment of perinatal mood disorders: A systematic review. BMC Pregnancy Childbirth 2016, 16, 38. [Google Scholar] [CrossRef] [Green Version]
- Nair, U.; Armfield, N.R.; Chatfield, M.D.; Edirippulige, S. The effectiveness of telemedicine interventions to address maternal depression: A systematic review and meta-analysis. J. Telemed. Telecare. 2018, 24, 639–650. [Google Scholar] [CrossRef]
- Schuster, R.; Pokorny, R.; Berger, T.; Topooco, N.; Laireiter, A.R. The advantages and disadvantages of online and blended therapy: Survey study amongstlicensed psychotherapists in Austria. J. Med. Internet Res. 2018, 20, e11007. [Google Scholar] [CrossRef] [PubMed]
- Wentzel, J.; van der Vaart, R.; Bohlmeijer, E.T.; van Gemert-Pijnen, J.E. Mixing online and face-to-face therapy: How to benefit from blended care in mental health care. JMIR Ment. Health 2016, 3, e4534. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Erbe, D.; Eichert, H.C.; Riper, H.; Ebert, D.D. Blending face-to-face and internet-based interventions for the treatment of mental disorders in adults: Systematic review. J. Med. Internet Res. 2017, 19, e6588. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kooistra, L.C.; Wiersma, J.E.; Ruwaard, J.; Neijenhuijs, K.; Lokkerbol, J.; van Oppen, P.; Smit, F.; Riper, H. Cost and effectiveness of blended versus standard cognitive behavioral therapy for outpatients with depression in routine specialized mental health care: Pilot randomized controlled trial. J. Med. Internet Res. 2019, 21, e14261. [Google Scholar] [CrossRef] [PubMed]
- Van der Vaart, R.; Witting, M.; Riper, H.; Kooistra, L.; Bohlmeijer, E.T.; van Gemert-Pijnen, L.J. Blending online therapy into regular face-to-face therapy for depression: Content, ratio and preconditions according to patients and therapists using a delphi study. BMC Psychiatry 2014, 14, 355. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, Y.J.; Kang, B.; Liu, Y.W.; Li, Y.C.; Shi, G.Q.; Shen, T.; Jiang, Y.; Zhang, M.; Zhou, M.G.; Wang, L.M.; et al. Health insurance coverage and its impact on medical cost: Observations from the floating population in China. PLoS ONE 2014, 9, e111555. [Google Scholar] [CrossRef]
- Davis, D. The emergence of a new urban China: Insider’s perspectives. Contemp. Social. 2013, 42, 860–861. [Google Scholar] [CrossRef]
- National Health Commission of the People’s Republic of China. Report on the Development of Chinese Floating Population in 2018. Available online: https://www.dyhzdl.cn/k/doc/c504711cbc23482fb4daa58da0116c175e0e1e73.html (accessed on 7 January 2021). (In Chinese)
- Luo, Y.; Li, M.L. Research progress on the current situation of reproductive health knowledge-attitude-practice and its influ-encing factors of female floating population. Chin. J. Mod. Nurs. 2016, 22, 2499–2502. (In Chinese) [Google Scholar]
- Zong, Z.H.; Huang, J.Y.; Sun., X.M.; Mao, J.S.; Shu, X.Y.; Hearst, N. Prenatal care among rural to urban migrant women in China. BMC Pregnancy Childb. 2018, 18, 301. [Google Scholar] [CrossRef]
- Luo, X.Q.; Gui, J.F. Analysis on the practice and cause factors of participation in medical insurance program for urban workers by migrants in cities. Popul. Dev. 2014, 6, 43–50. (In Chinese) [Google Scholar]
- Cai, X.Z.; Yang, F.; Bian, Y. Gap analysis on hospitalized health service utilization in floating population covered by different medical insurances: Case study from Jiangsu Province, China. Int. Equity Health 2019, 18, 84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, Y.H.; Wang, T.; Fu, J.X.; Chen, M.Z.; Meng, Y.T.; Luo, Y. Access to reproductive health services among the female floating population of childbearing age: A cross-sectional study in Changsha, China. BMC Health Serv. Res. 2019, 19, 54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Q.; Zhang, Y.; Li, X.; Ye, Z.; Huang, L.; Zhang, Y.; Zheng, X. Exploring maternal self-efficacy of first-time mothers among rural-to-urban floating women: A quantitative longitudinal study in China. Int. J. Environ. Res. Public Health 2021, 18, 2793. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.M.; Ye, Z.W.; Fang, Q.Y.; Huang, L.L.; Zheng, X.J. Surveillance of parenting outcome, mental health and social support for primiparous women among rural-to-urban floating population. Healthcare 2021, 9, 1516. [Google Scholar] [CrossRef]
- Zheng, X.J.; Morrell, J.; Watts, K. Changes in maternal self-efficacy, postnatal depression symptoms and social support among Chinese primiparous women during the initial postpartum period: A longitudinal study. Midwifery 2018, 62, 151–160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baggett, K.M.; Davis, B.; Sheeber, L.B.; Ammerman, R.T.; Mosley, E.A.; Miller, K.; Feil, E.G. Minding the Gatekeepers: Referral and Recruitment of Postpartum Mothers with Depression into a Randomized Controlled Trial of a Mobile Internet Parenting Intervention to Improve Mood and Optimize Infant Social Communication Outcomes. Int. J. Environ. Res. Public Health 2020, 17, 8978. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. Int. J. Surg. 2011, 9, 672–677. [Google Scholar] [CrossRef] [Green Version]
- Cohen, J. Statistical power analysis. Curr. Dir. Psychol. Sci. 1992, 1, 98–101. [Google Scholar] [CrossRef]
- Gao, L.L.; Chan, S.W.; Sun, K. Effects of an interpersonal-psychotherapy- oriented childbirth education program for Chinese first-time childbearing women at 3-month follow-up: Randomized controlled trial. Int. J. Nurs. Stud. 2012, 49, 274–281. [Google Scholar] [CrossRef]
- Bandura, A. Self-Efficacy: The Exercise of Control; Freeman and Co.: New York, NY, USA, 1997. [Google Scholar]
- Tietjen, A.M.; Bradley, C.F. Social support and maternal psychosocialadjustment during the transition to parenthood. Can. J. Behav. Sci. 1985, 17, 109–121. [Google Scholar] [CrossRef]
- House, J.S. Work, Stress & Social Support; Addison-Wesley: New York, NY, USA; Reading, MA, USA, 1981. [Google Scholar]
- Zheng, X.J.; Morrell, J.; Watts, K. An Exploration of Factors Which Influencematernal Self-Efficacy in Primiparous Women in China During the Initial Postnatalperiod; The University of Nottingham: Nottingham, MA, USA, 2015. [Google Scholar]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression: Development of the 10-item Edinburgh postnatal depression scale. Brit. J. Psychiat. 1987, 150, 782–786. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Y.Q.; Guo, X.J.; Lau, Y.; Chan, K.S.; Yin, L.; Chen, J. Psychometric evaluation of the Mainland Chinese version of the Edinburgh postnatal depression scale. Int. J. Nurs. Stud. 2009, 46, 813–823. [Google Scholar] [CrossRef] [PubMed]
- Gierk, B.J.; Löwe, B.; Murray, A.M.; Kohlmann, S. Assessment of perceived mental health-related stigma: The Stigma-9 Questionnaire (STIG-9). Psychiat Res. 2018, 270, 822–830. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Zheng, X.X. The relationship between social support and postnatal depression of primiparous women. Chin. J. Nurs. 2001, 36, 731–733. (In Chinese) [Google Scholar]
- Wang, H.M.; Patrick, D.L.; Edwards, T.C.; Skalicky, A.M.; Zeng, H.Y.; Gu, W.W. Validation of the EQ-5D in a general population sample in urban China. Qual. Life Res. 2012, 21, 155–160. [Google Scholar] [CrossRef]
- Siu, B.W.M.; Ip, P.; Chow, H.M.T.; Kwok, S.S.P.; Li, O.L.; Koo, M.L.; Cheung, E.F.C.; Yeung, T.M.H.; Hung, S.F. Impairment of Mother-Infant Relationship Validation of the Chinese Version of Postpartum Bonding Questionnaire. J. Nerv. Ment. Dis. 2010, 198, 174–179. [Google Scholar] [CrossRef]

| Items | Intervention Group | Control Group |
|---|---|---|
| Brief name | “Hi, Mom” + routine care | Routine care |
| Who provided | Researchers | Obstetricians, obstetric nurses, community doctors |
| Where | Web environment, home | Hospital, home |
| How (medium) | Online intervention by internet Offline intervention by face-to-face | Routine care by face-to-face |
| What | Information module; communication module; ask-the-expert module; peer story module; and face-to-face consulting. | Routine postpartum care, home visiting. |
| How long and how often | From childbirth to 3 month postpartum. The total intervention time not less than 12 weeks. Reminder telephones every week, reminding them to log in the online session at least twice a week, and no less than total 1 h per week; and attending 2 face-to-face consulting meetings, about 30–45min each time. | From childbirth to 1 month postpartum. At least 2 home visits. |
| When assessed | Baseline (preintervention) Postintervention (immediately after intervention) Follow-up (three months after intervention) | Baseline (preintervention) Postintervention (immediately after intervention) Follow-up (three months after intervention) |
| Variables | Baseline (T0) | Postintervention (T2) | Three Months Follow-Up (T3) |
|---|---|---|---|
| Sociodemographic and clinical data | ※ | ||
| Postpartum depression symptoms | ※ | ※ | ※ |
| Postpartum depression stigma | ※ | ※ | ※ |
| Social support | ※ | ※ | ※ |
| Quality of life | ※ | ※ | ※ |
| Mother–child bonding | ※ | ※ | ※ |
| Satisfaction with health care received | ※ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qiu, X.; Li, T.; Fang, Q.; Huang, L.; Zheng, X. Online and Offline Intervention for the Prevention of Postpartum Depression among Rural-to-Urban Floating Women: Study Protocol for a Randomized Control Trial. Int. J. Environ. Res. Public Health 2022, 19, 7951. https://doi.org/10.3390/ijerph19137951
Qiu X, Li T, Fang Q, Huang L, Zheng X. Online and Offline Intervention for the Prevention of Postpartum Depression among Rural-to-Urban Floating Women: Study Protocol for a Randomized Control Trial. International Journal of Environmental Research and Public Health. 2022; 19(13):7951. https://doi.org/10.3390/ijerph19137951
Chicago/Turabian StyleQiu, Xichenhui, Ting Li, Qiyu Fang, Lingling Huang, and Xujuan Zheng. 2022. "Online and Offline Intervention for the Prevention of Postpartum Depression among Rural-to-Urban Floating Women: Study Protocol for a Randomized Control Trial" International Journal of Environmental Research and Public Health 19, no. 13: 7951. https://doi.org/10.3390/ijerph19137951






