Increasing Women’s Knowledge about HPV Using BERT Text Summarization: An Online Randomized Study
Abstract
:1. Introduction
2. Literature Review
2.1. Deep Learning in the Medical Domain
2.2. Text Summarization in the Medical Domain
2.3. Research Gap and Research Objectives
3. Methods
3.1. Intervention
3.1.1. Original Text
3.1.2. Auto-Generated Summarized Text
3.2. Study Design
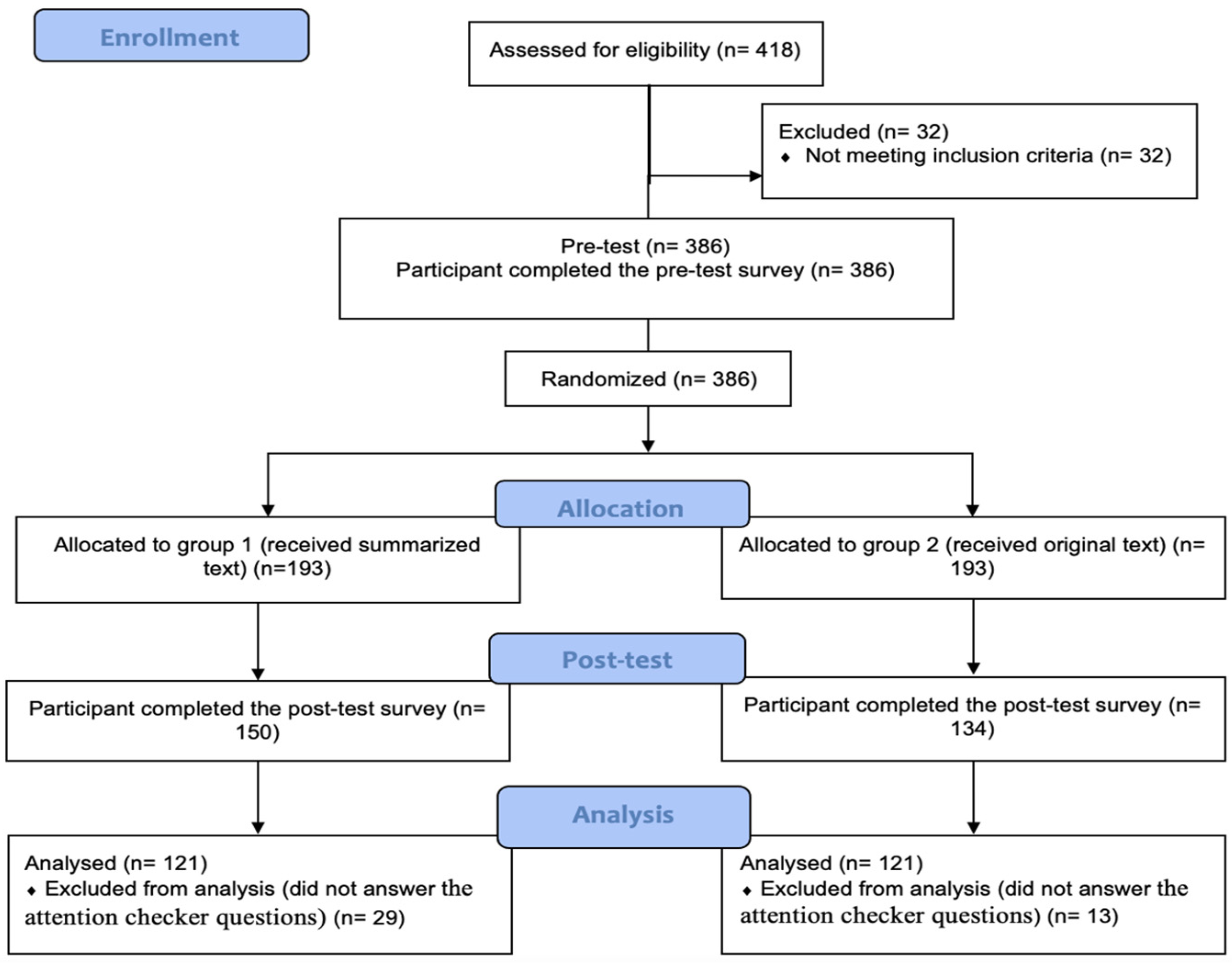
3.2.1. Eligibility and Randomization
3.2.2. HPV Knowledge Measurement
3.2.3. Participant’s Recruitment
3.3. Statistical Analysis
4. Results
5. Discussion
5.1. Principal Findings
5.2. Empirical Implications
5.3. Limitations and Future Directions
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jradi, H.; Bawazir, A. Knowledge, attitudes, and practices among Saudi women regarding cervical cancer, human papillomavirus (HPV) and corresponding vaccine. Vaccine 2019, 37, 530–537. [Google Scholar] [CrossRef] [PubMed]
- The Cancer Genome Atlas Research Network. Integrated genomic and molecular characterization of cervical cancer. Nature 2017, 543, 378–384. [Google Scholar] [CrossRef] [PubMed]
- Baccolini, V.; Isonne, C.; Salerno, C.; Giffi, M.; Migliara, G.; Mazzalai, E.; Turatto, F.; Sinopoli, A.; Rosso, A.; De Vito, C. The association between adherence to cancer screening programs and health literacy: A systematic review and meta-analysis. Prev. Med. 2022, 155, 106927. [Google Scholar] [CrossRef] [PubMed]
- Oldach, B.R.; Katz, M.L. Health literacy and cancer screening: A systematic review. Patient Educ. Couns. 2014, 94, 149–157. [Google Scholar] [CrossRef] [Green Version]
- He, J.; He, L. Knowledge of HPV and acceptability of HPV vaccine among women in western China: A cross-sectional survey. BMC Women’s Health 2018, 18, 130. [Google Scholar] [CrossRef] [Green Version]
- George, C.; Roberts, R.; Brennen, D.; Deveaux, L.; Read, S.E. Knowledge and awareness of Human Papillomavirus (HPV) and HPV vaccines among Caribbean youth: The case of the Bahamas. Hum. Vaccines Immunother. 2020, 16, 573–580. [Google Scholar] [CrossRef]
- Gamaoun, R. Knowledge, awareness and acceptability of anti-HPV vaccine in the Arab states of the Middle East and North Africa Region: A systematic review. East. Mediterr. Health J. 2018, 24, 538–548. [Google Scholar] [CrossRef]
- Grigore, M.; Teleman, S.I.; Pristavu, A.; Matei, M. Awareness and knowledge about HPV and HPV vaccine among romanian women. J. Cancer Educ. 2018, 33, 154–159. [Google Scholar] [CrossRef]
- Wang, M.; Wang, M.; Yu, F.; Yang, Y.; Walker, J.; Mostafa, J. A systematic review of automatic text summarization for biomedical literature and EHRs. J. Am. Med. Inform. Assoc. 2021, 28, 2287–2297. [Google Scholar] [CrossRef]
- Zhang, L.; Fan, H.; Peng, C.; Rao, G.; Cong, Q. Sentiment analysis methods for hpv vaccines related tweets based on transfer learning. Healthcare 2020, 8, 307. [Google Scholar] [CrossRef]
- Kim, T.; Yun, Y.; Kim, N. Deep learning-based knowledge graph generation for COVID-19. Sustainability 2021, 13, 2276. [Google Scholar] [CrossRef]
- Datta, S.; Si, Y.; Rodriguez, L.; Shooshan, S.E.; Demner-Fushman, D.; Roberts, K. Understanding spatial language in radiology: Representation framework, annotation, and spatial relation extraction from chest X-ray reports using deep learning. J. Biomed. Inform. 2020, 108, 103473. [Google Scholar] [CrossRef] [PubMed]
- Afzal, M.; Alam, F.; Malik, K.M.; Malik, G.M. Clinical Context–Aware Biomedical Text Summarization Using Deep Neural Network: Model Development and Validation. J. Med. Internet Res. 2020, 22, e19810. [Google Scholar] [CrossRef]
- Lai, P.-T.; Lu, W.-L.; Kuo, T.-R.; Chung, C.-R.; Han, J.-C.; Tsai, R.T.-H.; Horng, J.-T. Using a Large Margin Context-Aware Convolutional Neural Network to Automatically Extract Disease-Disease Association from Literature: Comparative Analytic Study. JMIR Med. Inform. 2019, 7, e14502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ayyoubzadeh, S.M.; Ayyoubzadeh, S.M.; Zahedi, H.; Ahmadi, M.; Kalhori, S.R.N. Predicting COVID-19 incidence through analysis of google trends data in iran: Data mining and deep learning pilot study. JMIR Public Health Surveill. 2020, 6, e18828. [Google Scholar] [CrossRef]
- Miotto, R.; Wang, F.; Wang, S.; Jiang, X.; Dudley, J.T. Deep learning for healthcare: Review, opportunities and challenges. Brief Bioinform. 2018, 19, 1236–1246. [Google Scholar] [CrossRef]
- Fan, B.; Fan, W.; Smith, C. Adverse drug event detection and extraction from open data: A deep learning approach. Inf. Process. Manag. 2020, 57, 102131. [Google Scholar] [CrossRef]
- Zhou, S.; Li, X. Feature engineering vs. deep learning for paper section identification: Toward applications in Chinese medical literature. Inf. Process. Manag. 2020, 57, 102206. [Google Scholar] [CrossRef]
- Șerban, O.; Thapen, N.; Maginnis, B.; Hankin, C.; Foot, V. Real-time processing of social media with SENTINEL: A syndromic surveillance system incorporating deep learning for health classification. Inf. Process. Manag. 2019, 56, 1166–1184. [Google Scholar] [CrossRef]
- Blanco, G.; Lourenço, A. Optimism and pessimism analysis using deep learning on COVID-19 related twitter conversations. Inf. Process. Manag. 2022, 59, 102918. [Google Scholar] [CrossRef]
- Chai, Y.; Bian, Y.; Liu, H.; Li, J.; Xu, J. Glaucoma diagnosis in the Chinese context: An uncertainty information-centric Bayesian deep learning model. Inf. Process. Manag. 2021, 58, 102454. [Google Scholar] [CrossRef]
- Yang, T.; Li, F.; Ji, D.; Liang, X.; Xie, T.; Tian, S.; Li, B.; Liang, P. Fine-grained depression analysis based on Chinese micro-blog reviews. Inf. Process. Manag. 2021, 58, 102681. [Google Scholar] [CrossRef]
- Kalyan, K.S.; Sangeetha, S. Bertmcn: Mapping colloquial phrases to standard medical concepts using bert and highway network. Artif. Intell. Med. 2021, 112, 102008. [Google Scholar] [CrossRef] [PubMed]
- De Vargas Romero, G.; Segura-Bedmar, I. Exploring Deep Learning for Named Entity Recognition of Tumor Morphology Mentions. In Proceedings of the Iberian Languages Evaluation Forum (IberLEF 2020), Málaga, Spain, 23 September 2020; pp. 396–411. [Google Scholar]
- Srinivasulu, K. Health-Related Tweets Classification: A Survey. In Proceedings of the International Conference on Recent Trends in Machine Learning, IoT, Smart Cities and Applications, Hyderabad, India, 29–30 March 2020; pp. 259–268. [Google Scholar]
- Zhang, X.; Zhang, Y.; Zhang, Q.; Ren, Y.; Qiu, T.; Ma, J.; Sun, Q. Extracting comprehensive clinical information for breast cancer using deep learning methods. Int. J. Med. Inform. 2019, 132, 103985. [Google Scholar] [CrossRef]
- Harnoune, A.; Rhanoui, M.; Mikram, M.; Yousfi, S.; Elkaimbillah, Z.; El Asri, B. BERT based clinical knowledge extraction for biomedical knowledge graph construction and analysis. Comput. Methods Programs Biomed. Update 2021, 1, 100042. [Google Scholar] [CrossRef]
- Sutphin, C.; Lee, K.; Yepes, A.J.; Uzuner, Ö.; McInnes, B.T. Adverse drug event detection using reason assignments in FDA drug labels. J. Biomed. Inform. 2020, 110, 103552. [Google Scholar] [CrossRef]
- Vunikili, R.; Supriya, H.; Marica, V.G.; Farri, O. Clinical NER using Spanish BERT Embeddings. In Proceedings of the Iberian Languages Evaluation Forum (IberLEF) 2020, Málaga, Spain, 23 September 2020; pp. 505–511. [Google Scholar]
- Radev, D.R.; Hovy, E.; McKeown, K. Introduction to the special issue on summarization. Comput. Linguist. 2002, 28, 399–408. [Google Scholar] [CrossRef]
- Moradi, M.; Ghadiri, N. Quantifying the informativeness for biomedical literature summarization: An itemset mining method. Comput. Methods Programs Biomed. 2017, 146, 77–89. [Google Scholar] [CrossRef] [Green Version]
- Singh, S.; Karimi, S.; Ho-Shon, K.; Hamey, L. Show, tell and summarise: Learning to generate and summarise radiology findings from medical images. Neural Comput. Appl. 2021, 33, 7441–7465. [Google Scholar] [CrossRef]
- Gayathri, P.; Jaisankar, N. Towards an Efficient Approach for Automatic Medical Document Summarization. Cybern. Inf. Technol. 2015, 15, 78–91. [Google Scholar] [CrossRef] [Green Version]
- Sarkar, K.; Nasipuri, M.; Ghose, S. Using machine learning for medical document summarization. Int. J. Database Theory Appl. 2011, 4, 31–48. [Google Scholar]
- Yoo, I.; Hu, X.; Song, I.-Y. A coherent graph-based semantic clustering and summarization approach for biomedical literature and a new summarization evaluation method. BMC Bioinform. 2007, 8 (Suppl. 9), S4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mishra, R.; Bian, J.; Fiszman, M.; Weir, C.R.; Jonnalagadda, S.; Mostafa, J.; Del Fiol, G. Text summarization in the biomedical domain: A systematic review of recent research. J. Biomed. Inform. 2014, 52, 457–467. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moen, H.; Peltonen, L.-M.; Heimonen, J.; Airola, A.; Pahikkala, T.; Salakoski, T.; Salanterä, S. Comparison of automatic summarisation methods for clinical free text notes. Artif. Intell. Med. 2016, 67, 25–37. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Human papillomavirus vaccines: WHO position paper, May 2017–Recommendations. Vaccine 2017, 35, 5753–5755. [Google Scholar] [CrossRef]
- Likes, W.M.; Itano, J. Human papillomavirus and cervical cancer: Not just a sexually transmitted disease. Clin. J. Oncol. Nurs. 2003, 7, 271–276. [Google Scholar] [CrossRef] [Green Version]
- Cutts, F.T.; Franceschi, S.; Goldie, S.; Castellsague, X.D.; De Sanjose, S.; Garnett, G.; Edmunds, W.; Claeys, P.; Goldenthal, K.; Harper, D. Human papillomavirus and HPV vaccines: A review. Bull. World Health Organ. 2007, 85, 719–726. [Google Scholar] [CrossRef] [Green Version]
- Hauser, D.J.; Schwarz, N. Attentive Turkers: MTurk participants perform better on online attention checks than do subject pool participants. Behav. Res. Methods 2016, 48, 400–407. [Google Scholar] [CrossRef]
- Carver, R.P. Reading rate: Theory, research, and practical implications. J. Read. 1992, 36, 84–95. [Google Scholar]
- Center for Disease Control and Prevention. HPV-Associated Cancer Diagnosis by Age. Available online: https://www.cdc.gov/cancer/hpv/statistics/age.htm (accessed on 13 September 2021).
- Suresh, K. An overview of randomization techniques: An unbiased assessment of outcome in clinical research. J. Hum. Reprod. Sci. 2011, 4, 8. [Google Scholar] [CrossRef]
- Waller, J.; Ostini, R.; Marlow, L.A.; McCaffery, K.; Zimet, G. Validation of a measure of knowledge about human papillomavirus (HPV) using item response theory and classical test theory. Prev. Med. 2013, 56, 35–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feder, M.A. Correlates of HPV Vaccination and Association with HPV-16 and HPV-18 DNA Detection in Young Women. Master’s Thesis, Department of Epidemiology, School of Public Health, 2017. Available online: https://epi.washington.edu/epi_research/correlates-of-hpv-vaccination-and-association-with-hpv-16-and-hpv-18-dna-detection-in-young-women/ (accessed on 13 September 2021).
- Coyne-Beasley, T.; Hochwalt, B.E. Protecting women against human papillomavirus: Benefits, barriers, and evidence-based strategies to increase vaccine uptake. North Carol. Med. J. 2016, 77, 402–405. [Google Scholar] [CrossRef] [Green Version]
- Naz, M.S.G.; Kariman, N.; Ebadi, A.; Ozgoli, G.; Ghasemi, V.; Fakari, F.R. Educational interventions for cervical cancer screening behavior of women: A systematic review. Asian Pac. J. Cancer Prev. APJCP 2018, 19, 875. [Google Scholar] [CrossRef]
- Saulle, R.; Sinopoli, A.; Baer, A.D.P.; Mannocci, A.; Marino, M.; De Belvis, A.; Federici, A.; La Torre, G. The PRECEDE–PROCEED model as a tool in Public Health screening: A systematic review. La Clin. Ter. 2020, 171, e167–e177. [Google Scholar] [CrossRef]
| Characteristics | Group 1 (N = 121) | Group 2 (N = 121) | Total (N = 242) |
|---|---|---|---|
| Age in Years | |||
| Mean (SD) | 38.3 (12.8) | 37.4 (11.6) | 37.8 (12.2) |
| Ethnicity, n (%) | |||
| Caucasian | 94 (77.7) | 92 (76.0) | 186 (76.8) |
| Hispanic | 7 (5.8) | 12 (9.9) | 20 (8.2) |
| American Indian | 2 (0.8) | 2 (1.7) | 5 (2.1) |
| Asian | 4 (1.6) | 7 (5.8) | 11 (4.5) |
| African | 6 (2.5) | 7 (5.8) | 15 (6.2) |
| Other | 8 (3.3) | 1 (0.8) | 5 (2.1) |
| Highest education level, n (%) | |||
| High school | 9 (7.4) | 11 (9.1) | 20 (8.2) |
| Associate degree | 15 (12.4) | 14 (11.6) | 29 (11.9) |
| Some collage, no degree | 22 (18.2) | 24 (19.8) | 46 (19) |
| Bachelor | 50 (41.3) | 48 (39.6) | 98 (40.5) |
| Master | 22 (18.2) | 22 (18.2) | 44 (18.2) |
| Doctorate | 3 (2.5) | 2 (1.7) | 5 (2.1) |
| Items | Answers | Group 1 | Group 2 | Total | p-Value a |
|---|---|---|---|---|---|
| Before Today, Had You Ever Heard of HPV? | Yes | 112 (92.6) | 116 (95.9) | 228 (94.2) | 0.449 |
| No | 8 (6.6) | 4 (3.3) | 12 (5.0) | ||
| Don’t know | 1 (0.8) | 1 (0.8) | 2 (0.8) | ||
| Have You Ever Heard of HPV Testing? | Yes | 94 (77.7) | 90 (74.4) | 184 (76.0) | 0.698 |
| No | 20 (16.5) | 25 (20.7) | 45 (18.6) | ||
| Don’t know | 7 (5.8) | 6 (5.0) | 13 (5.4) | ||
| Before Today, Had You Ever Heard of HPV Vaccination? | Yes | 97 (80.2) | 103 (85.1) | 184 (76.0) | 0.449 |
| No | 21 (17.4) | 17 (14.0) | 45 (18.6) | ||
| Don’t know | 3 (2.5) | 1 (0.8) | 13 (5.4) |
| Items a | Group 1 | Group 2 | p-Value b | ||||
|---|---|---|---|---|---|---|---|
| Correct n (%) | Incorrect n (%) | Do Not Know | Correct n (%) | Incorrect n (%) | Do Not Know | ||
| Having Many Sexual Partners Increases the Risk of Getting HPV (T) | 114 (94.2) | 4 (3.3) | 3 (2.5) | 117 (96.7) | 3 (2.5) | 1 (0.8) | 0.335 |
| A Person Could Have HPV for Many Years Without Knowing It (T) | 104 (86.0) | 14 (11.6) | 3 (2.5) | 108 (89.3) | 12 (9.9) | 1 (0.8) | 0.435 |
| HPV Is Very Rare (F) | 99 (81.8) | 18 (14.9) | 4 (3.3) | 93 (76.9) | 25 (20.7) | 3 (2.5) | 0.341 |
| HPV Can Cause Cervical Cancer (T) | 117 (96.7) | 3 (2.5) | 1 (0.8) | 112 (92.6) | 9 (7.4) | 0 (0) | 0.154 |
| HPV Can Be Passed on During Sexual Intercourse (T) | 114 (94.2) | 5 (4.1) | 2 (1.7) | 111 (91.7) | 6 (5.0) | 4 (3.3) | 0.450 |
| HPV Always Has Visible Signs or Symptoms (F) | 88 (72.7) | 26 (21.5) | 7 (5.8) | 95 (78.5) | 26 (21.5) | 0 (0) | 0.295 |
| Using Condoms Reduces the Risk of Getting HPV (T) | 97 (80.2) | 12 (9.9) | 12 (9.9) | 105 (86.8) | 15 (12.4) | 1 (0.8) | 0.166 |
| HPV Can Cause HIV/Aids (F) | 83 (68.6) | 28 (23.1) | 10 (8.3) | 83 (68.6) | 31 (25.6) | 7 (5.8) | 1.00 |
| HPV Can Be Passed on by Genital Skin-to-Skin Contact (T) | 98 (81.0) | 13 (10.7) | 2 (1.7) | 109 (90.1) | 11 (9.1) | 1 (0.8) | 0.061 |
| Men cannot get HPV(F) | 101 (83.5) | 15 (12.4) | 5 (4.1) | 98 (81.0) | 19 (15.7) | 4 (3.3) | 0.614 |
| Having Sex at an Early Age Increases the Risk of Getting HPV(T) | 110 (90.9) | 9 (7.4) | 2 (1.7) | 104 (86.0) | 16 (13.2) | 1 (0.8) | 0.228 |
| There Are Many Types of HPV (T) | 98 (81.0) | 13 (10.7) | 10 (8.3) | 112 (92.6) | 5 (4.1) | 4 (3.3) | 0.008 |
| HPV Can Cause Genital Warts (T) | 108 (89.3) | 9 (7.4) | 4 (3.3) | 108 (89.3) | 11 (9.1) | 2 (1.7) | 1.000 |
| HPV Can Be Cured with Antibiotics(F) | 79 (65.3) | 23 (19.0) | 19 (15.7) | 80 (66.1) | 32 (26.4) | 9 (7.4) | 0.892 |
| Most Sexually Active People Will Get HPV at Some Point in Their Lives (T) | 78 (64.5) | 32 (26.4) | 11 (9.1) | 76 (62.8) | 35 (28.9) | 10 (8.3) | 0.789 |
| HPV Usually Doesn’t Need Any Treatment (F) | 83(68.6) | 29 (24.0) | 9 (7.4) | 47 (38.8) | 70 (57.9) | 4 (3.3) | 0.0001 |
| Items a | Group 1 | Group 2 | p-Value b | ||||
|---|---|---|---|---|---|---|---|
| Correct n (%) | Incorrect n (%) | Do Not Know | Correct n (%) | Incorrect n (%) | Do Not Know | ||
| If a Woman Tests Positive for HPV She Will Definitely Get Cervical Cancer (F) | 90 (74.4) | 25 (20.7) | 6 (5) | 90 (74.4) | 30 (24.8) | 1 (0.8) | 1.000 |
| An HPV Test Can Be Done at the Same Time as a Pap Test (T) | 101 (83.5) | 8 (6.6) | 12 (9.9) | 103 (85.1) | 13 (10.7) | 5 (4.1) | 0.724 |
| An HPV Test Can Tell You How Long You Have Had an HPV Infection (F) | 63 (52.1) | 40 (33.1) | 18 (14.9) | 69 (57) | 40 (33.1) | 12 (9.9) | 0.439 |
| HPV Testing Is Used to Indicate if The HPV Vaccine Is Needed (F) | 66 (54.5) | 44 (36.4) | 11 (9.1) | 75 (62) | 41 (33.9) | 5 (4.1) | 0.241 |
| When You Have an HPV Test, You Get the Results the Same Day (F) | 47 (38.8) | 42 (34.7) | 32 (26.4) | 75 (62) | 26 (21.5) | 20 (16.5) | 0.0001 |
| If an HPV Test Shows That a Woman Does Not Have HPV, Her Risk of Cervical Cancer Is Low (T) | 53 (43.8) | 51 (42.1) | 17 (14) | 66 (54.5) | 48 (39.7) | 7 (5.8) | 0.095 |
| Items a | Group 1 | Group 2 | p-Value b | ||||
|---|---|---|---|---|---|---|---|
| Correct n (%) | Incorrect n (%) | Do not know | Correct n (%) | Incorrect n (%) | Do Not Know | ||
| Girls Who Have Had an HPV Vaccine Do Not Need a Pap Test When They are Older (F) | 97 (80.2) | 17 (14) | 7 (5.8) | 92 (76) | 28 (23.1) | 1 (0.8) | 0.437 |
| One of the HPV Vaccines Offers Protection Against Genital Warts (T) | 86 (71.1) | 24 (19.8) | 11 (9.1) | 98 (81) | 17 (14) | 6 (5) | 0.071 |
| The HPV Vaccines Offer Protection against All Sexually Transmitted Infections (F) | 91 (75.2) | 28 (23.1) | 2 (1.7) | 83 (68.6) | 38 (31.4) | 0 (0) | 0.253 |
| Someone Who Has an HPV Vaccine Cannot Develop Cervical Cancer (F) | 93 (76.9) | 22 (18.2) | 6 (5) | 92 (76) | 25 (20.7) | 4 (3.3) | 0.880 |
| HPV Vaccines Offer Protection against Most Cervical Cancers (T) | 97 (80.2) | 15 (12.4) | 9 (7.4) | 99 (81.8) | 18 (14.9) | 4 (3.3) | 0.743 |
| The HPV Vaccine Requires Three Doses (T) | 69 (57) | 23 (19) | 29 (24) | 79 (65.3) | 30 (24.8) | 12(9.9) | 0.187 |
| The HPV Vaccines are Most Effective if Given to People Who Have Never Had Sex (T) | 91 (75.2) | 17 (14) | 13 (10.7) | 94 (77.7) | 19 (15.7) | 8 (6.6) | 0.649 |
| Item | Group | N | Mean (SD) | p-Value a |
|---|---|---|---|---|
| General HPV Knowledge | 1 | 121 | 12.97 (2.69) | 0.282 |
| 2 | 121 | 12.87 (2.76) | ||
| HPV Testing Knowledge | 1 | 121 | 3.47 (1.52) | 0.017 |
| 2 | 121 | 3.95 (1.58) | ||
| HPV Vaccine Knowledge | 1 | 121 | 5.15 (1.42) | 0.586 |
| 2 | 121 | 5.26 (1.63) | ||
| Total HPV Knowledge | 1 | 121 | 21.6 (4.74) | 0.449 |
| 2 | 121 | 22.09 (5.24) |
| Items | Mean a | Std. Error | F | p-Value | ||
|---|---|---|---|---|---|---|
| Group 1 (N = 83) | Group 2 (N = 89) | Group 1 (N = 83) | Group 2 (N = 89) | |||
| Total HPV Knowledge | 22.07 | 22.43 | 0.333 | 0.322 | 0.591 | 0.443 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bitar, H.; Babour, A.; Nafa, F.; Alzamzami, O.; Alismail, S. Increasing Women’s Knowledge about HPV Using BERT Text Summarization: An Online Randomized Study. Int. J. Environ. Res. Public Health 2022, 19, 8100. https://doi.org/10.3390/ijerph19138100
Bitar H, Babour A, Nafa F, Alzamzami O, Alismail S. Increasing Women’s Knowledge about HPV Using BERT Text Summarization: An Online Randomized Study. International Journal of Environmental Research and Public Health. 2022; 19(13):8100. https://doi.org/10.3390/ijerph19138100
Chicago/Turabian StyleBitar, Hind, Amal Babour, Fatema Nafa, Ohoud Alzamzami, and Sarah Alismail. 2022. "Increasing Women’s Knowledge about HPV Using BERT Text Summarization: An Online Randomized Study" International Journal of Environmental Research and Public Health 19, no. 13: 8100. https://doi.org/10.3390/ijerph19138100
APA StyleBitar, H., Babour, A., Nafa, F., Alzamzami, O., & Alismail, S. (2022). Increasing Women’s Knowledge about HPV Using BERT Text Summarization: An Online Randomized Study. International Journal of Environmental Research and Public Health, 19(13), 8100. https://doi.org/10.3390/ijerph19138100






