Getting to the Bottom of Saddle Sores: A Scoping Review of the Definition, Prevalence, Management and Prevention of Saddle Sores in Cycling
Abstract
:1. Introduction
2. Methods
2.1. Stage 1: Identifying the Research Question
2.2. Stage 2: Identifying Relevant Studies
- Articles written in English;
- Peer-reviewed published articles (widened if insufficient papers);
- Articles that include specific reference to skin conditions affecting the saddle area;
- Articles related to dermatological saddle conditions in both genders;
- Articles related to dermatological saddle conditions arising in either elite or recreational settings;
- Articles related to dermatological saddle conditions, specifically arising from cycling.
- Articles not published;
- Inability to access full-text article;
- Grey literature.
- Search Strategy
- MEDLINE, EMBASE
- saddle sore*.mp.
- perineum/
- perineal health.mp.
- perineal.mp.
- saddle*.mp.
- folliculitis/
- bicycling/
- cycli*.mp.
- cyclist’s nodule.mp.
- third testicle.mp.
- perineal nodule.mp.
- nodular induration.mp.
- perineal abscess.mp.
- biker’s nodule.mp.
- perineal nodular induration.mp.
- nodular swelling.mp.
- perineal mass.mp.
- abscess*.mp.
- nodule*.mp.
- 1 or 2 or 3 or 4 or 5 or 6 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19
- 7 or 8
- 20 and 21
- limit 22 to (english language and humans)
- Web of Science
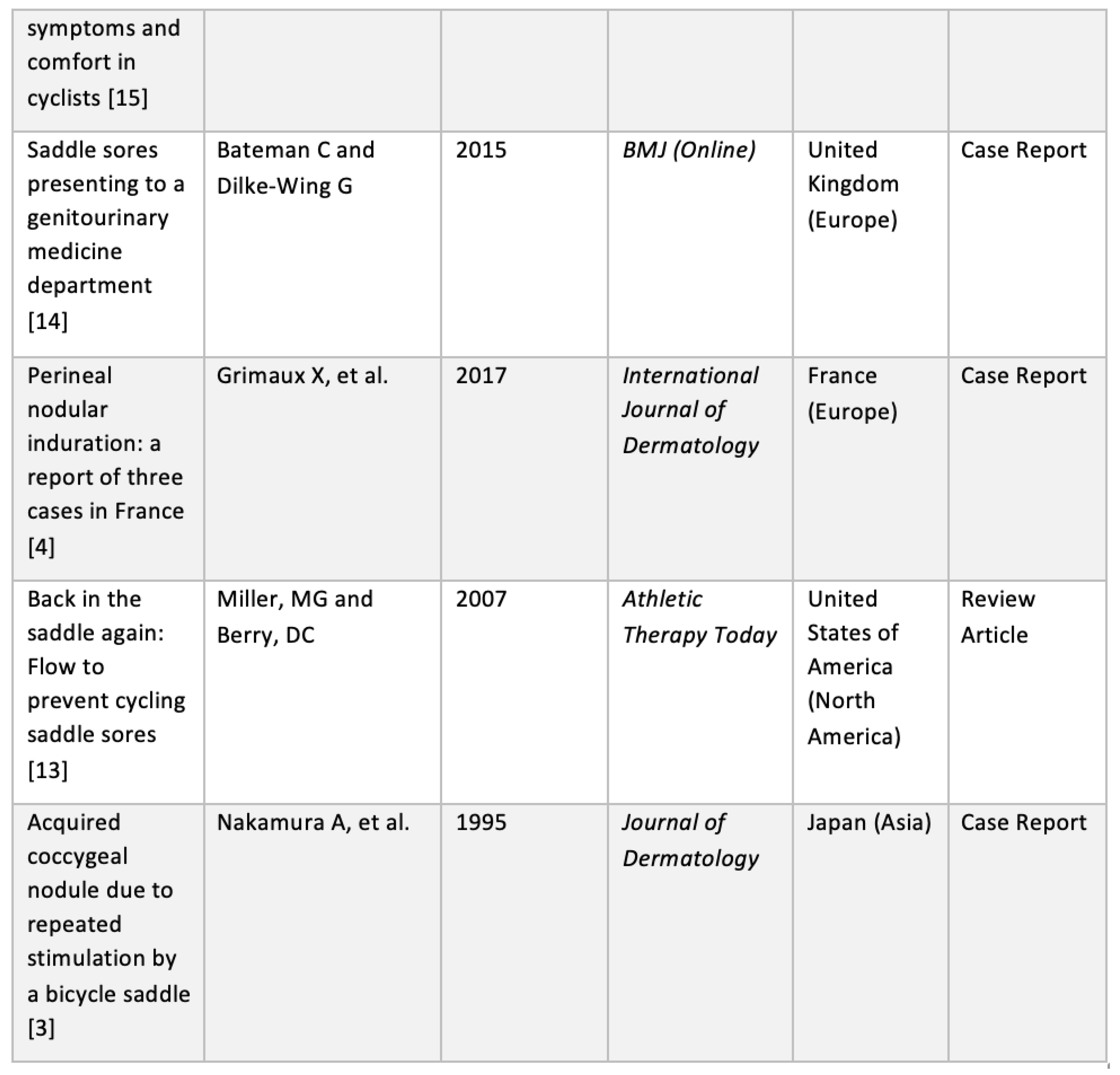
2.3. Stage 3: Study Selection
2.4. Stage 4: Charting the Data
- Author;
- Year of publication;
- Journal/Source of publication;
- Region of publication;
- Aims/Purpose of the study;
- Study population;
- Study design;
- Intervention type and duration (if applicable);
- Outcome measures and details of these (if applicable); and,
- Important results that relate to the scoping review research question above.
2.5. Stage 5: Collating, Summarising and Reporting the Results
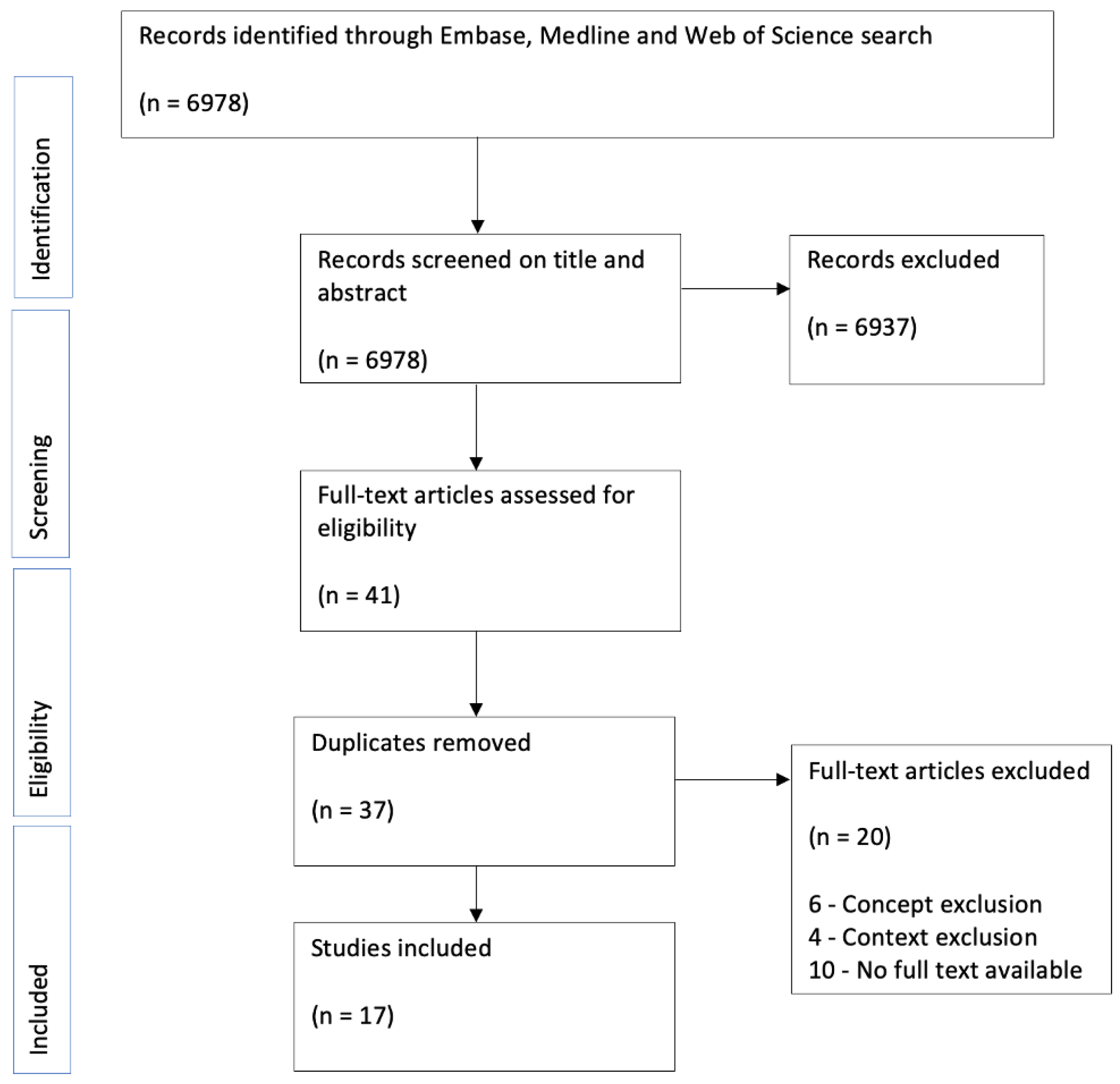
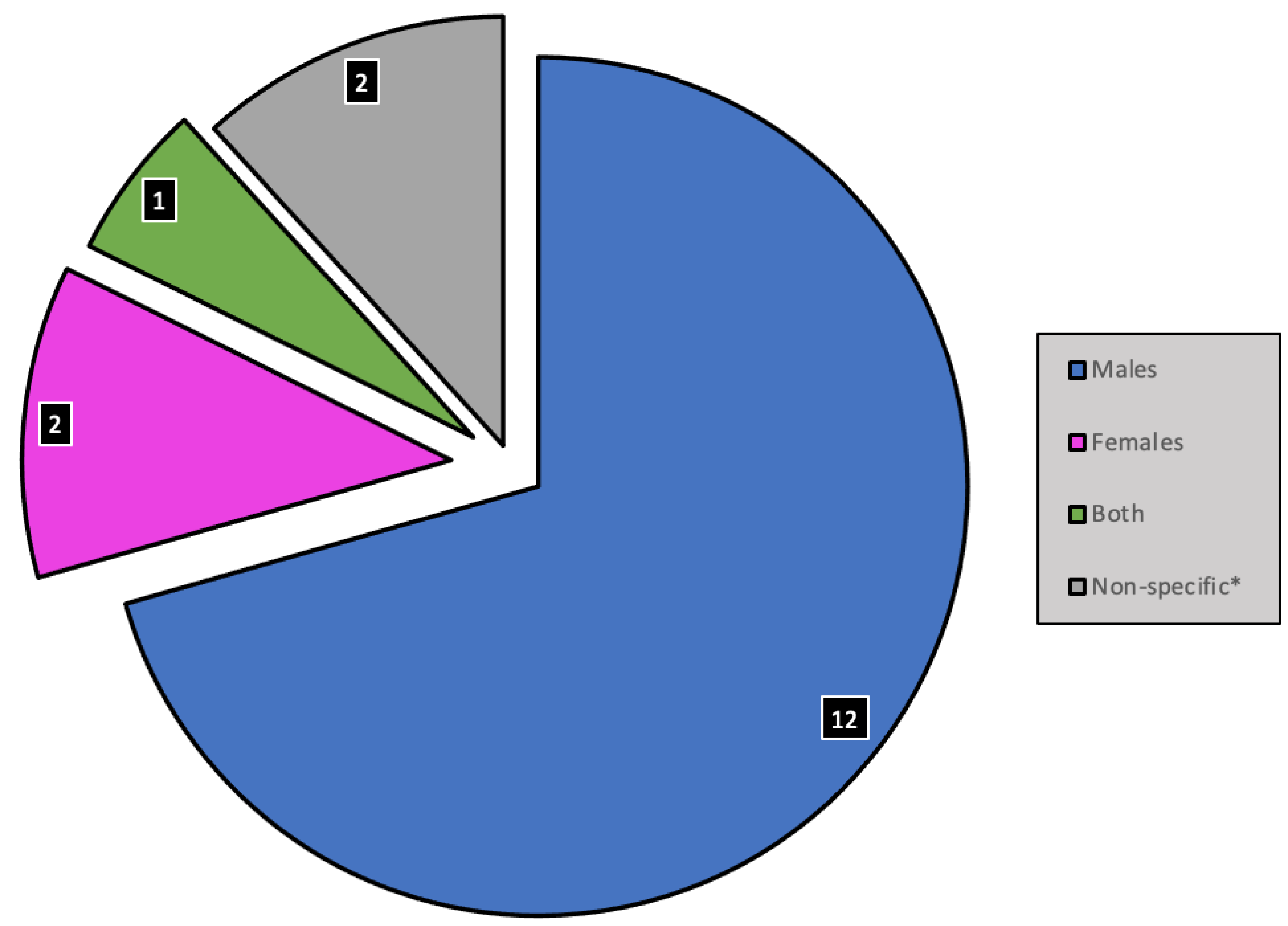
- Numerical analysis was used to summarise the data statistically. The demographic characteristics of the included studies were summarised, and outcome measures were grouped and used to assess definition, prevalence, risk factors, prevention and management. The numerical analysis is presented in tabular and graphical form (see Figure 1 and Figure 2, Table 1 and Table 2);
- Narrative synthesis was used to summarise the main findings of the review. The findings of the studies were grouped into the outcome measures definition, prevalence, risk factors, prevention and management. No assessment of the methodological limitations, risk of bias or meta-analysis of the data took place in this scoping review.
3. Results
3.1. Overview of Data
3.2. Definition
3.3. Prevalence
3.4. Risk Factors
3.5. Prevention
3.6. Treatment/Management
4. Discussion
4.1. Summary of Results
4.2. Definition
4.3. Prevalence
4.4. Risk Factors
4.5. Prevention
4.6. Treatment/Management
4.7. Proposals for Future Saddle-Sore Studies
4.8. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
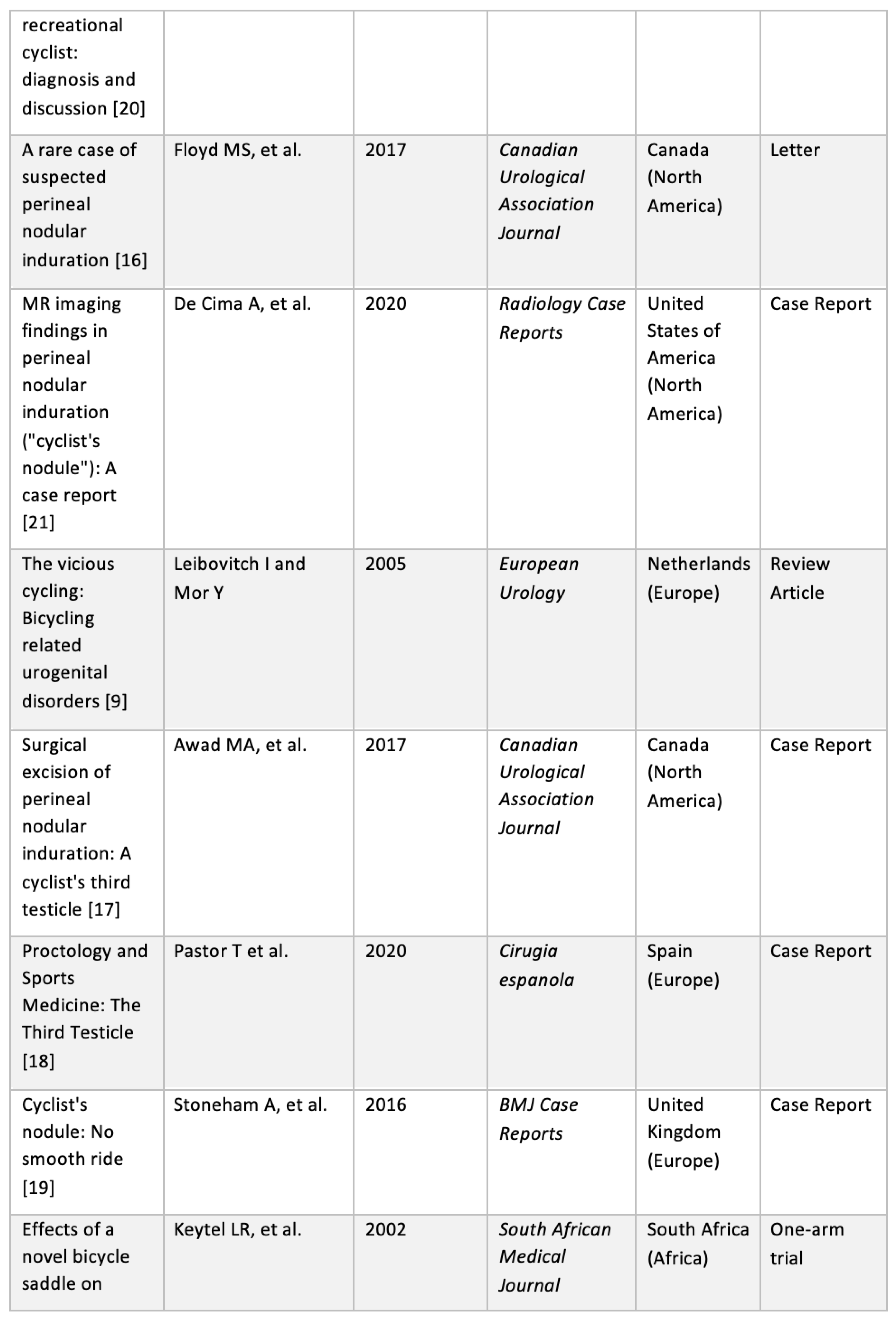
Appendix A. Data Charting

References
- Bury, K.; Leavy, J.E.; Lan, C.; O’Connor, A.; Jancey, J. A saddle sores among female competitive cyclists: A systematic scoping review. J. Sci. Med. Sport 2021, 24, 357–367. [Google Scholar] [CrossRef] [PubMed]
- Awad, M.A.; Gaither, T.W.; Murphy, G.P.; Chumnarnsongkhroh, T.; Metzler, I.; Sanford, T.; Sutcliffe, S.; Eisenberg, M.L.; Carroll, P.R.; Osterberg, E.C.; et al. Cycling, and male sexual and urinary function: Results from a large, multinational, cross-sectional study. J. Urol. 2018, 199, 798–804. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakamura, A.; Inoue, Y.; Ishihara, T.; Matsunaga, W.; Ono, T. Acquired coccygeal nodule due to repeated stimulation by a bicycle saddle. J. Dermatol. 1995, 22, 365–369. [Google Scholar] [CrossRef] [PubMed]
- Grimaux, X.; Delorme, B.; Le Clec’h, C. Perineal nodular induration: A report of three cases in France. Int. J. Dermatol. 2017, 56, 455–457. [Google Scholar] [CrossRef] [PubMed]
- Scheiba, N.; Hartschuh, W. Perineal Nodules Caused by Bicycling. Dtsch. Ärzteblatt Int. 2020, 117, 100. [Google Scholar] [CrossRef]
- UK Government Department for Transport. Road Traffic Estimates: Great Britain. 2019. Available online: https://www.gov.uk/government/statistics/road-traffic-estimates-in-great-britain-2019 (accessed on 23 October 2021).
- Warburton, D.E.; Nicol, C.W.; Bredin, S.S. Health benefits of physical activity: The evidence. Can. Med. Assoc. J. 2006, 174, 801–809. [Google Scholar] [CrossRef] [Green Version]
- Harvey, S.B.; Verland, S.; Hatch, S.L.; Wessely, S.; Mykletun, A.; Hotopf, M. Exercise and the prevention of depression: Results of the HUNT cohort study. Am. J. Psychiatry 2018, 175, 28–36. [Google Scholar] [CrossRef] [Green Version]
- Leibovitch, I.; Mor, Y. The vicious cycling: Bicycling related urogenital disorders. Eur. Urol. 2005, 47, 277–287. [Google Scholar] [CrossRef]
- De Saint Aubain Somerhausen, N.; Geurde, B.; Couvreur, Y. Perineal nodular induration: The ‘third testicle of the cyclist’, an under-recognized pseudotumour. Histopathology 2003, 42, 615–616. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miller, M.G.; Berry, D.C. Back in the saddle again: How to prevent cycling saddle sores. Athl. Ther. Today 2007, 12, 19. [Google Scholar]
- Bateman, C.; Dilke-Wing, G. Saddle sores presenting to a genitourinary medicine department. BMJ 2015, 350, h2247. [Google Scholar] [CrossRef] [Green Version]
- Keytel, L.; Noakes, T.D. Effects of a novel bicycle saddle on symptoms and comfort in cyclists. S. Afr. Med J. 2002, 92, 295–298. [Google Scholar] [PubMed]
- Floyd, M.S., Jr.; Omar, A.M.; Khattak, A.Q. A rare case of suspected perineal nodular induration. Can. Urol. Assoc. J. 2017, 11, 288. [Google Scholar] [CrossRef] [Green Version]
- Awad, M.A.; Murphy, G.P.; Gaither, T.W.; Osterberg, E.C.; Sanford, T.A.; Horvai, A.E.; Breyer, B.N. Surgical excision of perineal nodular induration: A cyclist’s third testicle. Can. Urol. Assoc. J. 2017, 11, E244. [Google Scholar] [CrossRef] [Green Version]
- Pastor, T.; Placer, C.; Tubía, J.; Enríquez-Navascués, J.M. Proctology and Sports Medicine: The Third Testicle. Cir. Esp. 2020, 98, 294. [Google Scholar] [CrossRef]
- Stoneham, A.; Thway, K.; Messiou, C.; Smith, M. Cyclist’s nodule: No smooth ride. Case Rep. 2016, 2016, bcr2015213087. [Google Scholar] [CrossRef]
- Van de Perre, S.; Vanhoenacker, F.M.; Vanstraelen, L.; Gaens, J.; Michiels, M. Perineal nodular swelling in a recreational cyclist: Diagnosis and discussion. Skelet. Radiol. 2009, 38, 933–934. [Google Scholar] [CrossRef] [Green Version]
- De Cima, A.; Pérez, N.; Ayala, G. MR imaging findings in perineal nodular induration (“cyclist’s nodule”): A case report. Radiol. Case Rep. 2020, 15, 1091–1094. [Google Scholar] [CrossRef]
- Bury, K.; Leavy, J.E.; O’Connor, A.; Jancey, J. Prevalence, prevention and treatment of saddle sores among female competitive cyclists: A scoping review protocol. Methods Protoc. 2020, 3, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dickersin, K. The existence of publication bias and risk factors for its occurrence. JAMA 1990, 263, 1385–1389. [Google Scholar] [CrossRef] [PubMed]

| Age | No. of Patients |
|---|---|
| <10 | 0 |
| 11–20 | 4 |
| 21–30 | 0 |
| 31–40 | 0 |
| 41–50 | 4 |
| 51–60 | 4 |
| 61–70 | 3 |
| >70 | 0 |
| Outcome Measure | Proposed Study |
|---|---|
| Prevalence |
|
| Prevention |
|
| Treatment |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Napier, D.; Heron, N. Getting to the Bottom of Saddle Sores: A Scoping Review of the Definition, Prevalence, Management and Prevention of Saddle Sores in Cycling. Int. J. Environ. Res. Public Health 2022, 19, 8073. https://doi.org/10.3390/ijerph19138073
Napier D, Heron N. Getting to the Bottom of Saddle Sores: A Scoping Review of the Definition, Prevalence, Management and Prevention of Saddle Sores in Cycling. International Journal of Environmental Research and Public Health. 2022; 19(13):8073. https://doi.org/10.3390/ijerph19138073
Chicago/Turabian StyleNapier, Daniel, and Neil Heron. 2022. "Getting to the Bottom of Saddle Sores: A Scoping Review of the Definition, Prevalence, Management and Prevention of Saddle Sores in Cycling" International Journal of Environmental Research and Public Health 19, no. 13: 8073. https://doi.org/10.3390/ijerph19138073