Does Vaccinating against Influenza in a Given Epidemic Season Have an Impact on Vaccination in the Next Season: A Follow-Up Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population and Setting
2.2. Study Instrument
2.3. Follow-Up Study
2.4. Statistical Analysis
3. Results
3.1. Demographic Characteristics of Patients
3.2. Influenza Knowledge Scores
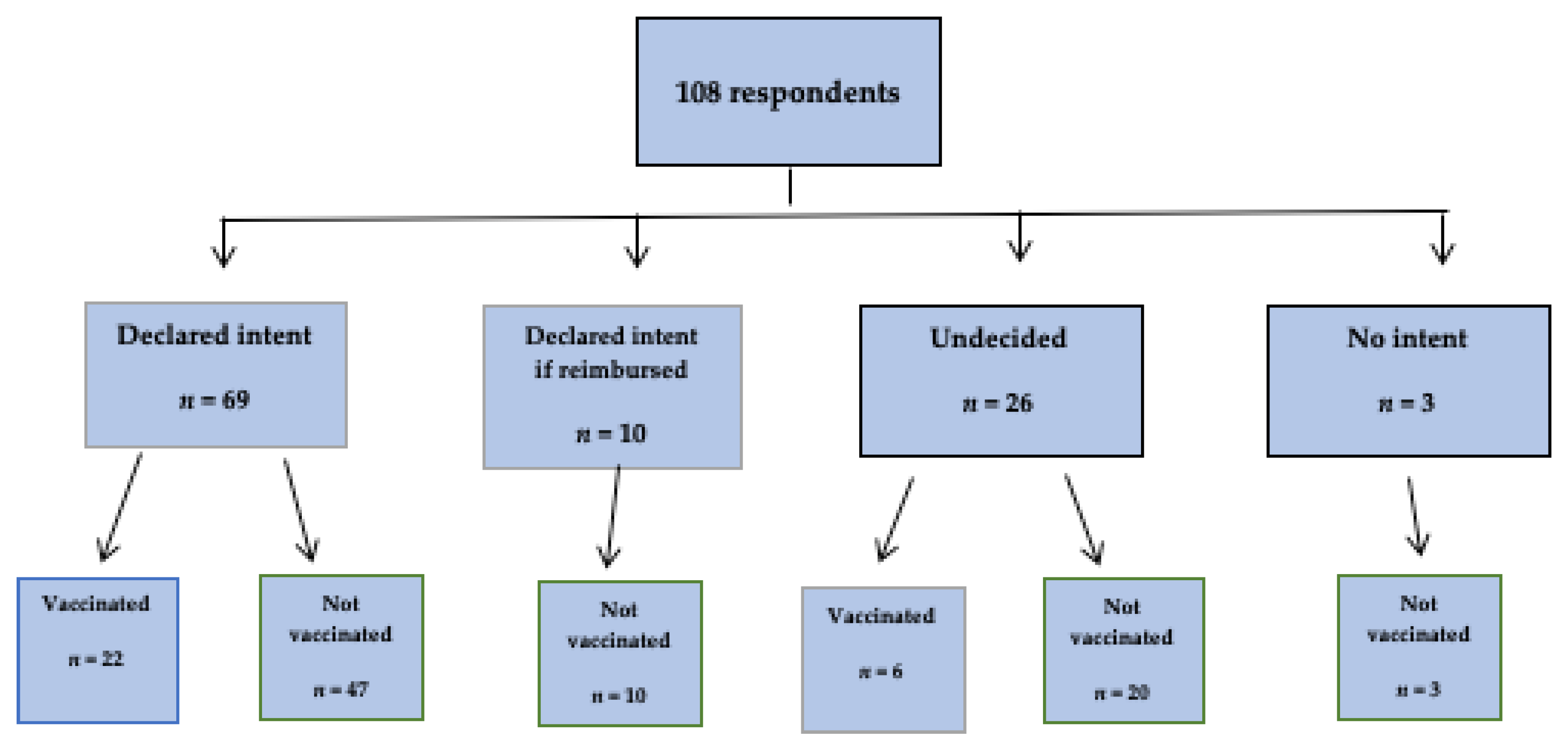
3.3. Influenza Vaccination Status
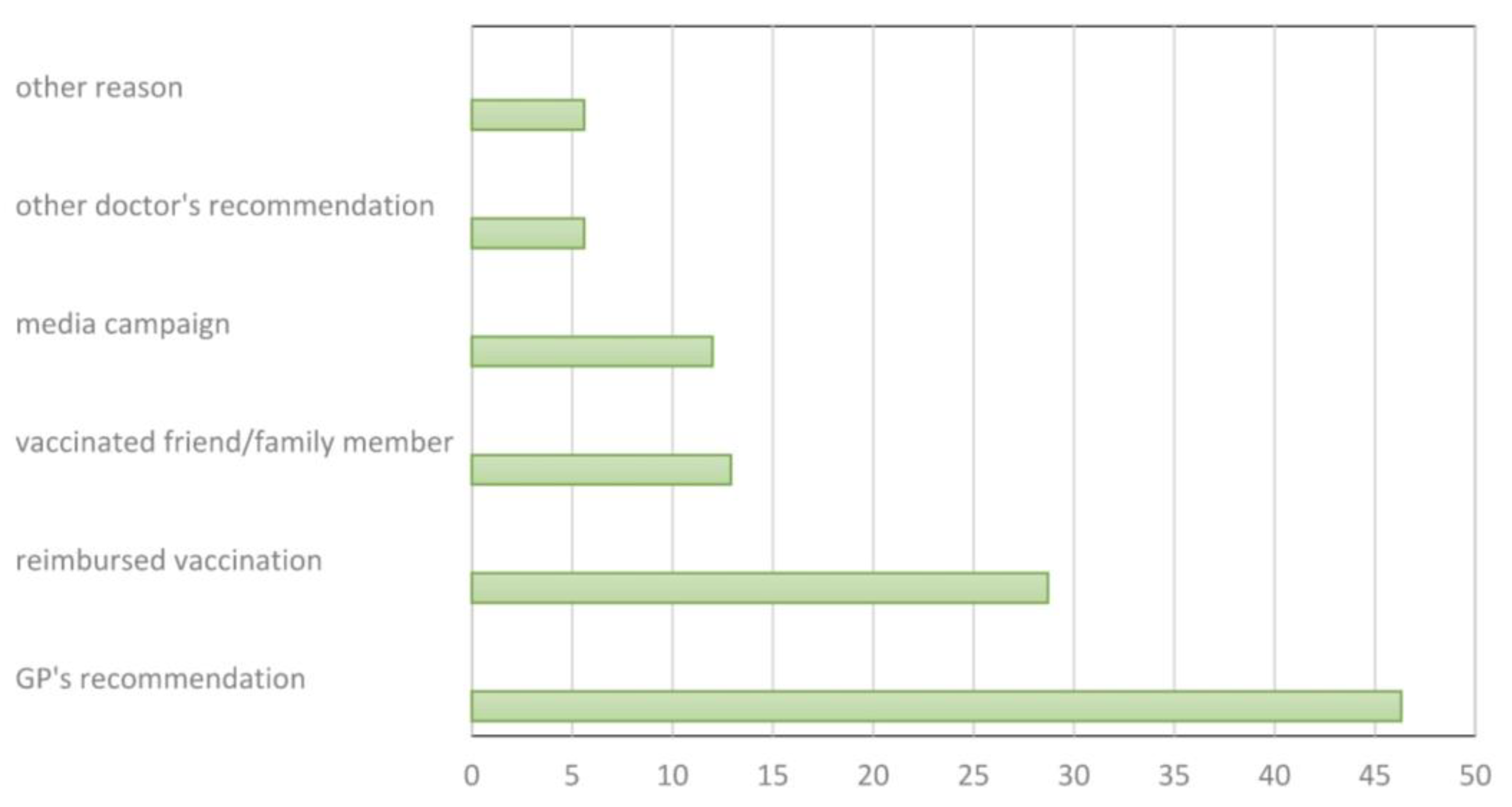
3.4. Factors Associated with Continued Adherence to Influenza Vaccination
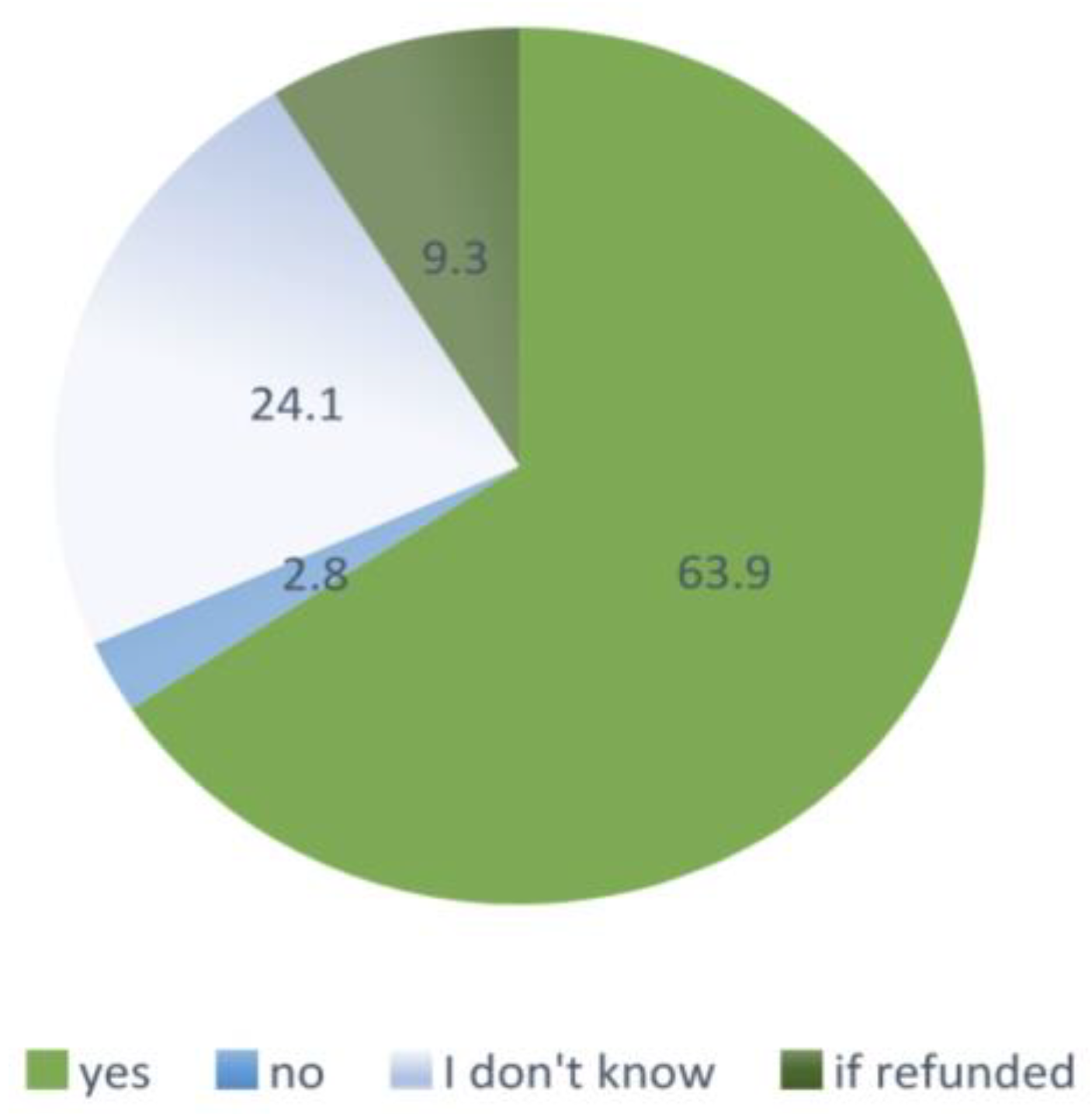
3.5. Predictors of Being Vaccinated in the Following Year
4. Discussion
4.1. Results Overview
4.2. Reported Influenza Vaccination Intentions and Vaccine Receipt in the Next Season
4.3. Limitations
4.4. Implications for Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cassini, A.; Colzani, E.; Pini, A.; Mangen, M.-J.J.; Plass, D.; McDonald, S.A.; Maringhini, G.; van Lier, A.; Haagsma, J.A.; Havelaar, A.H.; et al. Impact of infectious diseases on population health using incidence-based disability-adjusted life years (DALYs): Results from the Burden of Communicable Diseases in Europe study, European Union and European Economic Area countries, 2009 to 2013. Eurosurveillance 2018, 23, 17-00454. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keilman, L.J. Seasonal Influenza (Flu). Nurs. Clin. N. Am. 2019, 54, 227–243. [Google Scholar] [CrossRef] [PubMed]
- Goettler, D.; Niekler, P.; Liese, J.G.; Streng, A. Epidemiology and direct healthcare costs of Influenza-associated hospitalizations—Nationwide inpatient data (Germany 2010–2019). BMC Public Health 2022, 22, 108. [Google Scholar] [CrossRef] [PubMed]
- Smetana, J.; Chlibek, R.; Shaw, J.; Splino, M.; Prymula, R. Influenza vaccination in the elderly. Hum. Vaccines Immunother. 2018, 14, 540–549. [Google Scholar] [CrossRef] [PubMed]
- Polish Mandatory Immunization Program for 2022. Available online: https://www.gov.pl/web/gis/program-szczepien-ochronnych-na-rok-2022 (accessed on 16 May 2022).
- Free Influenza Vaccinations for Adults. Available online: https://szczepienia.pzh.gov.pl-bezplatne-szczepienia-przeciw-grypie-dladoroslych (accessed on 29 January 2022).
- National Institute of Public Health—National Research Institute Department of Epidemiology and Surveillance of Infectious Diseases. Vaccinations in Poland in 2020. Influenza. Available online: http://wwwold.pzh.gov.pl/oldpage/epimeld/2020/Sz_2020.pdf (accessed on 26 April 2022).
- ECDC. Seasonal Influenza Vaccination and Antiviral Use in EU/EEA Member States; Technical Report; ECDC: Stockholm, Sweden, 2018; Available online: http://www.ecdc.europa.eu/en/publications-data/seasonal-influenza-vaccination-antiviral-use-eu-eea-member-states (accessed on 12 May 2022).
- Okoli, G.N.; Lam, O.L.T.; Racovitan, F.; Reddy, V.K.; Righolt, C.H.; Neilson, C.; Chit, A.; Thommes, E.; Abou-Setta, A.M.; Mahmud, S.M. Seasonal influenza vaccination in older people: A systematic review and meta-analysis of the determining factors. PLoS ONE 2020, 15, e0234702. [Google Scholar] [CrossRef]
- Dyda, A.; Karki, S.; Hayen, A.; MacIntyre, C.R.; Menzies, R.; Banks, E.; Kaldor, J.M.; Liu, B. Influenza and pneumococcal vaccination in Australian adults: A systematic review of coverage and factors associated with uptake. BMC Infect. Dis. 2016, 16, 515. [Google Scholar] [CrossRef]
- Nagata, J.M.; Hernández-Ramos, I.; Kurup, A.S.; Albrecht, D.; Vivas-Torrealba, C.; Franco-Paredes, C. Social determinants of health and seasonal influenza vaccination in adults ≥ 65 years: A systematic review of qualitative and quantitative data. BMC Public Health 2013, 13, 388. [Google Scholar] [CrossRef] [Green Version]
- Jain, A.; van Hoek, A.; Boccia, D.; Thomas, S.L. Lower vaccine uptake amongst older individuals living alone: A systematic review and meta-analysis of social determinants of vaccine uptake. Vaccine 2017, 35, 2315–2328. [Google Scholar] [CrossRef]
- Ganczak, M.; Gil, K.; Korzeń, M.; Bażydło, M. Coverage and Influencing Determinants of Influenza Vaccination in Elderly Patients in a Country with a Poor Vaccination Implementation. Int. J. Environ. Res. Public Health 2017, 14, 665. [Google Scholar] [CrossRef] [Green Version]
- Kwong, E.; Pang, S.M.-C.; Choi, P.-P.; Wong, T.K.-S. Influenza vaccine preference and uptake among older people in nine countries. J. Adv. Nurs. 2010, 66, 2297–2308. [Google Scholar] [CrossRef]
- Nessler, K.; Krztoń-Królewiecka, A.; Chmielowiec, T.; Jarczewska, D.; Windak, A. Determinants of influenza vaccination coverage rates among primary care patients in Krakow, Poland and the surrounding region. Vaccine 2014, 32, 7122–7127. [Google Scholar] [CrossRef] [PubMed]
- Harris, K.M.; Maurer, J.; Lurie, N. Do People Who Intend to Get a Flu Shot Actually Get One? J. Gen. Intern. Med. 2009, 24, 1311–1313. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Baz, I.; Aguilar-Palacio, I.; Morán, J.; Albéniz, E.; Aldaz, P.; Castilla, J. Factors associated with continued adherence to influenza vaccination in the elderly. Prev. Med. 2012, 55, 246–250. [Google Scholar] [CrossRef] [PubMed]
- Ye, L.; Fang, T.; Cui, J.; Zhu, G.; Ma, R.; Sun, Y.; Li, P.; Li, H.; Dong, H.; Xu, G. The intentions to get vaccinated against influenza and actual vaccine uptake among diabetic patients in Ningbo, China: Identifying motivators and barriers. Hum. Vaccines Immunother. 2021, 17, 106–118. [Google Scholar] [CrossRef] [PubMed]
- Greyson, D.; Dubé, È.; Fisher, W.A.; Cook, J.; Sadarangani, M.; Bettinger, J.A. Understanding Influenza Vaccination During Pregnancy in Canada: Attitudes, Norms, Intentions, and Vaccine Uptake. Health Educ. Behav. 2021, 48, 680–689. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, B.A.; Ruiter, R.A.; Chapman, G.; Kok, G. The intention to get vaccinated against influenza and actual vaccination uptake of Dutch healthcare personnel. Vaccine 2014, 32, 6986–6991. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maurer, J. Inspecting the Mechanism: A Longitudinal Analysis of Socioeconomic Status Differences in Perceived Influenza Risks, Vaccination Intentions, and Vaccination Behaviors during the 2009–2010 Influenza Pandemic. Med. Decis. Mak. 2016, 36, 887–899. [Google Scholar] [CrossRef] [Green Version]
- Statistics Poland. Demographic Base. Gryfino. Available online: https://www.demografia.stat.gov.pl (accessed on 12 December 2021).
- Ganczak, M.; Korzeń, M.; Sobieraj, E.; Goławski, J.; Pasek, O.; Biesiada, D. COVID-19 Vaccination within the Context of Reactogenicity and Immunogenicity of ChAdOx1 Vaccine Administered to Teachers in Poland. Int. J. Environ. Res. Public Health 2022, 19, 3111. [Google Scholar] [CrossRef]
- R Development Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2008. [Google Scholar]
- Hosmer, D.W.; Lemeshow, S. Applied Logistic Regression, 2nd ed.; John Wiley & Sons Inc.: New York, NY, USA; Chichester, UK; Weinheim, Germany; Brisbane, QLD, Australia; Singapore; Toronto, ON, Canada, 2000. [Google Scholar]
- Venables, W.N.; Ripley, B.D. Modern Applied Statistics with S, 4th ed.; Springer: New York, NY, USA, 2002. [Google Scholar]
- Kharroubi, G.; Cherif, I.; Bouabid, L.; Gharbi, A.; Boukthir, A.; Ben Alaya, N.; Ben Salah, A.; Bettaieb, J. Influenza vaccination knowledge, attitudes, and practices among Tunisian elderly with chronic diseases. BMC Geriatr. 2021, 21, 700. [Google Scholar] [CrossRef]
- Shen, S.C.; Dubey, V. Addressing vaccine hesitancy: Clinical guidance for primary care physicians working with parents. Can. Fam. Physician 2019, 65, 175–181. [Google Scholar]
- MacDonald, N.; ESAGE Working Group on Vaccine Hesitancy. Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Beckett, M.K.; Elliott, M.N.; Haviland, A.M.; Burkhart, Q.; Gaillot, S.; Montfort, D.; Saliba, D. Living Alone and Patient Care Experiences: The Role of Gender in a National Sample of Medicare Beneficiaries. J. Gerontol. Ser. A 2015, 70, 1242–1247. [Google Scholar] [CrossRef] [PubMed]
- InterviewMe. Are Poles Concerned of Retirement? 2021 Survey. Available online: https://interviewme.pl/blog/czy-polacy-boja-sie-emerytury-badanie (accessed on 2 April 2022).
- Population Structure and Ageing; Eurostat Statistics Explained. 2022. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=population_structure_and_aging#The_share_of_elderly_people_continues_to_increase (accessed on 1 May 2022).
- Yang, J.; Atkins, K.E.; Feng, L.; Baguelin, M.; Wu, P.; Yan, H.; Lau, E.; Wu, J.T.K.; Liu, Y.; Cowling, B.J.; et al. Cost-effectiveness of introducing national seasonal influenza vaccination for adults aged 60 years and above in mainland China: A modelling analysis. BMC Med. 2020, 18, 90. [Google Scholar] [CrossRef] [PubMed]
- García, A.; de Lejarazu, R.O.; Reina, J.; Callejo, D.; Cuervo, J.; Larragueta, R.M. Cost–effectiveness analysis of quadrivalent influenza vaccine in Spain. Hum. Vaccines Immunother. 2016, 12, 2269–2277. [Google Scholar] [CrossRef] [Green Version]
- Brydak, L.; Roïz, J.; Faivre, P.; Reygrobellet, C. Implementing an Influenza Vaccination Programme for Adults Aged ≥65 Years in Poland: A cost-effectiveness analysis. Clin. Drug Investig. 2012, 32, 73–85. [Google Scholar] [CrossRef]
- Kim, Y.-K.; Song, J.Y.; Jang, H.; Kim, T.H.; Koo, H.; Varghese, L.; Han, E. Cost Effectiveness of Quadrivalent Influenza Vaccines Compared with Trivalent Influenza Vaccines in Young Children and Older Adults in Korea. PharmacoEconomics 2018, 36, 1475–1490. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meier, G.; Gregg, M.; Nautrup, B.P. Cost-effectiveness analysis of quadrivalent influenza vaccination in at-risk adults and the elderly: An updated analysis in the UK. J. Med. Econ. 2015, 18, 746–761. [Google Scholar] [CrossRef]
- Gorman, J.R.; Brewer, N.T.; Wang, J.B.; Chambers, C.D. Theory-based predictors of influenza vaccination among pregnant women. Vaccine 2012, 31, 213–218. [Google Scholar] [CrossRef]

| Characteristics | n/N | % | p | OR | 95%CI | |
|---|---|---|---|---|---|---|
| Gender | Female Male | 13/49 15/59 | 26.5 25.4 | 1.00 | 0.59 | 0.41–2.74 |
| Age (years) | 55–67 68–85 | 18/59 10/49 | 30.5 20.4 | 0.27 | 1.06 | 0.21–1.54 |
| Marital status | Married Other | 25/71 3/37 | 35.2 8.1 | 0.002 * | 6.07 | 1.64–33.95 |
| Employed | Yes No | 8/16 20/92 | 50.0 21.7 | 0.03 * | 3.57 | 1.02–12.5 |
| Comorbidities | Yes No | 9/37 19/71 | 24.3 26.8 | 0.82 | 0.88 | 0.31–2.38 |
| Vaccinated in the 2017/2018 season | Yes No | 10/17 18/91 | 58.8 19.8 | 0.002 * | 5.67 | 1.69–20.28 |
| Vaccinated ever before the 2017/2018 season | Yes No | 17/41 11/67 | 41.5 16.4 | 0.006 * | 2.61 | 0.98–7.02 |
| Who recommended vaccination | Doctor/nurse Other | 16/57 12/51 | 28.1 23.5 | 0.66 | 1.19 | 0.23–4.16 |
| Vaccination intent in the next year | Yes No | 22/69 6/39 | 31.9 15.4 | 0.07 | 1.47 | 0.49–5.03 |
| Sources of knowledge about influenza | Doctor/nurse Other | 17/71 11/37 | 23.9 29.7 | 0.64 | 0.75 | 0.28–2.03 |
| Influenza knowledge level | High Low | 9/31 19/77 | 29.0 24.7 | 0.82 | 1.25 | 0.43–3.44 |
| Variable | Estimate | 95% CI | p |
|---|---|---|---|
| Intercept | 0.30 | 0.0005–168.61 | 0.71 |
| Married/cohabitating | 6.12 | 1.68–34.57 | 0.01 * |
| Non-employed | 0.22 | 0.04–0.996 | 0.05 * |
| Vaccinated in the previous (2017/18) season | 4.22 | 1.08–17.66 | 0.04 * |
| Vaccinated ever before the 2017/2018 season | 1.72 | 0.56–5.16 | 0.33 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ganczak, M.; Dubiel, P.; Drozd-Dąbrowska, M.; Korzeń, M. Does Vaccinating against Influenza in a Given Epidemic Season Have an Impact on Vaccination in the Next Season: A Follow-Up Study. Int. J. Environ. Res. Public Health 2022, 19, 7976. https://doi.org/10.3390/ijerph19137976
Ganczak M, Dubiel P, Drozd-Dąbrowska M, Korzeń M. Does Vaccinating against Influenza in a Given Epidemic Season Have an Impact on Vaccination in the Next Season: A Follow-Up Study. International Journal of Environmental Research and Public Health. 2022; 19(13):7976. https://doi.org/10.3390/ijerph19137976
Chicago/Turabian StyleGanczak, Maria, Paulina Dubiel, Marzena Drozd-Dąbrowska, and Marcin Korzeń. 2022. "Does Vaccinating against Influenza in a Given Epidemic Season Have an Impact on Vaccination in the Next Season: A Follow-Up Study" International Journal of Environmental Research and Public Health 19, no. 13: 7976. https://doi.org/10.3390/ijerph19137976
APA StyleGanczak, M., Dubiel, P., Drozd-Dąbrowska, M., & Korzeń, M. (2022). Does Vaccinating against Influenza in a Given Epidemic Season Have an Impact on Vaccination in the Next Season: A Follow-Up Study. International Journal of Environmental Research and Public Health, 19(13), 7976. https://doi.org/10.3390/ijerph19137976






